After attempting to explain the cardiovascular issues in ME/CFS, Klaus Wirth and Carmen Scheibenbogen take on the energy and muscle issues. Warning – this is complex!
Klaus Wirth and Carmen Scheibenbogen brought the chronic fatigue syndrome (ME/CFS) world something entirely new in 2020 with their hypothesis paper, “A Unifying Hypothesis of the Pathophysiology of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Recognitions from the finding of autoantibodies against ß2-adrenergic receptors”.
The hypothesis was notable in its ability to potentially explain different features of ME/CFS.
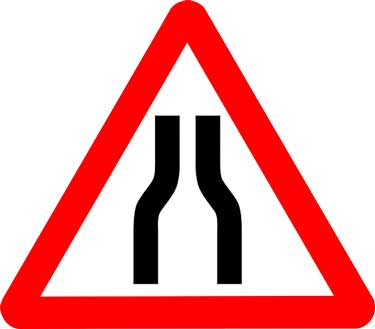
W&S believe narrowed blood vessels trigger the production of vasodilators, which causes symptoms.
They proposed that two factors – sympathetic nervous system hyperactivity and ß2AdR receptor problems – are knocking the blood vessels of people with ME/CFS for a loop. As sympathetic nervous system hyperactivity is giving them a good squeeze, the ß2AdR receptors which are supposed to open them up are getting hammered by the immune system.
That leaves the blood vessels unable to deliver the proper amounts of blood to the muscles, brain, organs, etc. The body, of course, can’t have that and so it attempts to fix the situation by releasing vasodilators like bradykinin and prostaglandins.
The authors believe these vasodilators spill over into the bloodstream where they, alas, produce fatigue, pain, and flu-like symptoms as well as headaches, gut pain, cognitive and sleep problems.
The Paradox Explained?
Enter the kallikrein-kinin-system (KKS) which produces bradykinin – and which opposes the RAAS system.
It turns out that higher sodium levels in the kidney and those same beta-adrenergic receptors highlighted in ME/CFS play critical roles in increasing renin production. By inhibiting sodium reabsorption into the kidney, bradykinin reduces sodium levels – thus inhibiting RAA activity.
The authors believe the message to trigger increased blood volumes has been “annihilated” in ME/CFS.
With the B2AdR receptors also knocked out, people with ME/CFS are missing two of the three major factors needed to stimulate renin production when their blood volume falls. Using rather colorful language, the authors assert that signal to increase blood volume is “annhilate(d)” in ME/CFS – thus potentially explaining, for the first time that I know of, the RAA paradox.
Having low blood volume turns out to be a big deal, indeed, as low blood volume, by itself, activates the sympathetic nervous system, which then squeezes the blood vessels, triggering vasodilator release and many of the symptoms found in ME/CFS.
Reduced Preload Explained?
The authors believe that increased bradykinin levels may also be causing the preload problems found by David Systrom. Reduced preload refers to lower than normal volumes of the blood being transferred to the heart – thus reducing cardiac output.
Systrom has found that the veins of a major subset of ME/CFS patients appear to be leaking. Because bradykinin increases blood vessel permeability, W&S believe high bradykinin levels may be causing the veins to leak blood into the “interstitial spaces”, thus ultimately reducing cardiac output.
(Systrom’s invasive exercise tests show that something reduces blood volume after the blood leaves the muscles and flows into the veins and back up to the heart. The “interstitial spaces” refer to the spaces found between the cells found just outside the blood vessels.)
The hypothesis could also possibly explain other findings such as the small hearts found, the chronotropic incompetence.
Their first hypothesis paper, then, with its potential to possibly explain symptoms ranging from the pain and fatigue experienced after exercise to the reduced preload found by System, and the RAAS paradox was quite a dynamo.
Round II: Explaining the Energy and Muscle Problems
“… high intracellular sodium levels are “the main cause for the exercise intolerance” in ME/CFS. The authors
The authors weren’t done yet, though. Their second hypothesis paper, “Pathophysiology of skeletal muscle disturbances in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)“, took on the energy and muscle problems in ME/CFS.
As anyone who’s watched shows outlining catastrophic failure like airplane crashes, nuclear plant meltdowns, space shuttle explosions, bridge collapses, etc., it’s not one thing that goes wrong – it’s usually a number of things operating in conjunction that causes complex systems to fail – and so W&S propose it is with ME/CFS.
In the first hypothesis paper, the authors proposed that vasodilators (bradykinin, prostaglandins), produced in response to narrowed blood vessels, are causing many of the symptoms of ME/CFS.
That sets up the idea that low blood flows could be causing an ischemia-reperfusion injury in ME/CFS. Ischemia-reperfusion injuries occur when during hypoxic situations where tissue is first deprived of blood and then reperfused with it. Ironically, the injury quickly occurs when the blood is reintroduced back into what’s become a hotbed of oxidative stress.
The authors don’t believe this kind of rapid and devastating situation occurs in ME/CFS but propose that something like it is occurring on a much larger timeframe.
“Major Failure Point”
The energy problems, they believe, probably start, though, with high sodium levels in the cell. Sodium enters the cell through something called the sodium-proton exchanger subtype1 (NHE1), which does just as its name suggests – as it brings in sodium ions it removes protons from the cell.
The anaerobic energy situation found in ME/CFS produces high levels of protons. As NHE1, in its attempt to deacidify the cell, removes more and more protons, the sodium ions can start to build up.
The authors point to four ways NHE1 activity could be increased in ME/CFS and state that they “strongly assume“, and that it would be “really surprising” if NHE1 activity was not increased in ME/CFS.

The authors believe that high intracellular sodium levels are the major failure point in the energy production system in ME/CFS.
Something called the Na+/K+-ATPase enzyme should be removing those sodium ions from the cell but, because a molecule of ATP is burned up every time Na+/K+-ATPase pushes sodium out of the cell, removing sodium is an energy-intensive process that likely hits a roadblock in ME/CFS – allowing the sodium ions to build up.
Plus, in a rather remarkable coincidence, those balky beta-adrenergic receptors (B2AdR) featured in W&S’s first hypothesis also stimulate Na+/K+-ATPase to remove sodium from the cell. If, as suspected, they’re not functioning properly, they may not be telling Na+/K+-ATPase to remove sodium from the cells. W&S write that they “strongly assume” that “the function of the Na+/K+-ATPase enzyme is severely disturbed in ME/CFS”. Wirth and Scheibenbogen, then, have identified two factors that might be interfering with sodium removal from the cell in ME/CFS.
Because ß2AdR also stimulates the Na+/K+-ATPase in the skeletal muscles, altered ß2AdR functioning could also affect muscle fatigability.)
Messed up ß2AdR receptors, low ATP production, and high levels of oxidative stress, as well as insulin resistance and lowered cGRP production may all play a role in the energy problems found in ME/CFS, but the authors believe the major failure point, energetically, is the inability of the Na+/K+ATPase enzyme to get the excess sodium out of the cell. They write the high intracellular sodium levels are “the main cause for the exercise intolerance” in ME/CFS.
Metabolic acidosis – the buildup of protons resulting from an overreliance on anaerobic functioning – has been tossed around as a possible cause of the exercise intolerance in ME/CFS, but W&S don’t believe it can explain PEM. Nor do they believe that low ATP levels are the major problem. Instead, they believe the metabolic acidosis and ATP problems found are pointing to the real problem in this disease: cellular sodium overload.
At high sodium levels, NCX changes course and starts importing calcium into the cell – causing PEM, exercise intolerance, etc. (Image-by-OpenIcons-from-Pixabay)
Please note that the high sodium diets that many people with ME/CFS/POTS are on to combat low blood volumes do not affect this problem in the slightest.
W&S believe those high sodium levels set the stage for the disaster that is ME/CFS because, at high sodium levels, the sodium-calcium exchanger (NCX) does something rather strange: instead of removing calcium as it usually does, it begins to import it into the cell.
It’s the high calcium levels that then whack mitochondrial functioning, mess up blood vessel functioning, and cause insulin resistance in the muscles. The sodium buildup problem, though, comes first.
Nanoneedle Connections?
The NHEI issue led them to the nanoneedle testing done in ME/CFS by Rahim Esfandyarpour and Ron Davis at Stanford. They found that plunking ME/CFS and healthy peoples’ cells into a salt solution dramatically altered the conductance of the ME/CFS patients’ cells compared to the healthy controls’ cells.
The Gist
- Wirth and Scheibenbogen’s 2020 hypothesis paper proposed that vasodilators – created in response to narrowed blood vessels – were leaking into the bloodstream of people with ME/CFS and causing fatigue, pain, etc.
- They believed that poorly functioning receptors (ß2AdR) that are supposed to dilate the blood vessels, plus sympathetic nervous system hyperactivity that was squeezing the blood vessels down was preventing normal amounts of blood from getting through to the muscles, brain, etc.
- The authors also explained why they believed the renin-aldosterone-paradox and the reduced preload found in ME/CFS was occurring.
- In their second hypothesis paper, the two German researchers propose that high intracellular sodium levels constitute the major failure point with regard to energy production in ME/CFS.
- The process starts off with proton buildup due to high levels of anaerobic functioning. In order to deacidify the cell (and pump the protons out), the sodium-proton exchanger (NHEI) brings more and more sodium into the cell.
- It turns out that it takes quite a bit of energy, though, for the Na+/K+-ATPase to remove sodium from a cell – energy that the cells in people with ME/CFS may not have. Plus, the balky receptors (B2AdR) that played a major role in their first hypothesis just happen also to play a major role in stimulating the sodium transporter to get sodium out of the cell. These two factors may be making it difficult for people with ME/CFS to remove from their cells.
- When intracellular sodium levels get too high, the calcium transporter (NCX) stops removing calcium from the cell, and begins adding calcium to it. It’s the calcium buildup that then interferes with energy production, blood vessel functioning, etc. The initial sodium buildup, however, is the spark that ignites that fire.
- The authors also suggest that the high NHE1 activity they believe must be present in ME/CFS could explain the nanoneedle findings.
- They also propose that high intracellular sodium levels could be putting people who exert themselves physically at risk for ME/CFS. This could explain how some people who did not experience an infection became ill.
- Once the process they outlined starts, they believe it takes little exertion to maintain it.
- The hypothesis also predicts that intracellular potassium levels will be low.
- The high sodium diets that many people are on have nothing to do with intracellular sodium levels.
- Klaus Wirth – a former pharmaceutical company researcher – reported that drug strategies can be derived from the hypothesis, and they are working on elaborating them.
- A third hypothesis paper explaining the neurological symptoms in ME/CFS is underway.
Altered sodium and calcium levels aren’t the only potential problems caused by reduced Na+/K+ATPase activity. Because Na+/K+ATPase takes up two potassium ions every time it emits three sodium ions, low potassium levels in the muscles, and possibly the blood (at rest), could result as well. They noted that several studies as well their unpublished work suggest this is so in ME/CFS.
Besides the infection triggers, the authors propose that overexertion may also be able to trigger ME/CFS in people with high intracellular sodium levels by reducing blood volume, increasing sympathetic nervous system activity, and mitochondrial problems in the muscles. Anyone with higher intracellular sodium levels may be susceptible to coming down with ME/CFS.
The crucial factor seems to be intracellular sodium levels high enough that they trigger a reverse flow of calcium into the cell. That reverse calcium flow then causes the energetic and blood vessel problems in ME/CFS. The higher the intracellular sodium levels, the worse the PEM (post-exertional malaise) that shows up.
The authors also noted that the compensatory changes that occur when someone has a severe case of orthostatic intolerance (OI) may be able to initiate ME/CFS.
Altered sodium and calcium levels aren’t the only potential problems caused by reduced Na+/K+ATPase activity. Because Na+/K+ATPase takes up two potassium ions every time it emits three sodium ions, low potassium levels in the muscles and possibly the blood (at rest) could result from impaired Na+/K+ATPase. The authors noted that several studies as well their unpublished work suggests this is so in ME/CFS.
The authors also propose that overexertion by itself may be able to trigger ME/CFS in people with high intracellular sodium levels by reducing their blood volume, increasing their sympathetic nervous system activity, and causing mitochondrial problems in the muscles.
Again, the crucial factor seems to be having intracellular sodium levels high enough to trigger the sodium-calcium exchanger (NCX) to reverse flows of calcium into the cell. It’s at that point that they believe post-exertional malaise and exercise intolerance occur. Problems with the endothelial cells lining the blood vessels also occur. The higher the intracellular sodium levels, the worse the PEM and exercise problems that show up.
Once this sodium-calcium-induced skeletal muscle pathophysiology (in particular the high NHEI activity) is established, they believe it takes very little exertion to trigger it. Everyday tasks could certainly do that.
Interview
I asked Klaus Wirth about the high sodium diets many people are on. He replied that “intracellular sodium is totally unrelated to sodium intake”. (No one should change their sodium intake as a result of this hypothesis.)
I also asked about ways to validate the hypothesis. Wirth replied that “Such complex disease hypotheses are usually not proven or disproven by single findings”, and that he thinks that “the final answer would come from the efficacy or inefficacy of drugs that are derived from the disease hypothesis. Effective drug principles derived from the disease hypothesis would prove the hypothesis.”
He did note that because the Na+/K+ATPase exchanges sodium for potassium, the hypothesis predicts intracellular potassium levels should be low. In principle, this strongly points to insufficient ATPase activity.
In fact, if he reported that “if the ATPase does not work properly as strongly suggested by the low intracellular potassium intracellular sodium must rise! By the way, low intracellular potassium has depolarizing effects to cause muscle cramps”.

Wirth, who spent much of his career at a pharmaceutical company, believes the hypothesis has treatment implications.
When I asked Wirth, who spent much of his career at a pharmaceutical company, about the treatment implications of the hypothesis, he reported that “potential pharmacological strategies can be derived from the hypothesis, and that they’re making an attempt to elaborate potential therapeutic strategies”.
Aside from that, Wirth and Scheibenbogen are working on a third hypothesis paper they believe could explain the neurological problems in ME/CFS.
Conclusion
Time will tell if Wirth and Scheibenbogen are correct or not, but the creativity and novelty of their hypothesis stands out. They’ve created a plausible hypothesis featuring factors (bradykinin, sodium-proton exchanger subtype1 (NHE1), Na+/K+-ATPase enzyme, sodium-calcium exchanger (NCX), and high intracellular sodium/calcium) that are new, so far as I can tell, to the MECFS field. They have one more hypothesis paper to go.
To some extent, ME/CFS (and long COVID) are numbers games: the more people we get looking at them, the more ideas will emerge and the better chance we have of solving them. Klaus Wirth is a living demonstration of the fact that every time someone shares an ME/CFS theory, the possibility is created that someone, somewhere will think “well, that is interesting …” and dig into it.
Wirth is just one of several professionals who have produced stimulating hypotheses after bumping into ME/CFS in different ways. Wirth’s interest was sparked by a German TV show. Robert Phair (of the Metabolic Hypothesis) read a Stanford magazine feature. Gerard Peirara of Cortene bumped into someone at a party.






You know… Ray Peat has written about the effects of high intracellular sodium… and calcium… and the loss of potassium and the inability of the body to hold on to magnesium when ATP moves outside the cell.
And inhibition of PDH and lactate
And nitric oxide
And tryptophan
And hormones and thyroid and cortisol
and histamine
and the adrenergic and cholinergic systems adapting for the lack of thyroid function
and the stress response
and and and
Issues and substances that have been observed in ME/CFS and FMS.
What’s more, he has an understanding of how all the systems interact
and general principles of degeneration (and regeneration)
– – – – – – – – – – – –
This business of the body attacking itself in autoimmunity…
– what if it were not?
The body ‘mistakingly’ attack itself…
– that made such little sense to me, early on.
Before the current model of immunity took hold,
there was another one that proposed:
that what this system does is detect tissue damage
not pathogens in themselves.
That means that *any* tissue damage can elicit autoantibody response.
and the antibodies are coming in to help heal the tissues.
Think about this:
when antibodies are measured in someone and found elevated –
is there any proof that they came first, and they caused the disease?
did doctors/scientist jump to this conclusion without the science to prove it?
how can we know if they had not been measured all along,
with all the other markers when the person was suspected to not be sick?
– – – – – – – – – – – – – – – – – – – – – – – – –
I think the ‘mistake’ that is often made – and I fell into this pattern too –
is that once we find something that is not in the normal range,
we assume that that is directly responsible for the problem, a knee-jerk reaction.
We do not stop to consider that it may be a consequence of the problem
and not even contributing
or it may even be a protective measure elicited
Or it may be responsible but indirectly, in a totally different manner from what we assume.
For example, think about Celiac disease –
for x reason that person cannot handle wheat
it causes irritation to the intestines and then come in the antibodies to help repair.
After a few months of not eating wheat, of not having the persistent constant irritation, the tissue heals, the antibodies go down.
This is another way of reframing all your autoimmune diseases:
what is it that is damaging the affected tissue, which process?
And remember autoimmunity is tied to tryptophan metabolism.
Estrogen and B6 have a strong effect in modulating it – which maybe gives us a clue why autoimmunity is higher in women. And a place to investigate in the men that have it (hint, their hormones).
B3, serotonin and neurotoxic substances like quinolic acid are also implicated (negatively)
– – – – – – – – – – – – – – – –
Just recently, I have been reading up on a different role of eosinophils – tissue rebuilding. The specific article was on muscle regeneration. I know that it is high in myalgia eosinophilia – a disease caused by very high levels of tryptophan (intake?) damage to muscles and high eosinophilia – may it be that they are coming in to repair the muscle? And why would tryptophan cause myalgia? and how may this relate to our tryptophan and muscle problems?
I diverge, the point was that the thought has been that high eosinophil count is ‘bad’ and must be brought down with immunosuppressants (are those fun for anyone??) – but what if they actually are helping repair?
– – – – – – – – – – – – – – –
I ask ME/CFS doctors and researchers to starting pulling together all these different findings, and recognize that the dysfunction doesn’t just fall on the particular area of hyper specialization of the researcher. And how do the systems interact. And that maybe some base assumptions on how the body works are faulty. Maybe all these paradoxes get resolved once you view how the body is organizing itself from a different perspective.
I read of a mathematician that recently solved a decade’s old mathematic conundrum that no one had been able to resolve. And it’s not even her area of study! She did like over breakfast while having coffee. She saw that they had missed something in formulating the problem, and that changed everything.
There is also a rich history of scientists whom have covered this land already, decades ago – almost a hundred years with some.
I didn’t know actually. I’m glad to hear of someone has looked at this. I imagine that others have as well.
I’ve heard that about autoantibodies: the more inflammation – the more tissue damage – the more opportunity for the body to mistakenly react to that.
Ray Peat is a nice man, but an almost complete nut-job. He believes essential fatty acids aren’t essential. Thinks starch and 90% of vegetables and fruits are toxic (because they have, gasp, fiber!), and believes Mexican coca-colas and assorted hormones are the answer.
The reality is Peat suffers not only from Cherry-Picking Syndrome, but seriously, from severe allergies to common foods, so he’s the last person to recommend for any health-related information.
Have you ever tried any of his recommendations
or to use the framework to view your health problem through
and start doing things to help, take notice of the effect, tinker, etc?
They are so lo-fi too, mostly all through nutrition.
So for example, in the other model of autoimmunity: our bodies are having difficulty with their energy process (thyroid)
the adrenergic system kicks in to make up for it.
the longer this goes on, the more detrimental substances and processes that are activated by it start affecting other systems and the normal energetic process further deteriorates, you need even more stimulation from these hormones and that is what is causing the damage to the receptors (in Carmen Schoenbongen’s research)
Restore the ‘normal’ energetic process
(no small feat!)
reduce the need for the adrenergic and cholinergic systems to kick in 24/7
and the receptors will heal.
A thought
[ this is very, very simplified ]
Good piece
I do get an awful lot of twitches in downspells in my muscles. Doc thought it was motor neuron at start.
Can be offset with lots of potassium (bananas) and it fades away.
Just one thing I noticed from a zillion other complaints.
Also find that my muscle twitching subsides with a high potassium intake. I had a toxic metals test once that had a statement at the bottom saying calcium in ion channels. I haven’t found any answers to this or what it means since but this article goes some way to explaining.
Some POTS people found Lorsartin to be a benefit. It actually increases potassium. (It did NOT work for me. And increasing potassium was not a help either for me. Different subset types.)
” a zillion other complaints ” LOL SO RELATABLE!
1. Its nobody with Cfs that dosnt have Thoracic outlet syndrom.
2. Intracranial hypertension is affected by Thoracic outlet syndrom and is seperatly know as the cause of fatique.
3. When radiologist isnt checking Interna jugula vena, and only have the doctors small note to work by they can never get 2+2 to be 4.
Quite a lot of people with an initial ME/CFS diagnosis have since been diagnosed with hypokalemic periodic paralysis. The genetic form is one option. Inflammatory diseases that mess with the kidneys can also make K drop randomly.
Agree, but for some reason, it takes potassium and magnesium supplements to calm mine down. Already eating bananas.
I have to take Rx potassium or I get really sick.
Many thanks to Wirth and Scheibenbogen! They seem to advance the field by not only building puzzle pieces but also connecting them with each other. I have a feeling we will hear more of them and so to our benefit. Thanks again! And thanks Cort for doing such great job simplifying this hard science.
Also find that my muscle twitching subsides with a high potassium intake. I had a toxic metals test once that had a statement at the bottom saying calcium in ion channels. I haven’t found any answers to this or what it means since but this article goes some way to explaining.
I am now seeing countless people now with diagnoses of ME/CFS Fibro Lyme even hypermobility with a genetic metabolic illness that can run in families from one or both parents, some can be carriers…There are 4 types of acute neuro forms, one is
so rare only 7 to 10 people have been diagnosed with this condition type, there are 8 types involved but as mentioned 4 types are Neuro kinds. The ADP type is the rare one so one can exclude this. The other 3 types 2 are connected to skin & Sun & light
issues the last one is the most serious type…The 2 Sun allergy ones can be found in stool tests found also in stool The 2 Sun/skin ones are (VP) Variegate Porphyria, the other is (CP) Coproporphyria all these 4 are Acute
Hepatic Neuro types. The other one is called (AIP) Acute Intermittent Porphyria. I have also heard that the defect of chromosome 12 is the same in Acute Intermittent Porphyria & the same in hypermobility. One Woman went to a VA Dermatologist told before she had also CFS Fibro & all the labels she has now been diagnosed with the (VP) Variegate type. I think it was found in the urine sample. I only thus far had the stool sample done I was negative to VP & CP…There is a Group on Facebook it is called ‘porphyria sucks’ & not always the urine has to
change colors & Tachycardia like syncope is a major symptom of the attacks so are abdominal pains even IBS labels have been given…Some can become psychotic or even manic or skitso but not all will have this…I am now waiting to see if I can be tested for AIP
Cort i hope you can make a video call with professor Scheibenbogen for an interview 🙂
Me too. Great idea 🙂
That would be wonderful, please ask for a video on this. Thanks
Yes, that would be very interesting.
Just a question. Would this affect the blood sodium tests on a CBP from your physician? I have a very odd situation in which no matter what I try my blood sodium levels are always low. I eat loads of sodium, stay hydrated without over hydrating, and tried to cut back on my sertriline to no avail as it can sometimes cause low blood sodium. Counter intuitive to that I actually have very high blood pressure although I’m quite thin. I have symptoms in every part of my body in every system as described above and many more. So therefore I’m curious if on the CBP results ME/CFS people are getting, are any of them like me with low NA and low CL ( hyponotremia ) without having issue in the kidneys , liver , etc, and have tried to increase by diet and electrolytes to no avail ? Would this result then not fit in the hypothesis above ?
I don’t know the chemistry but I suspect, given what Klaus Wirth said about the influence of diet on intracellular sodium levels, that blood sodium don’t have anything with this process.
What an interesting situation you are in though. Have you tried trioral oral rehydration solution?
https://www.healthrising.org/blog/2020/09/15/saline-ors-oral-rehydration-pots-chronic-fatigue-syndrome/
Interestingly enough the last CBP that was done in May showed I now have a borderline high glucose level of 108. I eat super healthy. I did eat carbs in the form of gluten free multi grain crackers and breads but now have had to change my diet to a low glycemic one due to THAT ! So therefore I am using and oral hydration powder sweetened with Stevia. If allowed below is the link to what I’m using from Amazon. I add this to my alkalized water and drink that through the day as it’s here by my bedside where as so many on here well know I suffer a multitude of disabling symptoms and mostly “live here”. I try to move throughout the day as I have a lot of issues with my vascular system as well but also get easily short of breath if I “overexert” by doing laundry even! I used to be a committed gym rat and avid hiker so I have to fight the disappointment in not being able to use my body in such a physical manner as I did all most of my life. This is a very interesting theory given how much they spoke about the vascular system as well ! Thanks Cort! Here it the link to the hydration powder I am using that is low glycemic; https://www.amazon.com/Enhanced-Electrolyte-Powder-Peach-B-Vitamins/dp/B0887TCVBY/ref=pd_yo_rr_rp_8/142-6151258-1655065?_encoding=UTF8&pd_rd_i=B0887TCVBY&pd_rd_r=f6da3a99-857a-4a22-b6cc-c9de19937021&pd_rd_w=GNzVR&pd_rd_wg=f0rgf&pf_rd_p=182844a1-e6d2-4ba5-a947-2cf78eae55fe&pf_rd_r=77T7T6GR190RB0W2JGS4&psc=1&refRID=77T7T6GR190RB0W2JGS4
I wouldn’t say that yet:
The Na+/K+ATPase pumps require plenty of energy (ATP) and we lack that. We seem to lack it in a time (and exertion) dependent manner. So at times we likely will lack ATP somewhat, at other times (like after exertion) badly.
The same goes with the sodium-proton exchanger subtype1 (NHE1) proton the researchers suspect to be involved in (restoring balance during) anaerobic energy production:
“The anaerobic energy situation found in ME/CFS produces high levels of protons.”
As we patients experience, it seems that the amount and excess of anaerobic energy production in us is time and exertion dependent too.
If we combine the above, the bodies ability to restore good intracellular sodium levels gets likely whacked in a time dependent fashion. If so, at times the intracellular sodium levels should be fine-ish. At other times like after exertion, they should be highly elevated.
=> So, where did all the sodium come from that gets transfered to the inside of cells after exertion? The remainder of body fluids?!
=> If so, either before the exertion the sodium levels inside our body fluids (blood and…?) were increased or after it they will be depleted. I suspect it to be a mix of both: at rest somewhat increased blood sodium levels, after exertion somewhat reduced ones. That extra sodium inside the cells has to come from somewhere doesn’t it?
I don’t believe they think that the intracellular sodium levels are ever normal or “fine-ish” once you are in ME/CFS. The system, they believe, gets set, and once it gets set even small amounts of exertion can trigger the calcium inflows into the cell. There surely must be a gradient though – from somewhat fine-ish to disastrous…
I don’t know where the sodium comes from. Wirth did not seem to connect this process with blood sodium levels but they must come from somewhere. If they change after exercise – would that be an indirect test of the hypothesis? Interesting idea 🙂
FYI Stevia is a vasodilator. It makes me feel Terrible.
If Stevia makes you feel bad, also look at other possibilities. It is being used to kill Lyme and other pathogens. Could there be a herx reaction happening? (I have issues with it too, but its not because of vasodilation. )
In the back of my mind, it could affect hormones too. (Time for me to stop commenting today… getting a brain fog moment coming….. LOL…..I can feel it coming.)
Mary,
You and I sound very much alike in that I have high blood pressure and borderline glucose (mostly just fasting blood sugar – usually not high after eating).
I have been taking the Trioral rehydration salts for the past 5 months. The WHO has found that rehydration salts must contain glucose in order to work. I put a packet of Tru lemon to make it taste better. Unfortunately, it does raise my systolic blood pressure by 10 points but my doctor feels that it is manageable.
Here is what I have noticed from this treatment:
I can stand at the kitchen counter to make dinner. That was amazing to me. My heart rate does not race just from standing. In fact I started playing ping pong for about 15 mins without ill effect.
I decided that maybe light exercise (think 55+ YMCA program) was now in my future, but unfortunately, the PEM still came even though my heart rate was much lower during the exercise than before the salts.
So now I am off of it for a week and will start back next week and leave off the exercise. 🙁
But overall, the rehydration drink has improved the quality of my life.
Issie — Stevia messes up the microbiome. That’s the problem…
@kelly, for me that seems true. It does seem to disrupt proper microbiome, it does affect my digestion for sure. I used it years ago when trying to eliminate Lyme, but my digestion got worse. Thanks for the input.
Exactly
Always low sodium like you
I drink salt in water and take licorice tea that helps keep sodium in but raises BP
The only other out of range test I hv is low lymph’s .6 ace when ought to be 1-4
This is the sign of having a chronic viral illness but I don’t hv any symptoms of virus?
Low body temp is another constant fwiw
Low body temp is so common for CFS. I have always wondered if that’s caused by pathogens “adjusting” the thermostat to their comfort zone. Have you also noticed that even when you know you are sick – flu or sinus infection, for example – you don’t develop a fever?
@Kate, I have written about this before. Pathogens do better in a cooler environment and don’t like heat. Thats why many get relief from Lyme disease when they use infrared saunas. It helps kill them. (But can cause die off and a herx.) But I do know a guy who did the opposite, at a clinic, and used hyperthermia to kill his Lyme. I guess that was an extreme, with doctor assisted monitoring. He says it worked for he and his wife, along with a long list of other things they had to do. I have also been told I need to get my body temperature up, as its very low. I Need it higher to fight lots of things. And with a wonky immune system, that would be helpful. Mine doesn’t appear to be thyroid related either.
I also have a low body temp. I can stand in a tornado of mosquitos and not get one bite.
I, on the other hand, tend to run a slighty raised temperature, and when stressed, a light fever.
My stress hormones kicking in?
So that those with lower temperatures, the body is adapting by hibernating?
Higher temperatures revving up (hypermetabolic)?
Maybe for some reason the body can’t mount enough adrenaline/noradrenaline in the low temps?
Opposite in the high ones?
This is the first article where I have seen something I have long felt was a connection to CFS/ME—sodium management in the cells. Since having mononucleosis decades ago, my body seemed to have a series of sodium-related water-retention issues. Mid-twenties began excessive night sweats (changing 7-8 shirts per night, drenching towels, etc.) An endocrinologist suggested it was disautonomia but no solutions were offered so I watched my sodium and noticed worse symptoms with higher sodium intake. (I am wary of scientists like the one in this article who are “certain” dietary intake has no effect). My body has been my experimental laboratory and since CFS/ME became severe at age 65 in 2019 after a Shingrix vaccine, with flare-ups after 2020-2021 flu and Covid vaccines—I’ve noticed that now ANY sodium in my diet causes me to become short of breath, lightheaded and with POTS-like symptoms and PEM. Now, with a low-sodium diet of just plain fruits, vegetables, nuts and seeds, and monitoring my heart rate with walking, I’ve been able to regain about 80% of my physical functioning after the next vaccines (flu and Covid) that exacerbated CFS symptoms last fall. It only takes a small amount of dietary sodium like 120 mg more that usual in a day from a plain chicken leg (I do get cravings for meat at times) to have me dizzy and short of breath. The other issue that I believe is connected to my body’s inability to handle sodium comes during summers here in Florida while walking outdoors. It’s a delicate balance, and I do not believe it was mono alone that created this problem, but genetics, too. All 3 of my sisters and my mother had mono and all of us have to be cautious with sodium, all are very thin, some with high blood pressure, but I’m the only one with CFS and such extreme sodium intolerance that I now have hyponatremia, most likely due to avoidance of sodium. Still, the article was striking to me in picking up on something no doctor has been able to uncover with standard blood tests. My cardiologist knows I have arrhythmia with the mildest of exercises, and just referred me to a pulmonologist after detecting pulmonary hypertension, which I suspect is caused by the narrowing of arteries described in the article since that is one possible cause. As with the multitude of symptoms stemming from CFS, and most doctors’ lack of knowledge about the cellular processes, I’m not expecting any great revelations from today’s pulmonary exam. For that reason, I do SO appreciate Cort’s blog giving us insights into what most doctors know nothing about.
hi, you wrote: When I asked Wirth, who spent much of his career at a pharmaceutical company, about the treatment implications of the hypothesis, he reported that “potential pharmacological strategies can be derived from the hypothesis, and that they’re making an attempt to elaborate potential therapeutic strategies”.
i speak normally dutsh so do not understand it well. Are there now therapeutic company’s working on this treatments or what does it mean? thanks!!!
Good question. You have to take this in context. Klaus Wirth spent his career in the pharmaceutical field. When he says (in good pharmaceutical speak :)) “potential pharmacological strategies can be derived from the hypothesis” – that means that yes, he sees ways to either find drugs or create drugs that will help fix the problem he and Dr. Scheibenbogen have identified.
With this “they’re making an attempt to elaborate potential therapeutic strategies” the question is what does elaborate mean? My guess is that it means that they’re working on ways to create real and effective therapeutic strategies which they hope will win over drug companies.
thank you so much cort for excplaining! it gives me hope!!!
Konijn: nee, nog geen medicijnen ‘potential’: potentiële strategieën voor medicijnen en Wirth en Scheibenbogen doen een poging om potentiële strategieën uit te werken (voor de farmaceutische bedrijven) Zo begrijp ik het. Maria.
bedankt Maria, ik had van cort wel begrepen dat er nu nog geen medicijnen waren. maar je maakt het nog duidelijker, ben heel ziek dus kop plu. hoop dat wat is het in europa ? euromene of zoiets of horizon 2000 en opvolger financiëel beter tussen komt dan NIH voor nancy klimas etc. and when i was still a bit better, not so long ago, i mailed cortene and the answer was, we are stuck with no money. I really hope europe puts money in it , much money, that it moves verry fast. amai mijn hoofd, nu was ik ineens in het engels aan het typen maar ben dan ook heel heel slecht, nogmaals bedankt!!! weet jij waarom ze gestopt zijn of zijn ze niet gestopt, scheibenbogen met die washout methode van die auto immuun antilichamen en omf heeft dat dan nog eens op een andere wijze over gedaan en had succes dacht ik. ik kan letterlijk bijna letterlijk niets meer lezen of volgen, dus daarom dat ik het aan jou nu te vragen, misschien weet jij iets. xxx!!!
Lots of research is funded by pharmaceutical companies. Many researchers have that money to do the research with a potential of new drug development to address a reason to a known dysfunction in the body. To make that hypothesis a fact, the idea has to be proven out. But in order to do that you have to be able to not only look at the science, but prove it out for that particular puzzle piece of the hypothesis. If calcium channel blocking potentially is part of the picture and there is too much calcium going into the cells causing the veins to constrict…..then there is a potential drug to correct that from happening. BUT, how much and in combination with what else will make that happen the best? For me, I listed 3 things in combination that works for me. One alone does not do it. 2 together make it good. And add the 3rd when there is MCAS connected to it. BUT, you have to go so low doses and I have to break down tablets and Capsules to get the amount low enough. And I have to time it correctly. And then, I have to rotate on and off or it stops working. So there is potential in what I use. That would need to be worked out and then the formula refined for best results with a select number of people and subsets would have to be determined for who this would be best suited.
So researchers who are granted money from pharmaceutical companies are looking to find the WHYS…..yes…..the goal is to help…..yes. But the goal is to also make money for the pharmaceutical company that funds the research.
I’m so happy to see this being explored.
I wrote of this with my own findings over 10 years ago on the DINET forum. My having low renin and aldosterone and feeling it absolutely wrong to force the kidneys to retain salt with one of the POTS medicines. I also talked about the need for me to vasodilate and not constrict my veins. Doing that made me soooooo much worse. I was going totally against anything being said to do for POTS. But it was the right thing for me. I had also realized that I needed to block calcium channels and that helped my POTS. I use GastroCrom and Tramadol to do that. They both help my POTS and MCAS. (I also find adding Bentyl, a mild muscle relaxer, to make the combination even better. But not too much or can cause depression. I rotate on and off and this is very, very low doses or it will stop working.)
(You can look up those writings if you Google DINET Forum or Healthrising blog and forum and words salt, renin and aldosterone, vasodilation, calcium channel blocker…..etc. and with my name….there is a lot there.)
Soooooo happy this is being looked into deeper. I had felt these things along with with glutamate issues to be key players. All this also affects autoimmune regulations and inflammation. Those being the core issues in my hypothesis. We are finding the pathways of dysfunction and with a few tweaks here and there, we can get better quality of life. We can’t totally “fix” it, but can apply a nice “purple bandaid?”.
Thanks for bringing this to more attention Cort!
hi issie or someone else, can you help me with my brain and translation of what i copyd obove your post? i do not understand it. thanks xxx!!!
Ik spreek een beetje Nederlands. I suggest copy paste and put into Google Translate. Goedendag, Mary
See above @konjin….hope that helps.
Blocking calcium channels….I don’t know how that works but it sure sounds interesting.
No, that makes moste people with POTS/ME much worse !
I have blocked it and i felt so sick. And i know more patiënts.
But as always maybe another subgroup will feel good with a blocker.
Be carefull!
For me being HYPERPOTS, and the other associated findings with it… calcium channel blockers dilate the blood vessels and prevent the calcium to go into the cells, particularly in the heart. What I use is a very, very mild form of it and just one of the properties in the medicines I listed.
I agree with Giji, I could NOT take a regular calcium channel blocker. But having the property there in these medicines (and those in miniscule amounts), works for me. I also use herbs to thin my blood and slightly dilate my veins more. Too much dilation and POTS is wayyyyyyy worse. There is a fine line of how much. You also need to have your timing right.
Thanks Gijs.
I really know nothing about calcium channel blockers. They worked for Issie but we are a complicated bunch.
Be careful in generalizing about Ca channel blockers. There effects vary a lot so if you have a worsening of symptoms or just a bad reaction then it may or may not be due to antagonism of channel. The ME research group at Griffith in Australia are looking at the effects of nimodipine, as reported on Health Rising:
https://www.healthrising.org/blog/2019/06/12/nimodipine-calcium-channel-blocker-fibromyalgia-chronic-fatigue-pt-i/
and https://www.healthrising.org/blog/2019/06/12/nimodipine-calcium-channel-blocker-fibromyalgia-chronic-fatigue-pt-ii/
@Ian, I forgot about those blogs. I never did try the one medicine Remy spoke of. We had talked about TRMP3 and the Griffith study before. The genes looked at in the study, all of my genes were wonky. So calcium channel function was/is at play with me and others in regards FMS, ME/CFS. The calcium channel blocker I tried years ago and it was too strong. That was before I knew to break things down and go way lower. The medicines I use occasionally now, having those properties in them, and working well for me, I stuck with what worked.
Thanks for the reminder!
Here is the forum post of us talking about the Griffith study. Remy list the snps to check.
https://www.healthrising.org/forums/threads/23andme-trpm3-snps-for-cfs-griffiths-research.5396/
Celery is a natural calcium.channel blocker and anti viral
@Oliver, yes and celery seed and olive leaf are also natural calcium channel blockers.
Note: I seldom use these RX medicines now. They are a back up and used occasionally now. Before, they were my best medicines.
ME/CFS: the disease of many hypotheses and no real answers.
i thought on this one, answer comes if treatments comes and are positive
Ha! Yes, many hypotheses….and no conclusions yet but hypotheses are a necessary step – are they not? After the hypothesis – this is what I think causes ME/CFS – comes the testing.
We have been rather rich in hypotheses and not so good in the testing but Ron Davis is testing the metabolic hypothesis, Cortene did do a small trial on their CT38 drug. Nancy Klimas is testing the drugs her models suggest will help, and hopefully, Wirth and Scheibenbogen will find a drug and test it in MECFS.
1. Its nobody with Cfs that dosnt have Thoracic outlet syndrom.
2. Intracranial hypertension is affected by Thoracic outlet syndrom and is seperatly know as the cause of fatique.
3. When radiologist isnt checking Interna jugula vena, and only have the doctors small note to work by they can never get 2+2 to be 4.
Cort, off topic, but what happened to the article on the peer-reviewed paper Whitney Dafoe had published? I was going to comment, but it seems like it’s vanished into thin air.
I just looked at my IGL Neuroscan results from Germany. Show my intracellular calcium is low, magnesium normal, and potassium high. Does say high oxidative stress. No intracellular sodium measurement. So I don’t show the high calcium or low potassium, but maybe they are looking at a micro level below that. Out of my league. However, my mitochondria show a lot of issues.
Lots of the puzzle pieces are coming together. When we get the WHYS we can get the tweaks. Have to get the WHYS first. Make sure we don’t treat symptoms (which are likely compensations and the lessor of the two evils) and get to the core of the problems, not the fringes of symptoms.
I agree issie. “Have to get the WHYS first. Make sure we don’t treat symptoms and get to the core of the problems…” Any effective systemic thinking from outside / in must be surrounded by many whys coming from many places at the biggest part of the outside “wheel” so to visualize, and work to the core as closely as possible until the last few “puzzle pieces” as you say may come together!
There is not a lot of value in testing treatments without knowing the basic physiology or biochemistry of the illness. (The core of the problems) Most treatment efforts I see with ME are based on higher level physiology or symptoms. These may help a little but are unlikely to lead to any form of recovery – just a relief of some symptoms. In addition the symptom relief by various treatments have also been temporary for most people or not effective for some.
Clearly there are some interesting treatments that can reinforce biochemical lines of inquiry, eg LDN (Naltrexone) restores some impairment of TRPM3 function in ME.
[https://www.frontiersin.org/articles/10.3389/fimmu.2019.02545/full]
This effect of LDN may be a facilitator of trpm3 function from an upstream lasting regulatory mechanism which affects the TRPM3 function and recovering calcium permeability function. Remember that naltrexone is an opioid receptor antagonist (a blocker). Opioids inhibit TRPM3 calcium flow and naltrexone recovers that.
So this helps to explain why LDN is helpful, of course its alleviation of symptoms is weak but definitely noticable. More work is needed to uncover the TRPM3 variants which are affected and their distribution to explain symptoms.
We definitely KNOW that TRPM3 channels are dysfunctional in ME. This is reliable and could be used as a test for the disease – but very expensive.
Of course we can get very complicated by brining in co-pathologies in ME but for clear research these must be isolated.
My example is to show that key molecular research is critical to finding treatments.
Amen. And the brain fog to keep us from understanding any of them….
It just seems like we are spinning around in a whirling dervish of theories. I am just getting ready to move forward with some treatments based on my Cell Trend lab results and now this new research from the same researcher in Germany comes forward. I don’t know if the two hypotheses are symbiotic or not. The word annihilation is powerful and unforgiving, pretty much describes an image of something that can never be retrieved, for us, any semblance of health or a real treatment. All so disheartening.
Not to worry about annihilation. As I remember they were talking about a signal that was blocked or annihilated. Restoring it would take removing for fixing what’s blocking the signal.
I believe their hypotheses are probably congruent with what you are trying as a key factor in them concerns immune damage to the B2ADR receptor. If you can get that fixed the blood vessels may be able to dilate better, you may get some help with blood volume, and your muscle fatigue may lessen…. Good luck!
Issie — no rush, please (you’ve typed more than enough for one day)!
When the time is right, would you share a few details about the glutamate issues you mentioned in an earlier post today? Thanks you!
@Elizabeth Kay, I see your question and wanted to acknowledge it. Dejurgen and I are working on blogs for Healthrising to put some of our ideas and hypothesis out. They will have the science included. Dejurgen is the technical writer between us. I’m more of the Summary type writer. We have both written about glutamate and you can do a search on Healthrising blog and forum and putting our names into the search.
Years ago (10 years or more) I wrote on DINET forum (site for POTS) about glutamate and where the idea/research first started. (Believe it or not by a really bad experience from chewing too much aspartame gum while writing about Salt, Renin and Aldosterone and questioning traditional ideas of treatment with POTS. Aspartame can create a glutamate overload. And I wound up in ICU overnight having a really bad MCAS response.)
Dejurgen has more of our updated ideas on Healthrising.
Much of this is above my paygrade (and brain fog level), but I have a question about the sodium. For years, I increased my sodium intake to help with osmotic pressure in the cells and seemed to feel better doing so. I definitely feel better (for up to a couple of weeks) when I have access to saline IVs. I know many others who have the same reactions. How is this explained with the theories in the article?
This article concerns that but is referring to something different. Their hypothesis states that the problematic B2ADR receptors are helping to turn off the renin-angiotensin-aldosterone system which is responsible for maintaining blood volume. Your salt intake and saline IV’s are probably helping to compensate for that problem.
Oral rehydration solution, by the way, is cheaper and possibly more effective than saline IV’s and safer than using salt https://www.healthrising.org/blog/2020/09/15/saline-ors-oral-rehydration-pots-chronic-fatigue-syndrome/
As for the osmotic pressure in the cells – I don’t have a clue about that.
IV saline is increasing volume, it is a short term solution. In an acute situation it greatly improves how you feel, especially if there is low blood volume or too thick blood. This is done a lot with POTS people. I have heard they are not doing it as much these days as in our earlier days of discovery. But for some, as a short term, crisis benefit…….its helpful. A lot of my old POTS buddies aren’t doing it as much as they once did. Some even got ports to do regular infusions. But as said, its short lived.
Yes, I believe that the oral rehydration salts after five months may be having less effect in making me feel good. I do know that they are still working to lower my heart rate on standing because I am measuring that regularly.
Currently, I have stopped them for a week to see if I can kick-start the energy from them again. I am a bit dubious that it will work, becaus eI have often tried things that work in the moment (like B-1) and then stop working.
I just looked at my IGL Neuroscan results from Germany. Show my intracellular calcium is low, magnesium normal, and potassium high. Does say high oxidative stress. No intracellular sodium measurement. So I don’t show the high calcium or low potassium, but maybe they are looking at a micro level below that. Out of my league. However, my mitochondria show a lot of issues.
Thanks Cort! This is the first article I’ve seen that gives a real explanation for that nasty exertion threshold. Mine is so strict, and if I go over , say 10%, I’m in really bad shape for a week with a PEM. Does it explain the delay? 12 hours after too much total exertion? If I go a little over my threshold, I can rest enough to avoid a PEM. But if I go too far over my threshold, nothing will stop that steady march to a full relapse the next day. Low-dose Abilify is helping me with the neurological symptoms (reducing brain inflammation) during a PEM though, so the relapses aren’t quite so horrible, but seem to have to plod along for days before stopping anyway. I can’t wait to hear what they have to say about the neurological symptoms. Maybe the delay will come up in that. I should ask them about spironolactone, which keeps me stable. I go into constant PEM’s without it. I think it impacts everything they mentioned.
@Chris, Spironolactone also helps increase potassium and lowers aldosterone and therefore salt. It is a diuretic. Some of us POTS people tried that too. (Didn’t work for me already having very low aldosterone and also not needing to increase my potassium levels. I also have high serum sodium levels.) But for a few people it was a help. It also affects adrenal function.
https://www.mayoclinic.org/drugs-supplements/spironolactone-oral-route/side-effects/drg-20071534?p=1
Spironolactone is a potassium-sparing diuretic (water pill). It prevents your body from absorbing too much salt and keeps your potassium levels from getting too low. This medicine is also used to treat or prevent hypokalemia (low potassium levels in the blood).
>>>>>>Just as a side note to people. Pay attention to properties of what you take. Figure out what that does in the body. (Medicines and herbs and any other supplement…..those are basically concentrated medicine too.) This is giving you clues what your subset type is. It can tell you what may be off in your body and what pathways to look into. It will help you figure out your own personal WHYS. We are all different. What will work for me, will not work for someone else. We may all have the same label on our DX…..but the WHY may be different. We may have some common WHYS though. So figuring those out and then the work around for the other complexities and the other factors putting us into different subsets…..thats the challenge. What I take and what Dejurgen takes, for the same pathway dysfunctions, are different. But there are some things we both take the same with equal benefit. And most of what we are doing are over the counter and ordered from Amazon. We both feel hopeful!
There is HOPE on the horizon and the puzzle pieces are coming together!!!!!
Thank you Cort for this hopeful article and also you Issie for your input. I remember I was diagnosed with Calcium in my cells that could not be explained and my potassium levels are always way low even though I take potassium supplement and drink at least a litre of coconut water a day. Again, doctors could not explain it.
I’m going to read your link Issie to see if there’s guidance on Spironolactone?
Interesting. I don’t know if it explains the delay – a really interesting part of ME/CFS.
Even though it’s different if you remember when you were able to exercise that if you really overdid there would be a delay too before the muscle aches would set in…
This is such a breakthrough theory! I praise God for this. It explains why I felt sick whenever I had my blood drawn. This makes so much sense to me. One time I donated blood and I was extremely fatigued that same day and the next. I know its part because loss of iron and other nutrients in blood etc…. but that was the only and last time I donated blood because of how awful I felt. These Gentlemen deserve the Nobel Prize in Physiology or Medicine! Cort this is beyond exciting!
Thank you for the article Cort,
Quote 1: “… high intracellular sodium levels are “the main cause for the exercise intolerance” in ME/CFS.
Quote 2: “I asked Klaus Wirth about the high sodium diets many people are on. He replied that “intracellular sodium is totally unrelated to sodium intake”. (No one should change their sodium intake as a result of this hypothesis.)”
I have been suffering from M.E. since 1989. For years my M.E. was so bad I was unable to exercise at all. I developed several food intolerances. Then I became “allergic” to salt. It felt like a harsh heartburn from my throat all the way down to my stomach whenever I had food with salt in it. So, I stopped eating salt completely, more than 20 years ago. Next my muscle cramps disappeared. And … I was able to start exercising again after years of being unable to exercise. I have now been exercising daily for more than 20 years. I jog 3-4 km daily, do push-ups, pull-ups, sit-ups, hand-stands, swimming. But I still struggle A LOT with the brain fog. And I suffer from severe MCS (Multiple Chemical Sensitivity) and food intolerances, etc.
After more than 10 years of daily exercise and eating no salt, I have moved to the coast, where for the past 9 years I swim in the (salty) ocean daily and I was told that your body would take up just enough salt through osmoses.
So, maybe the intracellular sodium would not be influenced by either a high salt diet or a lower salt diet – but maybe cutting salt out of your diet COMPLETELY, as I did – WOULD reduce the body’s ability to create enough intracellular sodium? Just asking, based on my experience with salt, cramps and the return of my ability to exercise after cutting salt out of my diet completely.
Nicolaas Roos, have you ever been tested for Porphyria types? I know some who can
exercise but not all, one does Iron Man Triathlons one of the lucky few a female. She
went decades without her Genetic diagnosis…
Nicolaas, thank you very much for sharing, fascinating insights.
I also struggle to think that a high salt diet might not adversely impact the problems Wirth and Scheibenbogen have identified (and I think their research is brilliant and gives me real hope for future understandings and treatments).
Salt is something I have gone back and forth about in my mind over and over. I experienced something similar to you when I cut it out completely (after I used to experience the same ‘burning’ sensation when I ate too much salt). My stamina improved a lot as did my gut health and libido and general clarity of mind. I have read research papers that show excess salt suppresses the thyroid, increases cortisol, breaks down muscle (at 12 grams daily) and more. Our hunter gatherer forebears would not have had access to salt save in the blood of animals they ate. I read a study in which hunter gatherers had a daily intake of 2 grams of salt.
On the other hand, do us ME folk need to take salt? Does our body really have difficulty holding onto it through low aldosterone or perhaps lactic acid causing us to wash salt out? Possibly – quite likely indeed. Then again, if our problems with hypovolemia are not caused by low aldosterone but by overly squeezed veins due to RAA axis disturbances, is adding extra salt to boost blood volume actually a good idea?
At the moment, I am back on a high salt diet as I felt that being on a no-salt diet was leading me to have excess thirst and urination. Those problems have stopped now, but they were intermittent before and usually occurred in a crash. I currently am finding it very hard to build up stamina despite a period of relatively stable health and your comment makes me wonder if perhaps I should cut down on salt again and see what happens.
Cort, I would also, like others have suggested, love an interview with these researchers. I would be grateful if you could put the example of those of us who have really struggled with salt (that burning sensation Nicolaas refers to) and the example of those who cut out salt and find their stamina improves. It does make sense that if there is less salt coming in, there would be less to build up intracellularly.
High salt solutions can be harmful. Much better to try oral rehydration solutions. Trioral works really well, can be found on Amazon and particularly when bought in the larger size is pretty inexpensive.
https://www.healthrising.org/blog/2020/09/15/saline-ors-oral-rehydration-pots-chronic-fatigue-syndrome/
From what I understand the possible problem with intracellular sodium and ME/CFS is that the cells are pumping in sodium to get rid of the proton buildup but having trouble pumping out again. Whether you have low or high salt intake makes no difference at all to that problem. Whether the cell decides to take in more sodium or not has nothing to do with the amount of sodium in your blood is loaded up with sodium or not. This issue starts and ends at the intracellular level. That’s what I understand.
Cort, this is very confusing to me. I had IV saline and I felt SO much better – for a few days. Tried the WHO oral solution – nada. No effect that I could tell.
Anyone have any ideas about that? Thanks
Nicolaas, when you wrote that you eliminated salt that you eliminated sodium, or just table salt?
There’s a film that has just been released featuring, amongst others, Carmen Scheibenbogen, by Daniela Schmidt-Langels. Bhupesh Prusty posted it on his Twitter account (he’s interviewed and Oystein Fluge and Olav Mella). It’s in German (I think!) but has English subtitles.
It’s called Living with Chronic Fatigue Syndrome. It’s 53 mins long and is available for 3 months. Be aware – there are noisy and visually striking graphics included.
‘An investigation into little known illness focusing on the experiences of three individuals suffering CFS: Ralf, Sonja and Aileen.’
https://www.arte.tv/en/videos/096283-000-A/living-with-chronic-fatigue-syndrome/
Has anyone had their bradykoinin levels measured?
Bradykinin is apparently very difficult to measure. I got the feeling that that is not an option unfortunately.
Re the low blood salt and chlorine levels, I almost always test below normal. An endocrinologist told me that even the low in the normal range is unacceptable in terms of energy. He suggested cutting back on drinking water. This doesn’t help with some other issues. Unlike Mary, my blood pressure tends to be “perfect” tending to the low side, and since almost eliminating sugar from my diet I have no glucose issues.
I assumed low sodium levels were typical of ME/CFS. Is that not so?
Thanks for this article, Cort. I need more biochemistry knowledge to follow it, but your translation helps a little.
“I assumed low sodium levels were typical of ME/CFS. Is that not so?”
Not with me, sodium is always close to max. My blood pressure is near always bang in the middle. My potassium levels are most of the measurements below average but in range.
My sodium levels are always to near top range and I eat very little salt. My potassium and calcium right in the middle. My blood pressure is variable. (With HyperPOTS, it can swing in both directions with extremes. You can’t treat the highs because of the lows or the lows because of the highs. And it can vary fast.)
I have me/cfs and use the oral rehydration recipe Cort mentions above per Dr. Chheda. In monthly labs my sodium is consistently low.
I’ve had both low sodium levels and low potassium levels. And I have low oxygen extraction and heart pre-load issue (via invasive cardiopulmonary exercise test)
Well, it would be interesting to see an actual scientific poll on it. My endocrinologist thinks the low sodium could be part of the fatigue.
PS The same endocrinologist tells me now that sodium levels are connected to thyroid levels, and my low sodium might be as a result of imbalance in thyroid hormones (I have Hashimoto’s like many of us). I’d like to see that question as part of the poll.
A lot of us don’t have autoantibodies against ß2-adrenergic receptors. I would be intensely surprised if ME/CFS turned out to be one thing. When that is said the calcium/sodium thing is interesting. I have low blood levels of calcium, sodium and potassium when I crash. It could just as well be effect as cause.
I can’t wait to read the next paper and their take on the neurological problems that ME brings. The loss of cognition is my sorest loss. Please explain to me the brain fog, the ADHD, the permanent dizzy, nauseated migraine, and a mood state that sits somewhere between hypervigilant PTSD and apathetic dysthymia.
Good description
Maybe the reason some ME/CFS patients improve on a ketogenic diet is due to reduction in the sodium-glucose co-transport into cells, particularly brain cells?
Worth noting that there are drugs that inhibit the co-transport of Na and glucose into cells – SGLT2 inhibitors, see https://en.wikipedia.org/wiki/SGLT2_inhibitor. They are used to treat type 2 diabetes but being investigated for broader anti-inflammatory properties, see bottom of wikipedia page.
Most *known* sodium-glucose transporters *seem* to be located in gut and kidney:
https://en.wikipedia.org/wiki/Sodium/glucose_cotransporter_1
https://en.wikipedia.org/wiki/SGLT2_inhibitor
However, there is doubt that all SGLT are known so some could be in the brain too.
But if this theory is correct, then should taking vasodilators like hawthorn or some medication be a remedy, right?`
Remember that herbals are very potent and can have some strong effects. Research well and make sure there is not some other health issues that would be adversely affected.
There are herbals used to vasodilate the veins, but may not have calcium channel blocking activities, but be more like an ACE inhibitor. Or even NO increasers. You have to know which pathway is wonky with you to know which one to choose.
And with POTS people, be careful! If you already have low blood pressure, lowering it more with herbals or other medications can be a huge disaster.
Know what things do, how they work and if it’s right for you. What I use will not be right for everyone. What someone else uses will not be right for me.
These are concentrated supplements and should be thought of as medicines. You need to know and understand what they do and know your body to know if that is what it needs.
Low and slow. Dejurgen and I both have to break open capsules and take less than what is considered a regular dose.
I wont recommend herbals on this subject because you have to get that right for each person and without backgrounds and knowing what is happening…..I can’t. It may be a trial and error thing. It was with me. Things that worked like ACE or ARB inhibitors were not good for me. And beta blockers caused me bad MCAS issues.
@ElizabethKay
Glutamate issues are quite difficult to understand and explain. Let me try and give you a somewhat accurate analogue here.
The brain uses neurons as components for their processing much like manufacturers of computers use electronic components. In electronics, the different components are connected with copper wires. That allows signals to travel from one component to the other.
In the brain, we don’t have copper wires. Our brains use chemicals that are guided from one neuron to another by being confined by a sort of tube in between both. When the sending neuron wants to send a message to the receiving neuron, it pushes a pack of specific chemicals down that tube towards the receiving neuron. When the receiving neuron gets a bunch of those chemicals, it knows it is expected to do something and what to do.
See https://en.wikipedia.org/wiki/Neurotransmission
Unfortunately, those tubes aren’t connected leak free. Mainly at the position of the receiving neuron, the pipe is connected “sloppy” to the receiving neuron (even if that might be for a reason). That creates the chemicals to spill “into the open space” (in the brain).
Compare that with a keyboard. So long the keyboard is dry, all messages are clear and clean. A keystroke is recorded well and transmitted to the computer for processing. Now spill a cup of coffee on the keyboard. The coffee creates small short circuits and quite many and erratic messages are send to the computer. The computer thinks you are typing as a madman on your keyboard and tries to process that overload of input. You see different applications opening, closing, saving, random text appearing on your screen and so on. It is a confusing process (like brain fog), it overloads the computer (like sensory overload) and requires a bunch of energy to do unwanted things (like being wired and tired or so much going on in your head and so few useful things happening).
Now glutamate is a main such chemical messenger in large parts of the brain. Some of the glutamate leaking “into the open” in the brain is normal. However, after each message the receiving neuron is supposed to clean up (“mop up”) the used chemicals (glutamate). The remaining glutamate that “escapes into the open (space in the brain)” must be cleaned up by other specialized cells like… astrocytes (aka astroglia).
Good cleanup of (excess) glutamate requires several things, like good transporters and energy. Having very poor (Issie) or poor (me) glutamate transporters slows the process, making us more vulnerable for the effects of poor glutamate clean up.
All of us ME patients are low in energy, slowing down glutamate removal (recycling). In so, we risk to be more confused and have more erratic signalling in our brains and things like sensory overload. That does cost plenty of energy and that further reduces the amount of energy available to clean up excess glutamate. That allows things like “wired and tired” or “sensory overload” to escalate and linger for quite some time before we manage to settle it down.
In very bad cases, the process can deplete the neurons so badly that there is massive neuronal death. The process https://en.wikipedia.org/wiki/Excitotoxicity is devastating and it seems to me our (ME/CFS patient) bodies are reasonably well able to avoid such permanent damage, possibly at the cost of strong (brain) inhibition / Dauer.
Now I mentioned poor glutamate transporters and low energy (and oxygen) in the brain, but also astrocytes / astroglia. Those play an important role in cleaning up excess glutamate and that helps calm down the brain and reduce energy waste by reducing erratic neuron triggering. Now the astrocytes are very often mentioned in ME/CFS too as being inflamed, causing a strong immune response… and those are very energy intensive processes too. So, that likely leaves less energy and focus left for the astrocytes to clean up the excess glutamate spilled all over the brain…
See https://en.wikipedia.org/wiki/Astrocyte and https://en.wikipedia.org and /wiki/File:Metabolic_interactions_between_astrocytes_and_neurons_with_major_reactions.png for the interactions between neurons and astrocytes.
This shows there are links between glutamate and sensory overload, being wired and tired, poor blood flow (too few oxygen and energy for this glutamate cleanup triggering this cycle), anaerobic energy production, brain inflammation (overactive astroglia not being able to do all thereir tasks like cleaning up excess glutamate)… and quite a few more things.
That will be for another time. I’m in the process of writing. As you see, mentioning something “plays an important role”, explaining why something plays an important role but still writing about lose ideas and trying to connect several lose ideas in ways that isn’t full of contradictions and makes sense are all entirely different challenges. Getting all done in ways that are easy enough to read and understand by others… extremely challenging. Even attempting this very slow and hard process makes ones appreciation for Cort’s skill and determination to get those blogs out despite such crippling disease grow :-).
Off topic but…just watched a good interview with Dr. Klimas on BodyPolitic. I was searching for an update on her research situation and whether she is getting funding. Well done as always. She is directing Longhaulers to this site.
I agree with the comments that answers will only be found when the cause of CFS is identified.
The history of CFS is certainly suggestive of an unique infectious agent perhaps interacting with toxic environments.
Incline Village was just one place with a cluster of CFS cases. The farming community of Lyndonville, New York had an outbreak in the 1980’s that started with 8 children who were sledding together and their illness spread to over 214 residents of the 862 people in the community. https://www.wsj.com/…/SB1000142405274870400540457617682…
During the same time as the Incline Village Outbreak, teachers in Truckee (20 miles away) also became ill.
In 1984 Chapel Hill, North Carolina, USA: “Epidemic amongst members of The North Carolina Symphony Orchestra. Low NKC [Natural Killer Cells] associated with high yield of lymphoma, astrocytoma, glioma.”
1984 Montreal, Quebec-Ontario, Canada: “Over 500 cases of M.E./CFS documented during August-November 1984 period
1985 Yerington, Nevada, USA: “In the same area [not far from Truckee, California] an M.E./CFS-like epidemic reputedly occurred in a reservation of American Native people
1986 Placerville, California, USA: “Outbreak of chronic fatigue syndrome ‘coincident with a heavy contamination of the local unfiltered water supply’.”
1988 Sonora, California, USA: “More than 35 children and adults were diagnosed with M.E. in the mountain country 100 miles from Lake Tahoe. Many of these patients were associated in some way with Columbia Community College.”
1989 Roseville, California, USA: Rosedale Hospital reported 11 cases of M.E./CFS among staff.
1990 Elk Grove, California, USA: M.E. epidemic among teachers and students
Thank you Cort for writing up this fascinating account of a hypothesis into the cause of ME/CFS. To my fairly unscientific knowledge it does sound feasible.
Does anybody know if this explanation of what is going wrong in our illness would account for feeling half dead every morning after even a good sleep? Feeling energetic on getting up is something I haven’t experienced for over 23 years of this illness.
On some mornings after my adrenal.thyroid medication has kicked in and I am still in bed I can feel ok but the energy deficit is massive once I am upright and have to start moving my body and especially my legs which will always feel like lead first thing. I would love to know if this situation fits with the researchers’ hypothesis.
I have not woken up feeling refreshed in over 30 years. I sleep well and sleep long, but not refreshed.
Just saw this regarding COVID long hauler studies. There are implications for use with ME/CFS and other diseases.
https://covid19criticalcare.com/ivermectin-in-covid-19/
Without a reliable animal model of ME/CFS, this is probably moot speculation, but given that digoxin, commonly used in cardiac disease, inhibits the sodium-potassium pump, I wonder if it might exacerbate ME/CFS symptoms, and lend some observational weight to these hypotheses.
2021 UCSD Research reveals postviral ‘Permanent Mitochondrial Lockdown’ , etc ! viralhttps://health.ucsd.edu/news/releases/Pages/2020-04-27-for-me-cfs-patients-viral-immunities-come-at-lifelong-cost.aspx
2021 UCSD Research reveals postviral ‘Permanent Mitochondrial Lockdown’ , etc !
https://health.ucsd.edu/news/releases/Pages/2020-04-27-for-me-cfs-patients-viral-immunities-come-at-lifelong-cost.aspx
Very interesting. But isn’t it from 2020?
Has this been covered on this website?
Hello Cort, Thank you for this article. For me it‘s mind-blowing.
What‘s your gut feeling about it?
Is it compatible with Ron Davies‘ ideas?
This is complex stuff – way beyond my ken – but I thought they presented a good possibility. They’re obviously very smart people and that accounts for a lot. Wouldn’t that be something if these two separate research efforts met in the middle? That would be a great sign 🙂
I agree. That would be wonderful.
All of this is easily explained with a SPECT Scan of the Brain!!! Blood flow is decreased in the brain after an emotional event.. The Brain is where it starts.. I have a Methyl Folate DNA deficiency .. I have what you need to know.. I am in touch with my body..also have had this disease since 1957.. I’m 80 now.. Heal the Brain ( not as a mental illness) Spect Scan and the body will follow.. here’s what had helped me.. Rest, no aerobic exercise .. affects the brain with massive energy and other problems in the body.. Oxygen… plenty of oxygen… and treat that with things that open the inflamed brain.. I use Brain enhancers.. Got knocked out of training for the Olympics as champion swimmer because of all this.. They have found strange looking white lymphocytes in my blood.. Natural killer cells are out of balance.. new knowledge.is this… Epstein Barr IS AN AUTO IMMUNE DISEASE…. I take anti virals…Sleep medicine, lots of B vitamins.. subliminal… I’ve lived this horrible illness… Check out what happened to a persoon before they collasped!!! Stress Burn out. and genectics are mostly the trigger.. a flare of inflammation.. touch your skin and you will find inflammation.. It’s painful but I didn’t know that’s what is was for years..Look and see if you have blood small blisters ozesing up and out on your skin.. I can’t take steroids.. They bring out all the herpes latent virus’s… Yes HERPES COMES IN SEVERAL NAMES.. cmv,Epstein barr,, Herpes Six B/// and more. There’s a new book out by Famous Physiatrist called * The End of Mental Illness as we know it””.. Drl Amen.. Amazon.. Many people are put in by polar or schizophrenia box! They never did a spect scan.. Surprise.. It looks like half the blood is missing..Inflammation is what I believe causes thie Herpes Six B…is know to cause Inflammation of the brain.. Ask a Neurologist and most of them don’t know this YET.. when they never did a Spect Scan or many other brain tests.. This is terrible but I understand why.. The Mental Health System takes 15 minutes and due to the way you come across, they call you mentally ill.. Once a doctor hears that….not knowing anything.. they rush to judgement.wHEN i HAVE PRESSURE HEADACHES THAT’S INFLAMMATION AND I COME ACROSS SCARED…hey, it’s like falling into “whoville.” Dr Suess
s. Ok.. That’s enough for now.. I am begging someone to ask me questions that are higher up.. Two of my son’s have this and my grand children..two of them//They began with some viral trigger as teenagers.. My doctor believes me so i’m lucky.. He doesn’t understand the why’s but he trusts my records and respects my information. i’m still alone on this…for now….But I fight back in a way that doesn’t upset me.. love to all.. Keep the hope… Work on tuning in on your brain.. The sharp pains, tightness like a head ban, blurry vision then go from there.. The autonomic brain is messed up for bodily symptoms… it sounds so complicated…It’s not.. Look under the hood doctors!!! That’s the brain.. It controls the flow of gasoline… LOL.. Look Damn it! Nila Shea Williams
Is there commonly available testing to check RAAS function?
My body won’t hold potassium so I have to take it Rx.
How complex is the human body?
How complex is the immune system?
How complex are all the processes of homeostasis?
I’ve been reading the articles and comments from a point of view of MS (of 20 years). I managed to drag myself out of a very dark place using diet and supplements. The doses of some supplements would be mind-boggling to most people! Eventually my brain cleared enough for me to do a (double) diploma in Nutritional Medicine.
My advice: keep it simple!
1) Sodium and potassium must be in balance. Most of us have too much sodium and not enough potassium. Under (almost) no circumstances is high sodium intake recommended. It certainly will contribute to intracellular sodium levels.
2) Calcium and magnesium must be in balance. Most of us have too much calcium and not enough magnesium. I use magnesium for cramps – it also helps to retain potassium over sodium. Note our kidneys inherently excrete potassium over sodium, to our detriment. Think of our aquatic evolution and the high levels of preservative sodium in amniotic fluid.
3) The above imbalances arise from our “Western diet”.
4) What you measure in the blood is not an accurate representation of total body content – if it’s not in the blood, it’s in the tissues. Thus the only accurate way of assessing cellular levels is by looking at symptoms, not through blood tests. The main exception to this is iron.
5) ATPase needs magnesium as an enzyme cofactor – importantly the Na+/K+ pump needs ATP, essential for keeping sodium out of cells and moving potassium in. We have boundless energy! But we can’t use it without magnesium.
6) Each of us is unique! Try to seek a more holistic approach to your health and use disease labels as a guide, rather than focusing too much on specific treatments. In terms of nutritional needs/deficiencies, required supplement doses can vary several fold between two individuals.
7) When supplementing, start slowly and give your body time to adapt. Also bear in mind there are many drug/nutrient interactions and talk to a professional if you’re at all unsure.
8) Vegetables contain minerals and so are best used exclusively over fruits in the early days of nutritional treatment.
Many thanks Cort, interesting times indeed!
I wish you all well.
PS Have I had a Covid vaccine?
No, I’m taking high dose vitamin D.
Notably I seem to have fewer infections and need far less probiotics.
Wondering about something.
Are there any people (pwme) reading this who always have high calcium & high ionised calcium (blood)?
.
Thing is:
“adrenergic antagonists can result in bradycardia, hypotension, hyperglycemia and even hypodynamic shock. This is because adrenergic stimulation by agonists results in normal calcium channel regulation. If these adrenergic receptors are blocked too often, there will be an excess in calcium channel inhibition, which causes most of these problems”.
.
So this is what Adrenergic antagonistic meds can do. But if … if you have Adrenergic autoantibodies you’re already in a state like this without any meds? Which could explain high calcium blood levels? Levels not “regulated” anymore?
Research that gives real hope.
The RAA axis abnormalities seem so key to understanding the illness.
I recently had my angiotensin II levels tested – the result 11.4 (range 19-38). And II is responsible for stimulating antidiuretic hormone and aldosterone and also regulates water/salt balance itself. I am clearly hypovolemic and I feel this result is direct evidence of that – not able to stimulate the aldosterone and ADH levels adequately.
However, I saw another article in which Cort said high Ang II levels have been found in ME and this confuses me. I wonder whether Cort or anyone else might insights on this. Have others had their Ang II levels tested and what did they find?
Recent research suggests there is an anti-inflammatory arm of the RAA axis which acts in opposition to the sympathetic/vasoconstrictive arm. It reduces blood pressure and increases vasodilation. I wonder if that might be in play as a kind of compensation. More info here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7524035/
Potassium being low – this would also link to the paralysis of many with severe or very severe ME – hypokaleimic periodic paralysis – which can be triggered by exertion (although triggering factors depend on the person) – potassium levels suddenly drop at a cellular level, which prevents communication signals in the nerves, preventing limbs from movement (and sometimes in my experience preventing sensations so all causing total numbness). See Stonebird (Greg and Linda Crowhurst) for research in this. Twice daily potassium tablet has reduced mine a lot (although bananas could do similar). Also see MEpedia on periodic paralysis.
FND as described by Jon Stone, pal of Michael Sharpe and with the awful website that suggests FND for almost anything neuro related, uses the explanation of FND being like the computer hardware (parts) work but the software (signals) don’t – which is how periodic paralysis could be described – except the signals are not psychological but biological / physiological.
This kind of makes sense. I have been baffled by something having to do with my chronic fatigue. Two years ago, I bought a swim spa and use sea salt in it. It has helped me tremendously and makes me feel amazing. When I am in the pool not only do I feel I can swim, I feel I might be able to be an Olympic swimmer. The reality it that I can’t even do a minute of swimming without crashing. But using the powerful jets as a massager, I have completely gotten rid of body pain I used to have. With the swim spa, a brain supplement and every-other-day of banana bag vitamins, I have days that I feel normal (20 years of illness not feeling normal). Because of dramatic improvement in how I felt, I expected for my chronic fatigue to improve slowly. It has no, I have only had very minor improvement. I am so shocked and frustrated. After reading this I realized that I am no longer constantly thirsty so the salt and minerals are helping me but the intracellular issue is still there. At first I was using pool sea salt and I felt great, when I started using dead sea salt I felt even better. I didn’t even want to get out of the pool, I had to time it and make myself get out.