SUNY University at Buffalo immunologists believe metabolic dysfunction were causing the exercise intolerance they were seeing in their fibromyalgia patients. (Image by SkieTheAce from Pixabay )
This unusual paper “Investigating Fatigue and Exercise Intolerance in a University Immunology Clinic” is the outcome of 20 years’ work (1998-2019) at the SUNY University immunology clinic in Buffalo, New York by the primary care doctors, rheumatologists, and others trying to figure out what was causing the “life-altering fatigue and exercise intolerance” they’d found in some of their patients.
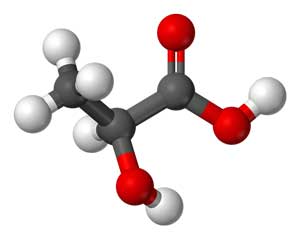
After normal laboratory tests failed to provide an explanation for the mysterious exercise intolerance, they turned – noting that the most common symptoms of a metabolic disorder are fatigue and exercise intolerance – to tests for metabolic disorders. (They also noted that other symptoms commonly found in their patients (heat intolerance, difficulty with some medications, recurrent infections, gut motility problems, and accelerated osteoarthritis) also frequently show up in metabolic disorders.) They focused on metabolism because metabolic processes produce the adenosine triphosphate (ATP) used to power our cells.
The Gist
- Immunologists at SUNY University at Buffalo have been digging into metabolic abnormalities in over 300 patients with mysterious problems with exercise intolerance and fatigue for over 20 years.
- Over eighty percent of the patients in the study were diagnosed with fibromyalgia.
- The study “Investigating Fatigue and Exercise Intolerance in a University Immunology Clinic” used lactic acid blood tests, ischemic forearm tests, muscle biopsy, biochemical tests, and genetic tests to determine if metabolic dysfunctions were present.
- The study reported that the testing provided a ‘treatable diagnosis” for 95% of those in the study.
- High lactate and/or CPK levels, muscle atrophy, abnormalities mitochondrial respiratory chain function, low carnitine palmitoyl transferase activity, and abnormalities in an enzyme in the glycogen storage pathway were common.
- The authors matched the metabolic dysfunctions found with rather simple treatment protocols involving mitochondrial enhancers and/or different diets. Dosing was not provided. They reported that many patients received “life-altering” responses. Those responses, however, were not quantified.
- The treatment response was not the big news from the study. Aside from the fact that dosing and treatment responses were not quantified, more and better treatment options now exist.
- The big news from the study concerned the widespread metabolic dysfunctions found which could conceivably be contributing to or causing the mysterious exercise intolerance and fatigue found.
- The authors pointed out that metabolic dysfunctions can be hidden until other stressors arise, that they can arise in middle age and they’re being investigated in more and more diseases.
The Patients
Many of the 372 patients included in this overview, they noted, had been sent to psychiatrists prior to seeing them.
Strangely enough, chronic fatigue syndrome (ME/CFS) is mentioned only once in this paper (to point out it may be a metabolic disorder) and is not included in the diagnostic section. This is probably not unusual and probably just reflects the diagnostic thrust the doctors at this University have taken. When confronted with a patient with fatigue, pain, and exercise intolerance they usually diagnose her/him with fibromyalgia (FM). (Over 80% of the patients in this overview had been diagnosed with FM.) With their high rates of gut problems and migraine they looked very much like ME/CFS/FM. That no instances of orthostatic intolerance were noted probably reflects the doctor’s focus on FM; orthostatic has only recently begun to be assessed in FM.
Diagnoses
The patients in the study had been diagnosed with a variety of conditions:
- Fibromyalgia – 81%
- Gut motility and IBS problems (gastroesophageal reflux, gastroparesis, nausea, vomiting, constipation, diarrhea, pseudo-obstruction) – 73%
- Migraine – 54% (as of the patients with migraines responded to centrally acting vasodilators, the authors believed they probably had reversible central nervous system vasospasm, or Raynaud’s of the brain
- Food hypersensitivities – 45%
- Recurrent infections – 44%
- Raynaud’s Disease – 37%
- Asthma – 17%
- Accelerated osteoarthritis (possibly due to poor muscle function supporting the joints)- 15%
- Anti-phospholipid antibodies – 15%
- Sjogren’s syndrome – 14%
- Depression – 11%
- Inflammatory arthritis – 10%
- Peripheral neuropathy – 6%
- Dyspnea – 5%
Tests
All the patients were given complete blood counts, comprehensive metabolic profiles, urinalysis, carnitine, TSH, free T4, CPK, ammonia, lactic acid blood test, and, in most cases, an ischemic forearm test.
Ischemic Forearm Test
They used an ischemic forearm test to assess changes in lactic acid and ammonia during exercise. (The test stresses one’s ability to produce energy using anaerobic metabolism).
Lactic Acid Blood Test Interpretation
- Normal lactic acid levels – lactic acid and ammonia rise 3-4 times the baseline levels.
- Failure of lactic acid to rise – glycogen storage disease
- Failure of ammonia to rise appropriately – a myoadenylate deaminase deficiency or a disorder of the urea acid cycle
- Elevated lactic acid test at rest on more than one occasion – increased reliance on glycolytic metabolism, suggestive of a mitochondrial disorder [30].
Muscle biopsy
Muscle biopsies were done in patients with normal or confusing lab findings, patients who failed to respond to treatments, and/ or patients who just wanted to search further.
The muscle biopsies assessed the levels of a wide variety of compounds (carnitine palmitoyl transferase, myoadenylate deaminase, phosphorylase, phosphorylase b kinase, phosphofructokinase, phosphoglycerate kinase, phosphoglycerate mutase, lactate dehydrogenase, acid and neural maltase, NADH dehydrogenase, NADH cytochrome c reductase, succinate dehydrogenase, succinate cytochrome c reductase, cytochrome c oxidase and citrate synthase.)
Biochemical Studies
Biochemical studies were done in most patients. They included: carnitine palmitoyl transferase, myoadenylate deaminase, phosphorylase, phosphorylase b kinase, phosphofructokinase, phosphoglycerate kinase, phosphoglycerate mutase, lactate dehydrogenase, acid and neural maltase, NADH dehydrogenase, NADH cytochrome c reductase, succinate dehydrogenase, succinate cytochrome c reductase, cytochrome c oxidase and citrate synthase from freshly obtained muscle biopsies. In some patients CoQ10 levels were also assessed.
Whole-exome/mitochondrial DNA sequencing
Genetic studies (whole exome/mitochondrial DNA sequencing) were done in 83 patients.
Results
Ischemic Forearm and blood lactic acid tests:
- Forty-six percent of the participants had an elevated lactic acid at rest. Forty-seven percent had an elevated CPK at rest.
- Ischemic Forearm Tests about half (48%) of the participants had an abnormal result during the ischemic forearm test.
- Ninety of the 123 patients with abnormal ischemic forearm tests had findings that allowed a treatment strategy to be initiated.
- Serum carnitine was low in only 17 patients (5%).
Muscle Biopsy Findings
Lactate levels were increased in about half the patients at rest and after exercise.
Few people had normal biopsy findings (11%) with muscle fiber atrophy commonly found (67%). Besides inflammatory myositis found in 11%, other abnormalities were rare (ragged red fibers or abnormal mitochondria on EM (4%), inclusion body myositis (3 patients), abnormal lipid deposition (1 patient), abnormal glycogen deposition (1 patient), and vasculitis (2 patients).
Mitochondrial Respiratory Chain Activity
The complexes refer to the different parts of the mitochondrial respiratory chain where aerobic energy is produced. Complex 1 and complex 3 activity was dramatically reduced in 33% and 22% of patients respectively.
- Complex 1 activity <70% – 71/216 (33%)
- Complex 1 activity <50% – 10/216 (5%)
- Complex 2 activity <70% – 15/216 (7%)
- Complex 2 activity <50% – 1/216 (0.5%)
- Complex 3 activity <70% – 48/216 (22%)
- Complex 3 activity <50% – 13/216 (6%)
- Complex 4 activity <70% – 16/216 (7%)
- Complex 4 activity <50% – 5/216 (2%)
Biochemical Study Results
CoQ10 activity was reduced in 22% of patients. Carnitine palmitoyl transferase activity was down <65% in 32% and LDH activity was <20% in 27% of the 216 patients tested.
Genetic Tests
Of the 83 patients given genetic tests, 17% had a glycogen storage disease of some type (Pompe, McArdle’s and Tarui disease, types IX, XIII).
Deep Dive into Metabolics Provides “Treatable Diagnosis” for Many

The metabolic tests provided 95% of the patients with unexplained fatigue and exercise intolerance with a “treatable diagnosis”
No studies have dug as deeply into mitochondrial and energy production issues as this study. The authors reported that the deep dive worked provided 95% of patients with a “treatable diagnosis”. Providing 58% of the treatable diagnoses, the biochemical studies were the most revealing followed by the genetic (21%) and laboratory (20%) studies.
The treatable diagnoses included
- abnormalities of a mitochondrial respiratory chain function (168 patients)
- abnormalities of an enzyme in the glycogen storage pathway (78 patients)
- low carnitine palmitoyl transferase activity (70 patients)
- defects in other mitochondrial proteins (12 patients)
- mutations in proteins associated with congenital myopathies (11 patients)
- mitochondrial depletion syndromes (8 patients)
- abnormal myoadenylate deaminase (7 patients)
Treatments
It should be noted that because other treatments to address things like sleep apnea, food hypersensitivities, and Raynaud’s were provided, all the improvements may not have been the result of the metabolic treatments. (The doctor clearly believed they were essential).
One of the great questions regarding enhancing mitochondrial activity involves targeting the specific energy production problems found with the right treatments. Different treatments were employed depending on which abnormalities were found. Doses, unfortunately, were not given.
Treatments For The Metabolic Conditions Found
Mitochondrial dysfunction or mitochondrial respiratory chain disorders – people with these issues were treated using a fairly standard mix of energy enhancing and antioxidant boosting supplements
- CoQ10 – transports electrons between complex 1 and III
- Carnitine – imports fatty acids into the mitochondria
- Alpha-lipoic acid (ALA) – strong antioxidant
- Creatine – generates ATP via the creatine phosphate shuttle
Low carnitine palmitoyl transferase activity – diets minimizing long-chain fatty acids. (Long-chain fatty acids are found in most fats and oils, including olive oil, soybean oil, fish, nuts, avocado, and meat.
Glycogen storage problems – diets that restricting complex carbohydrates with larger amounts of simple sugars
Low lactate dehydrogenase activity – provided treatments for mitochondrial dysfunction (because of the influence of lactic acid on mitochondrial functions)
Myoadenylate deaminase deficiency – D-ribose plus the mitochondrial supplement treatments
Treatment Results
The authors reported that while improvements in treatments for metabolic disorders are clearly needed that the treatments were “life-altering for many of these patients”. That, unfortunately, was the end of the story.
We don’t know what “life-altering” means (10%, 20% more functionality? 50%???) nor were any statistical analyses done. We simply know that the doctors considered the treatments “life-altering for many of (their) patients.”
Conclusions

The authors reported that the treatments produced “life-altering results” for many but did not define “life-altering” (Image by SkieTheAce from Pixabay)
This rather astonishing paper contains thirty years of work documenting the metabolic results in around 300 patients with a fibromyalgia/chronic fatigue syndrome-like diagnosis. We’ve never seen anything like it. Unbeknownst to us, doctors at a University Immunology center in New York have been working away for decades on a topic – metabolic disorders – that’s only now getting much attention in the fibromyalgia / ME/CFS world.
With their forearm test, their muscle biopsies, and their biochemical and genetic analyses this University group tried harder than any medical group I’ve seen to try to metabolically explain the strange exercise intolerance found. In fact, given that exercise intolerance implies problems producing energy exist it seems strange that we haven’t seen these kinds of analyses more often.
Many abnormalities were found with particularly high rates of increased lactic acid levels at rest or after the ischemic forearm test (%50), CPK levels at rest (47%), and muscle atrophy (67%).
Other common diagnoses included: reduced Complex 1 activity (33%), reduced carnitine palmitoyl transferase activity (32%), reduced LDH activity (27%). reduced complex 3 activity (22% ), reduced CoQ10 level (22%), glycogen storage problem (17%).
The treatments were simple, dosing was not provided, no control groups were present and treatment effects weren’t quantified.; i.e. the treatment news wasn’t the highlight of this study. Better treatments are available. Health Rising’s Mitochondrial Enhancing Series, for instance, is not nearly done and it’s already covered some potential mitochondrial enhancers they didn’t use.
The Mitochondrial Enhancers for Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia Series
- Pt I: D-Ribose, CoQ10 and PQQ
- Pt II: L-carnitine and Acetylcarnitine
- Pt. III: Magnesium
- Pt IV: N-acetyl cysteine (NAC)
- Pt V: Oxaloacetate
Plus, new and better forms of CoQ10, as well as “new” supplements like oxaloacetate, are showing up. Since defective mitochondria are often inflammatory mitochondria that further impair mitochondrial production, more effective antioxidants (new forms of NAC, glutathione, cysteamine, hydrogen sulfide donors, and intranasal preparation for the brain) and antioxidant protocols promise more help for these problems.
The big news from this study was the high degree of metabolic dysfunction found. The authors noted that metabolic disorders are greatly underdiagnosed and that many people who unknowingly have them have found their way around by altering their activities. People with inherited metabolic disorders typically avoid competitive sports; people with glycogen storage diseases often learned to avoid complex carbohydrates. It’s only when other stressors such as infections (which cause post-infectious illnesses) is it clear that something has gone really wrong.
These metabolic disorders can have surprising downstream effects. Metabolic problems with immune cells, they report, can result in recurrent and long-lived infections which then further impair gut functioning, causing food hypersensitivities and increasing the risk of autoimmunity. Metabolic disorders can affect blood vessel functioning – possibly a very big deal in ME/CFS/FM and long COVID – by reducing the production of such important vasodilators like nitric oxide. Mitochondrial problems are being investigated in many neurological diseases including Parkinson’s Disease, multiple sclerosis, and migraine.

Metabolic abnormalities are getting more and more attention over time. Could they hold the key to ME/CFS?
Plus, in a statement that has potentially important implications for ME/CFS, FM, and long COVID, the authors report that it’s become clearer over time that many metabolic disorders can pop up as a result of another disease or stressor. People with hypoxia-producing diseases, for instance, can develop secondary mitochondrial dysfunction as a result of oxygen deprivation. People with sepsis can develop “multiple secondary metabolic disorders”. Chronic inflammation can damage the mitochondria where the inflammation is occurring.
The fact that the paper didn’t come close to meeting rigorous standards of academic scholarship shouldn’t be a surprise. This was an apparently unfunded effort by a group of researchers and doctors to get the word out and inspire others to investigate these diagnoses, treat them, and inspire more rigorous studies. While this study is clearly not the answer to the question of how important metabolic disorders are in ME/CFS/FM – we need studies with better methodologies – it’s hopefully a stepping stone to those studies.
One such study is underway. Dr. Camille Birch found rare mutations that could be affecting the energy metabolism in five out of ten ME/CFS patients. Among other things, several of those mutations could be producing glycogen storage issues similar to those reported in this study. Aided by a Ramsay Award from Solve ME Birch is taking a deep dive into genetically produced metabolic dysfunctions in ME/CFS – some of which might not be manifested until middle age or until other stressors appear.






Those treatment options are a slap in the face for everyone with this disease. Might as well tell them to just breath and hope for the best. This is 50 year old wisdom to try some Q10, Carnitine and some fatty acids. More money wasted on useless stuff that gets repeated again and again to get some undergrad student and profs some reputation. There is nothing in it for the patients, us.
I agree that if you were looking for new treatment options you may not have found them – although I imagine that not everyone has tried them.
As the blog noted better treatments are now available, and if metabolic dysfunctions are as common as this study found – which was the real story of this study for me – it could provide a real opening for new and better treatment options that were not present in this study. Personally, this study makes me think I should dig deeper into all the different energy-producing options that are available.
At the very least this study cries out for much more study into energy metabolism – and that potentially is a big deal for fibromyalgia and ME/CFS.
Agree.
I would immediatly if possible let do all this tests! Even if it might be (only) a part of ME. Or exclusionary…
I wished they do it here in my country. A pitty they said no more of the treatments.
I had long time ago allready extreme severe periferal and respiratory weakness findings but no explanation. it only went worse. trouble speaking, breathing, etc
i orderded the Oxaloacetate as fast as i could to try together(must i still order-i can not do much) , but one after the other with a bunch of stuff imidiatly.
If it only helps for 1 or 2%, i already would be glad in my situation!
but what i did not understood, ordering it (with the 3000 mg a day) was that kaufman used the jubilance with less Oxaloacetate (100mg) and i thought 150mg vitamine C per pill,. and that benagene had the same (Oxaloacetate and vitamine C), but i see it now no more on there website also pure higher Oxaloacetate claimed for cfs.
but my main point is, i wished someone excamined me so well as in this study! And maybe not only metabolic…
Cort, because you have mentioned that your ME/CFS had a gradual onset (vs trigfered by an infection)
And because its course has not devolved into a severe severe state,
I am curious:
– have you ever tried thryoid?
A tiny bit of T3, just to see how you respond?
As far as mitochondrial energy production, I and others, have had significant improvement in our ME/CFS fatigue, by taking high-dose Thiamine, (Vitamin B-1). I am still experimenting with the dosage. The fact that this treatment purportedly works upon the theory of making one’s mitochondria release energy.
By this same reasoning, it would not seem a given that the pain of ME/CFS would get better.
That is my experience. The flu-like malaise and lack of energy to muster up any enthusiasm about anything, is significantly better. The pain is the same. At least I have two kinds of opioids to help the pain. The constant sickness and exhaustion are the worst parts and there was nothing that helped that.
I am interested in trying the additional supplements, listed in this study
Someone seeing Ambrus (lead author) emailed and said that Ambrus is trying other supplements and mentioned one I’d never heard of – so he is clearly doing more than those mentioned in this study.
Thanks, Meirav,
I did extensive thyroid testing with a specialist early in my illness and tried thyroid. Unfortunately, it had no effect. Haven’t had it tested in a long time, though.
Cort, what is that supplement that you’d never heard of, from the patient seeing Ambrus?
I have had ME/CFS for 35 years…and I agree. This article will not give any step by step instructions on how to deal with the disease. Hovever, it could help link important parts of the puzzle together. FOR EXAMPLE, I found out many years ago that the quitting eating was the most beneficial thing I could do for ME/CFS. I had often fasted for religious reasons and whenever I went without food for 3 or more days I felt great. Recently I have found great benefits in the keto diet. This suggests to me that there is a very real potential that GLYCOGEN STORAGE is a potentailly a major issue. I am going to try going back on the Keto diet.
Yep, totally agree.
I was homebound with Fibroamazing. (Now commonly called post-viral syndrome) for 9 years. My mom felt so bad for me she suggested I get a 2nd opinion with her Rheumatologist even though my own has been amazing. This new Dr didn’t know my history like my current Dr but she did run extensive labs which revealed I may have hyperparathyroidism. I consulted an Endocrinologist and long story short, in late 2019, I had 2 parathyroid tumors removed and my fibro pain went away immediately.
I had a hard time bouncing back from the surgery so my Rheumatologist suggested I take NAC. It was life changing. I was in the middle of packing up to sell my house to move to a more temperate climate. Between the surgery and NAC, I developed incredible stamina and completed my move while losing 30 pounds. Another fast forward to current day, while I still have to take Valacyclovir to keep the Epstein-Barr Virus quiet, as well as SQIG for CVID (that diagnosis and subsequent IgG therapy has completed my recovery), I am now pain free and work out at the gym and swim 3 days a week as well as I walk 4 miles on non-gym days and I am an avid hiker with no PEM. I’ve also lost another 50 pounds.
I still take the NAC every day and am dairy and gluten free and eat primarily a whole foods organic vegetarian diet, (I will eat organic non-GMO chicken and eggs from a local farmer) very thankful for my farmer’s market and it’s organic produce. I urge everyone to get tested for hyperparathyroidism because I have my life back!
Note that this is not a research study but a case report — i.e. a doctor who has been attempting to diagnose and treat patients is publishing what he has come across and done; note that there are no sources of funding – patients and their insurers presumably paid to attend the clinic.
As a case report, it is quite detailed and analytic and provides ample leads for researchers to seize and follow up on. From my experience, we need more MDs like this who are trying to understand the root causes of disease and who are publishing information on what they have seen and done in order to better bridge the gap between clinical practice and research.
Amen to that!
What was interesting though is that is said to MINIMISE fatty acids. This is opposite to all the advice I’ve been given. Could be interesting ?
Couldn’t agree more.
Rudi: I don’t see anything written here that says that just taking random supplements is going to cure you. The fact that all of these treatments have shown incredible results for a few people once in a while and usually not for others just speaks to the importance of getting good diagnostics and identifying the issue before treatment. Is it surprising that the wrong thing for the wrong issue in the wrong dose doesn’t work well? Very few ME/CFS patients will ever get a proper Inborn Error of Metabolism workup and without that, you’re likely to run out of money and time long before you accidentally stumble on a treatment that helps. Moreover, with some of these illnesses the treatments are highly specific and require certain forms or cofactors. So lets say a patient has a B-vitamin pathway issue and they tried B-vitamins, but did they try 100 times the dose in a specific form with a specific co-factor for 6 months? There are metabolic disorders that require that kind of specificity or medically produced substances that aren’t available over the counter.
I did the twenty three and me testing, and I personally show a bit of mitochondrial dysfunction, and I do respond to some of these supplements. I do better with acetyl carnitine, coq10, and ribose. Some people do not, but perhaps I respond since i show some abnormality. I think it the tests were more specific, and we each knew what we needed it may make a difference to help people with CFS function better.
How incredible the numbers diagnosed with disorders.
Is there any group currently accepting people to have these unusual diseases uncovered?
what kind of cost would it be for a patient group to develop some sort of co-op where ordering large numbers of tests might give some sort of discounted rate to have these done– and hopefully if a large enough group, some researchers might add $$ to the pot for the opportunity to mine the data–especially if it became a huge co-op?
I agree with Sunie. Is staggering how many rare disorders were diagnosed.
It suggests that ME patients and the population as a whole are currently seriously underserved by existing medical diagnostic services. If doctors don’t find something on the standard labs, too often patients are relegated to the psychological basket. It’s lazy medicine and dangerous.
I also think this research very much leaves the door open for different explanations of severe illness caused by things like metabolic trap, etc. Am certain that genetic weak points stack up like dominoes just waiting for a trigger to start the cascade. As Rudi pointed out, treatment and cure can be very complicated. And is the metabolic shutdown caused by genetic defects or is it mediated by the immune or the nervous systems?
I found that the symptoms list for metabolic disorders read like a checklist for my own health problems and some of them I have had since infancy, particularly recurrent infections, asthma and allergies. Gut problems amplified in my teens. ME came in my late teens. New problems have materialized every decade since.
Interestingly after sudden onset of severe reflux I recently changed my diet to a dairy free, heavy fruit and vegetable diet and I am surprised by how much better my energy is. Following this blog will look into issues with glycogen storage. Going dairy free has massively helped the reflux but it seems to be the fruit that is helping my digestion and energy. Fruit has been a bit vilified in recent times due to the fructose but I find it gentle. I tried a paleo diet once and it just made me worse so I guess it goes to show we are all unique.
I would jump on that one!
I know I have high lactic acid in my blood not from any diagnostic test but from the mosquitoes that love to bite me the moment I step out while everyone around me is untouched. They love sweet blood indeed!
This is a diagnostic study with a poorly described patient cohort which in a few patients comes up with a distinct diagnosis of a indeed treatable entity (which is the interesting part). In the vast majority of cases however, they find some form of mitochondrial dysfunction, which they also call „treatable“ – not because they have observed successful treatment but because they obviously believe that some supplementation may help. Yet, this is up to debate: secondary mitochondrial dysfunctions as seen in many disorders with inflammatory stimulation and/or misery perfusion (ME/CFS and FM are typical in this group) plausibly may only be treatable by treating the underlying pathology. For me this study is full of overstatements.
Very odd paper. I think it presents a distorted picture. 372 patients over 20 years averages out to about 19 patients per year. I would wonder how many of these patients were even correctly diagnosed with PEM or fibromyalgia. How could sleep disturbance and all of it’s likely effects on metabolism not be part of the picture and discussion? Just don’t know what to make of it.
I suspect they nailed the exercise intolerance part…how many doctors even know of that? If they know of it I assume they got it right. This is clearly a fibromyalgia-oriented group, though, and in that way it’s distorted. I was surprised that they only mentioned ME/CFS once and did not include it in their list of diagnosed diseases. They may not have included sleep disorders in their comorbid disease diagnoses section because people with ME/CFS don’t tend to have a diagnoseable sleep disorder.
Don’t tend to have a diagnosable sleep disorder?
What do you mean Cort?
I had 2 sleep tests and both concluded: mixed apnea’s, major amount of micro-awakenings (which I’m not aware of), severe alpha-delta sleep intrusions, flattened breathing (only seen in obese healthy people, I’m slender).
In other words:
-my brain remains too active during sleep (nervous system issue?) and I don’t get enough oxygen.
-Then there is reversed circadian rhythm too.
-Without sleep meds I almost get no sleep at all (1,5hrs).
I know many ME patients with the same sleep issues.
These issues are objectively measurable when visiting a sleep clinic.
I salute the doctors who ignored the groupthink on fatigue which has so long condemned it to the psychological basket. They have demonstrated that currently available science can diagnose and treat many patients with fatigue, thereby putting to shame the majority of doctors who just dismiss us.
However many different subgroups potentially means lots of treatment trials will be needed for relatively smaller patient groups. This will be expensive and take time. Just have to hope that the rewards look promising enough for pharmaceutical companies to get involved and push treatments forward.
You hit the nail on the head! I learned in 2012 that I have Lyme and co-infections, but the gene issues were all there, as I could not even run half court girls basketball in high school without problems. Thankful for the very wise functional medicine MD who ran testing to learn that I had mitochondrial dysfunction in 2014. ATP Fuel, d-ribose, COQ10 and other supplements are my mainstay. Even now, I will take d-ribose before physical therapy for my arthritic knee, and then later in the day I will take another dose just to avoid the buildup of lactic acid and the muscle pain that results. My grandmother suffered from Parkinson’s and one of her son’s died at the age of 3 from a muscular disorder.
May I ask who your Functionzl medicine physician was, and do you know what the testing was for mitochondrial function? I take Q10 and L carnitine daily, but would also like to know the ATP product you are taking if you don’t mind me asking. I see you also take D-Ribose. I am going to add that to my list.
I take ATP fuel by Researched Nutritionals…it was developed by Garth Nicolson, good product, and it does help me.
Any research on the role of glutathione supplementation in the treatment of these types of metabolic anomalies?
Isn’t this something!
That a number of them had identifiable disorders.
This has been my fight, that before a doctor arrives at the basketcase diagnoses of FMS, hEDS, HSD, and ME/CFS, they should practice due-dilligence and rule out/in identifiable conditions.
I have learned that some are misdiagnosed with hypophosphatasia or one of the homocystinurias.
I myself have a clinical history from childhood and a set of symptoms that are not seen in ME/CFS, and are more properly aligned with congenital adrenal hyperplasia [CAH]. Then I have a set of symptoms that are not seen in CAH, and more properly align with ME/CFS.
There is no djfferential diagnosis for CAH. My genes are pointing to CAH a little ambigously. My testing is not. That same testing also has certain pecularities that are the opposite from what has been reported in ME/CFS.
And while every member of my family has a touch of the ME/CFS hypothyroidism hEDS, etc, I’m the one worse off. And they also don’t present with the clinical history particular to CAH like I do – may this be why I’m the most affected/disabled?
I also learned that in chronic kidney disease, fatigue is a major component. And one person referred to it as his ME/CFS part of the disease. I read a recent metabolomics on CKD: there were very similar findings as to ME/CFS ones (PDH inhibition, etc).
I have been thinking lately that there are various roads to severe ME/CFS.
And what underlies them all is a severe hypothyroid state. It may come from the pituitary (this is not picked up by regular blood tests. You need a TRH test that is now days ‘obscure’).
What a refreshing paper, doctors that dug deeper!
Top doctors now use a new test, 24 hour urine test, to diagnose hypothyroidism to avoid the severe shortfall of the “immaculate “ TSH test.
That’s very interesting to know. I’ve been treated, rather unsuccessfully, for Hashimoto’s for decades by throwing different kinds of thyroid supplements at it and seeing what happens. The Hashimoto’s antibodies don’t dependably reveal themselves in every blood test, but doctors have told me that once you have a test showing them, you don’t need another for a diagnosis.
Does the 24-hour urine test have any better treatment implications?
I guess 24-hour urine is old-school, before the advent of blood tests.
You can track heart rate and temperature through out the day to assess thyroid function. Better than them tests.
I think the best way to measure metabolic rate is to measure O2 consumption /CO2 production.
If the recommendation is avoiding diets rich in olive oil, fish, nuts, and meat, then this is exactly opposite to what was recommended by my ME specialist and also the dietician at the Complex Chronic Disease Program at Vancouver General Hospital. So instead of clarifying matters this only increases confusion.
I’m afraid that’s only natural. What else, really, was likely to happen when someone did a bunch of tests that few of us have done? Anything like that is going to provide new perspectives on things. I suspect, though, that dietary change would only apply to a few people.
Excepting the concentration on possible metabolic underpinnings of fatigue, I was very disappointed with this review. Sloppy.
Being in the Ehlers-Danlos camp, and knowing that some large percentage of us (80-90%) have ME/CFS like symptoms (especially fatigue) and nowhere in the review did they mention EDS.
In the beginning, I was diagnosed with fibromyalgia too, and many with EDS are as well, but oftentimes, EDS issues are NOT fibromyalgia! Many doctors are not even aware of EDS and given that it is on a spectrum, more people can have it than the often stated 1 in 500 statistic. Anyway, patients with fatigue issues self sort for studies like this. Stanford’s CFS clinic has a very large proportion of people with EDS.
I do wonder how many of their ‘fibro’ patients really had some sort of Hypermobility Spectrum Disorder instead.
As for all the improvements with various supplements and diets, I have tried just about every single one of them (not oxaloacetate yet) with little to no improvement. And just who can get all those exotic tests? Not everybody.
Makes me a tad upset for those claims of improvement as if it was so easy…
Very few doctors assess EDS. I don’t know if that means they’re sloppy or not. It may just mean that they don’t know about it. It’s very rare to see it as a diagnosis even in an ME/CFS paper. While few of us have gotten or can get these tests I think the goal of this paper was to make it easier to get them
easier to get these tests because of precident set?
or because possible larger study group of patients might be able to enroll in a future larger study by same researchers?
Chris; I too have had remission like days after not eating for 2 days.. Just water!!.. Sounds like allergy, doesn’t it? They tested me for all that and nothing came of it.. Also Colonic cleaning was very successful ( 3 ) treatments in a row.. 3 days…
Why Glycogen? I have decided for myself that when really weak and drained that food, especially pasta brings my level up of feeling better. Had this slow onset in 1950.s and came into full force after severe stress ( divorce) and Flu 1968. 60 yrs//// I can’t take it back so I just live each day hoping and doing my best!! Nila
I think EDS has been even more neglected than CFS.
As somebody who is currently undergoing a year-long SIBO treatment process, making progress as i am going along, I appreciate this study because a) these doctors cared enough, b) my experience so far would give this study validity, and c) anything that affects the gut affects the brain, including the regulation of homeostasis.
Ehlers-Danlos, Fibro, CF, my list is very long too. Has anyone looked into exocrine pancreatic insufficiency or something similar? Can it be so simple that enzymes might be an answer for some of us? I can’t tolerate olive oil and so many other things. Any studies on this?
I developed exocrine pancreatic insufficiency during a relapse over 4 years ago and I’ve been taking pancreatic enzymes since being diagnosed. My main symptom was unintended weight loss due to fat malabsorption.
I still get crashes and relapse in the winter time, so it’s not a miracle cure. But I might be worse off without it.
The research clearly shows many things are going wrong. Unfortunately, those who have tried all of the listed supplements can attest to none or no significant improvements. It is not as simple as just adding in a few key supplements to fill in the gaps of a malfunctioning system. The supplements must be utilized correctly in order to provide benefit; the problem is a malfunctioning system lacks the capacity to do that.
it would be interesting to know, out of those who have tried every flavor of help/ health supplement, what percentage have had whole exome, or whole genome, sequencing done, and what % of people showed useful results?
wonder if numbers are similar to that reported here in this study, how many received a genetically based diagnosis?
This is interesting – Cort, I’m amazed at how you find all the info you do! Thanks for posting this.
Yes, Thanks to you Cort and your complete dedication. I hope you have peace. Thank you to everyone who has good ideas and comments. You all make a difference. Some of you can critically think Whoohoo! This is the ONE place I can go to replenish because I am really sick of everyone dismissing me. Peace to you Deirdre
(…) ”This is the first study showing reduced parasympathetic reactivation during recovery from physical exercise in ME/CFS. Delayed HR recovery and/or a reduced HRV as seen in ME/CFS have been associated with poor disease prognosis, high risk for adverse cardiac events, and morbidity in other pathologies, implying that future studies should examine whether this is also the case in ME/CFS and how to safely improve HR recovery in this population”.
https://www.mdpi.com/2077-0383/10/19/4527
Cort, or someone with the knowledge, explain to me
the intricacies as to why a doctor in the States at a university hospital
is the one that is able to dig deeper
and has more leeway with testing and treatment referral ?
What about the system allows for this?
Does it have to do with health insurance policy too?
The one thing I was told by a Dr in the States
was that they get more time with a patient.
Thank you
Ooops… I ate some words:
Cort, or someone who knows – *could you* explain…
😉
I have tried nearly all of these supplements as well, and none of them helped, in fact they mostly just made me feel bad in different ways. This has always led me to believe that getting to the REASON that these metabolic issues are happening in the first place. It’s as if my body does not want to produce the energy for some reason and pushing it to through supplementation always backfires. Genetics? Maybe this is where gene therapy might help someday.. or some other underlying “reason” to be dealt with
Crystal, in my experience, my reactions to stress are the most important factor in my symptoms, though high doses of B1 and melatonin and their cofactors have helped me a lot with ME/CFS/FM, and other symptoms. The major thing that has helped me cope with stress is praying the Bible verses in Psalms 91 and 23 and other Psalms, as well as all the verses that promise divine healing. Dr. Brene Brown and Dr Bruce Lipton have written books and made podcasts on YouTube that have helped me greatly with stress reduction also. I hope that you find the help that you want
Dear Experts, This summary did not mention Clients who had been given a diagnosis of Fibromyalgia as – the diagnosis of exclusion- but who actually had Hypophosphatasia (HPP). Yes, the genetics are complicated, it is considered “rare” (when two recessive genes come together) and the presentation in infants can be simply horrendous. The adult presentation is now suggested as much, much more frequent than ever expected. HPP is just not being diagnosed with Drs considering Somatic Symptom Disorder, providing Psychosocial interventions, refusing pain medicines but also ignoring the consequence of low ALP bloods with unexplained but obvious signs such as para articular calcification/ crazy arthritis. The adult phenotype IS complex and NOT necessarily “mild” as described by researchers. Significant fatigue, musculoskeletal pain, fractures that don’t heal and many bodily processes can be problematic. Vitamin B6 toxicity can also be very damaging eg nerve death. This illness sounds highly “metabolic” to me! Is there new understanding in this illness, especially related to trauma/ surgery triggering middle aged adult presentation or “flares” and worsened health? Thank-you, P