

A Solve M.E.-funded project to uncover and assess the latest Long-COVID research findings made these blogs possible
The coronavirus was only a trigger. The question is what did it trigger?
The goal of these continuing research reviews is to find out what researchers are learning about long COVID and how it might apply to chronic fatigue syndrome (ME/CFS), fibromyalgia (FM), postural orthostatic intolerance syndrome (POTS), and related diseases.
With long COVID becoming a thing last summer, and many studies taking years to create, complete, and get published, we’re probably still getting only a taste of the work underway to understand long COVID. Several things are already clear, however. The work on long COVID is very broad-based, with researchers all over the world participating, very few of whom have any connection with ME/CFS. That’s excellent news for ME/CFS as people with ME/CFS make a natural control group that some of these researchers will want to employ in future studies.
First, though, a look at what the big research funder in the long COVID field – the National Institutes of Health – is doing to support both long COVID and its sister disease, ME/CFS.
The NIH, Long COVID and ME/CFS/FM
One negative note to report: while the NIH is talking a good game about ME/CFS and long COVID it’s not doing anything to include ME/CFS in its studies. The NIH grants are not allowing ME/CFS patients (or other disease groups) to be used as controls. Nor is it clear if the NIH is even asking researchers to assess if long COVID patients meet the criteria for ME/CFS (or fibromyalgia for that matter).
This certainly doesn’t mean that long COVID research won’t lead to breakthroughs for these diseases – it will and a future blog later will demonstrate how. It does indicate, though, that despite the close connection between the two conditions, the NIH is not doing anything to integrate ME/CFS into its huge long COVID funding opportunities. (Check out questions ME Action and Solve ME submitted to the NIH regarding integrating ME/CFS into long-COVID research)

Advocacy efforts directed at the US Congress are crucial. We almost achieved a monster win last year.
This highlights the fact that we’re going to continue to have to fight for what we get and how crucial effective advocacy. It was Congressional advocacy, after all, that got the NIH the $1.15 billion to spend on long COVID. Despite Dr. Collin’s public concerns about long COVID, despite all the publicity long COVID has received, it’s very important to note that NIH didn’t do anything to specifically support long COVID until it got money from Congress. So far as the NIH was concerned it was almost as if long COVID didn’t exist. If Congress hadn’t acted, the NIH probably wouldn’t be producing any large-scale efforts to recruit long COVID researchers There would certainly be no huge studies, no biobanks, no data collection centers, no consistent methodological approaches. Instead, the small amounts of long COVID research that did get funded would have been done in a haphazard and inefficient manner.
All sorts of advocacy opportunities exist – and they are all helpful – but legislative efforts directed at Congress potentially bring the most bang for the buck. While not easy to achieve they have the potential to literally change the landscape of ME/CFS funding overnight. We actually came close to doing that last year.
An Opportunity Missed

Passing HR 7057 last year could have provided a breakthrough in NIH funding for ME/CFS this year.
Our failure to come together and pass HR 7057 (the U.C.S. ME/CFS Act) last year to have Congress directly oversee MECFS funding at the NIH had real consequences. If it had passed Congress would have taken control of the $15 million in funding ME/CFS got last year. The real purpose of the bill, though, was for Congress to determine if NIH funding for ME/CFS was adequate the next year, the year after that, and the year after that.
The Solve ME Initiative and the advocates who supported its work during Lobby Day and afterwards made sure Congress well knew the long COVID-ME/CFS connection. Given that it would have been surprising, indeed, if Congress had not told the NIH to dramatically increase its funding for ME/CFS this year – finally fulfilling decades of effort to increase funding for this disease.
Two Other Major NIH Initiatives Underway
This is the second major research opportunity into which ME/CS seemingly fit like a glove and has, at least thus far, been excluded. The first was the $170 million NIH-funded exercise initiative seeking to get at the molecular roots of exercise. As that effort specifically did not include any other disease groups it was no surprise that ME/CFS wasn’t included.
That was the bad news. The good news is that both these two huge efforts are aimed directly at core issues in ME/CFS and long COVID and will undoubtedly help them greatly. The NIH’s HEAL initiative on chronic pain makes it three large NIH initiatives underway that are focused on the key symptoms in these diseases.
That is great news. They underscore, though, the need to make sure that the ME/CFS/FM research fields are in position to quickly take advantage of the insights that will surely flood in over the next couple of years.
The other good news is that the long COVID research results continue to suggest that it is indeed closely related to ME/CFS/FM and that findings from long COVID will likely translate to these conditions and vice versa. With that onto the research review…
Long-COVID Study Research Review
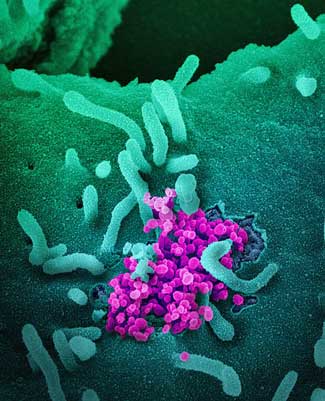
Immune System
T-cell exhaustion has been proposed in ME/CFS, and interest in the role T-cells play in fibromyalgia is growing. One study suggests T-helper cells that help drive the immune response are reduced in long COVID – perhaps indicating a role in the immune response that allowed the coronavirus to be active longer and produce more long-term damage. A similar finding has been found in multiple sclerosis and helper T-cells have been targeted in fibromyalgia.
Another long-COVID study found that cognitive deficits and reduced quality of life was associated with reduced expression of memory T cells. Plus, in a really intriguing finding which could perhaps explain some of the negative responses to the COVID vaccines in ME/CFS/FM, the study found “aberrantly elevated” T cell responses to SARS-CoV-2 mRNA vaccines in the long-COVID patients.
Another study found that neutrophil dysfunction appears to be causing long-term immune suppression in long-COVID patients. That was interesting given that neutrophils appeared to be kicking the bucket in larger numbers than usual in ME/CFS and that abnormal neutrophil counts were found as well. The long COVID study also suggested that histamine producing or triggering cells may be upregulated in long COVID – suggesting that mast cell activation may be occurring. On that note, a long-COVID mast cell study didn’t have much to say about biology, but it did note that the symptoms found in mast cell and long-COVID patients were virtually identical.
We don’t know if ME/CFS or long COVID are autoimmune diseases and no studies have assessed ME/CFS patients response to the coronavirus, but the fact that people with autoimmune diseases appeared twice as likely to come down with long COVID, and have more severe long-COVID symptoms, suggested some type of connection is present.
Mayo Clinic researchers looked for a condition called autoimmune encephalitis – which is about as nasty as it sounds – and found it in long COVID – but only it in a very small percentage of patients.
An ACE-2 / Gut / Dopamine / Brain Connection?
The ACE-2 receptor that the coronavirus binds to in order to enter cells potentially presents a fascinating connection as ACE-2 problems have also been found in ME/CFS. ACE-2 receptor problems, for instance, could play a role in the low blood volume found in ME/CFS. A French group took it upon themselves to look for the receptor in gut tissues and found that a coronavirus infection of those cells reduced dopamine production, and given the role that gut-produced dopamine plays in the brain, could produce “prolonged brain alterations.”
That’s a pretty nice connection given that Miller’s ME/CFS studies suggest that a key dopamine-producing area in the brain (the basal ganglia) may be dysfunctional in ME/CFS.
On the subject of dopamine, no less than three 2021 studies found that different dopamine agonists (enhancers) (Daphnetin, Ropinirole, Pramipexole) reduced symptoms in fibromyalgia mouse models. Dopaminergic drugs have not been used much in chronic pain, but a recent review suggests more trials will be coming.
A deranged ACE-2 receptor may not be the only potential microbiome connection between ME/CFS, fibromyalgia, and long COVID. Several studies suggest that a bad bloom of gut flora plays a role in both ME/CFS and fibromyalgia. Not only did a study of the oral microbiome (in the mouth) in long COVID find evidence that more pro-inflammatory bacteria were present, but the authors specifically stated that the bacteria found were similar to those found in ME/CFS.
Blood Vessel Connections Rising
Aortic hypermetabolism – presumably associated with inflammation – or a virus- was detected about 20% of long-COVID patients. The possibility that inflamed endothelial cells lining the blood vessels are present has been suggested in both ME/CFS and fibromyalgia. A 2019 study, in fact, proposed that a marker of endothelial cell dysfunction might prove to be a diagnostic biomarker for FM.
As has been found in cardiac studies in ME/CFS, no heart structural abnormalities that could explain the fatigue/exertion problems in long COVID were found in a Turkish study. Increased i18F-FDG uptake was found, also suggesting that a hypermetabolic state associated with inflammation was present. Plus, low NO (nitric oxice) levels suggested that endothelial dysfunction was present and was impeding blood flows. (The endothelial cells lining our blood vessels dilate them using NO.
An Italian study also found evidence of endothelial cell dysfunction and reduced blood flows. The two twists in this study were that the blood flow reductions were associated with pulmonary problems – which have not been found in ME/CFS – and were found in men but not women with long COVID.
The endothelial dysfunction idea fits in very well with ME/CFS hypotheses put forth from Wirth/Scheibenbogen, Fluge/Mella, Systrom and Shungu as well as several findings in fibromyalgia.
Exercise testing
Exercise testing is a crucial test for long COVID, ME/CFS and FM because of the potential for the role that energy production plays in these diseases. Exercise comes easier to people with FM than to people with ME/CFS, but that doesn’t mean it’s a walk in the park. Studies suggest that people with FM have trouble raising their heart rates to optimal levels during exercise, that peak energy production may be reduced, and that oxygen delivery to the muscles may be impaired. Plus, a recent review of the role pain plays in post-exertional malaise confirmed “pain as a component of PEM” and emphasized “its debilitating impact in ME/CFS and FM”.
The first long-COVID exercise test did show similarities to ME/CFS. Find out more about that here
The long-COVID exercise study appears to have recruited Donna Mancini, an exercise physiologist, to work on ME/CFS. That’s a very good thing – the more exercise physiologists poking into ME/CFS, the better.
The Mancini-Natelson Exercise Study is Now Open
An NIH-funded 2-day exercise study – called “A Cardiovascular Analysis of Post-exertional Malaise” – aims to dig deeper into the exercise problems found in ME/CFS than has been done before.
The question they’re trying to answer is a central one: why do people with ME/CFS tend to blow through their aerobic energy production systems so quickly during exercise – leaving them trying to squeeze little bits of energy out of their anaerobic energy production system?
This several million-dollar, 120-person study is going to have severe and non-severe ME/CFS patients, and healthy controls. It’s taking place at the Icahn School of Medicine at Mount Sinai University In New York City. They have funds to help participants with travel expenses and time spent (but not airfare). To find out more, call the Pain & Fatigue Study Center research staff at 212-844-6665.
The Gist
- The NIH is not including ME/CFS patients in its long COVID studies and, indeed, is not doing anything specifically for ME/CFS in its long COVID work.
- While ME/CFS still stands to benefit enormously from the long COVID work it highlights how important advocacy is. The NIH wasn’t going to do anything for long COVID until advocates got Congress to pass money to study it. Likewise, it’s not going to specifically do anything for ME/CFS unless advocates get Congress to push it to do that.
- We missed a big opportunity when we failed to come together and pass HR 7057 – the U.S. ME/CFS Act – last year which would have given Congress oversight over the NIH’s funding for ME/CFS. Given the connection between long COVID and ME/CFS, it seems likely Congress would have told the NIH to dramatically increase its funding for ME/CFS this year.
- Immune findings remain pretty sparse but neutrophil dysfunction has been found in both ME/CFS and long COVID. Gut studies suggest that dopamine production problems could reach all the way up to the brain. That’s intriguing as several studies in both FM and ME/CFS suggest dopamine problems in the brain may be present.
- Endothelial cell dysfunction in the blood cells has quickly become a topic in long COVID and has been a topic in fibromyalgia and ME/CFS for quite some time. As blood vessels problems could explain much – reduced energy production, reduced blood flows to the brain, microcirculation problems – in all three diseases it’s good to see long COVID researchers concentrating on them so early – and coming up with similar results.
- Similarly, it’s very good to see exercise studies crop up in long COVID so quickly – and for those studies to display some similar findings to those found in ME/CFS. Hopefully, it’s only a matter of time before the 2-day exercise studies Workwell has championed in ME/CFS, get underway, and long COVID researchers begin using exercise to stress their patients’ systems.
- Findings suggesting that a hypercoagulable state is present in long COVID are intriguing given similar findings which showed up in ME/CFS/FM about 20 years ago. They present another way to explain reduced blood flows to the muscles, reduced cellular energy production, etc.
- A finding that a hypercatabolic state appears to exist where people with long COVID are breaking down their muscles to produce energy is eerily reminiscent of similar findings in ME/CFS. The metabolomic studies sure to show up in long COVID will be fascinating indeed.
Another finding suggesting that the blood is having trouble getting to the muscles in some long-COVID patients is reminiscent of Systrom’s findings as well. It was interesting and encouraging as well that these authors – hailing like Systrom does from Harvard – suggested that non-traditional (i.e. more in depth) exercise testing is needed. Let’s hope that they’re in touch with Systrom.
Next came an Israeli exercise study which found reduced peak V02 and other findings lower in long-COVID patients. Chronotropic incompetence – the inability to raise the heart rate to high enough levels during exercise – was the believed cause. The study also found reduced stroke volume, which was believed due to a reduction in diastolic volume. Chronotropic incompetence has also been found in ME/CFS, and, if I’m reading them correctly, the Isreali findings like a match for Systrom’s finding of reduced preload, which is likely caused by microcirculatory leaks that are reducing blood flows to the heart.
That long-COVID researchers have so quickly turned to exercise studies to attempt to explain long COVID is a surprising, at least to me, and very welcome development. That, fingers crossed, should lead to employing Workwell’s 2-day exercise tests in long COVID, and hopefully in fibromyalgia as well.
The 2-day exercise results – which have found that exercise one day damages one’s ability to exercise the next day – are apparently so unusual that some exercise physiologists explain them by assuming that Workwell must be doing something wrong. Similar results showing up consistently in long COVID would present the medical world with a real problem – how to explain something they don’t believe should exist.
A Hypercoagulable State?
Thick, clotty blood could presumably impair oxygen delivery to the muscles and it was thick, clotty blood that the next long-COVID study found. The study found “a significant failure in the fibrinolytic process. Of particular interest was the presence of persistent anomalous (amyloid) microclots and a pathological fibrinolytic system”.
In fibrinolysis, fibrin clots – which are found in coagulated states – are broken down. Hypercoagulation was quite a thing in both ME/CFS and fibromyalgia about 20 years ago, but after a quite small study – which noted that it was too small to be definitive – found no evidence of it in ME/CFS, that was pretty much it for that idea. Dr. Holtorf, though, apparently still uses heparin to good effect in some of his ME/CFS/FM patients.
Muscle Breakdown in Long COVID and ME/CFS?
It looks like hypercoagulation may be a big subject in long COVID as an Italian study also found high markers of coagulation, suggesting that an inflammatory/hypercatabolic state was present.
It was really intriguing to hear hypercatabolism mentioned given that it implies “a breakdown of muscle and adipose tissue… as a result of injury, metabolic stress, or sepsis or an unduly rapid breakdown of body tissues”. As was just noted in the Chris Armstrong interview, the ME/CFS metabolomic studies suggest that people with ME/CFS are indeed in a hypercatabolic state and are breaking down their muscle tissues for energy.
Health Rising hasn’t dug into fibromyalgia metabolomic studies as much, but recent studies have also highlighted metabolites associated with energy production and amino acid metabolism. One study – which mimicked findings in ME/CFS – highlighted energy, lipid, and amino acid metabolites, which suggested that heightened oxidative stress, inflammation, and tryptophan degradation play a key role in FM.
Metabolomics is often touted as an excellent diagnostic tool for diseases with unknown origins. As the metabolomics field has become more and more settled, over time we can expect many long-COVID metabolomics studies to show up. One such study found distinct metabolic differences between long-COVID patients and people who’d completely recovered from COVID-19.
Musculoskeletal
Explaining the musculoskeletal problems in fibromyalgia (FM) and ME/CFS – including the evidence of things like cranocervica instability (CCI) and tethered cord syndrome – has presented a problem. A two-person case series may have an answer. This report from Italian researchers of two patients who developed an inflammatory condition called sacroiliitis after a mild coronavirus infection suggests that a systemic inflammatory response triggered by the virus may have produced it. This area clearly needs a lot more research and we may get it as the massive NIH-funded studies follow long COVID patients over time and start to pick up the musculoskeletal problems that show up.
Gender

Will gender bias inhibit long COVID efforts?
An Italian review found, interestingly enough, that women experience less severe short-term complications from COVID-19 but more severe long-term complications; i.e. are more likely to come down with long COVID. It almost seems as if women are better equipped to fight off the virus (a stronger Immune response?) but that doing so is more apt to destabilize them. This may make sense with regard to autoimmunity. Infections can trigger autoimmune diseases – which women are also more susceptible to.
Another paper tackled the gender question head-on, calling gender disparity “a black hole for long COVID”. The paper stated, “Unfortunately, there is also “a school of thought” sustaining that the Long COVID gender skew could simply represent an artefact: it could just be conceived by “hysterical, middle-aged women”, and then noted that females have stronger innate and acquired immunological and hormonal responses than males and have a higher incidence of autoimmune diseases.
The Long-COVID ME/CFS Connection
Finally, with some long-COVID patient groups reportedly shying away from being associated with ME/CFS, it was good to see a spanish group take the bull by the horns and explicitly ask: “Long COVID: Is it really myalgic encephalomyelitis?”. They concluded “that persistent COVID syndrome does not constitute a new entity but is, in fact, in some cases, a myalgic encephalomyelitis.”
That’s an interesting conclusion given that while many studies assess long-COVID symptoms, I’ve only found one which assessed how many ex-COVID patients met the criteria for ME/CFS. That study found that symptoms such as fatigue were common six months after infection and that 13% met criteria produced for “systemic exertion intolerance disease” – the term developed by the IOM panel for ME/CFS. Those findings suggest that COVID-19 is indeed very good at producing ME/CFS – and that it’s also producing distress in people who don’t meet the criteria.
Conclusions
The NIH may not be specifically supporting ME/CFS in its long COVID studies but the long COVID research studies thus far provide plenty of room for encouragement for ME/CFS and fibromyalgia patients as similar immune, blood vessel, exercise, metabolomic and other findings suggest that the diseases are quite similar. The fact that long COVID researchers have already jumped on exercise studies is surprising and encouraging and suggests it’s only a matter of time before the crucial two-day exercise studies are mounted in the long COVID field. The fact that many researchers from outside the ME/CFS/FM fields are studying long COVID suggests that the ME/CFS/FM research fields are due to expand as some of them gravitate to it.
We’re still at the very beginning of learning about long COVID, with many more studies likely to come. The NIH, for instance, has yet to announce the recipients of roughly $500 million in grant funding. So far, though, so good.
Check out the first long COVID research review.








I should start by saying I’ve had severe ME for over 33 years and earlier this year complained to the UK government demanding money for ME research. But….
I can kind of understand why they are throwing everything at Long Covid and excluding ME. I read an article about Long Covid research on the Cambridge University website at the beginning of the year. One of the researchers was saying ‘In CFS we don’t know the cause, although it’s thought that infection can be a trigger. In long Covid we know people have had a specific infection’.
Even those who are sure they have Long Covid but no test to prove they had Covid are often being excluded from research. I think it would muddy the waters if they included other similar illnesses like ME too soon.
I take heart from the fact that all the top researchers and best brains in the world are desperate to get involved and help with this crisis – and be the first to make new discoveries! There is also a huge amount of private funding, as well as money from many governments around the world. Many researchers see it as a huge opportunity to learn about viruses and the immune system and the way different peoples bodies deal with them, and hope it will help them learn more about many illnesses not just ME.
Well put, Kate. I imagine that the immense amount of research that will follow will tell us not only about ME/CFS/FM/POTS but autoimmune diseases and inflammatory conditions. I wonder if we will learn that infections may sometimes produce effects and trigger illnesses that we hadn’t thought of. With 15,000 people in the study they will certainly have the power to assess the incidence of all sorts of conditions. It’s going to be fascinating.
I still do think that ME/CFS with its often post-infectious onset would have made a nice control alongside the healthy control but we will certainly benefit from all these studies.
(…)”Cambridge University website at the beginning of the year. One of the researchers was saying ‘In CFS we don’t know the cause, although it’s thought that infection can be a trigger. In long Covid we know people have had a specific infection’.”
What a short-sighted if not stupid statement for someone from Cambridge. Specific infection? Isn’t he aware that, for example, Epstein-Barr virus (EBV) is also a specific infection that causes ME? Of course ME patients have suffered from a specific infection prior to the disease (not all). The point is that no damage is found to organs or any other physical cause. That is also the case with most of LC so you can call it ME.
I hope they will use ME patients as a control group along with healthy people in studies into the cause of LC. That would be great for us.
i completely agree with you! not only EBV but so many other infections. they should take ME/cfs as controls just like even FM and chronic lyme etc. for me it is just again: not interested in ME (the infectious onset group). And yes, they will learn a lot about long covid-immunesystem, etc but no money for us. for resarch for us. big money. so big money that it can move things, also for us and other groups.
I agree with you that Long Covid is ME. Researchers at Cambridge Uni started taking regular blood samples from a group of patients who tested positive for Covid in summer 2020. Varying degrees of illness – some asymptomatic. They have been able to monitor the immune system right from the early stages of a virus, and see what changes happen to the immune system over months in the Long Covid patients. Most of us with ME have been ill 5 plus years already, so it is too late to see what gradual changes happened to our immune systems to leave us with ME.
https://www.cam.ac.uk/research/news/biological-fingerprints-of-long-covid-in-blood-could-lead-to-diagnostic-test-say-cambridge
Kudos yet again Cort for an excellent roundup.
I’m intrigued by the study showing a response to histamine blockers.
They note in the discussion: “All symptoms improved except dysautonomia, suggesting that this arises through another mechanism. Indeed, dysautonomia following other viral infections is associated with autoantibodies to adrenergic and cholinergic receptors, and COVID-19 is linked with autoimmune phenomena.”
My ongoing “research” (personal observations/readings/thinking) as PhD in a different field are leading me to believe the histamine elevations (and symptoms) are being driven by microbial histamine from the gut microbiome, rather than mast-cell histamine release.
The microbiome studies for ME/CFS to date have consistently shown an increase in the Bacteroides genera, which are histamine producers.
I suspect this microbiome shift towards histamine producers is occurring coincidently because of the “other mechanism” behind dysautonomia the authors reference. For instance, the Bacteroides genera is generally more aerophilic than the average anaerobe and may be growing because there’s more oxygen in the blood, as Dr. Systrom has shown in at least some ME/CFS patients.
In other words I suspect the microbiome signatures and histamine-mediated symptoms are secondary. Likewise for sleep symptoms, which may be partly mediated by histamine as well (a wakefulness promoter).
Personally I’m on a mast-cell downregulating probiotic and it’s having a stronger effect than my earlier trial on an H1 blocker (Claritin) for my breathlessness, ENT, and sometimes ocular symptoms. But it’s having no benefit for my orthostatic intolerance or post-exertional malaise symptoms. Exactly as they show as well: the PEM was nearly as unchanged as the dysautonomia.
I’m happy to discuss in greater detail these hypotheses with anyone interested.
Hello @Vijay Iyer, thank you for sharing your experience and thoughts. Do you have insomia/daytime drowsiness as part of your symptomatology- if yes, did the mast-cell downregulating probiotic have any effect on these particular symptoms? Thanks again.
Hi @lush.green.pastures. I actually haven’t had much daytime drowsiness in my symptoms. I have generally felt like I’ve been wakeful through my fatigue and have had only mild insomnia (mattress cooling has helped me with this some). The main benefit of the Lactobacillus rhamnosus strains I’ve been trying has been on upper respiratory symptoms. But unfortunately no benefit for fatigue.
What an interesting idea – histamine being produced from the gut. Did you see the recent nature study showing that some of the gut pain associated with conditions like IBS is histamine related –
Following subsequent oral ingestion of the respective dietary antigen, an IgE- and mast-cell-dependent mechanism induced increased visceral pain. This aberrant pain signalling resulted from histamine receptor H1-mediated sensitization of visceral afferents. Moreover, injection of food antigens (gluten, wheat, soy and milk) into the rectosigmoid mucosa of patients with irritable bowel syndrome induced local oedema and mast cell activation.
https://pubmed.ncbi.nlm.nih.gov/33442055/
I hadn’t seen that one Cort, thanks for the tip. Very interesting to see that IgE can be active locally and that its effect goes beyond classic allergy symptoms.
I’ve been keeping an eye on the situation where bacteria secrete histamine directly. This hasn’t been strongly characterized, but it seems pretty clear that the Bacteroidetes produces more than Firmicutes, among the top two gut phyla. Here’s one paper on the topic: https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-021-08004-3.
Hi Vijay,
What mast cell downregulating probiotic are you using that you found helpful?
I have ME and have gone from being totally bedridden to almost being well again. I have long believed that it is a post viral syndrome and even those who didnt have a virus, Covid is showing us its possible to actually have a virus with no symptoms. My theory is that due to stress the body is under that those who are stressed or get up too quickly and dont rest enough with a virus are more subsceptible. The term yuppie flu int 90s for the illness was derogatory but actually if you think about it and my theory is correct, its these types of people who get LC/ ME etc – high achievers who go to work when ill , who exersise in gym during flu etc !
You have said something that is not correct:
“….despite all the publicity long COVID has received, it’s very important to note that NIH didn’t do anything to specifically support long COVID until it got money from Congress. So far as the NIH was concerned it was almost as if long COVID didn’t exist.”
I was enrolled in NIH studies on Long COVID last fall, several months before the $1.15 B appropriation was enacted in December. I know that you are focused on NIH’s extramural funding. But, NIH’s intramural program launched its efforts before the new funding was provided.
Thanks for that. That’s a great project and it was initiated by the NIH. I will amend the blog to note that. I was thinking more, though, of broad efforts; i.e. something like an RFA or some other program that would serve to attract many researchers to long COVID. I’ve amended a sentence to clarify that: “the NIH probably wouldn’t be producing any large-scale efforts to recruit long COVID researchers” (f not for Congress)
I’m glad you’re making that edit. Even with that change, however, I still think your point runs counter to the facts, because you imply that NIH is doing this against it will. I do not think that is true. Collins devoted his Sept 3 2020 blog post to Long COVID, and Long COVID research is specifically prioritized in the NIH-wide Strategic Plan for COVID. We also know that NIH aggressively sought the supplemental funding for Long COVID research. So your “if not for Congress” argument doesn’t hold water in my opinion.
Please don’t put words in my mouth. I did not imply that the NIH is doing this against their will. I never said that. I think the NIH and Dr. Collins were very happy to get all this funding and as the recent Mammoth Blog demonstrates I think they’ve done an excellent job with it.
https://www.healthrising.org/blog/2021/09/18/nih-mammoth-effort-understand-treat-long-covid/
I said the NIH didn’t do anything special for long COVID and I think the record bears me out. Unless I’m missing something if you go to the NIH Reporter (https://reporter.nih.gov/search/dzoGdzKRHke92njQgHg4jw/projects ) you’ll see how many long COVID studies the NIH has funded over the past year and a half. (Astonishingly few)
We’ve learned over the years that program announcements, plans, and good words mean little if not nothing if forward funding is not provided for diseases like ME/CFS or long COVID which do not have a strong established research base. Collin’s blog posts on ME/CFS, for instance, while welcome, did nothing to increase funding for ME/CFS. Neither have NIH workshops or conferences. The only things that have done are RFA’s that come with funding attached.
I overstated when I said that you wouldn’t have known long COVID existed by the NIH as Collins did the blog and long COVID was included in the strategic plan but in real terms, the statement was correct in the main because the NIH knew long COVID was out there, knew a lot of people were getting sick, knew it was funding very few studies and did not take actions to correct that. Given that I’m going to stick to my conclusion that without Congressional action the NIH would have continued on as it had, let things go as they had been going, and would not have developed the paid funding programs needed to boost interest in long COIVD. The long COVID research it did fund would have dribbled in overtime in an unorganized fashion.
In my experience that’s how the NIH operates – its funding is driven by researcher interest and if researcher interest is not there, unless the disease becomes some sort of political issue- see the HEAL Initiative which I believe was initiated by the NIH in response to the opioid crisis – the disease will not get funded.
Given that there really hasn’t been a post-infectious research field and precious few researchers outside of ME/CFS are acquainted with it, it’s no surprise that the NIH, up till the Congressional action, appears to have funded embarrassingly few long COVID studies. Acting by itself the NIH is totally at sea with diseases that affect a lot of people but don’t attract many researchers (see ME/CFS, fibromyalgia, IBS, POTS, until recently long COVID.)
I don’t know what you mean that the NIH aggressively sought supplemental funding for long COVID research. Do you mean from Congress? If so, that’s good to hear. Note, though, that it was waiting for someone else to take action.
In case anyone is interested, here is the link for the NIH-wide Strategic Plan for COVID-19 Research.
https://covid19.nih.gov/sites/default/files/2021-05/NIH-Wide-COVID-19-StratPlan_2021_508_1.pdf
I’m not sure you ran the right search on NIH REPORTER. The link you provided was a search on the words “long” and “COVID”, and the report was so long I never was able to scroll to the bottom of it, as it listed all awards that contained either of those terms. Here is a link for a report of awards from the FOAs issued for the RECOVER Initiative: https://reporter.nih.gov/search/J2yq9hkjE0SOzliUYYFdzg/projects?shared=true
It’s more interesting, I think, as it shows just 2 awards, recognizing that the NYU award will have dozens of sub-awards as part of the national network.
It did show a lot of awards that didn’t fit – more than usual – but that’s pretty much par for the course. I put in long COVID, long-COVID, Post COVID, PASC, Post-Acute Sequelae SARS… and very little showed up – and quite a few duplicates did. The best matches should show up on top. A chronic fatigue syndrome search brings up ME/CFS and myalgic encephalomyelitis award pretty quickly – after that – hundreds of awards that have no real relevance.
Yes, NYU Langone is apparently in charge of deciding on and disseminating the awards. It’s a very organized process. We should know about them soon.
There’s a new study about disruption to the basement membranes in the cerebral vessels of COVID infected mice. It might be relevant to the muskoskeletal question, given its biological proximity to connective tissue, and related findings regarding increased expression of the MMP9 gene and decreased expression of Collagen IV.
“The basement membranes of cerebral vessels were shown to be damaged, although the TJs [tight junctions] were not significantly altered in either infected K18-hACE2 mice or hamsters. An increase in MMP9 expression could explain collagen degradation, resulting in the destruction of the basement membrane. ”
Something to keep an eye on.
Study: https://www.nature.com/articles/s41392-021-00719-9
Thanks Cort. Did you see that one about the differentiation between the immune profiles of FM and ME/CFS? That was really interesting. Maybe you have written about it before.
Long Covid CURE!: https://w
ww.youtube.com/watch?v=wliXL53LzUs
Has anyone seen the news articles featuring researchers in South Africa and Ireland who have both found large numbers of blood clots in the blood of Long Covid patients?
If Covid wasn’t killing people, no money would be spent on it…the long haul version or the acute illness. Long haul Covid would likely be given only lip service in funding since it doesn’t kill you….just makes you feel like you are dying.
Recognition of long, complicated illnesses like Long Haul Covid and ME/CFS come with costs no one wants to pay…disability payments, endless medical bills, loss of productive members of society.
But if any funding becomes available, the “more study is needed” industry will take over. This is where no two studies are funded with the same protocols so no finding can be confirmed and at the end of every study, the authors will say, “we may have found something”, but more study is needed. Of course more study is needed when the base rate for NIH grants averages about 52%—meaning the agency pays a school $52,000 to cover overhead costs on a $100,000 research grant.
How many long haul ME/CFS people have been contacted and included in the long haul COVID research? There are .. how many thousands? .. ME/CFS long haulers since the 1980’s that would make a good research pool to work with. ….. very telling.
In my near-daily research, I have come across a doctor who has been treating CFS for decades, and teaching other doctors to follow a protocol that works for most patients. His name is Jacob Teitelbaum, MD, and had suffered with CFS himself. His website is end fatigue.com. He healed himself completely with multiple supplements. I’ve just begun part of his protocol, and I will add more supplements after an appropriate period of “loading”. I started with D-Ribose, which I had ordered just before coming across the You Tube video of his long discussion of CFS, and the treatments he recommends, one of which is D-Ribose. His research even shows up on PubMed – my trusted source. There is MUCH to learn, reading about his protocols, which includes a natural supplement mix for sleep. I am beginning to feel optimistic after 8 years of life-altering fatigue with accompanying depression.
Per Times of Israel this week, Israel recognizing ME CFS and FMS as disabilities
Yah! Good to hear. One wonders if this is at least in part an add-on from the long COVID issue.
I was wondering exactly the same thing.