

Along with fatigue and nausea, pain has been one of the defining symptoms of my daughter’s illness. After she was diagnosed in 2018-2019 at age 14-15 with hypermobile Ehlers-Danlos syndrome (EDS), chronic fatigue syndrome (ME/CFS), craniocervical instability, Chiari malformation, occult tethered cord syndrome, postural orthostatic tachycardia syndrome (POTS), and mast cell activation syndrome (MCAS), we learned of treatments that have helped to reduce her pain. Low-Dose naltrexone has reduced the pain in her back and ribs. After starting mast cell stabilizers, her joints have become less likely to pop out of place, reducing pain from joint dislocations.
But certain forms of pain persisted and even worsened over time. In particular, many parts of her body, including her abdomen and upper arms, were painful when touched. She also had pain in her chest, lower back near her coccyx, and face, among other locations. One doctor suggested the pain was caused by central sensitization, potentially related to her MCAS or craniocervical instability.
Locations where lipedema occurs (From Stat Pearls – Lipedema (https://www.ncbi.nlm.nih.gov/books/NBK573066/)
These factors may well be contributing to her pain, but I have come to believe that the most proximate and important cause of the pain in her abdomen, chest, upper arms, and lower back has been the build-up of lymphatic fluid and the resulting formation and fibrosis of adipose tissue. I believe this because we have made dramatic gains in treating this pain through a combination of manual lymphatic drainage and massage techniques designed to break up fibrotic tissue and reduce the build-up of fluid in her tissues.
Her arms and abdominal areas are no longer painful when touched. The coccyx pain is also largely gone and the pain in the chest and face is more manageable. The treatments, which we do regularly, have also helped reduce problems with swallowing, breathing, and sitting up as well as swelling and pain around previously engorged lymph nodes. In the abdomen and thighs, the treatment has eliminated bubbles that could previously be felt under the skin; in these locations and on the upper arms, the skin now has a smoother texture. The treatment also helps to reduce the feeling of heaviness in her arms and legs.
I cannot say whether my daughter’s experience is generalizable to others with her conditions, but as I have done more research into the lymphatic system, adipose tissue fibrosis, and the related disorder of lipedema, I have become convinced these are important topics that merit further exploration in the context of EDS, fibromyalgia and ME/CFS. At a minimum, I would encourage broader awareness of lipedema, a condition involving the build-up and fibrosis of adipose tissue, which may be an important comorbid condition in some people with EDS, fibromyalgia, and ME/CFS. More broadly, I would encourage researchers to investigate whether the build-up of lymphatic fluid and the fibrosis of adipose tissue play an important part in the disease cycle of one or more of these conditions, even in the absence of noticeable weight gain.
Lipedema
As described in a recent article on the standard of care for lipedema in the United State:
“Lipedema is a disease of fibrotic loose connective (adipose) tissue . . . on the lower abdomen, hips, buttocks, and limbs of females, sparing the trunk, hands, and feet. Lipedema is rare in men. A trigger for the development of lipedema tissue may be an increase in fluid and connective tissue remodeling that occurs alongside body changes during puberty, childbirth, menopause, stress associated with lifestyle change, or by altering tissue structure after surgery or trauma. A hallmark of lipedema tissue is inflammation, resulting in tissue fibrosis and pain, and in some cases, the tissue may become numb.”
The literature suggests lipedema is quite common: “Prevalence estimates for lipedema range from 6.5% in children in the US, 6%–8% in women in Germany, and 15%–19% in vascular clinics.” These estimates are based on small samples, so they could overstate the incidence of lipedema. But even if the prevalence of lipedema were only a fraction of the stated estimates, it would be a fairly common disorder. Moreover, a large percentage of women with lipedema are hypermobile. One study of 160 patients with lipedema found that 58 percent had a Beighton score of 5 or more, a marker of hypermobility.

Four stages of lipedema
The most widely recognized symptom of lipedema is weight gain in specific areas of the body, but lipedema can be difficult to detect in the early stages when it is most easily treated. There are five types of lipedema, which describe different patterns of affected areas, which can include the buttocks, hips, thighs, calves, and arms. Lipedema can also affect the abdomen. Other areas may be affected in some patients. For example, a study of 160 women with lipedema found nodular fat, fibrosis or edema to be present in the mid-back (76 percent of the sample), chest/breast (43 percent), and hands and feet (33 percent).
There are three main stages of lipedema:
- “In Stage 1, the skin is smooth but there are pearl-sized nodules in the fat underneath.
- In Stage 2, there is retraction of the skin due to fibrosis of connective tissue fibers surrounding fat lobules and pearl-sized and larger masses in the fat tissue.
- In Stage 3, there are pearl-sized nodules, larger masses, and lobules of the skin and fat.”
Lymphedema, which is sometimes classified as a fourth stage of lipedema, can occur at any of the first three stages but is more common in stage 3 than stages 1 or 2. In lymphedema, the lymphatic system is blocked or damaged, leading to the noticeable swelling of the affected tissue.
Early-stage lipedema in adolescents can be difficult to detect given the many changes occurring during puberty. In our daughter’s case, the pain in her abdomen, arms, and coccyx area was present before we noticed any unusual weight gain. Eventually, she experienced more noticeable weight gain and we observed nodules under her skin, but we would not have recognized them as problematic had her physical therapist not suggested they may be related to the build-up of lymphatic fluid.
According to consensus guidelines, conservative treatment for lipedema includes compression garments that help lymphatic fluid move through the lymphatic system and “manual therapy [that] . . . includes soft tissue mobilization to reduce pain, inflammation and musculoskeletal restrictions, and manual lymphatic drainage as part of an individualized comprehensive therapy program to stimulate lymphatic flow and reduce edema.” Conservative treatment also includes nutritional guidance, sequential pneumatic compression pumps, and exercise.
While there are no medications approved specifically for lipedema, the consensus guidelines mention sympathomimetic amines, metformin, diosmin, and vitamin D supplementation as possible therapies. The guidelines also recommend against the use of thiazolidinediones, which increase subcutaneous adipose tissue, treatments that lead to weight gain, and the long-term use of diuretics, which can concentrate protein in the lymphatic fluid, obstructing the flow and contributing to fibrosis.
Dr. Karen Louise Herbst, a leading expert on lipedema, also recommends supplementation with selenium and avoidance of oral corticosteroids and medications that promote fluid retention, including NSAIDS, sex hormones, calcium channel blockers, beta-blockers, clonidine, and gabapentin.
Lipedema can also be successfully treated with surgery, utilizing a specialized form of “liposuction, excision and manual extraction that spares blood and lymphatic vessels.”
Applicability to EDS, Fibromyalgia and ME/CFS
I am unaware of any research documenting the incidence of lipedema in people with EDS, fibromyalgia, and ME/CFS, but if lipedema is anywhere near as common as estimated, the overlap is likely to be significant. Hypermobility is common in lipedema, EDS, fibromyalgia, and ME/CFS. Overlapping symptoms have also widely been observed – for example, between lipedema and fibromyalgia and between EDS and fibromyalgia. One study found that “symptomatic hypermobility predict[ed] symptom severity in pain and fatigue conditions” in a sample of people with ME/CFS and fibromyalgia.
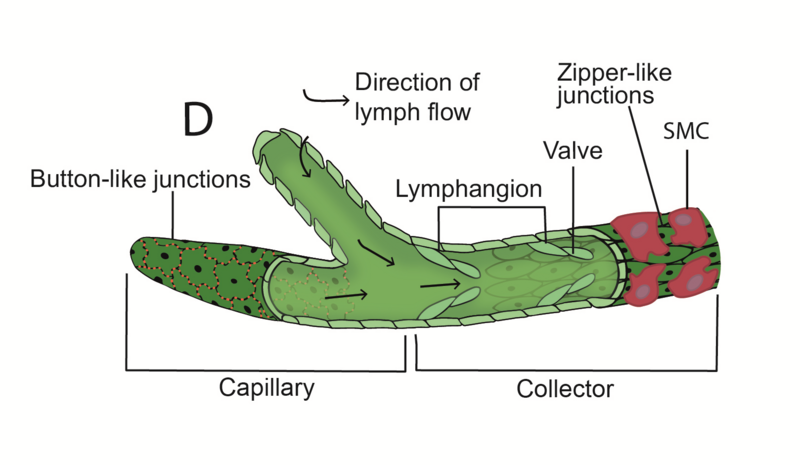
Engorgement of the lymphatic system could affect many parts of the body.
I am not by any means suggesting these disorders are the same. But the high incidence of hypermobility in all four disorders suggests that connective tissue problems may play a role in each one, at least for a cohort of affected individuals. (Since some connective tissue disorders are not marked by hypermobility, it is possible the overlap would be even greater once these other connective tissue disorders were factored in.) The common thread of connective tissue problems raises the possibility that a significant share of patients with EDS, fibromyalgia, and ME/CFS may also have or be susceptible to lipedema.
The Gist
- Lipedema is a disorder characterized by the build-up of lymphatic fluid and the resulting formation of subcutaneous adipose tissue, which then becomes fibrotic and painful.
- Given high rates of hypermobility across all four conditions, lipedema may be a fairly common, yet underappreciated, comorbid condition of Ehlers-Danlos Syndrome (EDS), fibromyalgia, and ME/CFS.
- The author has found some of the treatments for lipedema – including manual lymphatic drainage and the break-up of fibrotic adipose tissue – to be helpful in treating the pain experienced by his teenage daughter, who has EDS, ME/CFS, MCAS, and POTS. Further research is needed to assess the potential of these and other lipedema therapies to help individuals with EDS, Fibromyalgia, and ME/CFS.
- Research is also needed to explore the possibility that the build-up of lymphatic and interstitial fluid and the formation and fibrosis of adipose tissue play important roles in the disease cycles of EDS, fibromyalgia, and ME/CFS. For example, these processes may be contributing to widespread pain, inflammation, and MCAS.
- The author also hypothesizes that leakage from microangiopathic blood vessels in people with connective tissue disorders may play a central role in post-exertional malaise, at least for some individuals with ME/CFS, leading to excess lymphatic/interstitial fluid that floods tissues, leading to hypoxia and inflammation.
- The author urges researchers working on EDS, fibromyalgia, ME/CFS, and lipedema to work collaboratively to identify opportunities for learning across these different domains.
Ehlers-Danlos Syndrome
While there are suggestions in the lipedema literature of a connection between EDS and lipedema, I have found little formal research exploring this connection, with only one case study of an individual with both conditions and no articles examining the use of manual lymphatic drainage in individuals with EDS. While there is a paucity of formal research on the connection between EDS and lipedema, patients are certainly discussing it. See, for example, this article by Oh TWIST and the comments on the article from individuals experiencing both conditions. There are also a number of articles on the overlap in the informal literature, such as this article by functional medical doctor Jill Carnahan.
Fibromyalgia
A number of small studies have found manual lymphatic drainage to be helpful in reducing pain in people with fibromyalgia. One pilot study of 17 women with fibromyalgia (and no controls) found that “[p]ain, stiffness, sleep, sleepiness, and well-being all improved during” treatment with manual lymphatic drainage, and that the benefits in these areas (except for sleep) were still apparent two months after cessation of treatment. Another study of 50 women with primary fibromyalgia compared the effectiveness of manual lymphatic drainage and connective tissue massage (with no control group), finding that both approaches were helpful in reducing pain but that manual lymphatic drainage may have been somewhat more effective. A recent article found strong similarities in the symptoms experienced by patients diagnosed with lipedema and fibromyalgia and notes the possibility of overlap in individual cases. The article does not explore the extent to which individuals experience both conditions, however, as patients with fibromyalgia in the study were not systematically evaluated for lipedema.
ME/CFS
Manual lymphatic drainage is, of course, central to the Perrin Technique for treating ME/CFS, but it’s not clear how widely manual lymphatic drainage is being applied outside of the practitioners certified in the Perrin technique. A search for “lymphatic drainage” and “chronic fatigue” on PubMed and Google Scholar revealed two articles by Dr. Perrin and a case study, but nothing that would suggest a broader formal evaluation of lymphatic drainage in ME/CFS. I have found no formal articles exphttps://theperrintechnique.com/loring the connection between lipedema and ME/CFS in-depth, though one recent preprint on a UK cohort of lipedema patients lists chronic fatigue as a comorbid condition and another article notes that myopathy (muscle weakness) has been observed in both people with lipedema and those with chronic fatigue.
To sum up: there is reason to believe that lipedema may be an important comorbid condition for some people with EDS, fibromyalgia, and ME/CFS, but only minimal exploration of this potential comorbidity has occurred. A lynchpin of lipedema treatment, manual lymphatic drainage, is being used to a limited extent to treat ME/CFS and fibromyalgia, but more research is needed to formally assess its benefits.
Recommendations for Research and Practice
The intersections of these conditions with lipedema merit further exploration through research and practice. I have five recommendations for making progress in this area.
I. Explore the extent to which individuals with EDS, fibromyalgia, and ME/CFS have lipedema
Research is needed on the prevalence of lipedema in individuals with EDS, fibromyalgia, and ME/CFS. A good place to start would be to look at women with EDS whose illness took a dramatic turn for the worse during adolescence, as lipedema appears to be associated with hormonal changes during puberty. The incorporation of protocols to screen for lipedema in studies of women with long-term fibromyalgia and ME/CFS would also help shed light on the prevalence of lipedema in these patient groups.
The Lipedema Foundation provides diagnostic questionnaires
Screening for lipedema may also be helpful in the care of individuals with EDS, fibromyalgia, and ME/CFS. The Lipedema Foundation has a number of helpful diagnostic resources for doctors and patients. An online diagnostic questionnaire is available from the Lipedema Project. There are also any number of self-assessment guides available on the Internet, such as this one from a physiotherapist in Toronto.
While there is no cure for lipedema, the literature suggests that early detection and treatment can help prevent the condition from becoming worse. There are also a number of treatments that can help reduce the associated pain, several of which I discuss in this article.
2. Explore whether manual lymphatic drainage and other massage techniques adapted from the lipedema literature may be helpful for individuals with Ehlers-Danlos Syndrome, fibromyalgia, and ME/CFS
I am not a physician and cannot provide medical advice. But given the reported benefits of manual lymphatic drainage for people with fibromyalgia and ME/CFS, it may make sense for people with one of these conditions or EDS to consider this treatment option whether or not one meets the formal diagnostic criteria for lipedema. If manual lymphatic drainage proves helpful and there are signs of adipose tissue fibrosis, a next step might be techniques that work to smooth or break up the fibrotic tissue. As with all potential treatment options, it makes sense to seek advice from knowledgeable doctors, physical therapists, or other trained practitioners to ensure the treatment makes sense and is safe for you. While the exact process by which manual manipulation remodels fibrotic tissue is not fully understood, we have found it to be enormously helpful in reducing pain, discomfort, and fluid accumulation.
If you are well enough to travel in a car, I would encourage a consultation and treatment session with a certified lipedema specialist or another individual trained in manual lymphatic drainage. If you are not well enough to travel, remote consultations with specialists can be helpful for getting started and implementing the guidance available on the web. My daughter’s physical therapist emphasized the importance of activating the lymph nodes before starting each area and showed us the location of additional lymph nodes that we were not aware of. (We have found that areas around the major lymph nodes can become engorged and painful; regular massaging of these areas has helped to substantially reduce that pain.) A good place to start is with manual lymphatic drainage of the neck/throat and face. We now do a modified version of lymphatic drainage regularly on pretty much the entire body as well as a scalp massage. It is possible to do manual lymphatic drainage on yourself, though a partner will be needed for the back.
It is more difficult to find online materials on how to smooth or break up fibrotic tissue and reduce the accumulation of interstitial fluid in tissues. I would strongly encourage reaching out to a trained physical therapist/physio to have them help with this. Getting treatment from a trained therapist can both provide an indication of whether these techniques are helpful for you and provide guidance on whether, and if so how, these techniques might be safely used at home.
The manual manipulation of subcutaneous adipose tissue to treat fibrosis can be quite painful, but my daughter reports that it provides lasting relief from pain and discomfort; she says it feels like stale fluid has been released. There are a number of techniques for treating fibrosis apart from manual therapy, including vibration and elastic taping. Given its potential for remodeling tissue, it seems plausible that Frequency Specific Microcurrent (FSM) also may be helpful in treating fibrosis, but I have not seen any formal literature on its use for lipedema and have no personal experience with it.
3. Develop clear medication guidelines for patients with these comorbid conditions
As summarized above, the lipedema literature describes a number of medications that might be helpful, as well as a long list of medications to avoid. Readers will note, however, that the list of medications to avoid includes numerous medications and supplements that are commonly used in treating people with EDS, fibromyalgia, and ME/CFS. Fluid enhancers, for example, are a mainstay of treatment for POTS, a common complication of all three conditions. Gabapentin and NSAIDs are used for pain and aspirin (an NSAID) is used to treat MCAS.
The carbonic anhydrase inhibitor and diuretic acetazolamide is used to treat intracranial hypertension, a common problem in people with ME/CFS and the neurological complications of EDS. As I discussed in two earlier Health Rising posts, many people with ME/CFS, fibromyalgia, and Ehlers-Danlos report benefitting from high-dose thiamine, but an in vitro study suggests it also functions as a carbonic anhydrase inhibitor and is thus likely also a diuretic. Quercetin and Luteolin, bioflavonoids used to treat MCAS, also inhibit carbonic anhydrase isoenzymes and thus presumably have diuretic properties. Many herbal supplements are also diuretics.
Given the potential of individuals with EDS, fibromyalgia, and ME/CFS to also have lipedema, it will be important to provide guidance on how to safely treat these conditions without exacerbating lipedema. It will also be helpful to better understand if regular manual lymphatic drainage or other compensatory strategies can help people with lipedema tolerate moderate doses of these medications and supplements.
In my survey of high-dose thiamine, many individuals reported benefitting from doses well below the levels evaluated in prior studies. In my view, the potential of diuretics to aggravate lipedema underscores the importance of formal research to confirm whether these lower doses are effective.
4. Develop creative and practical solutions to help increase the movement of lymphatic fluid in people with severe EDS and ME/CFS
It seems clear to me that physical inactivity was not the initial cause of my daughter’s lipedema or build-up of lymphatic fluid and fibrosis of adipose tissue. (To the contrary, the initial crash that made her disease evident appears to have been prompted by physical exertion.) But conventional wisdom suggests there is a risk that prolonged physical inactivity following a crash could exacerbate these problems by inhibiting the movement of lymphatic fluid through the system.
Assuming this widely held belief is true, we need creative and practical ways to increase the movement of lymphatic fluid in people whose severe EDS or ME/CFS inhibits their ability to get out of bed. This could involve the use of pneumatic compression pumps, for example, or simple exercises that could be done in bed without aggravating patients’ symptoms. These approaches need to be introduced with sensitivity and respect, in a manner that carefully avoids blaming patients for health problems they did not create. It seems to me that timing matters here – introducing these approaches soon after a crash may help to ward off further problems while avoiding an insinuation that inactivity is somehow responsible for the patients’ symptoms.
5. Explore whether the build-up of lymphatic fluid and the formation and fibrosis of adipose tissue play important roles in the disease cycles of Ehlers-Danlos Syndrome, fibromyalgia, and ME/CFS
In addition to studying the formal overlap with lipedema, research is needed on whether the build-up of lymphatic fluid and the fibrosis of adipose tissue might play important roles in the disease cycles of people with EDS, fibromyalgia, and ME/CFS. This topic merits a column of its own, but I briefly describe below five questions to consider in future research.
A. Could the build-up of lymphatic fluid be contributing to intracranial hypertension? The lymphatic system of the brain is called the glymphatic system and was only discovered in 2012. A recent study found that patients with idiopathic intracranial hypertension have impaired glymphatic function. The exact mechanism for the impaired flow of lymphatic fluid in the brain is unclear. The authors “suggest that in IIH pathological alterations at the glia-neuro-vascular interface may restrict transport of fluid and solutes along perivascular pathways and to and from interstitial tissue via astrocytic inter-end feet gaps.”
Peter Wostyn hypothesizes that impaired drainage of cerebrospinal fluid plays a central role in both ME/CFS and Long COVID. In Long COVID, he suggests this may be due to damage to olfactory sensory neurons and infection of lymph endothelial cells.

An adipose (fat) cell. Could fibrosis of fat cells be obstructing lymphatic flows in ME/CFS and other diseases?
Since we know that adipose tissue fibrosis obstructs the lymphatic flow in other parts of the body, this seems like a mechanism worth exploring for the glymphatic system as well. Our personal experience suggests that the bridge of the nose may be one area to focus on; massaging of this area has led to reductions in the symptoms of intracranial pressure in my daughter (as well as fluid draining down the spine and throat). The cribriform plate, which is behind the bridge of the nose, plays an important role in the drainage of cerebrospinal fluid. Could the blockage or impairment of drainage at the cribriform plate contribute to increased intracranial pressure?
B. Could fibrotic adipose tissue be contributing to some of the inflammation and MCAS experienced by people with ME/CFS and EDS? Researchers have found that people with lipedema have excess interstitial fluid, possibly related to dysfunctional microangiopathic blood vessels, which may be a consequence of a connective tissue disorder like EDS. As described by researchers, this excess fluid generates hypoxic conditions at the cellular level, which leads to inflammation: “When excess fluid is present, [loose connective tissue] becomes compliant, allowing more fluid to collect, stimulating proteoglycan synthesis. Excess fluid limits cell access to oxygen resulting in hypoxia, inflammation, and fibrosis.” This book chapter provides a more complete description of the process by which lipedema may lead to hypoxia.
Could the hypoxia from fluid inundation be a significant contributor to the inflammation and MCAS experienced by people with EDS, ME/CFS, and fibromyalgia? Among other evidence that is consistent with this hypothesis is the finding that adipose tissue leads to increased levels of IL-6 cytokines in people with impaired lymphatic function. IL-6 levels also tend to be elevated in people with ME/CFS and fibromyalgia.
C. Could the build-up of lymphatic fluid be contributing both to widespread pain and some of the neurological symptoms attributable to median arcuate ligament syndrome (MALS) and thoracic outlook syndrome (TOS)? Earlier in this article, I describe how the use of manual techniques adapted from lipedema treatment has substantially reduced my daughter’s pain in areas that were painful when touched. While the precise “etiology of pain in lipedema is unclear,” I would propose, based on my daughter’s experience, that there could be at least two distinct mechanisms at work: the first is the build-up of lymphatic fluid that causes nerves to be impacted when touched; the second is pain from fibrotic adipose tissue.
Is it possible that some of the pain currently associated with central sensitization or small fiber neuropathy is due to the build-up of lymphatic fluid or the fibrosis of adipose tissue? Similarly, could the build-up of lymphatic fluid be contributing to the compression of nerves seen in the neurological manifestations of MALS and TOS? We had reached the point of researching surgeons for these conditions before we discovered techniques to drain lymphatic fluid, which have helped to significantly ameliorate the symptoms prompting this investigation. Notably, MALS occurs near the cysterna chyli (largest lymph node in the body) and TOS occurs near the point where all lymph travels to drain.
D. Could excess lymphatic or interstitial fluid be responsible for some of the symptoms associated with post-exertional malaise (PEM)? In July 2020, following a trip to the hospital to get an MRI, my daughter experienced a major crash from which she has still not fully recovered. The incident left her with a feeling of “awfulness” throughout her entire body that was incredibly debilitating – one of the worst sensations she has ever experienced. We have since come to recognize that this sensation is related to the presence of excess lymphatic/interstitial fluid in her tissues that responds to manual lymphatic drainage and squeezing, which leads to substantial improvement.

Could excess lymphatic fluid be causing the poisoned feeling that some experience with post-exertional malaise?”
For a long time, we thought her experience was anomalous, but as I have read more about PEM, I have come to believe that at least some other people with ME/CFS are going through similar experiences. For example, I have seen descriptions of PEM by people with ME/CFS on Twitter as feeling like every cell in your body is poisoned – a description my daughter strongly identifies with. Similarly, the literature on PEM notes that there is often a delay of hours between exertion and the onset of the horrible feelings associated with PEM, which my daughter also experienced. The whole-body shaking my daughter experienced after the delay has apparently also been reported by others. And of course, the increased discomfort that my daughter experiences with exercise is widely reported by people with ME/CFS.
Could some of the symptoms of PEM for some individuals with ME/CFS be related to excess lymphatic or interstitial fluid that literally drowns the affected tissue, resulting in hypoxia and inflammation? This could happen through several potential mechanisms. One possibility is that exercise causes an increase in the leakage from microangiopathic blood vessels that occurs in people with connective tissue disorders, perhaps through a short-term increase in blood pressure; as one study notes, “[s]ystolic blood pressure (BP) normally rises with exercise as cardiac output increases during exercise in responses to the increased demand of oxygen from working muscles via increased sympathetic tone.” (Could this tendency for leakage be related to the reduced endothelial function observed in people with ME-CFS?). Increased fluid volume from elevated estrogen, cortisol or medication/supplements could potentially exacerbate the problem by increasing blood volume and pressure (leading to increased leakage from blood vessels) and by increasing the overall amount of lymphatic and interstitial fluid. Exercise could also cause joint dislocations that lead to the release of additional interstitial fluid.
Another, more dramatic possibility, is that a mast cell reaction causes the release of inflammatory mediators that increase the permeability of blood vessel walls (increasing the leakage of fluid) and possibly impair the functioning of lymphatic vessels as well (inhibiting the uptake of fluid). This could happen for any number of reasons, including mast cell reactions to perfumes or mold or dislocation in the spine that increases intracranial pressure. A biphasic mast cell reaction could explain the delay that is often seen before the onset of severe PEM.
(More speculatively, could a virus or other pathogen cause endothelial damage / dysfunction in blood vessel walls and lymphatic vessels – either directly, as in the case of COVID-19 or indirectly, through a cytokine storm or other overactive inflammatory response—in people with a connective tissue disorder, laying the groundwork for the leakage of lymphatic fluid and resulting experience of PEM at the onset of post-viral ME/CFS?)
E. Could some of the benefits attributed to vagus nerve stimulation stem from stimulation of the lymphatic system? Like many others, my daughter derives benefit from some of the techniques that are said to stimulate the vagus nerve, such as deep breathing, singing, and stimulating conversation. We have begun to wonder, however, if some of these benefits may be due to stimulating the lymphatic system to more efficiently remove excess fluid, rather than, or in addition to, stimulating the vagus nerve.
For the most part, these are unproven hypotheses that need evaluation through further research. My point in raising them is not to suggest they are all fully accurate or to suggest that the lymphatic system or adipose tissue fibrosis explains all the pathologies of EDS, fibromyalgia, and ME/CFS. Rather, I seek simply to suggest that these are additional avenues that merit exploration – in addition to and in conjunction with other inflammatory processes and abnormalities related to the spine, mitochondria, and blood.
As connective tissue disorders like EDS affect every system of the body, it should be unsurprising that they affect the lymphatic system as well.
Acknowledgements: This article benefited from review and comments by a number of reviewers, including Danielle Ayers; Elke Christ; and Karen Ashforth, MS, OTR, CLT-LANA, Board Certified Lymphedema Therapist; Clinician, Consultant, Educator. In addition, the article benefitted from research citations shared by Elizabeth Swope.
[1] Jeffrey Lubell is the parent of a teenager with chronic illness. He is not a doctor and does not have medical training.
Health Rising’s BIG (little) Donation Drive Update
Thanks to the over 160 people who have contributed to Health Rising’s year-end donation drive!
Health Rising has probably left some bruised egos out there. We’re constantly getting requests for guest blogs but we turn almost all of them down. Why? Because we’re looking for well-researched blogs that open up new areas of ME/CFS, fibromyalgia, long COVID, and other diseases – and those don’t come often. When they do, though, they can be inspiring, informative, and sometimes hard-hitting.

Keep the guest blogs coming – support Health Rising
Over 70 people have contributed blogs to Health Rising over time. Guest blogs from the last year included: Jeffrey Lubell (Could High Dose B-1 Help?, this lipedema blog, Brendan (The Coronavirus Vaccine: Is There a Better Way?), Amber Ella (Are We Failing People with Extreme ME/CFS?), Jeff Wood (Is ME/CFS be a Chronic, Ongoing Brain and Spinal Cord Injury Exacerbated by Exertion?), Michael Sieverts (A Science Insider Takes an Inside Look Nath’s Long Covid Study), Art Mirin (The Education of an ME/CFS Advocate), and Dorothy Wall (Review of “Sick and Tired: Intimate History of Fatigue“)
If these are the kind of blogs that support you – please help Health Rising keep them coming – and support us.






For me, regenerative medicine is the only way out if this. It’s clear there are many faults in the collagen. Everything else is downstream
I’ve been having prolotherapy/PRP for my overstretched lacks ligament/tendon’s. How would these injections work for lipedema?
Thank you so much for this.
After 40 years of Lipedema which had spread all over my body I saw a magazine and finally understood what it was. The Lipedema predates my ME by around 5 years.
In my area if England I was able to get a diagnosis but treatment is difficult to impossible given the complications of having ME and house or bedbound. Support stockings (tried many kinds) were problematic. Massage not affordable. Self massage causes PEM. Skin brushing has the best results for me at home but causes PEM in other than small amounts.
I bought a machine which inflates in my legs which has some small useful effect and no PEM for me.
There is a UK charity and a Facebook page for support and ideas. They are a nice bunch.
Hi I’m in the UK what charity and Facebook page please?
Wait I can go to a regenerative medicine doctor? Will my insurance cover this?
I wish we made the very clear distinction of Hypermobile EDS (hEDS) from the other EDS types.
With time, most likely, it will come to be known that it is not even EDS…
The EDS society has said that there was an intention to give this a name, so that patients could have some validation of their experiences in the medical sphere. (When EDS type III changed to hEDS / HSD)
It has happened before: former EDS type IX, with the advent of molecular testing was found to be a defect in copper gene and moved to be part of the Menkes family of disorders, as Occipital Horn Syndrome (OHS).
Plenty of other diseases present with joint hypermobility and the multisystemic symptoms of hEDS (fatigue, allergies, pots, hypoglycemia, etc):
hypophosphatasia, the homocystinurias, congenital adrenal hyperplasia – X…
Most rheumas and EDS ‘specialists’ are not aware of these, and it does happen that some are being misdiagnosed with hEDS when it’s one of the above.
Also, you find joint hypermobility left and right in East Asian populations. There is something about the diet of these groups and effects on metabolism…
I agree KayT: I’m not hyper mobile, however my joints pop and click to the point of people commenting and I have other symptoms of EDS. Hoping diagnosis and treatment options will evolve.
Jeffrey Lubell: Through your writeup I realize I have lymphedema (I thought is was natural body changes from me/cfs related decreased activity). Now to find some self treatment options….
Your daughter is fortunate to be under your care, and in sharing your research you’re legitimatizing me/cfs. Thank you!
Glad to hear the write-up provided useful information. I hope you find treatment options that are helpful!
You just validated what a member in a different Facebook group said… Asians are known to be hyper mobile!
I noticed her daughter was doing horrible party trick in a folder and made a comment. Thought she might want to have some attention of the hyper mobility,I noticed her daughter was doing horrible party trick in a folder and made a comment. Thought she might want to have some attention of the hyper mobility, and associated conditions. She had no concerns, claiming that’s what is common in her Chinese ancestry.
Lately I have been thinking hEDS might be what they call ME/CFS when it happens to people with joint hyperlaxity…
Joint instability is altogether a different issue. And a person can have both. And also have only one without the other.
And ME/CFS seems to affect joint stability and proprioception.
I experience it that way. At my worst, I was very clumsy and joints not where they should be. As I get better, diminishes drastically.
Hypermobility by itself doesn’t have to be an issue nor indicative of pathology. It gives many dancers, athletes and musicians an advantage.
People from India also tend to have supple joints. I don’t think it is a coincidence that yoga originates in this culture…
I have CFS/Fibromyalgia, hypermobility, proprioception defects, Multiple Chem Sensitivities, and I am generally ill. I knock things all over the bathroom and kitchen, which is very frustrating. Do you have any suggestions on how to handle all these problems? Particularly proprioceptive problems? Is there a clinic in California where I could be evaluated? I had not heard about a link between proprioceptive deficits and the other problems. I am a retired physician, and am now so limited in what sorts of activities I am able to do.
Hi Sandy – I’ve found that getting out of the stress response totally stabilizes my joints and I’m not clumsy. It’s like flipping a switch, on/off. The first time I noticed this was when I took a large dose of pregnonelone to deal with something else. I found Ray Peat’s work very helpful in figuring out how to get out the stress response, and improve my metabolic function and hormones. It can be different for each person; the basic principles apply to all. There is a website with many free articles and some books up on the internet free archive
This is a reasponse to Sandy S. Here are some resources that could help you locate a clinic or doctor that might help. http://www.dysautonomiainternational.org/page.php?ID=14 and https://www.healthrising.org/forums/resources/categories/doctors-finding-a-doctor-your-doctor-visit.201/ . Hope you are able to find someone who can help.
KayT — you make excellent points, especially about the diet of East Asian populations. Diet, pathogens and DNA — shouldn’t that be the starting point of investigations?
I’ve seen multiple “rheumas” and you’re right, they don’t know homocystinuria (et al). But that is only one component of my condition, and I’m diagnosed with hEDS plus a long list of comorbidities. That’s the nature of a syndrome, right? It’s a conglomeration of diseases.
Misdiagnosis happens across every field of medicine, even within the same field/bodily system. It’s not profitable (or easy) to thoroughly investigate and consider all possibilities. Also, medical researchers need a better depository of knowledge to redefine how diseases/disorders are connected, labelled and treated — with a holistic approach.
Side note: This article mentioned nearly all of my conditions and made some intriguing and helpful connections! No wonder I’ve so much inflammation!! I hope lipedema surgery helps rewind some of the damage. I’ll have to switch to a Japanese diet! Yum.
It still blows my mind that us patients have way more insight into this condition than the so called experts.
I’ve seen eds ” experts” in the UK who don’t make the connections.
I really think relengthening telomeres ( already possible) and eventually hopefully crispr to target these genes as well as stem cells to further strengthen and repair collagen.
Obviously anything is welcome but long term surely this has to be the way s cure is made
I too hope for a genetic cure someday for my daughter and others. In the meantime, I’m focused on how to help address her symptoms.
Any progress made here. I’ve been given telemere supplements (?) but still have lipedema. Very stretched out skin in thighs even though I weigh 130 lbs and weight lift.
Interesting, 20 years with ME/CFS and fibro. I got so sick from a lymph node that died before I was believed and treated.
Thanks for sharing. Hope you find strategies that help alleviate symptoms.
Jeffrey,
This is a beautifully researched and wide reaching article. You pull together myriad angles that I’ve not seen connected before. As a CFS/ME patient and a CranioSacral therapist I am right there with your hunches and their interconnected web. Your daughter is so fortunate to have such a dedicated, curious and perceptive dad.
Another tool for keeping the lymph moving that I find helpful is a Rebounder. Mine is a Bellicon and I love it. Between that and Qi Gong I am able to live a somewhat functional life. I realize not everyone can tolerate rebounding.. for those who can it is worth a try..
Thank you for the feedback. Good to hear that I may be on the right track. I’ve heard from others as well about the importance of rebounding. My daughter has craniocervical instability, however, so likely cannot tolerate it. Glad it has been helpful for you!
This all rings true for me. I have also discovered my own massage techniques that reduce face pain around the jaw line. Also upper arms and legs. I have often thought about a vessel leakage theory with exercise as I get temporary swelling at back if knees and inner elbows with a crash. Movement is good however. The root cause is elusive though. Also I was one of the many people who was exercising heavily at a time of hormonal change at onset
Thanks for sharing your experience. Glad you have found some techniques that are helpful!
Wow! I have never known or understood what all of the knots under the skin on the sides of my legs were. I never knew why I experienced such severe pain in my upper arms when touched. I have very large areas of swelling around lymph nodes above my clavicle. I finally I have a name – lipedema. Diagnosis without treatment is cold comfort.
Hi Donna. This sounds a lot like my daughter’s experience. Hopefully, you will find someone who can help While there is no cure for lipedema there are treatments that are helpful. We have been able to treat the pain successfully, at home, with some coaching from professionals. Good luck!
Please, please, please research the above! My mom has lymphedema and on kidney dialysis now. I have chronic EBV, EDS, pots like syndrome, migraines, fibro, etc.
Massage really does help… and of course I have to run and void afterwards, every time, which tells me, yes, it is helping. I get worried when my ankles swell up.
I wouldn’t be surprised, salt disregulation, Lipedema, and maybe even Diabetes Insipidus or something similar. How does one get dehydrated while drinking lots of water (and numerous trips to void), etc. and no diabetes? Confirmed I have no diabetes, abdominal ultrasound, just enlarged liver (fat intolerance? time will tell)
Glad to see this article pop up. If I end up having Lipedema like my mom, then my worries are for my child and her children. My DNA shows I have a very, very old blood line and my tree is huge, which means if this is genetic, there could be very, very many of us out there, and this is not going away any time soon, not for generation to come.
I grew up “very underweight” and skinny people are laughed away if you complain you gained 10 lbs out of nowhere. Now that we skinnies gained weight, still, not taken seriously, just lose your weight gain and all will be fine. Hmmm. I’ve seen both sides of the weight coin. Clearly there is more going on with us all.
Protocol of questions asked to patients seriously needs to change. Lipedema needs to be caught early, in childhood, so as hopefully not to lead as painful a life.
Thanks so much for the article and I am crossing my fingers that those medical issues mentioned in the above article get a serious look.
Thanks for sharing your experience!
Hi
Thank you for this article , Jeffrey.
I also have lipedema, me/cfs, pots etc.. and suspected h Eds.
I have come to know that my mother has lipedema, and she is hypermobile too.
I suspect me of having autism too. Sadly, no or few current research tries to connect these diseases.
Research on lipedema shows small bloodvessel leaks, know as microangiopathy. Also mastcells have been found and inflammation in fat tissue.
Other research shows perivascular spaces around capillaries in fat tissue in lipedema, perivascular spaces, and spaces between collagen fibers in the dermis. These perivascular spaces are thought to exist in EDS people. ”The ability of dermal fibers to separate may be a marker of a hypermobile connective tissue disorder such as the hypermobile Ehlers Danlos hypermobile spectrum disorder”
Source:
Interstitial Fluid in Lipedema and Control Skin October 2020Women s Health Reports 1(1):480-487
DOI: 10.1089/whr.2020.0086
In van Elzakkers research he demonstrates enlarged perivascular spaces in brain of me/cfs.
My question is, is the same process occurring in the legs also taking place in the brain ? Are the small bloodvessels in the brain leaking, is microangiopathy in brain happening and does this contribute to loss of white matter as other me/cfs brain research have shown? Can mastcell degranulation due to mcas or hereditary alpha tryptase (high levels of tryptase, platet factor 4 etc) be the cause of dysfunctional small blood vessels? Stanford doctor found platet factor 4 as biomarker for lipedema.
It is said that lipedema is a lymphatic disease. Is the lyphmatic system in the brain of me/cfs affected? and how does this connect to connective tissue diseases like EDS.
These are some observations and questions I also have gathered this Year. I have shares these thoughts on perivascular spaces with van Elzakker. But no reaction.
Lots of great questions. Thanks for sharing your thinking. Researchers have found problems with the lymphatic system in the brain (the glymphatic system), which contributes to intracranial hypertension. I’ve been focused on improving the drainage through of CSF through the cribriform plate, but it’s an interesting question about whether there might be other damage. I think you’re on the right track in suspecting that mast cell activation contributes to endothelial dysfunction in blood vessels and thus more leakage. Hope you continue your research and help us make progress in addressing these chronic debilitating conditions.
Hello Jeffery,
Thank you for this excellent post. Do you have a way to share the massage techniques you use on the nose/face for drainage?
I’m in the midst of being worked up for IIH and/or a CSF leak. I’m 31 years old. I have hEDS, POTS, MCAS, ME/CFS, Small Fiber Neuropathy, and Endometriosis.
I would like to run your techniques by my doctor and try them! I get a lot of squeezing and pressure behind my nose especially. It’s not sinus congestion…it’s like the pressure in my head is not right. Among a lot of other symptoms I won’t list out.
Rachel this is a late reply to your comment, and not from Jeffery sorry but I want to mention that Ray Perrin’s nasal release exercise has been very helpful for me. It increases the lymph flow out from behind the cribiform plate. It takes up to 7 minutes to get a release initially but after a week or so it takes more like 1 minute.
There was a recent paper: “Nasopharyngeal lymphatic plexus is a hub for cerebrospinal fluid drainage” that seems to support Dr Perrin’s approach.
I’ve only skimmed the article so far and plan to reread in depth, but already I’m astounded by all the points that ring true for me. #1 is the mention of joints popping out and rib pain. I’ve been to 4 doctors so far this year just about that, and none mentioned lipidema. The only healthcare professional who did notice was my chiropractor, who said the lower right rib had popped out of position and she would then pop it back into place. But it never stayed for long—and now that I’ve read about swollen lymph nodes, it makes perfect sense. My chiro would also work on my neck and back (because of previous car accidents) and always noticed knots in the muscles of my back. Now I’m wondering if those ‘knots’ could be enlarged lymph nodes. How can a layperson tell the difference? I guess professionals can. In any case, manual therapy (massage) is key—for me, anyway. I’ve known that for 20 years, but insurance stopped paying for it about 15 years ago. If you don’t have a family member at home (willing) to massage your back and shoulders, the buildup and pain just gets worse.
My overall body pain (diagnosed years later as fibromyalgia) started when I was pregnant, so I believed fluctuating hormones as the cause, but I was also diagnosed with serious edema in third trimester which I dismissed because the visible ankle swelling went away after delivery. Now I wonder if having had—being prone to— edema is relevant and should be added (again) to my health history. (I have moved a lot—including UK & Germany—and though I always brought all my medical records with me, not all were really transferred when I requested, or made the transition to electronic medical records (EMRs) when health systems updated or changed their software. I am still fighting to get dx’s added.) My guess is that hormones and genetics trigger edema—and possibly lipidema? Much to study.
I never really gave much thought to the lymph system except for that time of month when menstruation began, because a ‘marble’ would always appear under my right lower jawline. I knew it had to be a lymph node, but just always thought it meant my resistance was at an ebb. Since menopause, that marble has never reappeared—but my resistance to disease has obviously waned, because I was recently diagnosed with a rare form of cancer, medullary thyroid carcinoma (not pertinent to this discussion). It was detected at first in a normal X-ray, then in a CT scan, then an ultrasound, then biopsied in another U/S. Then the surgeon ordered another U/S scan, a mapping of the lymph nodes of my neck. Thankfully those were clear and normal—probably thanks to my chiropractor who always does her little trick to drain the lymph nodes in my neck and ears at the end of every visit. But the rib pain persists. So maybe it’s time to bite the bullet and pay out-of-pocket for a full/body massage focusing on lymph nodes—especially in the back. Easy for those flush with funds; not so easy for those living alone on a fixed budget.
My deepest gratitude goes to this author who has obviously put in many hours of thought and research then the writing of this extremely helpful article. Thanks too to Cort for sharing it with us. It astounds me too that a layperson has managed to make a connection that has eluded MDs. Your daughter is incredibly lucky to have a father willing and able to persevere in his quest for answers! Thank you SO much for sharing.
My pleasure! I’m glad you found the article stimulating. Thank you for sharing your story as well. It’s so helpful to learn more about others’ experiences. (And not TMI!)
PS: My heart goes out to your daughter who has so much to deal with at such a young age. I hope she is getting answers and the relief she needs.
PPS: Sorry for the length of my first response! Probably “TMI”…
I should have said (in my first Comment): “that has eluded_most_MDs”. I too hope more research is done on the lipidema-FM-CFS/ME connection. For the record, I too have been diagnosed with CFS/CFIDS, aka CFS/ME, and POTS/OI/NMH (back in the mid-‘90s). Along with many other conditions, probably not relevant to this discussion.
Very interesting article that prompts a couple of thoughts. The feeling of being poisoned and the painful patches described by Jeffrey’s daughter in those very specific locations were also significant for me in the early days (+30y).
I had the Perrin Technique from Raymond Perrin with significant success over a two-year period. Prior to this I made strict dietary and lifestyle changes, which started to make a difference; the addition of the Perrin Technique propelled me to normal living again, which my doctor had told me would never happen as I had become too debilitated. That was the first ten years.
I experienced a brief glorious recovery, but serious assaults on my immune system (typhoid, Lyme & co-diseases, hep b vaccination etc) brought me back to living in my bedroom. I now live alone in a rural area where I cannot access a Perrin Technique practitioner and I don’t have anyone to support the strenuous home treatment it requires for success.
I can say that I never again experienced the lymphatic engorgement that made it too painful to hug my children and made wearing even loose clothes painful. The ‘pizza face’ acne on my chest and back cleared completely never to return. These are all signs that my lymphatics had remained healthy following the Perrin Technique twenty years ago,
Now dizziness from POTS, chronic and acute pain from EDS and mast cell flares dominate, although I wonder if the Perrin Technique might deal with the latter.
It is sad that Raymond Perrin will probably achieve retirement before his particular insight is properly investigated, despite his unstinting efforts to get NHS approval. Every piece of the jigsaw needs to be examined to get the full picture. He stumbled upon his approach when working as an osteopath to athletes (osteopath to junior olympics or something similar) and noticed that those athletes who had ME all had a series of body characteristics in common, ( lymphatic engorgement, stretch marks, flattened thoracic spine etc) that made sense to him as a physical therapist. At the core of this was the unhealthy condition of lymphatic fluid that his treatment seeks to correct. I believe he has some recent ideas about how the blood brain barrier can be breached through (I think) various sinuses. Maybe an interview with him would be worthwhile.
I also believe that adipose is an important factor. A lightbulb moment for me early on, was learning that when the body is overwhelmed by toxic waste that it cannot fully process, it protects the organs etc by storing the excess toxins in adipose to deal with later.
This made sense to me as I suddenly put on 3 stone when I first became ill, which was unusual for me then, but no amount of calorie control would shift it. I eventually lost that excess fat over a two year period, identifying which foods and activities my body seemed to regard as toxic and avoiding them. Significantly during this time, when I had unexpected flare-ups for no discernible reason it was always linked to weight loss, the released adipose freeing its toxic load into my bloodstream making me feel rotten.
Jeffrey has written more than I can read right now, but his insights are important as this is the lived experience that a lot of us recognise, that are clues to the nature of our disorders, but is rarely validated by our physicians
Thank you for sharing your experience, Rosemary. Very helpful to learn of your success with the Perrin technique and subsequent history.
Fascinating – great catch Jeffrey. One of my first signs of this disease, which came after a flu vaccine, was increasing fatigue, facial flushing, and a swollen watery abdomen (where I’d always had a very flat stomach previously). I was otherwise very thin, followed finally by pleuro-pericarditis. When in hospital for repeat pericarditis, where they put me on steroids after my 2nd occurrence within a week, the most noticeable (and wanted!) result was that my belly immediately went back to normal. Yay!! (Sadly, that wasn’t to last)
The first hospitalization they gave me antibiotics and an IV drip, and then finally discharged me with a belly so bloated I looked and felt (and walked) like a 7 months pregnant mother-to-be. Interestingly, when admitted my veins were so collapsed they had to get a specialist from the cancer ward to get an IV in me – for whatever that’s worth. So I obviously have some issue with fluids.
After my third bout with pericarditis (after tapering prednisone) and ‘successful’ treatment with NSAIDS and colchicine (successful meaning no more ‘myocardial infarction’ readings on my ECG but too ill to work or even do most tasks of daily living) I was ‘cured’ – meaning don’t bother the doctors any more with this. But the lipedema slowly but constantly increased, where I am now regarded (disregarded more like) as ‘obese’. But my face, hands and feet remain thin, but apparently that’s an unimportant detail.
BTW, Cort I believe the photo Wikimedia is using is incorrect. That is a photo of the stages of lymphedema (affects one side only, men as well as women), as opposed to lipedema that Jeffrey is discussing here. It wasn’t until I came across this article that it started to make any sense to me, and I assume others will also be confused by the distinction between the two conditions: https://lipedemaliposuctioncenter.com/difference-between-lipedema-and-lymphedema/
Thanks for sharing your experience, Anne. And thanks for the heads up on the photo. While I didn’t discuss in the article because I want to do more research on it, I have heard a number of reports of lipedema getting worse in people with a connective tissue disorder following surgery or other hospitalization. This merits further follow-up as it is a serious complication.
Thanks, Anne – that photo was my mistake – the correct one is now up. 🙂
Thanks for the great article. My original diagnosis was Intracranial hypertension. I had much success with lymphatic drainage, based on a you tube video, which really helped to lower my pressure. Ultimately the diagnoses continued, fibromyalgia, MCAS, ME, POTS. I’ve been evaluated for CTD, but no clinical findings. I do not have lipedema, but I can relate to much of the pain your daughter experiences. During a flare, I have flu like toxic feeling and swelling. Less edema like and more like third spacing. I read the Perrin technique but there are no practitioners in my area. I utilize craniosacral therapy and fascia work and it’s helpful. I wish you the best with your search to find answers.
Thanks for sharing your experience. I hope you find additional treatments that can be helpful. We do our treatments ourselves, at home, with periodic online coaching from trained therapists. I’ve also noted that there are therapists who specialize in manual lymphatic drainage and lymphedema even in my remote corner of the U.S. (eastern Vermont), so that could be an additional option at some point. Perhaps there are similar resources near you?
Hi Jeff, have you heard of backmice.info? A researcher and ER doc in Spain is researching the history and treating the herniation and edema of fibro-fatty nodules. Sacro-iliac nodules can cause possible cluneal nerve entrapment. Of course, fatty nodules elsewhere can cause the symptoms you describe throughout the body. Those of us taking guaifenesin for fibromyalgia notice first an initial decrease in spasm and fluid around nodules, followed by a decrease in the nodule size and related pain over time. Thank you for this important article and all the best to you and your daughter.
Very interesting! Thanks for letting me know about this site. It looks intriguing. At first blush, it sounds like this may be a related phenomenon to what I review in this blog post, but I will explore further to learn more.
Great article, I’ve been a big fan of the Perrin Technique and it’s helped me massively when nothing else will. There’s certainly lymphatic dysfunction in CFS so it’s puzzling why researchers aren’t pursuing more concrete testing and trials when we have a lead.
I also wish that researchers would analyze the HOMES of people with CFS (ie elaborate testing for mold, dust, viruses, formaldehyde, drywall dust, etc), which may be at the SOURCE of the problem if people with CFS are more sensitive to everyday contaminants without knowing it. To date, 100% of CFS research has just been testing of the patient themselves but never their environments.
Glad to hear the Perrin Technique has been helpful. I do hope we can encourage more research on lymphatid dysfunction in CFS. Hearing from you and others that this is an important issue is important for encouraging researchers to focus more attention on this system. Appreciate also your point about analysis of the Home environment. Certainly important for asthma and likely also for MCAS. I am hopeful that perhaps reducing the fibrosis of adipose tissue could reduce inflammation in the body and cause the body to react less to these stressorts, but this is just a hope at this point; we need some solid research on this question.
I want to thank you, Jeffrey, for solving a mystery about a condition my grandmother greatly suffered with that I can see in the photos must have been lipedema. I forwarded your article to my geneticist because my description of her legs didn’t register a specific condition. I commend you for hoping these different specialties will come together with greater focus on connective tissue disorders.
I have EDS, ME/CFS, and MCAD, and like Jeffrey and others have wondered what the discovery of the glymphatic system might say about our conditions. Could viruses spread there and evade detection with blood tests? How does this system work in faulty tissues disorders like EDS as compared with healthy controls?
Thank you for this thoughtful, reasoned, well-researched article, Jeffrey. Your daughter is fortunate to have such a caring and engaged father, though I’m sorry she has suffered so. Hoping for better for her and all of us ahead.
A very useful knowledge about diseases.
The hypothesis of impaired glymphatics/lymphatic congestion as underlying CFS is gaining traction:
https://www.frontiersin.org/articles/10.3389/fncel.2022.888232/full?fbclid=IwAR0EahK0-ESXiguOBVQRHzWs9nArHRn9S6w2ynT6_hYFter4hxscB1Uzz78
Your daughter may also benefit from taking the supplement pycnogenol, particularly if she also has varicosities. It has been shown to help increase vessel wall resistance/decrease extensibility, which can help the venous system which the lymphatics drain into.
This is also interesting:
https://www.mdpi.com/1422-0067/23/6/2975
In my experience the only thing that has helped is surgical removal of the lipedima. I have had many flab removals that will never firm up with diet ad exercise and never returned after surgery. I should never have waited so long but then, I did not know what was happening to me and no diangosis yet of heds,mcas,pots
Did you pay out of pocket?
Have you looked into CIRS (chronic inflammatory response syndrome)? There are a lot of similarities. Dr Andrew Heyman is a good source on youtube and website.
Experience traditional manual therapy in Brampton, ON at New Hope Physiotherapy. Our skilled therapists provide personalized care for optimal recovery.
Phone: 905-846-4000 Email: admin@newhopephysio.com web: http://www.newhopephysio.com
Thank you for sharing your ideas. Every comment makes a difference, and we’re glad to hear from you. Your support helps build a better, stronger community.
There was a study last year regarding the comorbidity of lipedema and fibromyalgia finding that 35% (!) of lipedema patients met the criteria for FM. It also concluded that the patients with lipedema had significantly worsened FM symptoms and lower QoL. I know this is an old article but I think it’s definitely relevant to this matter!
Here’s the study: https://pubmed.ncbi.nlm.nih.gov/38127646/
Thank you for this insightful article highlighting the connection between lipedema, lymphatic system issues, and conditions like Ehlers-Danlos Syndrome, fibromyalgia, and ME/CFS. It’s encouraging to see the emphasis on manual lymphatic drainage and massage techniques as effective treatments. For those seeking additional support in their recovery journey, Vita Bella Health offers tailored injury and recovery solutions, including therapies designed to enhance healing and restore vitality.