

The muscles, the mitochondria and fibromyalgia – what a potentially potent mix. Over the past six months, at least three fibromyalgia muscle studies have popped up. (Health Rising has reviewed all three). Plus, a study examining energy production problems in fibromyalgia (FM) just appeared.
- Painfully High Muscle Pressures in Fibromyalgia Put Old Paradigm to the Test – Health Rising
- Muscle Study Finds Key Differences in Fibromyalgia and Chronic Fatigue Syndrome (ME/CFS)
In his 2020 Swedish study, “Evidence of Mitochondrial Dysfunction in Fibromyalgia: Deviating Muscle Energy Metabolism Detected Using Microdialysis and Magnetic Resonance“, Gerdle et al. took the study of the muscles in FM to new heights.
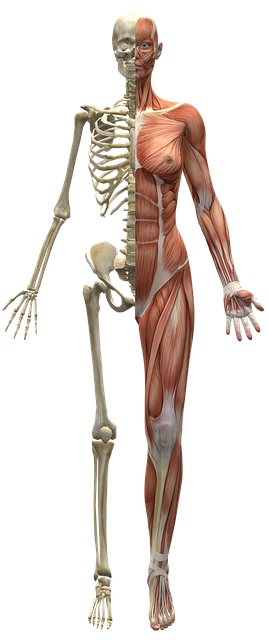
Evidence of muscle problems in FM has been piling up. (Image by Ryan Hoyme from Pixabay)
Gerdle had last studied energy metabolism in FM in his 2013 study, “Decreased muscle concentrations of ATP and PCR in the quadriceps muscle of fibromyalgia patients–a 31P-MRS study – PubMed (nih.gov)“. That study found substantially reduced muscle ATP and phosphocreatinine (30%) concentrations in the quadriceps muscle. It concluded that the abnormalities probably resulted from a combination of inactivity and dysfunctional mitochondria.
The authors, though, seemed to be reaching a bit with the inactivity conclusion. The (rather simple) activity assessment they used in the study indicated that the FM patients and the healthy controls had similar activity levels.
They’d also concluded that the FM group has normal aerobic capacity, but the exercise test (1 day submaximal exercise test) they used has produced misleading results in chronic fatigue syndrome (ME/CFS).
Despite the fact that the BMIs (body mass indices) of the two groups were similar, they also suggested that the higher intramuscular fat levels found in the muscle may have the reflected the higher percentage of obese individuals in the FM group.
After suggesting that fat, inactive FM patients may be contributing to their findings, the authors swung, though, to a fascinating possibility – that even though they were less active, FM patients might still be “overusing” their muscles.
They suggested that psychological factors (high persistence behavior (i.e. overly hard-driving FM patients)), plus studies showing that FM patients’ muscles do not relax in between muscle contractions, plus another study showing an apparently abnormal “activation pattern(s)” (unexplained) suggested that FM patients might be overusing their muscles even as their activity levels suggested they were underusing them.
The authors, it should be noted, also suggested that mitochondrial problems could be causing the reduced muscle ATP and PCR concentrations, and the increased concentrations of lactate and pyruvate that some studies have found.
To be fair, the authors simply seemed to be covering all the bases. More than anything, with these researchers swinging from one hypothesis to the other, this 2013 study simply seemed to show how in flux the muscle field of FM was.
What was causing the strange muscle findings in FM? Was it inactivity, abnormal muscle activation patterns, mitochondrial issues or all of the above? Nobody knew.
Findings Coalesce – the 2020 Study
Seven years later, the group published a study designed to make up for shortcomings in FM muscle studies. It was larger (n=64) (but not all that large), assessed metabolic status in two places (trapezius, erector spinae muscles), assessed blood flows, and used more comprehensive statistics.
The study, “Evidence of Mitochondrial Dysfunction in Fibromyalgia: Deviating Muscle Energy Metabolism Detected Using Microdialysis and Magnetic Resonance” – PubMed (nih.gov) was revealing indeed.
Sometimes it’s hard to tell if a field is making progress. Eight years later, it’s clear that step by step, study by study, this aspect of fibromyalgia research has made real progress.
Results
The time, the authors lead off the discussion with the rather definitive statement:
“FM was clearly associated with higher levels of pyruvate and lower levels of ATP and PCr, a finding that suggests muscle mitochondrial dysfunctions in FM.”

Similar findings have popped up in chronic fatigue syndrome (ME/CFS) (Image-by-Peggy-und-Marco-Lachmann-Anke-from-Pixab)
Noting that this was the fourth study to find so, the authors reported that FM “seems” to be associated with increases in pyruvate and lactate – two products of glycolysis.
That’s a very interesting finding given the similar findings that have shown up in chronic fatigue syndrome (ME/CFS). Pyruvate is the end product of the first half of the energy production program (glycolysis/anaerobic energy production). It is converted into acetyl-CoA, which is transported into the mitochondria where it’s used, in a series of five complex steps, to produce massive amounts of ATP (aerobic energy production).
The higher levels of pyruvate and lactate (a breakdown product of pyruvate) found in the FM patients’ muscles suggest that pyruvate is not getting properly metabolized, thus depriving the mitochondria of the fuel they need.
The lower levels of ATP and phosphocreatine (PCr) found in the FM patients validated that idea. (PCr is important for the muscles as it “shuttles” a phosphate from ATP to the them).
The Gist
- Numerous studies have found muscle abnormalities in fibromyalgia dating back for decades
- This Swedish group’s 2013 study found signs of mitochondrial dysfunction (low ATP, PCr) in the muscles of FM patients. The authors pointed to a variety of different factors that might have come into play (mitochondrial problems, muscle overuse, inactivity, obesity).
- Seven years later the authors returned with a bigger, more effective study – and a stronger conclusion. They again found evidence of reduced ATP and PCr as well as increased pyruvate. Similar findings have shown up in chronic fatigue syndrome (ME/CFS)
- With proteomic, metabolomic and other studies coming to similar conclusion the authors concluded that mitochondrial problems are present in FM.
- They also proposed that mitochondrial problems are playing a role in chronic pain in general and noted that pain is common in people with primary mitochondrial disorders.
- The authors also reported that reduced ATP levels have been found in a wide variety of tissues including the muscles, skin, plasma, platelets, nerve and immune cells.
- While obesity was increased in FM the analyses suggested it had no impact on the muscle issues found.
- An altered phosphorous/PCr imbalance and increased pyruvate levels seemed to particularly impact pain levels.
- The authors suggested that a variety of factors may be in play including oxidative stress and mitochondrial induced inflammation.
The authors proposed that mitochondrial problems were likely the problem – not just for FM patients – but for others who experience chronic pain. (They also noted that chronic pain is common in people with mitochondrial diseases). They aren’t the first to propose that and, in fact, proposed that possibility in the 2013 paper, but now have much stronger legs to stand on. At least six studies from the past couple of years have come to the same conclusion. That those studies are coming to similar conclusions from different directions (proteomic, metabolomic, urine metabolite studies) – suggest that the finding is a robust one.
When it came to explaining the findings, the authors were, again, at something at a loss. They noted that aging and obesity – neither of which could explain FM (plenty of young people have FM, and plenty of obese people do not) are associated with mitochondrial problems.
While higher rates of obesity were found in the FM patients (FM – 27.3% overweight, 42.4% obese/severe obese; controls – 22.6% overweight, 6.5% obese/severe obese; p < 0.001) but the multivariate statistics suggested it played no role in the FM patients. (Increased BMI in both groups, though, was associated with reduced PCr ATP and pyruvate levels.) In this larger study, the submaximal exercise test also suggested that aerobic capacity was lower in the FM patients.
Given the possible connection between altered circadian rhythms and mitochondrial activity, they suggested that poor sleep in FM might play a factor. They also brought up the possibility of overactive muscles.
The authors also noted that the low PCr levels were throwing the PCr/phosphorous balance off – affecting blood flows and pain levels. Regression analyses indicated that fifty percent of the pain intensity could be explained by problems with blood flows and the metabolic abnormalities. The phosphorous/PCr imbalance and the increased pyruvate levels were particularly important factors.
They noted that another study found that proteins associated with mitochondrial production were strongly implicated in the production of pain. (Interestingly, a large cytokine study found that cytokines were not.)
In the end, the authors painted a complex picture in which increased oxidative stress, mitochondrial-induced inflammation, a mitochondrial-produced “damage-associated molecular pattern” which triggers inflammation, NLRP3 inflammasomes that tweak sensory neurons, and others could be involved.
In their conclusion, the authors noted that they’d found significant metabolic and blood flow alterations in the muscles of FM, which may result from dysfunctional mitochondria in the muscles. After the pages of dense biological discussion, it was strange to see the authors revert to their tropes from eight years ago.
“Although it is unclear why muscle mitochondrial dysfunctions are found in FM, inactivity, obesity, aging, and pain per se may be involved.”
Perhaps the editors of the journal demanded it.
All of this brings up an intriguing question: With all the evidence of ATP and muscle problems that have been found in FM, why does exercise seem to work – and how well does it work?






In answer to why does exercise seem to work: Exercise helps everything in the body including depression. Most fibromyalgia patients experience with exercise is that it causes the pain to be worse and can cause a flare up. Exercise will keep muscles conditioned but there is a high price of increased pain to pay.
Exercise may aid with blood flow, plain and simple
Re “With all the evidence of ATP and muscle problems that have been found in FM, why does exercise seem to work – and how well does it work?”
I can’t say why exercise seems to work and in my case, it’s only certain exercise like walking in nature so I can only postulate that when I am in pain, I tend to walk which seems to help somewhat to ease my pain so can’t say if it’s due to endorphins being released in response to walking or what else it might be. I do know that since being on T3-only thyroid medication for Hashi’s with hypothyroidism, eating/living a low-to-no inflammatory diet and lifestyle, balancing sex hormones with some forms of BHRT, getting some decent sleep finally from prescription high dose melatonin & Nabilone (synthetic THC) & a GABA containing OTC product with some other sleep aids, and Low Dose Naltrexone, I am largely pain-free now but still have no energy reserves so that might be due to mitochondrial dysfunction as I still tire easily but also am no longer sick at the drop of a hat anymore, constantly fighting off some kind of upper respiratory bug week to week like I did for 18 horrible years prior to the above measures. I just wish I could find a way to conquer the low energy issue!
May be all the mitochondria in the muscles are not dysfunctional!
Remaining normal mitochondria produce enough ATP that could help the FM patients, though for a little while. Thus explains that exercise is helpful.
HELLO WOW I SEEM TO BE LIKE YOU. HAVE NOT GOTTEN TO THE HEALING POINT. YOU HAVE GOOD INFO O WILL TRY TO START. I LIVE IN TOO COLD A CLIMATE. NEED TO MOVE. BUT.. CANT…YET.
REPLY IF YOU SEE THIS. WOULD LOVE TO SHARE MORE. GOING TO TRY YOUR IDEAS.
TAKE CARE.
I remember reading Myhill, Booth, and McLaren-Howard (2009) over 10 years ago and thinking there was an answer. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2680051/
At times it feels as though we’re going nowhere fast. I have continued hope that at some point researchers use their findings to propel some more effective strategies that medical professionals will adopt.
Yes it can feel that way but check out what’s happened to the muscle findings in FM over the past 8 years. More studies have popped up – and almost imperceptibly a wave has been going. It seems that these studies are prompt even more studies. My hope is that the evidence will continue to build with the mitochondrial connection to FM and chronic pain in general will be a major thing – and will produce more effective strategies.
Another hopeful endeavor is the huge effort the NIH is putting into understanding exercise – something that could and should benefit both diseases.
@Cort, what about the study that the Lights did in Utah? They measured the Mitrochondria Complexes and their functions and energy out put. That’s just one of the things they looked at. There were many other genetic markers that came up connected too. But for me, Mitrochondria was a huge flag of dysfunction.
Absolutely. I agree. I’d simply like to see more research testing strategies at this phase, along with the research for cause and effect. Staying the course and keeping an eagle eye – thus always appreciating those in this community who keep reading voraciously and sharing!
(Considering pain, fatigue, brain fog, and oft disillusionment, I always admire this community for their resiliency and continued effort.)
Here is my study as part of my dissertation looking at how mindfulness can promote better mood therefore less pain.
https://nupsych.qualtrics.com/jfe/form/SV_73z43yvl4uB8194?Q_CHL=social&Q_SocialSource=facebook
Emma, I practiced mindfulness last night. I woke at 1am with burning pain in my arms and back pain. I could not get back to sleep for 1.5 hours. I practiced mindfulness, deep breathing, paying attention to the painful areas, and was asleep in 1/2 hour. My i-watch sleep report shows 2 hours of deep sleep in the next 4 hours and my HRV was much higher than normal. I woke up feeling refreshed. I am so happy to have learned mindfulness techniques from apps that I subscribed to. I no longer need the paid subscription to practice effective mindfulness.
Mare what dose of melatonin do you use? And what kind of doctor prescribed it?
This study is fascinating! Muscles are like batteries, which reminds me of this paragraph from Dr Jacob Teitelbaum’s 4th ed. of “From Fatigued to Fantastic“ “Because of the body-wide energy crisis seen in CFS/FMS, most of you have found that you are unable to condition beyond a certain point. This is because it takes energy to store energy in the muscles, which is what conditioning is. And the energy crisis in this illness has limited your ability to make this energy. Most physicians are not aware of this. Instead they usually push you to exercise, and you spend the next two days in bed . . ) “ he goes on to say that you have to build up your energy stores (the book is about using his protocol to do so) before saying you will then be able to make the energy to store energy and be able to exercise more and more, which will lead to feeling stronger and stronger. My son’s exercise physiologist is following a similar plan: Rest, analyse, supplements & meds, psychological support and time = partial recovery. Next step is a little walking to start to store energy.
Christobel, thank you for highlighting a quote from
Dr Jacob Teitelbaum’s 4th ed. of “From Fatigued to Fantastic“
$ are tight, but this picqued my interest.
thanks again
This will be a rather technical comment.
In the muscles myoglobin is sort of an essential secondary carrier of oxygen, next to hemoglobin found in the RBC.
The paper “Lack of myoglobin causes a switch in cardiac substrate selection” From “Ulrich Flögel,… Jürgen Schrader” says:
“Myoglobin is an important intracellular O2 binding hemoprotein in heart and skeletal muscle….”
“the observed shift in substrate metabolism benefits energy homoeostasis and therefore represents a molecular adaptation process allowing to compensate for lack of the cytosolic oxygen carrier myoglobin.”
So, myglobin sort of helps transport oxygen from the cell wall to the mitochondria.
Now, a nasty chemical called Wikipedia(Methylglyoxal) is formed more under conditions of high blood sugar (ME/?FM? tends to have elevated morning blood sugar) AND during lipid peroxidation. Lipid peroxidation happens at large scale if there is plenty of oxidative stress inside the cells (and mitochondria can produce plenty of oxidative stress (inside the cells) in a defensive reaction or when oxygen supply is too low).
Now here comes a long shot hypothesis I had to dig deep for, but the paper “Methylglyoxal-induced modification causes aggregation of myoglobin” from ”
Fatemeh Elahian, Zargham Sepehrizadeh, Bahareh Moghimi, Seyed Abbas Mirzaei” says:
“Post-translational modification of proteins by Maillard reaction, known as glycation, is thought to be the root cause of different complications, particularly in diabetes mellitus and age-related disorders. Methylglyoxal (MG), a reactive α-oxoaldehyde, increases in diabetic condition and reacts with proteins to form advanced glycation end products (AGEs) following Maillard-like reaction…
…MG induces significant structural alterations of the heme protein, including heme loss…
…These changes occur gradually with increased period of incubation. Incubation of Mb with MG for 7 days results in formation of the AGE adducts…
…On increasing the period of incubation up to 14 days, additional AGEs namely…
…MG also induces aggregation of Mb, which is clearly evident with longer period of incubation (18 days), and appears to have amyloid nature. MG-derived AGEs may thus have an important role as the precursors of protein aggregation, which, in turn, may be associated with physiological complications.”
The reaction of the nasty chemical methylglyoxal (formed plentifull during high reactive oxidative stress inside cells) with myoglobin (obviously too inside the cells as its function is to store and transport oxygen inside cells) creates:
* broken defunct myoglobin less able to store and transport oxygen inside muscle cells
* amyloid like protein aggregation; that is a process similar to forming plaque in Alzheimer Diseasse patients and its nasty stuff that is hard to remove and it would aggregated inside the muscle cells.
Important note: one of the people having most FM insights that used to be frequent on Healthrising, Phillip Hayward, sort of in half of all his many comments mentioned those “lumbs” forming (quickly) in his muscles.
Here is another paper “Effect of aldehyde lipid oxidation products on myoglobin” by “M P Lynch, C Faustman”
“The effects of aldehyde lipid oxidation products on myoglobin (Mb) were investigated at 37 degrees C and pH 7.2. Oxymyoglobin (OxyMb) oxidation increased in the presence of 4-hydroxynonenal (4-HNE) compared to controls (P < 0.05). Preincubation of metmyoglobin (MetMb) with aldehydes rendered the heme protein a poorer substrate for enzymatic MetMb reduction compared to controls"
"Preincubation of MetMb with 4-HNE enhanced the subsequent ability of the heme protein to act as a prooxidant in both liposomes and microsomes when compared to controls (P < 0.05); the effect was reduced in microsomes containing elevated concentrations of alpha-tocopherol (P Translated:
The products formed by interaction between strong oxidative stress inside the cells and the cell walls are called “aldehyde lipid oxidation products”.
The previous paper showed that the “aldehyde lipid oxidation product” methylglyoxal can create “amyloid like plaque” when it interacts with myoglobin.
The current paper shows that another “aldehyde lipid oxidation product” 4-HNE can impair recycling of oxidized / “broken” metmyoglobin. Wikipedia(Metmyoglobin) is oxidized myoglobin and has poor oxygen storing and carrying capacity and has pro-oxidant properties further increassing oxidative stress.
Both problems can create a vicious circle:
* Amyloid like structures and “lumbs” building up inside cells isn’t a good thing. A natural reaction of the body to it will be either to invite / attract immune cells to attack those aggregations and / or to switch mitochondria to their pro-oxidative stress producing mode (that also lowers ATP production) in order to bombard these lumbs with oxidative stress. When these lumbs are however formed as a reaction between myoglobin and byproducts of too much oxidative stress, new damaged myoglobin may be quicker produced then the oxidative stress can “eat” away.
* Metmyoglobin is *another* form of changed myoglobin. It can be recycled to “good” myoglobin, but the same lipid peroxidation products that cause myoglobin aggregation also slow down recycling of metmyoglobin to “good” myoglobin. As oxidized myoglobin aka metmyoglobin increases oxidative stress, it offers the change to create more lipid peroxidation products and in this way too creating a vicious circle.
=> The combination of low blood volumes, poor blood flow, constricted blood vessels, unflexible RBC, RBC in part being (staying) inflexible due to high oxidative stress and aldehyde lipid peroxidation products, RBC unwilling to give away their oxygen to the tissues… could add up with myoglobin being oxidized and aggregating.
All pull towards the same outcome: less oxygen provision to the mitochondria, more oxidative stress produced by both the RBC (damaged heme due to oxidative stress further increases oxidative stress), increased metglobin and oxygen starved mitochondria (mitochondria increase oxidative stress production both when there is too much and too few oxygen available to the mitochondria).
That all pulls towards increasing lipid peroxidation, and that can (will) further damage RBC and myoglobin.
Too much and intense exercise would in that view be a logical danger: if oxygen shortage is present at rest, it will get a lot worse during long and intense exercise. Some exercise can however help with circulation and removal of waste products. The balance between some and too much however is delicate.
Side note: cytochromes and complexes I-IV in the cells and mitochondria have heme properties too and hence might be prone to some of these processes too. So cells without myoglobin still *may* be prone to similar damage / vicious circles. If I recall well research says the complexes I-IV for example can degrade due to excessive oxidative stress and the damaged complexes I-IV become sources of increased oxidative stress themselves.
Exercise doesn’t work for all Fibromyalgics. Whenever I get into any exercise that is meaningful, I feel like I cannot get enough oxygen & I start sucking in air. I have no lung impairment, no cardiovascular problems. I also get fatigued for 3-4 days after, even if it’s just walking for 2o minutes 2 days in a row. Then I cannot even do just basic chores around the house. I have settled into just doing chores & small outside things that must be done because anything more robust and calorie burning, leads to far too much time lost due to fatigue. I live alone; there is no one else to do anything if I am down for 4 days exhausted.
SAme here. What little energy I have is used doing daily maintenance of my home and myself. I have no caregiver … its just me. So ‘exercise’ is a luxury I can ill afford.
PS: If I force myself to get down on the floor and do some modified yoga stretches, my muscles do feel better. But finding the energy does not happen often.
Judyjo and TigerKim, I wholeheartedly agree. I have the same issues. I can no longer cook, do laundry, or clean. I have no social life. Ten years into full disability and no improvement in stamina. Exercise makes my horribly ill. Anything that taxes my body makes me ill.
iI hear you!
To Tiger Kim, I hear you!
to Tiger Kim, I understand what you are saying.
I’m not surprised by this at all. I have fibromyalgia and lost two infants over 30 years ago from a mitochondrial myopathy cytochrome oxidase deficiency complex IV
I’m still trying to get to the right doctor’s
I’m glad their doing more research on this
Hope they can find something to help people
Many years ago, in the mid-nineties, while living in Germany, Drs diagnosed “mitochondriapathy” as the reason for my muscle pain and weakness. Exercise only exacerbates the lack of function, and causes flares within a day or two. Drs in North America routinely rolled their eyes in disbelief and ignorance at this term involving the mitochondria, but could never offer another explanation. I was subsequently diagnosed with FM by a rheumatologist, but again with no help for treatment. I seemed to improve with the guaifenesin protocol, but had to discontinue when it was no longer available here in Canada. The lab which provided the guai in bulk was banned by the government. In the years since then, my condition has continued to worsen, with complications too numerous to mention. I continue to read whatever I can find re other people’s experiences, and really appreciate “Health Rising” and this blog. The recent article re mitochondrial involvement in FM is particularly interesting.
Cort, this may sound off the wall, but I’ve had an interesting experience in the last six months or so. I’ve been working for over 5 years with my endocrinologist to address my hypothyroid and blood sugar issues (I have had both ME/CFS and FM since 2006). We were able to get them both under control. I still had to pace drastically, and was unable to do much of any kind of exercise. Then, about 9 months ago he put me on Rybelses, along with the Metformin SR that I was already on and lo and behold, after about 3 months, I was able to walk a little – a quarter mile or so. A little more tweaking, and I’ve been walking up to 1 1/2 miles. Yes, I still have to pace, but this is something I haven’t been able to do in years! With what I’m reading about the glycolysis and other metabolic processes, I’m very curious as to what is exactly happening to my mitochondria. It hasn’t affected pain much, but I just deal with it. Also, as a person who hasn’t been able to lose weight at all in the last 30 years, even with a restricted calorie diet and exercise regimen (my leptin levels were about 3 times higher than they should have been), I’m actually starting to lose weight to the tune of about 1 pound a week. Energy to walk and losing weight works for me! The only thing that has changed is the Rybelses being added in. It would be very interesting to figure out how that changed things.
(Certain types of) exercise can induce mitochondrial biogenesis.
Might be one way movement can be beneficial.
The key is in which type of movement, and at which point in the recovery process.
{ personally, movement inside a body of water works best for me, as did taiji. Better yet: taiji inside water }
Lack of ATP produces something like a pre-rigor mortis state in muscles. The ‘hypertonicity’ of FMS (and ME/CFS and hEDS for some…)
The minerals that are inside vs outside the cell also has something to do with this.
So, the right kind of movement at the right time, i.e. when prometabolic measures are already in place, getting ATP back into the cell, etc.
“Lack of ATP produces something like a pre-rigor mortis state in muscles. The ‘hypertonicity’ of FMS”
Do you have a link to info about this phenomenon?
That is intriguing! I’ve read two places that reduced ATP levels causes the muscles to stay in a contracted state. If I remember correctly – it takes more energy to relax the muscles…
Tronstad in Norway has hypotezised that a fault in the pyruvate dhydrogenase enzyme happens in ME. (And is still working on testing the hypothesis)
https://pubmed.ncbi.nlm.nih.gov/28018972/
Lien has found increased lactate in ME
https://pubmed.ncbi.nlm.nih.gov/31161646/
This sounds remarkably familiar…
Something I continue to find very puzzling is the seeming lack of recognition of the fact that thiamine is an essential cofactor to, among others, the functioning of the pyruvate dehydrogenase enzyme complex, without which it doesn’t work properly. If thiamine is deficient, pyruvate is unable to enter the citric acid cycle, instead being converted to lactate via anaerobic metabolism, with greatly reduced ATP production. This is routinely discussed in papers and articles, for example:
https://med.virginia.edu/ginutrition/wp-content/uploads/sites/199/2014/06/Parrish-March-17.pdf
To me this strongly suggests that thiamine deficiency has a part to play in ME/CFS and related conditions. Yet the whole subject of thiamine deficiency seems to be curiously “missing in action” in ME/CFS discussion and research, such as the Norwegian research of Dr Fluge, and that of Dr. Davis and the Open Medicine Foundation, and now in this new research. I have pointed this out numerous times on Twitter, e.g.:
https://twitter.com/boretrol/status/1381588914587148290
and since August I have been tweeting about the similarity between symptoms of Long Covid and ME/CFS, and thiamine deficiency disease, otherwise known as beriberi. As my pinned tweet thread states, my suggestion is based on the work of Drs Derrick Lonsdale and Chandler Marrs, who published a very comprehensive book in 2017 called “Thiamine Deficiency Disease, Dysautonomia, and High Calorie Malnutrition”. Dr Marrs runs a website called “Hormones Matter” which has many articles which should be of interest to readers of this blog. I believe the work of Dr. Lonsdale will eventually be recognized as the key to many chronic conditions, including ME/CFS and Long Covid.
It is the same old, same old what came first chicken or the egg over and over again; anyone else sick of the merry-go-round??
There are plenty of folks who are ill who are young AND not over-weight who also suffer from M.E. – CFS – FM or any combination thereof. I am so frustrated, heartened, and thoroughly underwhelmed with the continued push that people who are ill with these conditions are just over-weight, old and out of shape.
There are many people who first became ill when young and in top physical condition; that can’t be explained away with : could be you are just old and fat and out of shape.
It is disgraceful and simply comes down to lazy science
Yes, indeed. It’s disheartening I know – particularly since obesity, as you point out could never be THE answer. Researchers do have to try and account for everything and since BMI can effect metabolism it has had to be taken into account. To be fair to these researchers they never ever suggested that obesity was the answer – they just wondered if it needed to be accounted for. They found that it did not.
The same thing has happened with ME/CFS with deconditioning. It was always a possible confounder and for decades, really, some thought it skewed the exercise results. That actually made sense as deconditioning can do that just as obesity can. Studies finally showed, including a very recent one, that it doesn’t have any effect on them.
This makes the most sense to me of all the studies and hypotheses I’ve read over my 25 yr battle with FM. I’m encouraged but hope it can move along quicker. Don’t agree at all with the earlier findings re: inactivity or obesity bring a factor though. I was in the prime of my life, vibrant, exercise nut, and healthy eater when FM came on. With this 2020 study/theory they need to look for similarities in histories of the participants or do a separate study on similarities. Just my humble opinion.
I bought an infrared light for muscle pain. It takes about 15 and the pain is gone. I use it every day. It is very comforting and soothing. I could not survive without it. Over time it heals up the mitochondria. You want a four wave light. Best Buy is from the lifegivingstore.com. Be sure to ask for the four wave As he has others . My dr suggested it
My cousins Dr in Colorado recommended taking (and I know how weird this sounds) mucinex every day because he believes FM occurs due to phosphate dysfunction that prevents the production of ATP. Mucinex apparently contains something that helps the body properly use phosphate to make more ATP…. idk it seems to be helping her a lot.
The tone of the article is misguided. Terms such as “seems”, “suggests” and” “infers” are used because in emprirical research, the data leads, not the hypothesis. It is a standard scientific approach to leave leeway for studies that don’t support the research, and further development.
Furthermore, the objective of research is not to form a definitive conclusion. It is to increase the research and data in a specific area. The fact that there were lots of question marks in terms of what the 2013 findings were is very typical, and if you read the Discussion sections of all empirical studies, you will always see areas the researchers suggest for further study. This also the area were mutliple suggestions as to why the data may look the way is does is the whole point of data research, and is standard practice and an important scientific step in understanding a phenomenon,especially a new development.
So next time just report the findings without your snarky uninformed remarks. Thanks.
Part of reviewing research is pointing out its shortcomings. Sorry that approach disagrees with you.