

The Mitochondrial Enhancers for Chronic Fatigue Syndrome (ME/CFS), FIbromyalgia (FM), and long COVID Series
This is the second part in a series on mitochondrial enhancers for chronic fatigue syndrome (ME/CFS), fibromyalgia (FM) and long COVID series. The series uses the book “Mitochondria and the Future of Medicine”, by Lee Know, a former naturopathic doctor in Canada, as a starting point, and includes insights from ME/CFS/FM practitioners.
- Pt I: D-Ribose, CoQ10 and PQQ
- Pt II: L-carnitine and Acetylcarnitine
- Pt. III: Magnesium
- Pt IV: N-acetyl cysteine (NAC)
- Pt V: Oxaloacetate
- Pt. VI: Niacin, Niacinamide and Nicotinic Riboside
Now the series turns to two interesting supplements that play vital roles in energy production: L-carnitine and acetylcarnitine.
L-carnitine and Acetylcarnitine
Several different forms of carnitine exist. While one form – L-carnitine L-tartrate – might be helpful in reducing muscle soreness and enhancing recovery after exercise, this review mostly focusses on L-carnitine and acetylcarnitine (also known as acetyl-l-carnitine).
L-carnitine
L-carnitine and acetylcarnitine (ALCAR) are similar but different. While Self-hacked reports that both can help with fatigue, L-carnitine is the bigger energy enhancer. It helps the body convert fat into energy by transporting fatty acids to the mitochondria, and has strong antioxidant properties as well.
According to Know, low L-carnitine levels inevitably result in reduced fatty acid metabolism. That’s important because our mitochondria love fatty acids: 60-70 percent of the energy produced by our mitochondria comes from metabolizing fatty acids. L-carnitine, also, interestingly enough, helps to mop up lactate – a byproduct of anaerobic metabolism – which may be causing a lot trouble in ME/CFS/FM.
Weight-lifters and other athletes latched onto L-carnitine early and the study results have been good. A 9-week placebo-controlled, double-blinded 2019 study of weight lifters found increases in peak power, antioxidant levels and reduced lactate levels. A quickie study found it improved antioxidant levels 1 hour after exercise – an interesting finding, as Nancy Klimas has reported that exercise triggers an unusually large burst of free radicals in ME/CFS. (Plus, oxidative stress appear to be high even at rest in ME/CFS). Another study found that supplementing L-carnitine with choline reduced oxidative stress after walking in women.
Fielding believes L-carnitine may be increasing blood flows and oxygen supply to the muscles – two other subjects of interest in ME/CFS.. One study, interestingly, given the interest in ammonia in ME/CFS, found L-carnitine may be able to reduce ammonia production during exercise.
Acetylcarnitine
Acetylcarnitine (or acetyl-l-carnitine, ALCAR,LAC, LCAR or a number of other acronyms and names), on the other hand, boosts acetylcholine and is able to get through the blood-brain barrier. It appears to be more effective at improving mental clarity, reducing mental fatigue, improving mood and protecting the neurons in the brain.
An Antidote for Depression?

Acetylcarnitine may be as effective as antidepressants – and with fewer side effects.
Acetylcarnitine is also being enthusiastically studied in depression. A 2018 two-center study (as well as other studies) have found decreased acetylcarnitine (LAC) levels in the brains of people with depression. The more severe the depression, the greater the LAC reductions. Greater LAC reductions were also found in women who had experienced childhood trauma.
The authors reported that LAC supplementation “induces rapid and lasting antidepressant-like effects via epigenetic mechanisms” which dampen down the release of the excitatory neurotransmitter glutamate.
One of the few meta-analyses I’ve read that uncategorically reported a positive outcome stated that acetylcarnitine was as effective as antidepressants and had fewer adverse effects:
“Acetyl-L-supplementation significantly decreases depressive symptoms compared with placebo/no intervention, while offering a comparable effect with that of established antidepressant agents with fewer adverse effects.”
Help for Neurological Disorders
Both L-carnitine and acetylcarnitine are also being studied in neurological disorders. A literature review reported that both substances are being studied for Alzheimer’s disease, depression, neuropathic pain, bipolar disorder, Parkinson’s disease and epilepsy in the elderly.
Besides the impact these substances may have on metabolism and energy production, the authors mentioned their ability to eliminate ammonia – which is, again, of interest in ME/CFS.
They stated that “ammonia and energy depletion seem to underlie most of the neurotoxic events” and concluded that acetylcarnitine “emerges as a simple, economical and safe adjuvant option in order to impair the progression of most neurological disorders.”
RxList reports that acetyl-l-carnitine is being used in a staggeringly wide variety of conditions ranging from Alzheimer’s to Lyme disease, to alcohol withdrawal, to multiple sclerosis and others. The website states that the evidence indicates that acetylcarnitine is possibly effective for improving memory problems, tiredness, testosterone deficiency, poor blood flows to the brain, reducing nerve pain, etc.
L-Carnitine Tartrate
To make matters a little more confusing, there’s also L-carnitine tartrate (LCLT), which a 2013 blog called a “new more promising form of carnitine”.
LCLT appears to be a somewhat pumped up form of L-carnitine. It’s reported to enhance fat metabolism, increase testosterone uptake into the muscles, reduce oxidative stress and improve lipid metabolism and energy production. It’s also most commonly used for its potent fat burning effects; i.e. apparently to leave one looking sleeker.
One site recommended taking LCLT with carbohydrates because of its possibly favorable impact on insulin.
ME/CFS and Fibromyalgia Studies
Several, but not all, studies have found evidence of acetylcarnitine deficiency in ME/CFS. Four studies reported reduced plasma l‐carnitine (free carnitine), total carnitine and/or acetylcarnitine levels in patients with ME/CFS. For instance, a small study found reduced acetylcarnitine in the brain in ME/CFS and a Chinese metabolomic study found that exercise decreased levels of L-carnitine in ME/CFS.
Several metabolomic studies suggest that disturbances in fatty acid metabolism may be present in ME/CFS. One found evidence of altered plasma levels of carnitine and other metabolites.
Some other studies, however, have failed to find reductions in either L-carnitine or acetylcarnitine.
The Australian Study
The premium ME/CFS carnitine study took place in Australia in 2010. Because carnitine exists in various forms in the body, the researchers speculated that assessing total carnitine levels might be obscuring deficiencies in individual carnitines. Their mass spectrometry study, “Long‐chain acylcarnitine deficiency in patients with chronic fatigue syndrome. Potential involvement of altered carnitine palmitoyltransferase‐I activity“, looked at twenty carnitines.
The study found no difference in total carnitine levels but significant reductions in 8 individual carnitines. The authors particularly pointed to reductions in two carnitines: oleyl‐l‐carnitine (C18:1) and linoleyl‐l‐carnitine (C18:2), which were highly correlated with fatigue levels in ME/CFS.
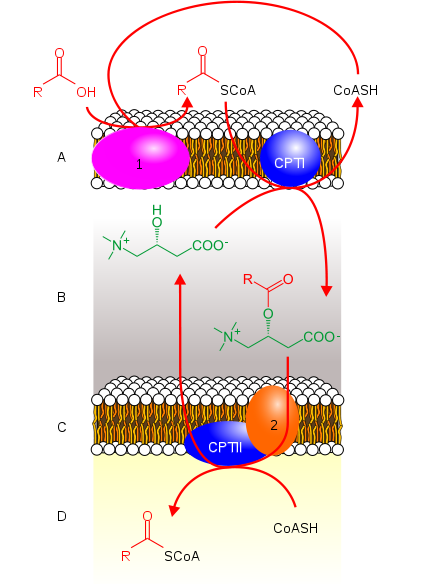
L-carnitine helps transport the mitochondria’s favored food – fatty acids – into the mitochondria (from Wikimedia).
They proposed that a reduction in the enzyme (CPT-1) responsible for the production of acetylcarnitine was likely responsible for the declines.
Piggybacking on a Maes study, the authors speculated that the ratio of free fatty acid to acylcarnitine (for certain acyl groups) was probably 2‐ to 3‐times higher in people with ME/CFS. Those “free” fatty acids aren’t doing much good if they’re not being burned up as fuel.
The authors proposed supplementing omega‐3 fatty acids in combination with l‐carnitine in order to boost the activity of the key enzyme (CPT‐I) in this process. That was an interesting suggestion given that low omega-3 levels have been found several times in ME/CFS, including one study in which over 90% of ME/CFS patients were found to have low levels.
The Gist
- L-carnitine and acetylcarnitine are two forms of carnitine that play vital roles in the energy production process.
- By enhancing the transport of the mitochondria’s main source of energy – fatty acids – L-carnitine is the big energy booster and is (with L-carnitine-titrate) the form of carnitine often used to boost athletic performance. Athletic studies have generally found that L-carnitine can improve performance and may be able to reduce lactate levels.
- Acetylcarnitine, on the other hand, is more often used to improve cognition, alertness, mental fatigue and mood. It’s being assessed in a surprisingly wide variety of neurological and mood disorders, and has been touted as a mostly side-effect free antidepressant.
- Some chronic fatigue syndrome and fibromyalgia studies have found reduced carnitine levels while others have not. The most sophisticated L-carnitine study found normal levels of total carnitine but reduced levels of individual carnitines, which correlated well with increased fatigue levels. Dr. Myhill reports that she invariably finds low carnitine levels in her ME/CFS patients.
- The L-carnitine/acetylcarnitine clinical trials in ME/CFS/FM are mostly rather primitive but have generally produced good results.
- Both Dr. Myhill and Dr. Teitelbaum suggest using 1-2 grams/day broken up into several doses.
- High doses (2-4 grams/day) may suppress thyroid functioning. Since low thyroid functioning also impairs carnitine functioning, some practitioners use carnitine in hypothyroid patients to improve energy levels. One study found that lower doses of carnitine improved the fatigue of their hypothyroid patients.
- The fact that L-carnitine is metabolized to TMAO – a factor associated with cardiovascular disease – raises other concerns. This is another complex issue as it’s not clear that TMAO is causing cardiovascular diseases and studies suggest that L-carnitine can improve cardiovascular fitness and does not promote factors known to cause aetherosclerosis.
- Supplementing carnitine with omega-3 fatty acids, choline, alpha lipoic acid, Vitamin C and B vitamins may be helpful.
- While studies suggest that something has gone wrong with the mitochondria in these diseases, we don’t know exactly – making it impossible to devise a targeted treatment plan. Still, both L-carnitine and acetylcholine, probably in conjunction with other mitochondrial enhancers, present an intriguing possibility.
Treatment Trials
We’re missing the large placebo-controlled, double-blinded studies that would give us results we could count on, but a couple of studies do suggest that acetylcarnitine supplementation could be helpful.
Two grams/day acetyl-l-carnitine improved mental fatigue and concentration in an open label ME/CFS study. L-carnitine improved most of the clinical parameters assessed in a 1997 ME/CFS study. One interesting study found ME/CFS patients who responded to azithromycin favorably tended to have low levels of acetylcarnitine. (Those who did not respond well to azithromycin did not.)
Fibromyalgia and Chronic Pain
A metareview of 18 metabolomics studies suggested that altered acetylcarnitine metabolites may play a role in chronic pain
A 102-person, double-blinded, 2007 Italian fibromyalgia study found that 2 capsules/day of 500 mg of acetyl-L-carnitine (LAC) plus one intramuscular (i.m.) injection of 500 mg LAC for the first 2 weeks, plus 3 500 mg capsules daily for the next 8 weeks resulted in significant improvements in visual analogue pain scores for both the treated and the placebo group. (Placebo does work!) Only the acetyl-L-carnitine group, though, showed significant improvements in functional (SF-36) scores.
A 2015 randomized, controlled trial which compared duloxetine to 1500 mg/day acetyl-L-carnitine (500 mg 3x’s/day) for 12 weeks found that both treatments resulted in reduced pain, reduced depressive symptoms and improved quality of life.
Other Studies
An interesting 2008 trial provided acetylcarnitine to almost 100 fatigued people over the age of 70 who met at least six of the minor Fukuda criteria for ME/CFS. Significant reductions in mental and physical fatigue were found. Plus, muscle pain and fatigue after exercise were reduced, and sleep was improved.
Acetylcarnitine supplementation reduced both mental and physical fatigue, and improved health-related quality of life in people undergoing treatment for hepatitis C (the treatment for hepatitis C treatment produces symptoms that are similar to ME/CFS.)
A large cancer study did not find, however, that 2g of L-carnitine a day improved fatigue in cancer patients and a meta-review did not support the use of carnitine for fatigue in cancer.
Doctors’ Reports
Sarah Myhill reports that her patients are almost always low in acetylcarnitine and regularly prescribes 2 grams of L-carnitine/day. Dr. Teitelbaum recommends 1-2000 mgs acetylcarnitine a day for 3-4 months and then dropping down to 500-1000 mgs/day. He reports that taking more than that may be less effective.
Side Effects
L-carnitine and acetylcarnitine are mostly described as side-effect free. At high doses, though, they may cause insomnia and gastrointestinal irritation.
One possible issue of concern people with ME/CFS/FM is the possibility that carnitine may inhibit thyroid production. High doses of carnitine (2-4 grams/day), in fact, have been used to reduce the high thyroid production found in hyperthyroidism. One website recommended avoiding any form of carnitine if you are on levothyroxine.
Other believe the issue is be more complex than that. Because thyroid plays an important role in L-carnitine’s ability to transfer fatty acids into the mitochondria, low thyroid levels can negatively impact carnitine effectiveness and energy levels. Some sites actually recommend carnitine for people with low thyroid (hypothyroid), and a 2016 placebo-controlled trial found L-carnitine improved physical and mental fatigue in hypothyroid patients. Another website actually lists L-carnitine as an essential supplement for hypothyroidism. Neither Teitelbaum nor Myhill mentioned thyroid as a possible issue at the doses they recommend.
Because L-carnitine’s is metabolized to TMA-N-oxide (TMAO) – a marker that’s been associated many times with an increased risk of cardiovascular disease – concerns have been raised about it’s effects on atherosclerosis and kidney disease.
This, too, is a complex issue as L-carnitine’s ability to enhance fatty-acid metabolism and reduce oxidative stress and inflammation has also lead it to be used to support heart health. While twenty-four weeks of L-carnitine supplementation did dramatically raise TMAO levels, it did not affect any of the markers (C-reactive protein, interleukin-6, tumour necrosis factor-α, L-selectin, P-selectin, vascular cell adhesion molecule-1, intercellular adhesion molecule-1 or lipid profile markers) associated with atherosclerosis. Other studies found that as L-carnitine supplementation raised TMAO levels it also decreased markers of blood vessel injury and oxidative stress, and improved lipid profiles, and did not increase signs of vascular inflammation. A recent review (funded by an L-carnitine manufacturer) proposed that TMAO is the result of an already present injury and is not causative.
Still many studies have linked high TMAO levels to cardiovascular issues. Like so many issues in medicine, the TMAO issue is not as clear as one would want.
If you decide to try L-carnitine, the advice to go low and go slow obviously applies. Consulting with your doctor is clearly a good idea.
Possible Synergies
Proposed synergies with other supplements include omega-3 fatty acids, choline and alpha-lipoic acid. Alpha-lipoic acid (ALA) is an antioxidant and neuroprotector. Animal studies suggest that acetyl-L-carnitine and ALA might work synergistically to improve cognition and mood but clinical trials have not tested this idea yet.
Dr. Teitelbaum reports that “taking 500 to 1,000 milligrams of L-lysine, which is cheaper, can decrease the amount of acetyl-L-carnitine you need to take by helping your body to make its own carnitine”. Vitamin C (200+ mgs/day) plus B-complex vitamins should also be taken.
Conclusion
Carnitine is needed for effective energy production. The role it might play in improving the energy levels of people with ME/CFS/FM is still unclear.
L-carnitine and acetylcarnitine present interesting possibilities. Both play key roles in energy production and/or fatigue and both have been studied in ME/CFS and fibromyalgia. The role L-carnitine and acetylcarnitine deficiencies play in either disease, however, is not clear as some studies have found low levels while others have not.
The Australian ME/CFS study was particularly intriguing as it found normal total carnitine levels but reduced levels of specific carnitines which appeared to impact fatigue levels. While most of the clinical trials have been rudimentary, the results, in general, have been favorable.
While both may be able to help with fatigue, L-carnitine has a leg up regarding energy production, while acetylcarnitine is being used more to improve cognition, mental clarity, improve mood and as a neuroprotector. Acetylcarnitine, in particular, is being studied in many diseases.
Two ME/CFS doctors recommended from 1-2000 mgs in divided doses a day. While one study found that using L-carnitine in hypothyroid patients improved their fatigue, several websites warn that using carnitine in high doses (2-4 grams/day) may be able to reduce thyroid production. Because L-carnitine is metabolized to TMAO – a marker associated with cardiovascular disease – concerns have been raised about that. Several studies, on the other hand, have found L-carnitine not to affect factors associated with aetherosclerosis and to reduce markers of oxidative stress and blood vessel injury.
More study is clearly needed. Plenty of studies suggest that something has happened to the mitochondria, but exactly what we don’t know. That means we’re shooting blind to some extent trying to use mitochondrial enhancers to affect the complex mitochondrial energy production.
Still, it’s intriguing to think what each might do as a part of a mitochondrial enhancing package. On that note, using these supplements in conjunction with omega-3 fatty acids, choline, lysine, Vitamin C and B, and/or alpha lipoic acid (ALA) may be helpful.
The Mitochondrial Enhancers for Chronic Fatigue Syndrome (ME/CFS), Fibromyalgia and long COVID Series
- Pt I: D-Ribose, CoQ10 and PQQ
- Pt II: L-carnitine and Acetylcarnitine
- Pt. III: Magnesium
- Pt IV: N-acetyl cysteine (NAC)
- Pt V: Oxaloacetate
- Pt. VI: Niacin, Niacinamide and Nicotinic Riboside






Years ago, when my fibromyalgia was bad, I tried acetylcarnitine and noticed no effects. Then I tried l-carnitine. My body was immediately energized, but it was way too activating. Not just insomnia, but I was buzzing around like a bee. I could not find a dose small enough to help that didn’t make me too wired (even after emptying 2/3 of a capsule). It felt like something I REALLY needed, but I could never take it. I am hypothyroid, on Synthroid (at the time), so maybe that was the problem.
I also tried acetyl-l carnitine and ended up with insomnia. It seemed as though my slow metabolism meant that it kicked in during the night. I went for 8 months with no more than 2-3 hours of sleep a night. I also developed terrible mood episodes when I did wake, probably from the lack of quality sleep. Once I stopped taking the supplement, my sleep patterns recovered to a more normal pattern- for me anyway. It does seem that either the strength or the time of day the supplement should be taken for people with ME/CFS should be explored.
Interesting here is the paper titled “Reductions in gut microbiota‑derived metabolite trimethylamine N‑oxide in the circulation may ameliorate myocardial infarction‑induced heart failure in rats, possibly by inhibiting interleukin‑8 secretion” by “Xiaoyan… …Jing Wang”
Interleukin-8 or IL-8 is a cytokine increasing mucosal barrier permeability (leaky gut, leaky brain…) and attrackting neutrophils to the site where more IL-8 is and come into action. Much of it might resemble (or even co-trigger) an MCAS attack I guess.
Would you be aware of how an MCAS attack feels? Did the response bare resemblance? It (or a similar quick immune activation) has IMO the potential to create a hyper, wired state.
Interesting observation. One of the first things I noticed since supplementing with ALCAR was a substantial decrease to my high neutrophil count.
Interesting news Christopher. I guess you had a blood count on neutrophils before and after taking alcar? And the numbers were remarkable enough to be likely related with the use of alcar?
Did it increase any gut sensitivities or immune related responses?
Thanks Cort. A very important series in my opinion!
I experienced something similar to Elaine and Cate. It happened not only with Carnitine but with other “Mito Enhancers” on Cort’s list, and I stopped experimenting with them completely for a couple years.
In the past year, however, I’ve made a potentially game-changing discovery. When I take them at low doses first thing in the morning, exclusively on days when I plan to try some physical exercise (about 2-3 times/week), not only can I exceed my normal energy envelope without significant PEM, but I also experience minimal side effects. It seems that the calming effect of exercise “balances out” the overstimulating effect of the mito supplements.
In combination with Pyridostigmine (Mestinon), hydration, hot-cold therapy and medical cannabis (high-CBD and full spectrum), this strategy has actually allowed me to rebuild muscle for the first time in years. It feels like the mito enhancers in particular help create a temporary physical pacing loophole, allowing me just enough exercise to get in better shape and experience the compounding benefits that come with it.
With that said, I’m fully aware that this strategy involves risk and obviously wouldn’t work for everyone. I still have to listen carefully to my body and take many precautions (e.g. limitations on type and duration of exercise, minimum 2-3 day recovery periods, etc.), and occasionally I still push too hard and get crash symptoms. I’m certainly not advocating that anyone abandon pacing in general.
(I’ve been working on a partial recovery story article about my experience. But I’m hesitant to share anything that might cause some ME/CFS sufferers to get worse, so I probably wont do anything with it.)
That is very interesting David.
Issie and I have sort of similar experiences, but you seem ahead of us. We seem to have benefit too by shifting “overstimulating” supplements either to the morning or more spread over the day rather then taking a single dose.
We both sure believe in going low and slow. Normal doses often are very aggressive and side effects often overwhelm good effects, but going with doses 10 times as low as what is labeled often gives us a notable boost in health with few side effects.
We lean towards thinking that overstimulating / mito enhancers also stimulate the immune system a whole lot. When that is already in uproar, that can fire back hard.
In the morning, the gut is most empty, digestion is mostly completed. It happens that digestion also is a rather inflammatory process. So when taking these “boosters” at the moment our immune system is more at rest and only taking minimal doses, we *might* get the benefit of having some more energy without driving our immune system in overdrive. Maybe a bit of that extra energy gets spend on repair and recovery?
I know it’s still not a rock solid idea. Your experiences would be rather valuable here. I see why you are hesitating so much. We try and be careful enough to not get people to do dangerous things too. How about considering changing the focus of your recovery story? Rather then “this helped me”, what about “could timing and reducing dose of supplements help us?”. The first approach may have some people dive in head first, the second invites people to try and get things safer and better.
Fascinating David!
I have never tried taking something before exertion although it certainly makes sense to try.
“at low doses first thing in the morning, exclusively on days when I plan to try some physical exercise (about 2-3 times/week), not only can I exceed my normal energy envelope without significant PEM, but I also experience minimal side effects.”
I like your regimen. 🙂
“In combination with Pyridostigmine (Mestinon), hydration, hot-cold therapy and medical cannabis (high-CBD and full spectrum)”
When do you take the high-CBD Cannabis? I find it great for sleep but haven’t tried it otherwise.
Thanks dejurgen and Cort!
Dejurgen, what you say about the empty gut and the immune system makes perfect sense of my experiences, not only with the mito enhancers but perhaps more recently with my trials of intermittent fasting (the 16/8 method a couple times per week). But that’s a whole other story.
Re: the medical cannabis, Cort, I have not had the same sleep benefits that others attest to, and that includes the high-THC indica-dominant strains that knock some people out.
For the purpose of exercise, I take high-CBD oil (20-40mg), mixed with a tiny bit of full spectrum oil, in the morning 1-2 hours before exercise, and then I usually vape a full spectrum dry herb (still more CBD than THC) in the late afternoon, when the oil has mostly worn off. The cannabis seems to do three things for me:
1) It significantly reduces the muscle pain and to a lesser extent the cognitive exhaustion associated with exercise recovery. For me it seems to function like a low-dose, side-effect-free NSAID. It makes me feel better than I would without it, although just like with NSAIDs, it doesn’t allow me to actually do more in the hours after exercising without PEM later on.
2) It seems to slightly speed up my recovery time (e.g. only two or three days rest instead of three or four). I’m not sure how it does this but I definitely notice a difference when I forget to take it.
3) As long as it doesn’t contain too much TCH, it also seems to slightly increase my concentration during exercise. I have no idea why it might do this. It may be partially related to the carrier oil rather than the CBD alone (a lot of CBD oils use MCT, which can temporarily improve mental energy).
With that said, I’m a Canadian with a medical prescription for licensed producers regulated by Health Canada. It’s very easy for me to find any cannabis strain configuration I can think of and know exactly what’s in it. It made experimentation and finding what works for me much easier than for others who don’t have legal access and cannot always rely on sketchy industry labels.
@David Graham
When I did an intermittent fasting like thing, I often had more resilience to exercise and brain work before eating in the morning. Often, but not always.
I think when I got in troublewhen trying to do something without eating first was when I got in trouble with too low blood sugar. I have genes that indicate poor blood sugar control.
That is why I left intermittent fasting for now: I try and spread out caloric intake and carb intake so that I will have as few as possible blood sugar swings.
I don’t mean to be rude, but 40mg of CBD is not high CBD oil. 1000mg is much closer.
My concern with carnitine is the side effect of possibly increasing TMAO levels which can promote atherosclerotic plaques and heart disease.
Seems we have the same concerns :-).
Thats the thing with supplements. They are very concentrated and with that concentration become more of a medicine. With any and every supplement, you need to know what it does, how it works, what its for. You also need to know ALLLLLLL the health history and how that can interact with each “symptom/illness/disease”. One supplement can help one thing and make another “illness” way worse. That has to be weighed out, between benefits vs. Side effects. And also not throwing off a system/function/balance because of something causing things to go too high or be too suppressive.
I’ve been in and around this “field” of alternative treatments, for a really long time. If I talk about something, I try to point out what it does for me…..as my body is different and it may not work the same for someone else. And I also try to point out any known side effects if you have.??????? Because not everything will be safe to take for everyone.
Functional doctors are good for this as they do testing to find out underlying issues and then treat accordingly. There is a plan and order to it too. You don’t treat everything, all at once. But there is a protocol and a method for the least amount of potential problems.
Thanks for pointing that out. I only came across that once but looking at the research literature there’s quite a bit on that. I just amended the blog. It’s a complex and not clearly resolved issue.
“While high TMAO levels have been associated with cardiovascular disease, the role it plays in producing heart disease is unclear as fish contain high levels of TMAO yet high fish diets have been shown to reduce the risk of heart disease. ”
That may be answered by the paper titled “Metabolic retroconversion of trimethylamine N-oxide and the gut microbiota” by “Lesley Hoyles… …Marc-Emmanuel Dumas” saying
“Conclusions: Reduction of TMAO by the gut microbiota (predominantly Enterobacteriaceae) to TMA followed by host uptake of TMA into the bloodstream from the intestine and its conversion back to TMAO by host hepatic enzymes is an example of metabolic retroconversion.”
In English: The gut isn’t good at taking TMAO up, but it’s precursor TMA. Depending on your gut microbiome, some of the dietary TMAO will be converted to TMA (that can be better absorbed by the gut).
Note: other gut microbes can convert carnitine, choline… to TMA. It is taken up as TMA by the gut and only inside our body converted to TMAO by the (human, body own) enzyme FMO3. That enzyme has it’s good uses too, so no need to try and suppress it.
Kamal Patel of Examine.com points out the many, many flaws in that study:
https://examine.com/articles/media-sensationalism:-meat-is-bad-for-your-heart/
My son, 37 has lived with CFS for 11 years now.
Severe lack of energy and getting very depressed and anxious.
Is being treated by a Psichiatrist at the moment with antidepressants etc.
I would like to talk to someone who is doing research on CFS
Can you recommend such a specialist or doctor?
We live in South Africa, Cape Town.
ATP (adenosine triphosphate) is available as a supplement. It has helped me. Any studies or recommendations for using ATP? I also use D-ribose, CoQ10, and other supplements.
“L-carnitine and acetylcarnitine are mostly described as side-effect free.”
Mostly may be important here.
Carnitine and acetylcholine are often low in ME/… patients. But the question in part is why? Part of that question could be answered by a paper titled ” Effects of dietary choline, betaine, and L-carnitine on the generation of trimethylamine-N-oxide in healthy mice” by “Zhu-Lin Yu… …Yu-Ming Wang”.
In the gut, some bacteria can convert all of those to TMA and in the body that converts to TMAO. It’s a component fairly strongly associated with arterial diseases. See for example the paper with title “Gut microbiota-derived trimethylamine-N-oxide: A bridge between dietary fatty acid and cardiovascular disease?” by “Mengxue He… …Yuanfa Liu”.
As our blood supply and arterial system isn’t likely optimal to say the least and many of us have a dysfunctional gut microbiome, it’s important to take that into consideration. There is the option that in *some* ME/FM/POTS/… patients our blood carnitine / choline / … levels are low because we have a dysfunctional gut microbiome converting most of our dietary intake to the nasty chemical TMA and that converting to TMAO in the body. That would leave us low carnitine / choline / … in the blood and high levels of TMAO being nefarious for our already prone arterial system…
So: as Cort says going low and slow and observing well any side effects (and progress over time or absence of it) might be key to determine if it is a good thing in your individual case.
I just added the TMAO issue to the blog. It’s a complex issue. Yes, L-carnitine does dramatically raise TMAO levels and yes high TMAO levels are associated with cardiovascular risk but it’s not clear that TMAO is causing them. L-carnitine is also used to improve heart health and several studies did not find that it enhances factors associated with atherosclerosis and in fact may reduce them.
One paper concluded: “In contrast, a number of studies demonstrate beneficial properties for l-carnitine consumption against metabolic diseases including skeletal muscle insulin resistance and ischemic heart disease. Furthermore, fish are a significant source of TMAO, but dietary fish consumption and fish oil supplementation may exhibit positive effects on cardiovascular health. ”
https://pubmed.ncbi.nlm.nih.gov/24267266/
I’m not saying they’re right. I don’t know – just raising another side of yet another complex issue…Our bodies seem to specialize in them.
The whole gut microbiota side presents another complication as you point out. If our gut microbiota is tuned to metabolizing carnitine to TMAO that might not be a good thing. On the other hand that might mean that altering our gut microbiome could be helpful. That, unfortunately, is not something we know how to do right now.
It is complex I agree. Carnitine has many good uses for the body, once it gets inside the blood stream.
I found a paper titled “Uptake of L-carnitine by a human intestinal epithelial cell line, Caco-2” by “E McCloud … …H M Said”
saying
“L-Carnitine uptake was also energy-dependent, being significantly (P < 0.01) inhibited by metabolic inhibitors."
So, having poor energy production in the gut leads to poor absorption of carnitine by the gut. That also leaves more to potential bad bacteria.
As we aren't high on energy production, ME patients who take carnitine might want to take it when they are in a rest and digest mode and away from heavy meals (costing plenty energy to digest).
Fecal Microbiota Transplantation.
I believe it is possible to alter ☝️ one’s gut microbiome.
If you get a FMT, make sure to adhere to a strict and disciplined regimen of prebiotic supplementation post procedure.
I have been supplementing with ALCAR + LCAR for years.
Great article Cort!
Most recent type of LCAR I am using is:
PROPIONYL L CARNITINE.
Give this LCAR a try one day. ?
I use atp fuel by researched nutritional. Works every time since I am losing atp every day according to my dr.
See the cell danger response by dr nuviax
I have cfs and 3MCC deficiency. Prior to my diagnosis of the latter condition, I went to a geneticist to see if they were doing any genetic studies on families with multiple members who have cfs and the like (fibro, POTs, etc.). They aren’t. I have multiple family members with those conditions. Anyways, that’s when they found the 3MCC deficiency. Some people with 3MCC have low levels of carnitine. Mine was slightly low. I’ve been taking a L-carnitine supplement 3 times a day (as prescribed), but haven’t noticed an improvement in my fatigue, even though my carnitine level is now in the normal range. Does anyone know of a cfs and associated family cluster genetic study going on currently, maybe in New England if they can’t/won’t do remote participation? It would be worth looking into.
Resveratrol can lower TMAO levels.
That’s interesting as it’s also on the mitochondrial energy enhancers list. Eating less red meat can too.
That can explain why a subgroup of CFS patiënts feel better when they drink red wine 🙂 Red wine also improves the intestinal flora, research shows. Resveratrol is an antioxidant and has anti-inflammatory, antiviral, antibacterial and nerve tissue protective effect 🙂 I would like this drug to be tested in a double-blind study on ME patients.
While it isn’t specifically aimed at familial issues, I’d imagine the DecodeMe study would be able to pick up some of these problems while they try to find out the genetic side of ME/CFS. If you haven’t come across this study yet, they will be analysing 20,000 ME/CFS patients! They are initially looking to source patients from the UK but are also keen for others around the world to sign up as part of their ‘Plan B’. The study has been delayed by covid, but they should start collecting samples in the autumn.
Acetyl l carnitine worked wonders for my CFS !!! My brain rallied unbelievably when I started it nearly 15 years ago . I know the power in this supplement !!
I took 1gm acetyl~carnitine / daily for many years, going back about 4 years ago. ( as advised by Sarah Myhill)
I had to stop it, as my urine and all body secretions began to smell VERY STRONGLY of trimethylamine
(Very Fishy !!)
Same with L ~carnitine.
It was UNBEARABLE.
Curiously I noticed that when I had a course of antibiotics ,,, the smell Disappeared !
It wouldn’t be curious that that smell disappeared while taking antibiotics. Part of the problem is gut bacteria converting too much carnitine to TMA. Antibitotics kill gut bacteria often very well.
The trouble is, taking antibiotics kills a wide variety of the gut bacteria very well, leaving it often in an unbalanced an prone state very long after it. It is not uncommon for the gut microbiome to become worse after stopping the antibiotics treatment then before it.
Note that the 1997 study mentioned where 12 out of 18 outcome
measures improved after 8 weeks, used a dosage of 3000 milligrams of
L-carnitine per day
I also bought a infrared light from radlites. It heals the mitochondria. It takes time. But it does get rid of any pain in about15 minutes.
It is very soothing and comforting as it does warm. Up. I use it when ever I have muscle pain and my dr suggested it to me. I could not survive without it. Look up infrared light treatment for pain and for CFS and Fibromyalgia. Less pain means more energy
You can get one from the living store .com. For 100 dollars and it is a four wave
Light which does the best job of healing up the mitochondria. Am I allowed to give the websites??
Red light therapy (infrared and far infrared types combined) helps the body do its work easier, and we do not have to figure all the supplement complexities. The body already knows most of what to do with healing if it is given the right bioterrain. The Mitomobile and other larger lights from this US company are wonderful.
It is true that with ten minutes of this light on the painful lower back area, the pain disappeared. Creates ATP too. Light/sound/frequency/magnetism are interrelated and are the medicine of the future, along with a physically and energetically detoxed environment.
Would supplementing with l-lysine, as suggested in the article, avoid the complications of supplementing directly with a form of carnitine, as discussed in the comments?
Interesting! I take acetyl-l-carnitine in the morning if I know I’m going to have a big day and want an extra buzzy boost. But if I take it more than once a week I get insomnia and that horrible over-tired, crashing feeling like it’s just too much stimulation. I wonder if taking plain l-carnitine would have the same effect?
L-Carnitine Tartrate seems to be the most common form of L-Carnitine available, not an entirely different product, so even it the label just says “L-Carnitine”, check the ingredient label as it might be L-Carnitine tartrate.