

In the third part of the Mitochondrial Enhancers for ME/CFS and Fibromyalgia series, we turn to magnesium – a mineral that potentially impacts an astonishing array of processes.
The Mitochondrial Enhancers for Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia Series
- Pt I: D-Ribose, CoQ10 and PQQ
- Pt II: L-carnitine and Acetylcarnitine
- Pt. III: Magnesium
- Pt IV: N-acetyl cysteine (NAC)
- Pt V: Oxaloacetate
- Pt. VI: Niacin, Niacinamide and Nicotinic Riboside
This is part III of an ongoing series on the mitochondrial enhancers for ME/CFS and FM.
Ubiquitous and underrated magnesium (Mg) is a mineral that everyone with chronic fatigue syndrome (ME/CFS) and/or fibromyalgia (FM) should think about. Featured in hundreds of biochemical reactions, magnesium is a muscle relaxant, blood vessel supporter, nervous system regulator, calmer, blood sugar regulator, HPA axis stabilizer, blood pressure (BP) reducer (in people with high BP) – it even has anti-inflammatory effects. Magnesium deficiencies promote the production of substance P – a nasty pro-inflammatory factor upregulated in fibromyalgia. Plus, it plays a major role in energy production.
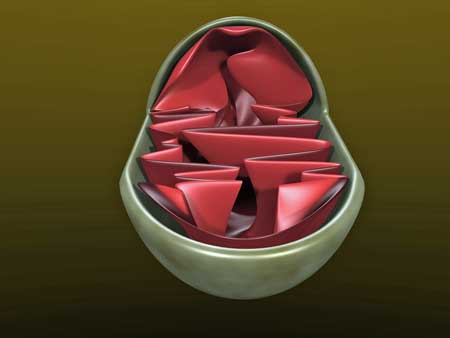
In “Mitochondria and the Future of Medicine” Lee Know reports that our mitochondria are the main intracellular magnesium storehouses in our bodies. Not only is magnesium bound to ATP, but it helps stabilize it and helps make it usable by our bodies. Carolyn Dean MD reports that magnesium plays a role in 6 of 8 steps of the Krebs cycle that powers aerobic energy production.
A magnesium deficiency in the smooth muscles lining our blood vessels could leave them tense and unable to relax – causing the blood vessels to narrow (vasoconstrict) – something that many believe is happening in ME/CFS/FM.
Craig reports, though, that the average intake of magnesium in the US has probably fallen markedly over the past 100 years. Antacids, antibiotics, antihistamines, and blood pressure-lowering drugs can all lower magnesium levels. A recent review article, “Magnesium Status and Stress: The Vicious Circle Concept Revisited“, adds high sodium, calcium, and protein diets, caffeine, and alcohol to the list. Dr. Dean adds fluoride, oxalic acid (spinach, chard, and rhubarb – cooking removes the oxalic acid), bronchodilators (for asthma), birth control pills, green and black tea, depleted soils, dairy products, and high Vitamin D intake to the list of possible magnesium depleters.
Craig believes that “chronic, subclinical magnesium deficiency” may be contributing to increased risk of cardiovascular disease and depression. Indeed, studies across countries often find an inadequate intake of magnesium.
Chronic fatigue syndrome (ME/CFS)
Magnesium levels are thought to be low in many adults but could they be even lower than that in ME/CFS? Some studies suggest so, but Craig knocks most ME/CFS magnesium studies for their low quality. One study that seems pretty good found that supplement Mg did increase in magnesium body stores, improved antioxidant status, and reduced free radical production.
Dr. Myhill believes mitochondrial problems are causing magnesium to leak out of cells and calcium to leak in. In “Magnesium: Reversing Disease“, Dr. Thomas Levy points out magnesium works to keep intracellular sodium and calcium levels down. Levy believes magnesium supplementation should be the first-line calcium channel blocker attempted and points out that magnesium supplementation may also support thyroid and sex hormone status.
Carolyn Dean MD, ND in “The Magnesium Miracle” agrees, asserting that an imbalance between magnesium and calcium can result in constricted blood vessels and muscles, increased blood pressure, headaches, gut motility problems, reduced ATP synthesis, inflammation, restricted breathing and asthma.
Dean’s and Levy’s calcium channel blocking ideas are interesting given that Wirth and Scheibenbogen have proposed that high intracellular sodium and calcium levels are causing post-exertional malaise in ME/CFS.
Fibromyalgia and Pain

Magnesium plays a role in an astonishing array of processes.
More magnesium studies have taken place in fibromyalgia and pain. Several studies suggest that both dietary and serum magnesium levels are low in FM.
Theoretically, magnesium should be effective in treating pain as it blocks calcium from activating the NMDA receptors, which then turn on the central sensitization process. In fact, because NDMA receptor activation should also deplete the neurons of magnesium, one might add disorders of central sensitization to the list of magnesium-depleting factors.
Ketamine and memantine also block these receptors. Substance P, which has been implicated in fibromyalgia, enhances NMDA receptor activity. A 2021 review, “Magnesium for Pain Treatment in 2021? State of the Art“, suggests that NMDA receptor activation may be also causing sleep, fatigue, and anxiety problems.
A 2020 review, “Magnesium and Pain“, reported that adding magnesium sulfate to anesthesia can reduce the levels of opioids needed as well as pain levels post-surgery. The fact that it may reduce the levels of other anesthetic drugs used during surgery suggests adding magnesium sulfate to anesthesia might be a good option for people with ME/CFS/FM. The 2021 review reported that 66% and 73% of randomized control trials found reductions in pain and the use of opioids after surgery.
The authors concluded that “Mg appears to be a good non-drug alternative for reducing post-operative pain by limiting the side-effects of commonly prescribed opioids, but this aspect needs to be explored further.”
The study also found that 44% of randomized control trials in migraine, 40% in renal pain, and 50% in chronic pain also found significant reductions in pain. Despite the generally good findings, the wide variety of dosages and types of magnesium used, however, precluded the authors from recommending or not recommending any specific form.
Migraine
Migraines are common in fibromyalgia and ME/CFS. A magnesium/migraine metareview concluded that “high levels of magnesium dicitrate (600 mg) seems to be a safe and cost-efficient strategy in clinical use.”
Dr. Teitelbaum recommends magnesium for migraines (see below) and states that magnesium IVs can stop an acute migraine attack in its tracks. He also recommends 75-200 mg of magnesium at night to help with sleep. Lower the dose if diarrhea occurs or try MagSrt, which Teitelbaum reports does not cause diarrhea. (MagSrt contains magnesium malate, plus active forms of B Vitamin Cofactors (B6, B9 and B12) to enhance absorption).
Magnesium and Stress
A French review, “Magnesium Status and Stress: The Vicious Circle Concept Revisited“, noted that the symptoms of magnesium deficiency and stress (fatigue, irritability, mild anxiety, muscle tension/cramps, stomach problems, headaches) are similar.
After demonstrating that magnesium interacts with the important players of the stress response and has a neuroprotective effect, the authors asserted that chronic stress should lead to magnesium depletion, which will increase chronic stress and so on. They highlighted one study which demonstrated an increase in heart rate variability after Mg supplementation in athletes. They recommended increasing magnesium supplementation during stressful times.
Meta Study Reviews
Because metareviews pool a bunch of studies together and review them as a whole, they’re more accurate than single studies.
While the quality of the existing evidence was poor (a common finding in metareviews), one metareview found a beneficial effect of Mg on anxiety. The evidence was also too mixed to come to a conclusion about chronic pain but the metareview did note that some trials had positive results. Another metareview concluded, though, that magnesium supplementation significantly reduced blood pressure in people with insulin resistance, prediabetes, or other non-communicable chronic diseases. It also reduced insulin resistance in people with that condition.
The Gist
- Magnesium features in a wide array of processes that may figure in ME/CFS and FM including energy production, muscle relaxation, blood vessel supporter, nervous system regulator, brain calmer, blood sugar regulator, HPA axis stabilizer, blood pressure (BP) reducer, anti-inflammatory.
- Most of the magnesium in our bodies is found in our mitochondria where it plays a role in 6 aspects of the Krebs cycle, which powers our mitochondria.
- With a wide variety of magnesium depleters present in our modern lives (see blog), some doctors think that magnesium deficiencies are common.
- Magnesium, interestingly, blocks calcium uptake into the cell. Wirth and Scheibenbogen believe high levels of sodium/calcium uptake are responsible for the post-exertional malaise found in ME/CFS.
- Some studies suggest magnesium deficiency occurs in ME/CFS and FM, but better studies are needed. Review articles, however, suggest that magnesium may be helpful in pain, migraine and other conditions.
- At least ten different kinds of magnesium – all with different properties – are available, making it difficult to choose one. Courtney Craig, an ME/CFS/FM specialist recommends glycinate, taurate, orotate, and malate. She particularly recommends magnesium taurate for ME/CFSFM patients, as studies show it easily makes its way to the brain. Individuals can have varying reactions to different forms of magnesium; if one doesn’t work for you, you can try another one.
- Epsom salt baths actually work. Studies show that a couple of Epsom salt baths a week can increase magnesium levels.
- Several alternative health doctors stated that serum magnesium tests are useless and, as magnesium supplementation is generally safe, recommend doing personal trials. Red blood cell magnesium tests appear to be pretty affordable and are more accurate.
- It is possible to overdose on magnesium but appears to happen rarely and mostly in hospital settings, according to Dr. Dean. Blood pressure reductions, difficulty breathing, irregular heartbeats, back and pelvic pain, and confusion can indicate too much magnesium is being taken.
- Some experts recommended 350 mg/day while others, such as Dr. Dean, went much higher (600-1200mg) for those with severe deficiencies. Dr. Dean reports it may take a year for magnesium levels to reach optimal levels.
Taking Magnesium
Magnesium may play a vital role in our bodies, but that doesn’t mean that supplementing with it is easy. Magnesium is available in a daunting array of forms. Some people may react poorly to some and well to others.
The Bioavailability Question
Some forms of magnesium have dramatically higher bioavailabilities than others. The authors of the 2021 review, however, warned about placing too much emphasis on bioavailability, as some studies using low bioavailable forms of magnesium (oxide) had good results while others using more bioavailable forms had worse results.

Many different forms of magnesium exist…Which to take?
A recent review, “Bioavailability of magnesium food supplements: A systematic review“, concluded that organic forms of magnesium (malate, citrate, glycinate, aspartate, glutamate) are the most bioavailable, that the type of magnesium you take determines where in your body the magnesium ends up, and that all magnesium supplements can be used to maintain physiological levels in healthy people.
It’s Elemental, My Dear Watson
(Thanks to PamC for bringing up this issue which I didn’t really understand until now). Because elemental magnesium is not easy to get into the body it is always bound to something else when you take it as a supplement. Magnesium citrate is bound to citrate, glycinate to glycine, and so on. The substance magnesium is bound to usually takes up more of the pill – quite a bit more of the pill – than the elemental magnesium itself.
That brings up the question is – if you’re taking 400 mg of, say, magnesium glycinate a day, how much elemental magnesium are you actually getting? According to Wikipedia not very much. Wikipedia reports that magnesium glycinate contains only 14.1 elemental magnesium by mass providing you with about 56 mg of magnesium a day.
Percent elemental magnesium
- Magnesium glycinate – 14.1%
- Magnesium taurate – 8.9%
- Magnesium malate – 15.4%
- Magnesium citrate – 11.39%
- Magnesium threonate – 12.2%
- Magnesium oxide – 4%
The only book I saw that this issue was discussed in was Dr. Dean’s “The Magnesium Miracle“. (See dosing for more on this topic.) She uses the low elemental magnesium levels found in supplements to argue for using ReMag which supplies more elemental magnesium. ReMag states
“ReMag Magnesium Solution is a 60,000ppm concentration of 99.99% pure elemental magnesium in liquid form and is very strong. You can begin with 1/2 cap or 1/2 tsp twice daily, for a total of 1 tsp, in water or juice with or without food. This dose is only used after several months of an introductory dose of 2-4 tsp. Begin slowly taking 1/4 tsp daily and increasing by 1/4 tsp every 2 days to the desired dose. Best taken in a liter of water – sipped through the day along with ReMyte and sea salt as preferred,”
There is bioavailability question as well. While organic forms of magnesium are more bioavailable, they also tend to contain less elemental magnesium than inorganic forms. Taking 400 mg. of magnesium oxide with its very low bioavailability might give you less magnesium than 100 mg. of magnesium glycinate which has higher bioavailability. A study found that even with their lower elemental magnesium levels, though, the organic forms tended to provide more magnesium overall; i.e. bioavailability trumps elemental magnesium levels.
Taking a $49 red blood cell magnesium test to assess your progress over time might help this confusing situation. Check Dr. Dean’s out here.
Types of Magnesium to Take
ME/CFS nutritionist Courtney Craig notes that the two forms of magnesium most recommended by doctors (oxide, citrate) have the worst bioavailability. She reports:
- Magnesium oxide/citrate – neither are well absorbed.
- Magnesium chloride, lactate, and aspartate: bioavailability improved over oxide/citrate.
- Magnesium sulphate: often used intramuscular injections or IV.
- Magnesium orotate: no stomach upset, subject of cardiovascular studies.
- Magnesium taurate: good absorption, gets through to brain, best for migraine.
- Magnesium malate: used in clinical trials of Fibromyalgia (though poor design), minimal GI side effects.
- Magnesium glycinate: better bioavailability and fewer GI side effects.
Dr. Levy, an alternative health MD, and the author of Magnesium: Reversing Disease“, reports:
- Magnesium oxide – poorly absorbed but definitely works if you take enough of it (take 500 mgs/daily).
- Magnesium citrate – cheap and commonly used to induce a cleansing diarrhea.
- Magnesium sulfate (Epsom salts) – best used in baths.
- Magnesium carbonate – becomes magnesium chloride in the stomach and has antacid properties (try if you have acid reflux).
- Magnesium taurate – very bioavailable, has antioxidant and anti-inflammatory properties, and is the most plentiful amino acid in the body.
- Magnesium gluconate – easily absorbable, is retained in the body well and is a good chelator. Use if attempting detox.
- Magnesium chloride – impressive anti-viral properties and is absorbed well. Use if fighting off infection.
- Magnesium glycinate – the most well-absorbed form, and should be helpful with oxidative stress.
- Magnesium aspartate and glutamate – should be avoided if you are taking high doses.
- Magnesium threonate – a liposomal form of magnesium with potentially high absorption, crosses the blood-brain barrier and may positively impact brain functioning. Levy says only buy from reputable companies. May be easy to overdose – assess blood pressure to see if it is continually lowering.
Dr. Carolyn Dean, the author of “The Magnesium Miracle“, mentions only three types of magnesium.
- ReMag – her ionic product.
- Magnesium sulfate in Epsom salt baths.
- Natural Calm – an effervescent magnesium citrate power.
Chemical analysis of magnesium oxide. (from Wikimedia)
Focus on Specific Magnesium Types.
- Magnesium malate was used in a fibromyalgia study. It is combined with malic acid (found in many fruits) which in animal studies has been shown to increase absorption. Malic acid may be able to promote muscle recovery after exercise. It is also reportedly a natural antacid.
- Magnesium threonate – numerous mouse studies suggest magnesium theonate may help cognition, pain and/or depression.
- ReMag – Dr. Dean’s formula which she maintains “is a breakthrough in magnesium therapeutics”, and which is absorbed at the cellular level. She asserts ReMag increases bioavailability and reduces gut problems because it’s absorbed into the cells in the mouth, esophagus, stomach, etc., rather than having to make its way down to the small intestine to get absorbed. It comes in liquid or lotion form and can be used in a spray bottle for muscle aches and pains.
- Magnesium aspartate / glutamate – Dr. Dean does not recommend either as they can break down into excitotoxins in the brain.
Possible Takeaways
- If you have problems with acid reflux – try magnesium malate or carbonate.
- If you have gut issues – try magnesium glycinate, malate, ReMag or orotate ((Dr. Dean reports magnesium is a safe and effective treatment for IBS-related constipation.) Dr. Dean reports that a few people may get a laxative effect from any form of magnesium (except ReMag).
- If you have cardiovascular issues – try magnesium orotate.
- If you have pathogen issues – Dr. Levy recommends magnesium chloride.
- If you’re looking for anti-inflammatory effects – try magnesium taurate.
- If you’re trying to detox – try magnesium gluconate.
- If you’re trying to reduce anxiety – try magnesium taurate.
- If you want to impact the central nervous system or have migraines – try magnesium taurate (Dr. Teitelbaum recommends taking 200 mg/magnesium at night as well as a product called Neurocomfort, which contains magnesium for better sleep).
- Be wary of magnesium aspartate/glutamate as they may trigger the production of excitotoxins in the brain.
Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia (FM)
Craig, an ME/CFS specialist, recommends four kinds of magnesium (Mg orotate, taurate, malate, or glycinate) for people with “clear mg. deficiency”.
If you’re a person with ME/CFS without a clear deficiency, and particularly if you have migraines, she suggests magnesium taurate as it is absorbed well and gets into the brain quickly. Click to consult with Dr. Craig).
Magnesium taurate has high bioavailability, has antioxidant, and anti-inflammatory properties, and gets into the brain quickly. It is Dr. Craig’s first recommendation. Magnesium glycinate is well absorbed and is good on the gut. Magnesium malate has been used in FM studies, may help with muscle recovery, and is easy on the gut. Magnesium orotate is interesting in that it has cardiovascular effects that could apply to ME/CFS/FM.
ReMag has not been well studied but is certainly another possibility. Note, though, that all forms of magnesium may be helpful.
Also, note that the reactions to magnesium can be quite individual. One person may tolerate one form or do well on one form and not another.
Testing
ME/CFS nutritionist Courtney Craig reports that because much magnesium is bound to proteins, blood tests for it may not be accurate. (Ninety-nine percent of magnesium in the body is found inside cells). Noting that the body does everything to keep serum magnesium levels within a normal range – including pulling magnesium out of bone and muscles, Dr. Dean calls serum magnesium test “worse than ineffective”.
Dr. Myhill also believes that measuring serum magnesium levels is a “waste of time”. Similarly, Dr. Levy believes that because magnesium does most of its work within cells, “body-wide deficiencies may be present” even when serum magnesium levels are normal.
Dr. Dean, Dr. Myhill, and Dr. Levy all suggest that if you have a condition that’s possibly indicative of a magnesium deficiency (ME/CFS and FM count) to simply give magnesium a try.
Testing may not be necessary, but if you’re going to get tested, red blood cell magnesium tests are affordable and fairly accurate.
The red blood cell magnesium test, on the other hand, is cheap, can be ordered online (wwwrequestatest.com / DirectLabs.com), and while it is not completely accurate, it is more accurate. With the normal range between 4.2-6.8 mg/dl, Dr. Dean asserts you want your level between 6.0-6.5 mg/dl (or 2.5-2.57 mmol/L). Dr. Myhill reports that she finds that red blood cell magnesium is invariably low in ME/CFS.
Dr. Dean reports that red blood cell magnesium levels may actually drop during the first couple of months of taking magnesium as the body pulls more and more of it in. After a time, though, they will begin to rise again. It may take a year for them to stabilize. Dr. Dean recommends repeating the test every three to six months.
Blood ionized magnesium and mononuclear cell tests are more accurate but are limited to research studies. IV magnesium load, muscle biopsy, and sublingual epithelial cells tests are also more accurate.
Dose
Dr. Dean believes that even with a good diet that provides about 250 mg/ magnesium daily, supplementation is usually needed. Dr. Levy believes that “some degree of supplementation is in order for just about everyone”.
Courtney Craig reports that the Institute of Medicine has set an upper limit of magnesium supplementation at 350 mg/day. She states that dose produces gut problems in very few people.
Dosing is complicated by the low amounts of elemental magnesium found in supplements (see earlier section). Taking the recommended 400 mg/day of the magnesium glycinate I purchased yields me only 56 mg. of elemental magnesium a day. I would have to take 28 pills a day to get 400 mg of elemental magnesium a day!
A good diet, however, is actually a good source of magnesium. High sources of dietary magnesium include nuts and seeds (including peanuts), beans, whole grains, dairy products, greens, dark chocolate, and some tap waters. A good diet should yield several hundred mg/magnesium a day – leaving perhaps a hundred or more magnesium to be derived from supplements. If that’s true the 400 mg of magnesium glycinate (56 mg of elemental magnesium) that I’m taking isn’t as far off the mark as I first thought.
Perhaps the best thing to do, though, is to get a red blood cell magnesium test, start taking magnesium, and see if your magnesium levels climb over time. (They may drop at first).
Dr. Dean recommends building up from 75 mg to up to 600 mg a day for one to three months and seeing if your symptoms improve. For people with severe magnesium deficiency, 600-1200 mg/day are needed. She believes it can take up to a year for your body to become fully saturated with magnesium. At that point, you can reduce your magnesium intake.
Dr. Dean recommends taking magnesium 2-3 x’s a day. Taking it at night may help with sleep. She notes that vitamins B-1 and B-6 increase the amount of magnesium able to enter the cells, and recommends taking a multimineral supplement as well. She also recommends getting enough calcium in your diet (600 mgs/day) or taking a supplement.
Dr. Dean believes you should get your magnesium levels up before supplementing with vitamin D. Because magnesium is required for vitamin D metabolism, Dr. Dean believes that taking a lot of vitamin D can soak up your magnesium stores, leaving you magnesium-depleted in other areas. Because magnesium grabs onto calcium she believes high vitamin D supplementation can result in high calcium levels – a bad situation in her book. Dr. Dean recommends only 1,000-2,000 mg of vitamin D daily – which is less than many supplements provide.
Dr. Dean is at odds with Dr. Myhill and Dr. Levy on vitamin D. Dr. Myhill believes that since vitamin D is needed for magnesium absorption, at least 2,000iu and often 10,000iu of vitamin D should be taken. Dr. Levy recommends 5,000iu a day.
Other Forms of Magnesium
Epsom Salt Baths
Can something as easy and satisfying as an Epsom Salt bath increase magnesium levels? Precious few studies have been done.

Magnesium is better absorbed through the gut, but one study suggested the Epsom Salt baths actually work.
While a 2017 research review would not recommend Epsom Salt baths on the basis of the evidence found (it said larger, better studies are needed), it did find studies suggesting that prolonged soaking (i.e. regular magnesium sulfate baths) were able to increase magnesium levels.
Rosemary Waring’s 2016 paper (which was not included in the 2017 review) asserted that while magnesium is best absorbed through the gut, that “some absorption across the skin can take place under favorable conditions“. Her paper, “Report on Absorption of magnesium sulfate (Epsom salts) across the skin“, outlined what those favorable conditions were.
She found that after seven days of baths “all individuals had significant rises in plasma magnesium and sulfate at a level of 1% Epsom salts (600 grams/per standard bath)”, and that most individuals had raised magnesium levels when Epsom salts were used in lower concentrations (400g MgS04 added to a standard bath).
The Waring paper reported that simply bathing 2 or 3 times/ week, using 500-600g Epsom salts (just over 1 lb) per bath each time, would provide the maximum benefit. Dr. Myhill reported that at that level, the water should feel “slightly soapy”.
IV Magnesium
Levy reports IVs are very effective ways of increasing magnesium levels and have been used in many settings but must be carefully dosed and applied. Dr. Teitelbaum highlights the role magnesium plays in “Myers’ Cocktails” stating that they open the blood vessels to the tight muscles flooding them with nutrients and washing away toxins. Magnesium chloride is often used in Myers’ cocktails.
Intramuscular magnesium injections
Dr. Sarah Myhill recommends magnesium injections, but if those aren’t available, she recommends her patients take her Multi Mineral Mix, which has magnesium and other minerals.
Side Effects
Magnesium is not like Vitamin C or the B-vitamins – you can overdose on it. While overdosing is rare, it can happen and when it does, it produces symptoms like drops in blood pressure, difficulty breathing, irregular heartbeats, back and pelvic pain, and confusion. Dr. Dean reports that the “very few reports” of magnesium toxicity have occurred in hospital settings where patients overdosed on magnesium IVs.
Sometimes doctors recommend increasing magnesium to the level when stomach upset occurs, and then pulling back. Some people, though, experience stomach upset at low doses of magnesium. They should try other forms, including possibly ReMag, which Dr. Dean says impacts the gut the least.
Dr. Dean reports that people with kidney failure, myasthenia gravis, excessively slow heart rates, or bowel obstructions should not take magnesium.
Conclusion
Most of the magnesium in our body is found in the mitochondria and it is heavily involved in energy production – and so many other things as well. Magnesium supplementation is not going to cure ME/CFS or fibromyalgia but it is involved in many processes that are believed to impact those diseases. With the energy production, brain, cardiovascular, and stress response problems present in these illnesses, magnesium is a kind of a foundational supplement that everyone with these diseases should consider.
People with these diseases might want to first consider if they’re regularly taking any of the magnesium energy depleters (antacids, antibiotics, antihistamines, bronchodilators (for asthma), blood pressure-lowering drugs, high sodium, high calcium, and high protein diets, caffeine, alcohol., oxalic acid (spinach, chard, and rhubarb – cooking removes the oxalic acid), birth control pills, green and black tea, etc.
Magnesium is safe enough to not require testing to begin supplementing with it. If you do get tested red blood cell magnesium tests appear to provide a nice combination of accuracy and cost-effectiveness. As with anything if you do decide to supplement with magnesium it’s best to start low and go slow. A variety of possibilities are available. If one type of magnesium causes upset then another can be tried. Gut upsets can be largely avoided by using more gut-friendly forms. A good response to magnesium can come quickly or take a month or more to show up.
The Mitochondrial Enhancers for Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia Series
- Pt I: D-Ribose, CoQ10 and PQQ
- Pt II: L-carnitine and Acetylcarnitine
- Pt. III: Magnesium
- Pt IV: N-acetyl cysteine (NAC)
- Pt V: Oxaloacetate
- Pt. VI: Niacin, Niacinamide and Nicotinic Riboside






Since I take some opioids for chronic EDS type pain, I take magnesium citrate every day for bowel mobility. Does help. Now, thanks to your article, I have to reevaluate… Perhaps taking several forms might be better…
Magnesium Glycinate works well for me as a muscle relaxant and it helps me sleep.
Good to hear. For some reason even though it’s been highly recommended for years and I have stiff contracted muscles, a raging stress response, and could really do with some calm, I have rarely taken magnesium. I’m kind of appalled that I’ve mostly ignored it for decades. Crossing my fingers.
I’m hearing you on the raging stress response! The older I get the worse it seems to get. My heart sometimes feels like it is jammed onto an over-drive setting and the shakes, anxiety and heart racing that accompany it are unpleasant.
On the subject of magnesium, I tried supplementing it a few years back (citrate / orotate blend) and it did feel very calming. I gradually stopped taking it though because it also made me feel slightly nauseous. However epsom salt baths sound like they could be soothing for a wired nervous system on so many levels. Thanks for the tip.
I just heard that powdered gaba held under the tongue works fast for stress and panic attacks.
Interesting – thanks!
Our holistic cardiologist (also board certifed) said magnesium is vital for so many things including using the calcium correctly, for heartbeat regulation, and several other important functions….we used magnesium gel daily ( about the size of a quarter on the chest) and I was tested to have good levels of it. When I told him I couldn’t take the magnesium citrate, because it gave me very loose bowels, he recommended that if I want to take it orally, I should use Magnesium Glycinate…the glycinate works well and helps bowels move normally taken every day.
Can you tell the name of the magnesium gel you used?
What are the studies on Magnesium in oil form? I’ve not tried these forms listed in the article in capsule/pill for. Or taken the liquid by mouth. Oil was recommended by an elderly man at work. Helps his inflammation.
I do use magnesium oil. I depend on it for my pain. Especially the awful numbness and tingling in my legs and upper body. The bloated and inflammatory feeling. Helps my digestion. Although I’m still sensitive to milk.
If I’m over stimulated (loud noises, someone hugged me too tight, I got scared, etc) it works within 10 minutes to calm my nerve pain. I don’t get migraines. But I get tension headaches after a flare up. And I just put some on my hand and wipe it gently on my kneck and forehead. Works fast. I don’t even need steriods anymore. I don’t need muscle relaxers (took the tension away so I can walk, but my body ached more because I’d sleep too much with these relaxers, feeling depressed).
I had to use the oil daily for a few months but my numbness and tingling have went from daily pain to triggered pain. A carry a bottle of it to spray on now. Pain all over my body happens when I’m triggered or stressed myself out.
I’d like to see if there’s any research on oil form.
If I remember correctly, a few studies show that magnesium in oil form can penetrate the skin.
Thanks for this summary, so many magnesium options.
I might try Dr Country Craig’s suggestion of Magnesium turate as I don’t have any clear deficiencies.
Does anyone know how, Doctor’s Best, High Absorption Magnesium 100% Chelated fits into this analysis?
I couldn’t see Chelated mentioned
The Doctors best label reads Magnesium
(from 2,000 mg magnesium lysinate glycinate chelate) 48% of recommended daily intake.
I have been buying from from iherb to Australia regularly
https://au.iherb.com/pr/doctor-s-best-high-absorption-magnesium-100-chelated-with-albion-minerals-100-mg-240-tablets/16567
I am a little confused about the recommendations given for the various types of magnesium. Are they talking about Elemental Magnesium doses or the amount in a supplement?
For example Cort you quote Dr Dean saying we should take between 75 mg to 600 mg day so is that elemental magnesium or the amount of the actual tablets? I presume she does mean elemental so if that is the case it would mean one would have to take large quantities of magnesium citrate or glycinate to get to that amount. I doubt many of us would be able to take that amount of mag citrate without having very loose bowels and G I discomfort.
Also doctors recommend 400 mg magnesium for relief of migraines but again are they referring to elemental magnesium or total mag from tablets? I have never seen that clearly stated even though my GP gave me a leaflet for a recommendation to supplement 400 mg of magnesium together with B2 and Q10.
Thanks Cort for this series to informative articles and for any clarification.
I am really glad I have read your article today because it’s made me take a fresh look at the amount I need to take each day especially for my severe muscle issues especially in my legs.
It’s a great and rather disturbing question. My understanding is that she is talking about elemental magnesium and she refers to the huge number of capsules she would have had to take to get her magnesium levels up. (She was severely deficient).
I checked out several brand-name magnesium bottles. They all refer to the amount of magnesium – as magnesium glycinate or magnesium citrate or whatever is in the capsules. It doesn’t appear that they’re separating out the glycinate portion from the citrate portion. Since they say that they’re providing magnesium as magnesium glycinate – we may not be getting as much magnesium we think.
Wikipedia says that magnesium glycinate contains 14% magnesium….https://en.wikipedia.org/wiki/Magnesium_glycinate which means that their daily serving of 400 mgs. only provides 56 mgs. of elemental magnesium.
Another issue is bioavailability. Magnesium glycinate has high bioavailability but how high? I don’t know.
Dr. Dean gets around this by taking ReMag which she says is absorbed right into your cells.
I just added a section to the blog which reports the amount of elemental magnesium found in many combinations. An added twist is the amount of magnesium we get from our diets.
Hi Pam and Cort,
Thanks for bring this issue up. Even some doctors who recommend mag supplementation don’t understand the difference between total quantity and elemental. I remember telling an ME specialist that I only take 200-400mg because it’s elemental and any more than that upsets my stomach. She had no clue what I was talking about and insisted on taking up to 800mg! Would have been a diarrhea nightmare if I had listened.
Not sure if this is available in the US, but I take mag. supplements by CanPrev, a Canadian company. All of their products clearly identify the amount of elemental magnesium on the front of the bottle. If fact, it’s part of the specific product’s name. For example, I use Magnesium BisGlycinate 200, which contains 200mg of elemental.
The other thing to note is that a lot of bigger, cheaper supplement companies mislead consumers about which type of magnesium they’re getting. I’ve seen a number of Mag BisGlycinate bottles which, if you read the full ingredients list on the back, turn out to contain higher amounts of inferior forms (apartate, citrate, oxide, etc.).
Cort, are you aware of Morley Robbins?
He’s got a very in depth protocol on how to reverse illnesses with magnesium.
Sometimes, people have a problem with magnesium because they don’t have cofactors such as as adrenal cocktail which enables the magnesium to be taken up
Never heard of him – thanks for the tip though! Magnesium has turned out to be quite an interesting and complex mineral! Not surprised there’s more to learn.
https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/warning-letters/new-capstone-inc-525164-06272017
ReMag has been questioned by the FDA.
A very important article! I use Ancient Minerals magnesium chloride cream that I buy on Amazon. I have found that I do much better at absorbing treatments transdermally than in oral form. Magnesium was a mainstay of Dr.Paul Cheney’s treatment protocol as were hydroxocobalamin b12 injections. In a patient communication, Dr. Cheney said that B12 injections were reported to be the most helpful treatment in a survey of a 1000 of his patients. I have just gone back on the B-12 protocol and am already feeling better. B12 seems to relieve my sense of chronic brain inflammation. Another part of Dr. Cheney’s protocol that I am on is Nexavir… the new form of Kutapressin… that is now available in cream form without a prescription. https://www.nexco-pharma.com/ Nexavir is recommended as an immune stimulant with antiviral properties on the HHV6 Foundation web site. https://hhv-6foundation.org/ Immunopro whey supplement is also recommended on this site and I have taken this for years.
When I think of magnesium I automatically think of Cheney…he loved magnesium for people with ME/CFS. Thanks for the tip on the cream…there are so many different formulations of magnesium, it’s good to hear some that have worked.
B-12 would be another potential foundational supplement. It’s kind of weird that I think I tried it once and know so little about it – yet it has been used again and again and again.
Again I follow a very private vit b deficiency protocol.
The co factors are so important.
They use oils there too.
Some severe cases have been reversed.
I can’t afford the protocol sadly
I forgot to add this to my prior post. In June a meta-analysis of studies was published linking ME/CFS to HHV6.
Human herpesvirus 6 infection and risk of Chronic fatigue syndrome: a systematic review and meta-analysis
https://pubmed.ncbi.nlm.nih.gov/34348314/
Thank you, Cort. Concerning the “Next up in the Mitochondrial Enhancers series – alpha lipoic acid” – I would recommend/urge you to include the warning about taking alpha lipoic acid if you still have mercury fillings, as it is a heavy metal chelator and can stir up/redistribute the mercury (as can cilantro, chlorella, etc). I know of folks who had serious reactions to alpha lipoic acid (initially not obvious). Dr. Andrew Cutler’s research on the use of alpha lipoic acid is very thorough. It requires a long and disciplined approach over a period of time (very specific protocols must be followed) and only after all mercury is removed, but better to be aware than take the ostrich head in the sand approach. Just concerned as I see so many online health professionals recommending this supplement without including the warnings. Thanks
Thanks – one thing I’ve learned doing this series is how tricky supplements can be. They’re not all as innocuous as I once thought.
I have had borderline low / low Mg levels per blood tests as far back as my records go.
No amount of supplementation, in whatever compound or form (liquid, transdermal, pills) nor diet high in magnesium has moved the needle. Same thing happened with iron.
Epsom salts do something, might be the sulfate, might be both. Not enough to move the needle.
My taurine was very low in a blood test and supplementing it raised all my minerals in subsequent tests – without me supplementing minerals at all.
Same with thiamine.
A hypothyroid state presents with low magnesium.
Taurine has something to do with the regulation of calcium (and other minerals). It doesn’t mean it will have this effect on everyone per se, I was very low on it. Some test too high in it, etc.
I no longer need it.
I find that working on my metabolism and thyroid, getting out of the stress response, and balancing hormones
All is contributing to minerals and vitamins distributing properly now. I drink copious amounts of milk (never in my life, not even as a baby 🙂 ). The calcium is key.
Naviaux latest paper, where they injected rodents with ATP, they observed how this affects the distribution of some of the Bs (inside/outside cells, though at one point I start to wonder about the use of these terms, what it really reflects). I can’t recall what it had on minerals.
The last post on the intracellular calcium and sodium – Gerald Pollack at Washington University has been studying this. His work is very relevant to understanding how this affects energy and our health problems.
I think it may do away with some of the ‘paradoxes’. He started out with muscle research, so very relevant.
He has a few lectures and presentations for those wanting to get a quick overview (or limited by energy).
ME/CFS researchers take note!
Carmen! Wirth! Davis! Naviaux! Janet Dafoe!
Legit science. Waiting to connect with you 🙂
https://www.pollacklab.org/
I wonder about the calcium. Both Dean and Levy warn about high levels of calcium. In fact, Dean wrote a whole book on it. Some calcium is needed but too much calcium, if I have it right, will actually deplete the cells of magnesium.
Maybe too much calcium for you?
Hmmm… There was very little calcium in my diet until recently.
When calcium is low in the diet, it can be pulled from the bones to maintain it in circulation. So a calcium blood test alone doesn’t say much. You need to look at parathyroid, D, K, E. 24-hour urine tests for minerals I have found helpful too, to look at in conjunction with the blood tests.
Many in the FMS/hEDS/ME/CFS communities tend to have osteopenia/osteoporosis at a much younger age than normal.
I don’t recall it being formally studied/observed in ME/CFS.
Sodium borderline low in tests, sometimes low, and yet even a few grains of salt – it would crash me. Hard and fast and bad.
Now that I have more energy, I am also able salt my food.
My renin was towards high within the normal range, while aldosterone was towards low. I think this stands in contrast with what Carmen found, per your most recent post on her research.
My experience has been that as I have improved my energetic state, minerals and vitamins distribute themselves more as they should, inside/outside cells. Milk was key. It fried my nerves the first time I tried; it also calmed my heart for 24 hours. I then learned to titrate my foods the same way I titrate my supplements. Low and slow. I’m also able to get my nutrients from diet alone.
Long ago when CFS was being called “yuppie flu” my D.O. doc was investigating what might be wrong with me. All “regular” blood tests showed nothing wrong. He decided to test my RBC magnesium. It registered at such a low level he was sure it was an error. Retested and it was the same. Said, “This can’t be true. You’d be dead!” I told him I had been telling him that’s just how I felt! He started me on SloMag and it took TWO years for my level to come into the normal range. Don’t know if the tests were ever accurate, but it was then the only abnormal level I ever had. He also had me take antioxidants (good for any illness) and complex B vitamins, saying B’s and magnesium are involved in almost all body chemical interactions. Many years later, I discovered the MTHFR allele and started on activated B vitamins which made a huge difference. Have continued the magnesium always. Daughter got CFS when more research was available, but we started ASAP on magnesium and antioxidants. Same doctor ordered “new testing” that showed about zero level of antioxidants even though she was taking various ones regularly. After many kinds of magnesium she settled on magnesium malate as best for her. Never deletes it from her regimen. I live within my envelope after 10 years disability. She’s been sick for over 25 years. Has tried so many more things than I did, but she got the double whammy genes from me and her dad.
Two years! Thanks for relaying your and your daughter’s story. I think we should all take note that different kinds of magnesium really do work better for some of us.
i certenly do not say ME is major depression but could need some help. long time ago i found this on pub med. the magnesium glycinate I could easyly buy. But the magnesium taurinate not. can anyone help? I found magnesium and taurine but not magnesium taurinate. https://pubmed.ncbi.nlm.nih.gov/16542786/
also pubmed is a wealth on information regarding magnesium, 2 excamples:
https://pubmed.ncbi.nlm.nih.gov/?term=magnesium+glycinaat
https://pubmed.ncbi.nlm.nih.gov/?term=magnesium+citraat
and you can go on and on
but it is difficult if you want to buy some sort because some disclaim that for excample that one type works slower, is slower absorbed, but then restored in the boddy, a buil up.
i have searching so many times on magnesium but because severelly ill, had to start over and over again.
ps in fact, one must be a chemestrist, nutritionist to know it all
This is a fantastic analysis and summary, Cort! Thanks so much. I’m always confused about how to get enough of each of Ca, Mg, and Vit D (and learned a couple of years ago that you have to take Vitamin K to help the absorption of Vitamin D!) and how they block or complement each other.
It is especially difficult to navigate when you take medications, such as certain thyroid meds, the effectiveness of which is reduced by minerals.
This is really helpful.
Magnesium bioavailability
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6683096/
That was really helpful, thanks for posting the link. I am from the UK and have just spent an hour searching out a suitable supplement and found one on Amazon. One capsule supplies 200 mg elemental magnesium from 4 different sources.
So the recommended daily amount would be just 2 capsules.
Can you provide a link to that?
Yes, PamC– Would greatly appreciate the link or or name of the supplement you found that supplies the 200mg of elemental magnesium.
With thanks in advance.
Hi Cort and Jane
Here is the link to the one that I think is probably best value and seems to contain what we need without having to take endless capsules/tablets –
https://www.amazon.co.uk/gp/product/B07PT8N8GP/ref=ppx_yo_dt_b_asin_title_o00_s00?ie=UTF8
I was given Ancient Formulas COR-MUSCLE years ago which has consistently kept muscle pain at bay. Combines Magnesium Gluconate 50 mg, Bioenergy Ribose 6.2 gr, and Malic Acid 298 mg. It mixes in water. I have Myofascial Pain Syndrome where knots form all through a muscle as a result of not enough energy available to decontract.. This supplement has allowed that to resolve.
Consumer lab found that ReMag was contaminated with lead. A small amount, but above acceptable level according to state of California. Just FYI.
One other thing I wanted to add which is slightly off topic is that due to poor motility issues I am still going to have to take between 500 – 1000mg mag citrate daily along with Triphala so I will possibly have to cut down to one of the new capsules containing 200 mg elemental magnesium so as not to overdose on magnesium?
I would guess I am not alone in having to juggle with the types of magnesium needed.
Hi Pam,
I would agree that it’s a good idea to cut down and probably consult a nutritionist or someone similar.
One thing to keep in mind is that most of the other forms of magnesium, even the ones advertised as easy on the gut, can still increase motility. So you may be able to cut down on citrate without sacrificing too much motility benefit.
Also, have you ever considered Pyridostigmine Bromide (Mestinon)? I got mine prescribed for POTS, but it’s being used for ME-only patients as well. It’s not a cure but can dramatically improve some ME symptoms. I mention this because it’s main side effect is hypermotility, which may be extremely helpful in you’re case. Maybe kill a handful of birds with one stone?
Mestinon can be very helpful for some! We have a great story on Health Rising on that.
Courtney Craig would be a great choice for a nutritionist I think – she’s steeped in ME/CFS and does consultations.
I think it might be a bit more complicated than originally thought regarding magnesium citrate and the amount of elemental magnesium in any capsule/tablet. I have checked with Biocare, a well know UK company offering supplements of excellent quality and they quote 100 mg elemental magnesium per 100 mg capsule.
Also I emailed Nature Best, another well know UK company regarding their MagAbsorb magnesium citrate tablet and I got this reply today – “We label all our minerals with the elemental levels rather than compound weights. Therefore Magasorb Ultra provides 150mg of elemental magnesium as citrate”.
Yet another company who advertises on Amazon uk site quotes 150 mg elemental magnesium per 500 mg capsule.
So to sum up, as far as I can see it is far from easy to work out how much elemental magnesium one is getting from a supplement of magnesium citrate!
Just be careful for folks who tend toward low blood pressure. I can supplement with a small amount of magnesium (and I get quite a bit through diet), but I’ve tried a zillion types of magnesium forms and it can easily drop my b.p. somewhat and make me feel icky.
It can certainly drop blood pressure. Thanks for the warning.
iHerb.com has almost all Mag supplements mentioned in the article ( from different manufacturers) I find it the best “Amazon for supplements”.
The best site for independent advice on supplements is examine.com – amazing database
Hope this helps