

The autonomic nervous system has two (or perhaps three) branches. All may be off in ME/CFS/FM.
Autonomic nervous system problems of one type or another appear to be ubiquitous in chronic fatigue syndrome (ME/CFS), fibromyalgia (FM), postural orthostatic tachycardia syndrome (POTS), and long COVID. One place they show up in is something called low heart rate variability (HRV) scores that are indicative of an overactive sympathetic nervous system (SNS) or fight/flight response.
Low HRV has been found in many diseases including ME/CFS/FM and its cousins (Gulf War Illness), irritable bowel syndrome (IBS), postural orthostatic tachycardia syndrome (POTS), as well as cardiovascular diseases, anxiety, depression, Parkinson’s disease, epilepsy, and others.
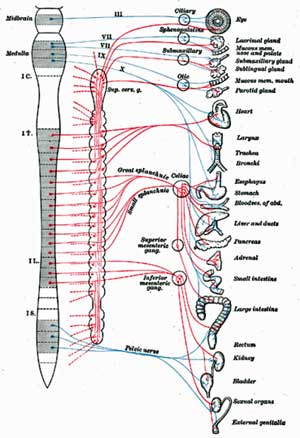
Because the vagus nerve controls the activity of the sympathetic nervous system, the SNS dominance seen in ME/CFS, FM, POTS, and similar diseases may be less a function of an overwrought SNS and more a function of an underactive vagus nerve.
Because the vagus nerve is such a ubiquitous nerve that does so many things (relays sensory signals to the brain, affects motor functioning, reduces inflammation, alters neurotransmitter levels, reduces gut permeability (leaky gut), promotes neuroplasticity), stimulating the nerve could potentially have profound effects.
Andrea Parker Gives Vagus Nerve Stimulation a Try

Andrea Parker described her results from her vagus nerve stimulation trial as “mind-blowing.”
All that led Andrea Parker, an Australian occupational therapist with a severe case of ME/CFS, to give vagus nerve stimulation a try. She found that it helped, shared her story with others, and then presented her findings at a 2019 ME/CFS South Australia Inc. seminar.
Andrea’s bout with glandular fever/infectious mononucleosis several years prior may have set things up. Thirteen years later, a stomach bug combined with stress left her with a case of “post-viral fatigue” and a three-month layoff from work.
It wasn’t until three years later, though, when too much exercise combined with stress left her with severe ME/CFS and knocked her out of the workforce for 15 months, that she said she really “got” what ME/CFS was. On her worst days she said she felt like she was dying – and noted that was a descriptive term – she actually had the feeling that her body was dying.
She’s much better now – is working again – and was at the seminar to share what helped her get better. She made it clear that she is not a doctor, is not claiming any new treatments or cures for ME/CFS, and requested that everyone check with their doctor before trying any new treatments.
The general timeline of her partial recovery was:
- May 2012 – severely ill, 15 months off work.
- Nov. 2012 – supplements began to improve her health
- Sept 2013 – She began a graded return to work and was able to slowly build up her hours up over time.
- 2019 – at the time she trialed tVNS she described her ME/CFS as moderate. The tVNS got her into a mild/moderate category.
She believes the problems with the autonomic nervous system (ANS) play a major role in ME/CFS/FM and similar diseases.
Two Theories of Illness
Two theories of illness undergird her understanding of what happened.
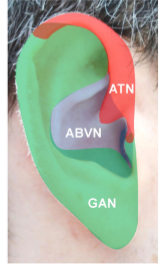
Non-invasive vagus nerve stimulation stimulates the vagus nerve via a device that clips onto the ear.
Bob Naviaux’s cell danger response (CDR) theory asserts that low levels of ATP production in the mitochondria are associated with an autonomic nervous system in a fight/flight threat response.
As classically understood, the ANS is composed of two circuits: (1) the sympathetic nervous system (SNS) or fight/flight circuit that arouses the body for action; and (2) the parasympathetic nervous system (PNS) or rest and digest circuit that calms the SNS down – allowing the body to rest and restore itself.
Stephen Porges’ Polyvagal Theory of illness, on the other hand, posits that the ANS has three circuits, not two. Besides the two circuits noted above, Porges believes a freeze/faint immobilization circuit is present.
Parker showed a fascinating chart from Babette Rothschild, a trauma specialist who has embraced Porges’ system, which depicts how symptoms change as the fight/flight system becomes more dominant.
- Active Alert Phase (SNS 1) – the moderate levels of arousal at this stage leave the muscles toned, breathing, heart rates and blood pressure increased. Feet feel cool, digestion slows, emotions like anger, shame, excitement, anxiety show up, and contact with others is “probable”.
- Fight or Flight (SNS II) – high levels of arousal result in tense muscles, faster heart rate, elevated blood pressure, cold hands and feet, and a complete stoppage of digestion. Emotions like rage and fear show up, and contact with others is limited.
- Hyper-freeze (SNS III) – muscles are rigid, tachycardia and hyperventilation occur, blood pressure is very high, extremes of cold/heat are felt, emotions like terror show up, and contact with others is “unlikely”.
Does What Happens in Vagus Stay in Vagus?
Parker’s goal was to take her system out of fight/flight, and in so doing, reduce inflammation, improve her ability to exercise, help her gut, improve her sleep and cognitive functioning, and so on.
Her question was whether she could use a vagus nerve stimulation device and other treatments to communicate messages of safety to the cells (e.g. the cell danger response) and potentially improve their energy production.
The Parasym Stimulator
Two forms of vagus nerve stimulation are available. An implanted version has been approved for use in the U.S. for epilepsy and treatment-resistant depression, and non-invasive stimulators which latch onto the ears are available in some countries.
In Australia in 2019, Andrea had her choice of three VNS stimulating devices that were available (Parasym, Nemos, Gammacore). She chose Parasym. Parasym had the advantage of not requiring a prescription, was at $1,200 actually cheaper, and simpler to use than the others. Parsym also provided a frequency and recommended duration (30 minutes AM/PM) for people with ME/CFS and was considered a relatively low-risk device.
(Parasym devices are available in the UK and European Union and Australia but not in the U.S. or Canada.)
Andrea Parker and Vagus Nerve Stimulation – the Short Version
Her Self-Trial
During her self-trial, she assessed her response using the Modified Fatigue Impact Scale. Overall, her score dropped from 40/84 to 20/84 – a 50% improvement in 8 weeks – something she described as “kind of mind-blowing”.
She experienced improvements in almost every area, and in some that were surprising. Besides improvements in thinking, malaise, exercise without PEM, pain in her hands, anxiety, and feeling stronger, she reported that her vision improved, that she could better handle noisy, highly stimulating environments, and that – she said with a big smile – her agility and ability to play the piano greatly improved.
She still has IBS, but her symptoms have improved and using the VNS device has started her gut moving. Neither her insomnia nor her tinnitus improved. (Parasym has, however, a tinnitus protocol which she has not yet tried.)
The only noticeable side-effects were weird bleeding episodes (nose, butt) and some bruising after about a month.
The Friends Trial
The results, she said, kind of fairly well “blew her brain” and she started communicating about them. After she found five friends willing to try the stimulator, she used Dan Neuffer’s ANS Rewire Questionnaire as the MFISM to assess the results. She noted that this was not a clinical trial and no conclusions can be drawn from it.
Of the five, none had the dramatic results that Andrea did. Looking at all three scores, one person had about a 15% improvement, another a 25% (ANSRO), and another a 25% improvement (MFIS). The other two had negligible improvements.
Those who did improve tended to experience reduced cognitive fatigue, reduced pain, light, sound, smell hypersensitivity, improved bowel symptoms, less IBS, and increased activity levels.
One person improved quickly, then ramped up her activity levels and crashed. She ended up being a non-responder who might have ended up as a responder had she taken it easier.
Andrea Parker and Vagus Nerve Stimulation – the Long Version
Improving Heart Rate Variability (HRV)
Andrea’s attempt to improve her heart rate variability level, and thus calm down her sympathetic nervous system or fight/flight response, led her to try a number of options that ended up helping. Her supplements began her partial recovery process. They included:
Fish oil – has been shown to enhance parasympathetic nervous system activity and it started her recovery. (SelfDecode recently reported that for some people with CRP gene variant, omega-3 fatty acids are effective for reducing anxiety. This is because high CRP levels produce inflammation and anxiety and omega 3 fatty acids can bring them down.)
Healthy diet and probiotics – L rhamnosus (Bioceuticals Ultrabiotic 45) – a probiotic – that is also believed able to affect HRV – produced a massive improvement in mood/cognitive functioning. She noted that it was very expensive and did not work when she was severely ill, but afterward it was very helpful.
Stress management – slow breathing and meditation with longer out-breaths helped. Since inhalation actually stops vagus nerve activity, holding your breath (as I know that I’m prone to do) jacks up the fight/flight response. The rest and digest response, on the other hand, is activated during the out-breath. (Andrea suggested trying breathing in for four counts and breathing out for six). CBT and acceptance commitment therapy helped to calm her system down as well.
Exercise – if safe and done within the energy envelope (tai chi, yoga, others), exercise can improve vagus nerve functioning.
Improving Her Low Energy State
To treat her low energy state, Andrea reported that she took lots of supplements, Vitamin D3 drops taken through the tongue, did cognitive rehab (brain HQ) – only if you have the energy to do it, as well as setraline (Zoloft) for anxiety, zolpidem tartrate and zoplicone (Imovane) for insomnia.
Improvements Using the HRV and Energy Enhancing Treatments
Andrea went from severe to mild/moderate ME/CFS. Besides the other improvements she noted with the vagus nerve stimulation, her severe and frequent migraines virtually disappeared, her anxiety and mood problems improved significantly, her sensitivities were reduced, her mild autistic traits (which she didn’t know she had) improved, and her hair stopped falling out.
She still has ME/CFS but is obviously much improved.
Vagus Nerve Stimulation Survey
Andrea didn’t stop with her five friends. She teamed up with Dawn Wiley, the founder of the Facebook Group “A Vagus Adventure AVA” and Physio for ME’s Dr Nicola Clague-Baker at the University of Liverpool to develop a survey of TNS effectiveness in ME/CFS.
If you have ME and have experimented with vagus nerve stimulation, please take the international survey.
Vagus Nerve Stimulation – the Future
Clinical Trials
Suffice it to say that many disease groups are interested in using vagus nerve stimulation to calm the sympathetic nervous stimulation down and reduce inflammation, improve gut functioning, reduce anxiety, improve neuroplasticity, and so on.
One person with extreme fibromyalgia benefited greatly from invasive vagus nerve stimulation. Several fibromyalgia studies that are, or have gotten, underway include Norwegian, a Turkish one, a U.S, and a large Spanish/German one. Several POTS vagus nerve studies are underway at the University of Oklahoma. One long-term study reportedly found that while “progressive global improvement” had occurred, significant symptom burdens remained. A shorter trial found increased HRV and improved norepinephrine levels.
No ME/CFS studies were found, but Sjogren’s Syndrome study did find that non-invasive VNS markedly reduced fatigue, improved immune functioning, and reduced pro-inflammatory cytokines.
The Gist
- Andrea Parker was battling ME/CFS as an occupational therapist when she decided to try vagus nerve stimulation and tame the fight/flight response she believed was depleting her energy, causing her cognitive, gut, sleep and anxiety issues, and other symptoms.
- The vagus nerve regulates the functioning of the fight/flight response which heart rate variability studies in ME/CFS, fibromyalgia, POTS, and many other diseases indicate is hyperactivated. Given the many systems of the body (immune, cardiovascular, central nervous system, gastrointestinal) the vagus nerve effects, trying to plump it up a bit in order to knock the fight/flight response down makes perfect sense.
- Andrea’s bouts with glandular fever/infectious mononucleosis, a stomach infection, and overwork/overexercise had landed her out of the workforce for an extensive period of time. She used other treatments to turn her severe ME/CFS into moderate ME/CFS and was back at work when she decided to try the vagus nerve stimulator
- She used a fatigue questionnaire to assess how effective the Parsym device (available in Australia/the UK) was. Her score reflected how she felt – a 50% drop in most of her many symptoms – a result she called “mind-blowing”. The only symptoms that didn’t dramatically improve were her insomnia and her gut symptoms.
- Of the five friends who replicated the trial three produced significant benefits (@25% improvements) and two did not.
- Andrea and others have created an International ME/CFS Vagus Nerve Stimulation Survey to see how others are doing.
- Vagus nerve stimulation trials are currently underway in fibromyalgia and postural orthostatic tachycardia syndrome (POTS) but not to my knowledge in ME/CFS.
- Andrea also listed other treatment approaches she used to tamp down the fight/flight response and improve her energy. She is now well but has vastly improved.
- With the National Institutes of Health (NIH) and private industry pouring money into mapping the peripheral nervous system and devising devices to manipulate it for better health, the future of this kind of stimulatory technology – whenever it shows up – appears to be bright, indeed.
Improved Devices
A recent review of the field suggested that the vagus nerve stimulation field is rapidly evolving, and that different forms and techniques are being developed. The review noted that the idea of using non-invasive approaches to stimulate the vagus nerve only first emerged in the early 2000s.
Newer, non-invasive ear-based vagus nerve stimulating devices called “closed-loop” devices, which adapt rapidly to changing conditions, could offer a more personalized approach. These devices would employ biofeedback to adjust the amount and frequency of stimulation present to keep the vagus nerve functioning at an optimal level.
SPARCING Vagus Nerve Stimulation Breakthroughs?
These awards have the potential to catalyze next-generation neuromodulation therapies that could bring improved specificity for patients over both drug therapies and previous-generation devices.” SPARC Program Manager Gene Civillico, Ph.D
The NIH’s Stimulating Peripheral Activity to Relieve Conditions (SPARC) could go a long way to improving vagus nerve stimulation. The $250 million 10-year initiative is largely engaged in funding basic research that will illuminate how the peripheral nervous system – of which the vagus nerve plays a large part – works and devise better ways to treat it.
The VNS technology available now simply stimulates a big nerve that engages in a multitude of activities. Fully harnessing the power of this complex nerve (the neck area of the vagus nerve contains over 100,000 fibers) is going to take some work, though, and significant resources are going to map in, fine detail, where the vagus nerve goes and what it connects to. Besides placing the stimulation more precisely, researchers hope to be able to determine which patterns and frequencies of stimulation work better.
Once researchers know which fibers stimulate which organs, more powerful and precise devices can be developed. One study, for instance, is mapping the vagus nerve projections to the brainstem – a possibly key area in ME/CFS. A Colorado team is developing an optical or light probe that will not only be able to report on the activity in the different branches of the vagus nerve but determine which stimuli can activate them.
Gut problems can be amongst the most difficult to fix in ME/CFS/FM and almost half of the SPARC-funded studies will focus on the “second nervous system” — the gut.
One will map the vagus nerve innervation in the small intestine to learn how it affects gut motility and functioning in hopes of finding new ways to treat the pain associated with irritable bowel syndrome and other “sensory” gastrointestinal disorders. A New York team is developing a wireless tool to monitor the activity of vagus nerve endings that innervate the gut.
Another study right up the ME/CFS/IBS alley found that epithelial cells lining the gut are – in response to the release of ATP – turning on the sensory nerves. Those activated sensory nerves, in turn, may be causing the mysterious gut pain that’s present even when no signs of inflammation are found. Another study with obvious IBS/ME/CFS connection attempts to determine how secretions from cells in the bowel are able to turn on pain pathways in the brain in IBS.
Others
In “A Spark in the Periphery” Emily Walz reported that GlaxoSmithKline and Verily Life Sciences (formerly Google Life Sciences) are pumping more than $700 million into a company, Galvani Bioelectronics, that will develop miniaturized electronic devices for peripheral nerve stimulation. DARPA, the Defense Advanced Research Projects Agency, is getting into the act as well, devoting $90 million into the hunt for better electroceuticals.
Conclusion
Theoretically, attempts to boost parasympathetic nervous system activity in ME/CFS and FM make sense and anecdotal reports suggest that it may be helpful for some. Vagus nerve stimulation research is in its infancy in ME/CFS and fibromyalgia, but with the international survey and fibromyalgia clinical trials underway, we should have some idea of its effectiveness in these diseases in the relatively near future.
As Andrea Parker demonstrated, other means of boosting vagus nerve activity and taming the fight/flight response can be helpful. A blog on using breathwork and other approaches to try and get the vagus nerve back on track is coming up.
With hundreds of millions of dollars being pumped into bio-electroceutical research by the NIH and private industry, future devices – whenever they come – should be more precise and more powerful.






Time for me to get out all my articles on stimulating the vagus nerve. I have collected quite a few, especially on how to hack a TENS device. Ultimately I never tried it because there can be some issues with the vagus nerve controlling heart rate which can be potentially dangerous. If I remember correctly, the left ear is ‘safer’ than the right–but I need to go back and confirm. Also precise information on what settings to use was a bit vague–probably because they really aren’t well researched/known yet. Last I looked there were ear pieces available on the Internet.
Will do some homework and get back to report.
Also there was some very early research (1970s?) on the use of vagus nerve stimulation in the treatment of achalasia–some experiments apparently quite successful. Achalasia is a very rare condition (1 in 100,000) of the esophagus. Of course along with EDS and ME/CFS, I have achalasia too! ;-( This means I have no peristalsis and my lower esophageal sphincter does not open properly. It works more like an eye dropper which means everything I eat sits in the esophauntil it drips, drips, drips into my stomach. That can take hours and if I eat too much, then it’s vomit, vomit, vomit.
Do hope more is done to study this very important organ!
Oh, terrific! (The research, not your horrifying condition.) I look forward to your post.
Lots of interest in the vagus nerve.
My sister has this. By any chance, can you make tears? What helps the best for you?
Nancy B. I highly recommend that you join the Facebook group mentioned in this article which is run by Dawn Wiley–A Vagus Adventure”. There are many folks, Dawn and much more recently myself, who have been using TENS units for Vagal Nerve Stimulation. There you will find information about the settings, etc. You are correct…only the LEFT ear for the ear clips.
Have the Parasym, have used it daily for two weeks. No result seen. It would be useful to try and know how the progression for improvement works; how many days to see a little change, and how many more for a bit more, etc. Severe ME patient.
How did you get the Parasym?
You order the unit from the Parasym company. Parasym.co
Assuming you are not in the US? Parasym claims they do not send to the US?.
Helen, it’s very personal. I had impact on my environmental sensitivities from my very first session. Other impacts took longer to develop.
Also, when you use it and for how long makes a difference. For my gut, it works best when I use the Parasym during and after eating.
There’s a lot to learn about how best to use vagus nerve stimulation, hence the survey to find out what people with ME/CFS are doing with it.
Later, there will be a somewhat similar survey for people with fibromyalgia who use the Parasym.
Hopefully, from the ME/CFS and fibro surveys, we’ll have a better sense of what is and isn’t working for people.
I was really interested in the help the stimulator had with Andreas problems with stimulating environments. I don’t really have that but help with environmental sensitivities would make a huge difference for me.
Penelope, I am very grateful for your comments. When you say ‘when you use it’ and ‘for how long’ I am not sure how one determines things. I use the Parasym for 1 hour as indicated in the manual. Do it after breakfast usually lying down. Interesting idea there, of doing it during and after eating. Where else can I look to get more ideas how to use this device. The parasym manual doesn’t really go into treatment issues. I am rather lost, truth be told. Any further advice is most welcome. Thank you
Do you know if this can be ordered if you live in the U.S.? I’m not having any luck on their website.
A simple “cheat” to stimulate the Vagus nerve (which I’ve found helps especially with my GI symptoms), is to perform a low humming sound through your vocal cords. I think this comes from the old Tibetan monk chanting meant to help with relaxation that we’ve made fun of at times. The Vagus nerve runs along the side of the neck, so if you can cause enough vibration in that area, it theoretically would “stimulate” the nerve and thus the autonomic system. And it’s free, although you may get some funny looks from those around you at the time!
Interesting. There are all sorts of kind of odd things suggested to help the vagus nerve. Glad it helps and thanks for sharing that 🙂
I researched VNS alcoves, when I was in moderate category. Now relapsed back to severe, writing things only way I have memory. I have to ” tame” it back to moderate, and since I have the double whammy of severe with NO caregivers, my focus is trying to eat and sleep where neither is functioning…
I hope to get well enough to find VNS and it will go in my documentation of 20 years from diagnosis of ME
Peter Levine suggests this technique too for calming fight or flight.
The vagus nerve is powerfully stimulated through cold. Turn up the cold water, pour it into face a couple times, then let it run over the sides of your neck, alternating (the vagus nerve runs right where you feel the carotid pulsating). All this takes just a few minutes. Can do it 2 or 3 times a day. For me it works well.
I also use a tVNS but from the fact that I have gradually skipped more and more sessions I deduct that I am not that confident that it makes a large difference.
Well, I’ve just ordered one! Excited to see if it makes a difference. I need something!
#severeME #FND #fibromyalgia
That’s really helpful to know! Thanks! The sensitivities to heat, light and sound are the features I’d like to try it for.
I’ve used the CES Ultra external VNS for a couple years. I use it in the morning while I meditate. I’ve notice increased calm and increased HRV. I don’t clip onto my ear, I use electrodes on my neck. It’s not a cure-all for me. But I’m moving for incremental gains.
Incremental gains are great..
Where on the neck are you placing the electrodes, Leadelle? I think I might try what you’re doing. Thanks.
It’s great there is also a clinical trial underway to study Vagus Nerve stimulation and Ehlers Danlos. The official title of the study is “Hypermobile Ehlers-Danlos Syndrome: Efficacy of Non-invasive Vagal Nerve Stimulation and Effects on Brain-Gut Physiology”. The estimated completion date of the study is June 30, 2023.
https://clinicaltrials.gov/ct2/show/NCT05212129
Good to hear! Thanks Kyn 🙂
Has Andrea been able to sustain her improvement with the Parasym since 2019? Sometimes what we believe initially to be a panacea turn out be another “placebo effect” disappointment.
Dawn Wiley has had significant improvement over several years of use. Consider joining her Facebook group for more information and support. I believe that Andrea has also been able to sustain her improvement. However, not everyone benefits or has a sustained benefit. Everyone is different. Some are very sensitive even to the lowest settings. Others tolerate it very well and want “more power”. The key is to start “low and slow”. Eventually stepping up (or down for the very sensitive) the duration and intensity until you find your “sweet spot”.
A couple of years ago I came across a book called “Accessing the Healing Power of the Vagus Nerve” by Stanley Rosenberg. It combines Stephen Porges’s Polyvagal Theory with Rosenberg’s many years experience as a craniosacral therapist. He describes a few simple exercises to stimulate the vagus nerve. I have much less brain fog and some improvement in PEM since doing his basic exercise every day. Most people with ME can do it as it mainly involves eye movements and can be done lying down. It might be a cheap way of seeing whether stimulating the vagus nerve could help before investing in expensive equipment. A word of warning, the basic exercise made me feel hideously nauseous to begin with and I have no idea why. It meant I could only hold it for a second at a time! But I persevered with it and gradually the nausea disappeared for good.
I also think it’s interesting that Rosenberg notes that whenever he finds a client has vagal nerve dysfunction, he also observes that they have an upper cervical misalignment. Maybe there’s a link between vagus nerve dysfunction and cranio cervical instability? Rosenberg says that the basic exercise helps to bring the C1 and C2 vertebrae back into alignment, which often corrects the vagal dysfunction. He also says that the basic exercise improves blood flow to the brain stem, which has a positive effect on the vagus nerve. I often feel a tingling sensation in my head after doing it and I feel less clogged.
I can’t say it’s the most readable book and he only mentions ME/CFS in passing but I found it worth getting for the exercises at the back. It also made me think about the position of my head and improving my posture as a way to increase blood flow to my brain stem and vagus nerve function.
Thank you for your recommendation. I’ve googled it and for those too ill to read a whole book, there seem to be also Youtube videos which can be found by searching for “basic exercise stanley rosenberg”. I might try this.
I bought a nervous vague tens. Only to see that I can not use it (was paper with warnings with it) because of a neck operation with a lot of metal in. A whole plate with screws over C4-C5 and bone from the bonebank. A friend of mine who’s englisch is better, wrote to parasym with my problem and got an answer from: yes you can use it, no you can use it not, go see the specialist. first of all I am severe bedbound. second of all, here in Belgium, who would know anything about it… Here it is still not ME but cfs and get and cbt and falls beliefs. hey would call me totally crazy!
but i really hope the future brings scientific good things that even coul be done here in a hospital.
Hi Konijin!
I decided to try a device my son found online called a Xen by Neuvana
a bit less expensive and available in north america
I asked for a discount code- was told GETXEN- gets you $40 off
no clue if this will help just saying it is easier to get and seems to do the same thing
Does anyone have experience with the Nervana Device?
Do you mean Neuvana? I checked the Facebook site mentioned in the article, A Vagus Adventure–Dawn Wiley, and there were two entries last fall from folks who tried it. They wanted it to work, but found the instructions & guidance to be insufficient and returned their units. Perhaps the company provides better information now.
Well done Andrea Parker. This is so similar to the work I have been doing for the past 18 years. I got 40% improvement from using the microcurrent device called the Alpha-Stim which enabled me to return to work as an occupational therapist. I did a similar trial with 18 members of our support group of people suffering from ME/CFS and FM. 83% found significant improvement I believe from similar points that Andrea noticed in the calming of the ANS. The difference is the Alpha-Stim can also help with insomnia. I agree with Andrea there is hope. I have now retired and I wish Andrea all the best in her work.
Linda, A few of the folks on the Facebook group “A Vagus Adventure-Dawn Wiley” have asked about the Alpha-Stim unit. Because of its expense, most folks there do not use the Alpha-Stim, but some are interested in it. Would you consider joining the group and adding your experience? Most of the folks use a Medfit EM3600A and some the InTENSity micro combo and a variety of others. Your experience and voice would be appreciated.
Please add Parasym to my comment. The comment should read: Linda, A few of the folks on the Facebook group “A Vagus Adventure-Dawn Wiley” have asked about the Alpha-Stim unit. Because of its expense, most folks there do not use the Alpha-Stim, but some are interested in it. Would you consider joining the group and adding your experience? Most of the folks use a Medfit EM3600A, Parasym, some use the InTENSity micro combo or a variety of others. Your experience and voice would be appreciated.
Hi Linda, thanks for sharing your experience and for your encouragement. I have an Alpha-Stim device which, as you may know is cranial electrotherapy stimulation, a little different to trancutaneous vagus nerve stimulation. I can only tolerate a low setting on this, which means a 1 hour treatment time. I can’t really do anything whilst using it (other than relax) because it makes me feel drowsy. As such I haven’t really found it helpful because it takes a big chunk out of my day.
With tVNS I can do activities during stimulation and it actually improves my clarity of thinking. This makes it easier to integrate into my daily routine. TVNS can improve sleep for many people and it is indicated for treatment of insomnia. Unfortunately it hasn’t done so for me. It’s great to hear that you got such great results with your own trial and yes the principles are similar. I’m sure the people you have helped are very grateful. Enjoy your well-earned retirement!
Hi Andrea, sorry for writing so late, I discovered this only now. Quick question: Does Alpha-Stim help with insomnia and what are the best settings/tim in your experience ? I joined the Facebook group recently, but found little info on the Alpha-Stim, so any input is useful to me. Thank you !
I think this is such an important area that Andrea Parker is focusing on. I’ve also found that calming down my sympathetic nervous system, whilst trying to enhance my parasympathetic nervous system, has been crucial to the progress I’ve made. I feel the freeze response is something I’m familiar with too. In the last year or so I’ve noticed that at times I too can hold my breath – this is outside of my consciousness and I only became aware of it because I caught myself doing it and then wondered how often it happened.
I’ve also noticed that if I irritate my stomach (gastritis) or my bowel (IBS) then this can set off my sns and irritate my brain. I wasn’t sure what pathway was responsible for this response. I came across this talk by Michael VanElzakker hosted by the American Society of Gene + Cell Therapy, which is 26 mins long, in which he talks about the Afferent and Efferent Vagus nerve, connecting the brain and the body, which possibly explains what’s happening with me. It’s a really interesting talk, which is relevant to this blog. It’s initially about Long Covid but he talks about ME/CFS and many other conditions. It’s packed with information, some of which I didn’t grasp but I still understood a good bit of it.
Considerations when developing ‘Long Covid’ therapeutics Michael VanElzakker PhD
https://www.youtube.com/watch?v=bLATy1SiwN0
I am so pleased to read this Cort and Andrea. I have had problems with my vagus nerve and parasympathetic nervous system for many years. My brilliant sacro-cranial osteopath is able to switch it back on at monthly treatments.
I have noticed an extremely low HRV, wake in panic every morning(physiological)
During a recent ME/CFS research programme where I was doing a standing test for 20 minutes my oxygen level fell into the 70s a couple of times prompting me to purchase a pulse oximeter. I suspect that I hold my breath unconsciously and note that my night time oxygen levels fall continuously into the low 90’s despite good daytime levels.
So this is very timely and I will look further into this. Many thanks
I’d really be interested in trying this, however it looks so highly priced for a small device. The latest quote on the Parasym shop website seems 599 Pound. Does anyone of you guys have up-to-date information whether there are comparable devices that may be cheaper?
Also it would be quite interesting in vagus nerve stimulation trials to ask participants whether they have symptoms that could be particularly indicative of an overactive sympathetic nervous system, such continuous feeling of being “wired/wound-up”, anxieties/high alertness, high sensitivities to environmental stimuli, and maybe fast speech?, and then pit that against individual trial results to see if predicting responders would be possible.
I am quite sure that my sympathetic nervous system is continuously overactive. I often feel like I am “humming” inside and have many environmental sensitivities.
For me it is the same: I’ve found that outbreathing calms me, but not classic inbreathing exercises like “breathe into your stomach”.
Does anyone know if the Parasym machine or the tVNS machine are more effective for CFS and depression.
I’ve bought a tVNS unit at £69.95. I will provide feedback
Thanks!
I wonder if my tDCS device for depression would do this as well. I use it on my temples now. The one currently on Amazon is called the Brain Driver. It’s different so I’m not sure it could be used for the vegas nerve. Hmmmm.
Tried the Basic Exercise by Stanley Rosenberg (used a 3:45 min Youtube video explaining how to do Rosenberg exercise by a channel called yoopod – Disclaimer: I don’t know this person). It does have some effect for me (I notice I get up more easily after doing it, as if muscles work better together?). As it takes very little time, can be done lying down and is a good pastime for those of us who have difficulty to “endure” necessary resting due to a wired-up feeling, I’d recommend giving it a try.
Also following discussion of fish oil in this article, I amped up on Omega 3 1000 (using a cheap brand from a German drugstore chain), and found it to have some calming and shielding effect. So I think it does strengthen parasympathetic activity. (Just a little worried whether my taking 3-4 times the normal daily dose of 1000 is safe concerning the Vitamin E added to make the fish oil effective?)
Other medication that I have found helpful in bringing down what is probably an overactive sympathetic nervous system but have seldom seen mentioned in ME/CFS blogs so far are low dose tricyclic antidepressants: Drugs like trimipramine have an established off-label use for inducing sleep without being addictive. It comes in a bottle as a 40mg/mg solution so it’s quite easy do dose single drops, with 1 drop corresponding to 1mg. I use 5-10 drops (5-10mg trimipramine) at night in combination with 0,5mg Melatonin. I drop directly into a mouthful of water 🙂 Currently I am trying an additional 10 drops (10mg) dose in the morning to reduce tension. I have also been using trimipramine (around 15-20 drops) during the day to help “take myself out of the action” so I can better tolerate doing nothing during an acute crash. I think my Dr mentioned that Trimipramine has an effect on stress system or central nervous system. I believe he said that in low dose range it induces sleep and will become more of an antidepressant in higher dose range. When I first started on it I had a huge reaction to only 3 drops (like walking through treacle) but that was only a brief initial effect.
I’m just curious as to why TENS units were not mentioned in this article. TENS is the only affordable option for regular folks and to my knowledge it does the same as a Parasympathetic device. Dawn Wiley was mentioned in the article and she uses a TENS.
I recommend joining the facebook group, A Vagus Adventure for more information. https://www.facebook.com/groups/492041135346672
This group has device information, settings, technical guidance, and how-to. In my quick scan, TENS units can be used if they meet the guidelines for lower power, low power increments and programmability. Per their recommendations, the devices need to start at low power (1ma) and have small (1ma) increments. Also, the device needs to be programmable, not just have “pre-set programs”. Any device that meets their requirements may work.