

Study suggests natural killer cells are whacking the small nerve fibers in fibromyalgia

Noting how much we DON’T know about FM, the authors explored the immune system – and appear to have hit paydirt.
After decades of surveying chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM) literature, the study, “Unbiased immune profiling reveals a natural killer cell-peripheral nerve axis in fibromyalgia“, counts as a big and potentially momentous surprise – and a very welcome one at that. Not that we should be surprised about being surprised in either FM or chronic fatigue syndrome. The authors point out with respect to FM, we really don’t understand what’s going on, and that lack of understanding has shown up in spades in the ineffectiveness of many FM drugs that the authors note fail to impart any “meaningful clinical benefit”.
So maybe we should look elsewhere, and that’s exactly what this Canadian-led international study did. Featuring researchers from Canada, Norway, Sweden, Turkey, the U.S., and Germany (including two major figures Nuncan Uceleyer and Claudia Sommers) this group eschewed the central nervous system and looked south to the body and a system – the immune system – that’s gathered more notice of late.
Then, instead of locking themselves down with a hypothesis, they opened things up with an exploratory “hypothesis-free, unbiased” multifactorial study featuring flow cytometry. In flow cytometry, individual cells are passed through a laser. Since each cell scatters the laser light a bit differently, researchers are able to quickly identify and assess the characteristics of tens of thousands of different cells in the blood.
Results
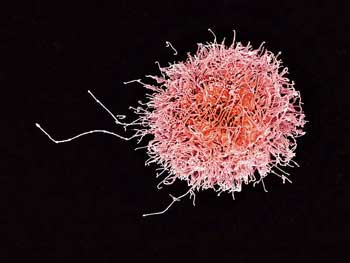
Instead of killing pathogens, are the NK cells in FM attacking the sensory nerves? (From Wikimedia Commons: CC-NHLBI)
I felt like rubbing my eyes. Natural killer cells? THE immune cell associated with ME/CFS? Possibly playing a major role in fibromyalgia? Yes! This unbiased study found that of all the immune cells assessed, natural killer cells (NK) were the ones that popped up.
Natural killer cell studies actually go way back in FM – they were first studied back in 1999 – but they’ve been kind of a sideshow in FM while they’ve been a major research topic in ME/CFS. We’re talking a couple of studies in FM versus dozens in ME/CFS over the years.
NK cells man the front lines of our immune defense – helping to hold the invaders at bay, while the big guns of the immune response, the T and B cells, gather their forces together. Reduced NK cell killing power or cytotoxicity has long been surmised to give pathogens quicker and deeper entry into people with ME/CFS.
This fibromyalgia study, though, could give NK cells a far more central role in these diseases. The immune system, with its multiple layers of defense, could potentially make up for some of the NK cell problems seen. This FM study, though, could link NK cells to the pain and sensory problems found in these diseases, and if Novak and Systrom find that the small nerve problems extend deeper to the autonomic nervous system nerves, to blood flows, gut problems, and more, that would be groundbreaking.
While a major subset of NK cells (D56dim) was depleted, the most significant finding was the reduction of a subset of regulatory NK cells called CD56bri. These cells have been implicated in a variety of pathological immune states including autoimmunity, neuroinflammation, cancer, and infection.
The CD56bri NK cells in the FM patients displayed a unique activation state: their cell surfaces had fewer CD16, CD226, and CD96 receptors, and more CD107are receptors. (The receptors found on the surface of a cell tell us what the cells have encountered and what the cells are up to. If a cell, say, has come into contact with a pathogen, it will display certain kinds of receptors that: a) inform the immune system, and b) enhance the cells’ ability to respond to that threat.
The NK cells in the FM patients appeared exhausted.
Fascinatingly, the authors noted that the CD56bri NK cells with this kind of expression are associated with “chronic activation and exhaustion”. That’s the same general scenario that’s been posited – not just for the not-so-deadly natural killer cells – but other parts of the immune system in ME/CFS.
Culture studies indicated that the FM patients’ NK cells were also “hyperresponsive”; i.e. when confronted with a challenge, they overreacted, producing significantly more of an immune factor called CCL4. They were also more likely to “degranulate”; i.e. release their cytotoxic stores into an infected cell to try and kill it.
This exhausted-but-hyperresponsive response sounds like nothing so much as an immune version of being “wired and tired”. The FM patients’ NK cells weren’t always “on” though. Perhaps because the downregulated CD16 receptor was found, they responded poorly when confronted with antibodies.
After two different analyses (pathway analyses of our RNA-seq transcriptomics data, GWAS-based genetic meta-analysis) in 2 other independent cohorts also found evidence of hyperresponsive NK cells, the authors undoubtedly felt quite good about their findings – and continued to dig deeper.
Next, they asked: if fewer than expected NK cells were present in the blood, did that mean they went someplace else? Could they have left the blood and traveled into the tissues – maybe even into the small nerve fibers that study after study has found damaged in a substantial number of people with FM?
With this thrust, they were exploring almost uncharted territory as few studies have explored the connection between NK cells and small nerve fibers. Knowing that NK cells get recruited to areas of damage by molecules called ULBPs that are produced by stressed or damaged cells, they looked and found higher levels of this substance in FM patients’ skin – and more NK cells around them.
The model – attracted by ULBP emissions from the nerves – natural killer cells gather around them and attack.
Now it was getting really interesting. Could NK cells in fibromyalgia be responsible for some of their pain symptoms? The authors popped in a rather remarkable connection – decreased levels of circulating NK cells have also been associated with ME/CFS (in one study) as well as a host of chronic pain states including chronic lower back pain, cluster headache, and vulvar vestibulitis.
Boy, do we need a new model of chronic pain – and we got one:
- Damaged or overactive peripheral nerves produce factors that draw NK cells to them like bees to honey.
- So many NK cells are drawn to these nerves that their levels in the blood drop.
- The NK cells then kill or tweak those nerves, producing the small fiber neuropathy seen in FM – as well as possibly in – ME/CFS, postural orthostatic tachycardia syndrome (POTS), and now long COVID.
The authors also produced an interesting side note: an increased expression of this NK attractant (ULBP) is found in FM whether or not small fiber neuropathy is present. This suggests that people with FM don’t need to have small fiber neuropathy for NK cells to be damaging their peripheral nerves.
The authors suggest these patients may be continually regenerating their small nerve fibers but are still experiencing pain because their nerve fibers are under constant attack. They also proposed that the waxing and waning symptoms sometimes found in FM – and one could certainly include ME/CFS here – could reflect this process of all-fiber dieback and renewal.
(One encouraging thing about small nerve fibers is that, in contrast to other nerve fibers, the body can regrow them: if they play a major role in FM, healing them could wipe it away).
The authors noted that the small nerve fiber/NK interaction could explain the skin issues sometimes found in FM including lichen simplex chronicus (one form of dermatitis), neurotic excoriation (skin picking), prurigo nodules (another form of dermatitis), pruritus Itching), burning sensations, and hyperhidrosis (excessive sweating).
The Gist
- Noting the lack of progress in FM, a Canadian-led international group of researchers took a new tack. Using flow cytometry, they took an unbiased look at the immune system.
- Out popped natural killer cells – THE immune cell in ME/CFS (!). The authors linked NK cells to FM, though, in a different and perhaps more fundamental way, than it’s been linked in ME/CFS. They propose that the NK cells in FM are attacking the small nerves, causing pain and other sensory issues.
- Finding reduced numbers of a subset of NK cells in the blood, the authors examined them and found that they appeared to be both “turned on” and exhausted at the same time; i.e. they appeared to be “wired and tired”.
- Speculating that the missing NK cells were somewhere else, they looked at the small nerve fibers that studies have found to be damaged in FM (as well as ME/CFS, POTS and long COVID) – and found NK cells gathering around those nerves in the FM patients.
- Next, they found that levels of an NK cell attractant produced by damaged nerves were increased in FM as well.
- With that, their model of disease was complete: damaged nerve fibers in FM are emitting a substance that’s drawing NK cells to them. The NK cells are then attacking the nerves, causing the nerves to disappear in a substantial number of FM patients – and producing pain and sensory issues.
- The inflows of NK cells to damaged nerves across the body is causing them to be reduced in the bloodstream. Interestingly, reductions in NK cells have been found in other chronic pain diseases.
- The fact that high levels of this NK cell attractant are also found in people with FM who do not have small nerve fiber damage suggests that this model could apply to everyone with this disease.
- The authors proposed that a latent, chronic infection, or an autoimmune process, is damaging the nerves in the first place.
- Systrom and Novak are looking to see if the small nerve damage goes deeper – thus damaging the nerves that carry autonomic nervous system messages. If it has, this NK cell model – if it extends to ME/CFS – could have widespread ramifications for both diseases.
- Some studies have found some issues – including hyperactivation – of these same immune cells in ME/CFS.
Conclusion
The idea that natural killer cells – long the object of study in ME/CFS – might be a major cause of pain in FM was a bit jaw-dropping. The authors, though, have produced a nice model: damaged sensory nerve fibers emit a substance that draws NK cells to them – and causes the NK cells to attack them – causing pain and sensory issues. Those NK cells appear to be on edge – and are ready to attack at the slightest provocation. The “wired and tired”, or exhausted, profile of the NK cells seems to fit well with what we know is happening in ME/CFS.
With so many possible factors present, it’s unclear which treatment possibilities would win out if this most intriguing research finding is validated, but they must include things like antivirals, autoimmune agents, and ULBP blockers.
This study will undoubtedly attract much attention and further studies. Every major advance – and let’s hope this is one – opens up more questions. Here are some.
NK Cell Attractant – We don’t know if the NK cell attractant (ULBP) that appears to be playing a central role, is causing, is caused by, or is simply exacerbating the nerve damage found in these diseases.
Cause of the Nerve Damage? – Piggybacking on that, we don’t know why or how the small nerve fibers are being damaged in the first place. Citing ME/CFS, the authors proposed two possibilities – a chronic or latent viral infection of the sensory nerves; or, citing the recent, exciting Goebel paper, an autoimmune process that’s been sparked by an infection.
Scope of the Problem? – Most importantly, we don’t know if the small fiber neuropathy (SFN) extends deep enough to affect the autonomic nervous system and blood flows. Being able to tie SFN problems to ANS problems and blood flows could conceivably revolutionize our understanding of these diseases.
How Many are Affected? – The fact that small fiber nerve damage might not need to be present for small fiber nerve problems to exist means these findings could apply to the entire ME/CFS/FM population. We need to know more about ULBP levels in these diseases.
Same scenario for ME/CFS and other diseases? – Is something similar occurring in ME/CFS, POTS, and long COVID? One ME/CFS flow cytometry study found increased levels of NKCD56 bright cells. Studies coming out of Griffith University, however, found reductions in this NK cell subtype, altered signaling, and increased activation levels.






where was this study published and who are the authors? Did I miss where it was documented? This sounds very interesting and hopefully they can find something to manage the disease if this proves to be one of the causes and this would be very helpful for me. Thank you for this explanation
You’re welcome! The study was published in the Pain journal and you can find it here – https://pubmed.ncbi.nlm.nih.gov/34913882/
Thanks, Cort — I found the abstract at that link but could not access the full article. Is there perhaps another link you might share?
Yes. Usually Pubmed provides a link to the free paper if there is one but this time they didn’t for some reason. I searched and wasn’t able to get it on Sci-hub but was then surprised and really happy to find the paper for free on the PAIN website.
https://journals.lww.com/pain/pages/articleviewer.aspx?year=9000&issue=00000&article=97873&type=Abstract
I have had FM for at least 20 years. This description of damaged nerve cells is exactly how it feels. It is also exacerbated by arthritis now.
I agree – it does feel like that.
It’s gone now but I have found a source. https://we.tl/t-b1wqFeeda8
What a fascinating study. I found it interesting that they mentioned skin picking. I’ve been picking my hangnails and adjacent areas for quite a while and here’s the funny part – I’ve believed that it’s a sign my body is trying to show me that I have a problem with my nerve endings. I view it as something akin to having an area on your skin that is itchy and our reaction is to scratch it. I don’t know if scratching an itch allows a substance to get released from our skin, but could skin picking be releasing the ulbp from the skin? Is this testable? This also makes me think of autistic children and their odd behaviors. What are their bodies trying to tell them?
I thought that was fascinating as well. Although there is no known cause for skin picking it’s classified as…what else? an obsessive-compulsive disorder. How much sense it makes that something might actually be irritating the nerves.
The skin issue I notice is burning feelings after exertion. I wonder what exercise is doing to the small nerve fibers in the skin and how it’s doing it. Lot’s to think about with this study. 🙂
The following are quotes from the book Trigger Point Dry Needling: An Evidence and Clinical-based Approach.
‘’Muscle referred pain may be accompanied by other symptoms, such as numbness , coldness, stiffness, weakness, fatigue, or musculoskeletal motor dysfunction. The term referred pain is perhaps not complete and a preferred term can be “referred sensation” as non-painful sensations such as burning or tingling would still be considered referred phenomena from trigger points.”
The fact that trigger points can cause numbness and coldness suggests to me that trigger points can cause damage to the nerves. They interfere with the local circulation.
“Muscle referred pain is a process of central sensitisation which is mediated by a peripheral activity and sensitisation and which can be facilitated by sympathetic activity and dysfunctional descending inhibition.”
Sounds like FM to me.
I was so shocked. I have Dermatillomania (which is a condition on the OCD spectrum), if this is related to my MECFS it would be mind-blowing
I have developed SFN in my hips (the side of my hips) on both sides. It really burns and is very numb. It’s getting much worse. I don’t know what type of doctor to go to. (I am so tired of all their abuse.) I have ME/CFS, FM and MCAS. Thank you so much for all the work you do Cort! It has been lifesaving at times…literally. Thank you.
PS. I would like to donate monthly but do not use my account at PayPal at all anymore. Is there another way?
You might try acupuncture. I found it helpful but it’s not an instant cure. Low dose naltrexone helps with nerve issues as well. Best wishes.
Sorry to hear that. Remember to feed your body ample nutrients to rebuild the nerves. The nerve nutrient particularly lacking in western diet is lecithin. This can be bought as a supplement.
Do any of the researchers in this study want to recruit real live FM participants? A lot of this makes sense to me and my experience. I am in Canada.
It appears that the participants came from members of the Association de Fibromyalgie du Quebec located in Quebec City. They have a nice website here – https://sqf.quebec/. Really good on Canada to support this work in so many ways. So did Germany, Norway and others. It was quite a group effort.
Very interesting. My daughter has severe me, fibro, SFPN, EDS etc etc – things are very dire indeed.. I’m so grateful for all research / studies so she can get her life back. One strange thing she notices is, when she itches it feels good, but afterward feels bruised. (Even a rub can do it..)
The Immune System is way smarter & more efficient than any doctor or scientist & it knows exactly what it’s doing: a pathogen has infected/attacked/infiltrated the small nerve fibers (& elsewhere), then IN REACTION TO THE INFECTION the immune system is going after those PATHOGENS (not the nerves) which are infecting the small nerve fibers—it’s NOT attacking the nerves for no reason, it’s attacking a prodigious major infection hiding in nerves—& unfortunately destroying nerve fibers and causing severe pain in the process (severity of destruction to nerve fibers is an indication of how severe the infection is).
‼️Just because doctors/scientists can’t figure out what the pathogen is that the immune system is trying to destroy, that does not mean it isn’t there or that the immune system is somehow malfunctioning or going haywire & attacking the nerves for no reason.
The NONSENSICAL IDEA that everyone’s immune systems are malfunctioning somehow resulting in AUTO-IMMUNE DISEASE IS RIDICULOUS. Basic common sense says THERE IS NO SUCH THING AS AUTO-IMMUNE DISEASE, THERE IS JUST AN AS-YET-UNIDENTIFIED PATHOGEN/INFECTION WHICH THE IMMUNE SYSTEM IS ATTEMPTING TO ERADICATE. If the body is attacking nerve fibers, then that’s where the infection is & where docs/scientists should focus their search for the pathogen.
🙂
We shall see about the pathogens! Particularly those in tissues that are hard to find. That description of latent, chronic viruses sure sounded like herpesviruses and there was that recent multiple sclerosis study where the authors came very close to saying EBV is causing MS.
There is also this thing called molecular mimicry in autoimmunity where the immune system attacks a part of the body which looks like a pathogen – but the pathogen has been eliminated.
Two good ideas to me. Hopefully one of them gets validated before too long.
Is there an antiviral for herpes virus? I definitely think I became ill after a virus where I also had my first cold sore, I was never the same again. My lip keeps tingling still years later but I’ve only ever had 1 more cold sore.
Is there anything worth a try for herpes virus?? Thanks
at the very least, you can try amino acid l’lysine-it helps herpesvirus as does monolaurin supplement
I find this interesting because I have had fibromyalgia for many years without major fatigue. In 2013 I had a mild virus and two weeks later I woke to pain everywhere and major fatigue. It continues to this day. I still haven’t had a diagnosis, however some testing has pointed toward sjogrens. I hope this study is followed up in a big way. Perhaps covid maybe useful in that it may encourage more studies.
There is certainly such a thing as autoimmune disease and it has been well studied for many years and the many different mechanisms of how it arises. I know because I have a PhD in Immunology and worked in a research lab for many years. I had autoimmune ITP when I was younger and 2 years later developed fibromyalgia, so it is quite realistic that fibromyalgia is a type of autoimmunity.
I agree. I has shingles 2 years ago on my left lower jawline. After receiving the \/ I developed burning sensations in my mouth as if there is shingles in there. My theory is the \/ woke up the virus that has laid dormant in that nerve now it misfiring.. The million dollar question is, how do I make it stop?
K.B. How right you are, everything you said is correct it is a pathogens or pathogens (virus or viruses) causing ME/CFS Fibromyalgia long Covid and all autoimmune diseases. Inflammation from the immune system response to the viruses is causing damage to cells and mitochondria .And also depleting the body’s natural anti inflammatory cortisol and inflammation becomes worse and blood pressure drops. One can only wonder why the Pharmaceuticals and Medical Profession do not peruse this. From my own research I have seen reports of people treated with HIV antiviral medications have had good results. Strange these medications can only be used for HIV.
Thank you for posting about this study, Cort, I find it really intriguing and that it might be connecting more of the dots we have been lacking. Hopefully this group will do further studies on mechanisms at play. My concern is in terms of therapeutics we can’t just block ULBPs as they play a necessary role in trafficking of NK cells that would likely leave people at a much increased risk of viral infection. However, it seems to me that other studies have pointed to the presence of autoantibodies in FM and all of this is painting a picture of autoimmunity. Whether the instigator is a previous infection is undetermined but if we can work out some of the upstream issues that might be a better place to target or re-purpose some existing therapies for autoimmunity. We know there is not necessarily overt inflammation happening so a lot of the current therapies for things like RA won’t help. Really hope this can open up more avenues around pathophysiology and better treatments!
I had a flow cytometry test recently but I don’t know how to read it. I am wondering if understanding my results in light of this article would help.
Did some digging on natural killer cells and ME/CFS. I might have missed something, but it appears studies have found a reduction of NK cells (natural killer cells) in individuals with ME/CFS. Initially that is what the researchers found in this particular study. But they were able to identify where those NK cells had congregated. Just wondering if prior studies on NK cells in people with ME/CFS that they missed a particular area of congregation too. Are NK cells really lower body wide in people with ME/CFS or they also somewhere else in the body attacking that area? This study certainly brings up more questions than it answers. I really hope we see good follow-up studies.
I’d be more than willing to take any experimental drug to read my body of this painful fiber myalgia chronic fatigue that makes my daily life so difficult
Kann mir das jemand ins Deutsche übersetzen bzw die wichtigsten Aussagen zusammenfassen? Danke
biene269@yahoo.de
Translate: Can someone translate this into German or summarize the most important statements? Thank you
Forscher können die Ursache für den kleinen Nervenfaserverlust bei Fibromyalgie haben. Es scheint, dass die beschädigten kleinen Nerven Faktoren aussenden, die natürliche Killerzellen zu ihnen ziehen.
Sie glauben, dass die NK-Zellen dann die Nervenfasern angreifen und Schmerzen und andere Symptome verursachen.
Zu den nächsten Schritten gehört die Suche nach der anfänglichen Ursache der kleinen Nervenschädigung und das Erlernen der Funktionsweise dieses Prozesses.
Researchers may have the cause of the small loss of nerve fibers in fibromyalgia. It appears that the damaged small nerves send out factors that attract natural killer cells to them.
They believe the NK cells then attack the nerve fibers, causing pain and other symptoms.
The next steps include finding the initial cause of the minor nerve damage and learning how this process works.
—————–
If you ever want to translate just go to google and type German to English and then copy/paste the paragraph into the window
Interesting that along with ME/CFS, FM, PoTs, I also have Burning Mouth Syndrome that my doctor says is small fibre neuropathy. This is the first time I have seen all of these conditions connected to small fibre neuropathy!
Burning mouth syndrome – ouch! It’s surprising how little is known about SFN – despite the many people that experience it. It may be different in FM as studies have shown disappearing small nerve fibers as well as narrowed ones. I think we’re going to learn a lot about this over the next couple of years.
My mouth starting burning, tongue swelling a little, changed from one side to the other until it covered the whole mouth. I had never heard of Burning Mouth Syndrome so I went to my dentist because I thought I had a tooth problem. A piece of my tooth broke off leaving it with a point. He took X-rays, & everything was fine. The dentist removed the point from the tooth. I came home feeling defeated as I have often felt with my FM/CFS. As usual I looked up qMayo Clinic & after some research I found Burning Mouth Syndrome. It truly does burn your mouth, & it took awhile to heal, eating soft food, eating on the side not hurting as much, etc. It finally healed & I just recently had another episode but not as bad. Thank God.
Interesting article and I wonder if it might explain Dercum’s disease and some of the other fat disorders linked to Dercum’s which form lipomas under the skin all over the body
Hi, I have ME/CFS and SFN, and my WashU test was positive for autoantibodies, TS-HDS and FGFR3, which means autoimmune-mediated SFN. I’m assuming these autoantibodies damage the small nerves which then leads to the ULBPs. It’s probably a chain of events and wondering if studies of these autoantibodies could be a place to start!?
Interesting – thanks Kerrie. I don’t know if those autoantibodies have been tested in ME/CFS.
For people with long covid:
https://www.gastrojournal.org/article/S0016-5085(22)00450-4/fulltext
Our results indicate that SARS-CoV-2 antigen persistence in infected tissues serves as a basis for post-acute COVID-19. The concept that viral antigen persistence instigates immune perturbation and post-acute COVID-19 requires validation in controlled clinical trials.
Alpha lipoid acid is good for nerve health. It works for the heel pain I get as a result of having Type 1 diabetes.
I started at 200mg per day and worked up to 600mg which takes away all the pain for 24 hours until the next dose.
Thanks for all your reporting!
Finally an explanation for the itchy skin problem I’ve had for the past year. Dermatologists have told me they can’t do anything about it. They prescribe compounded creams that help to relieve the itching but I have to apply it every day. Hope this study results in positive treatments.
Here’s saliva test for HHV6 that may show correlations between exacerbations in ME/CFS symptoms and increases in levels of HHV6 and 7. Why are there no big studies on this?
https://hhv-6foundation.org/all/levels-of-hhv-6b-and-hhv-7-dna-in-saliva-may-distinguish-people-with-myalgic-encephalomyelitis-chronic-fatigue-syndrome-from-healthy-control-subjects
I wonder what this would mean for people who have both fibromyalgia and ME/CFS, considering the findings for ME/CFS seem to show that there’s reduced NK cell function in that condition, which would be the opposite of this right? I’m not very good with the science so I might have it wrong.
Any specific immune modulation can help slow down the barrage of NK cells? ..to buy time to rebuild the tissues? What is driving NK cells? IgGs? …that is why we feel worse with immune stim herbs/supplements…but if one has reactivated viruses (herpes ebv, cmv, hh6)…and there are other pathogens …perhaps developing humoral immunity is important for balancing….
Does anyone know where to find this Goebel paper?:
“Cause of the Nerve Damage? – Piggybacking on that, we don’t know why or how the small nerve fibers are being damaged in the first place. Citing ME/CFS, the authors proposed two possibilities – a chronic or latent viral infection of the sensory nerves; or, citing the recent, exciting Goebel paper”
A blog on it is here
https://www.healthrising.org/blog/2021/07/02/blood-cause-fibromyalgia-autoantibodies/
I stepped over a doggy gate and pulled a muscle . I had pain from SI joints up to my whole back . My legs felt like lead. This pain was excruciating for 3 months and lessened . Every day I’m in pain .its been over a year now so I’m now diagnosed at FM. I had my first child 25 years ago . I worked with a specialist from Chicago who flew out monthly to CA . His name was Dr. Beer. He told me my NK Assay was the worse he saw but not to worry he’d work with me. He was wonderful . Fast forward I started thinking if my NK are a factor of getting FM?
Very interesting paper, and great to see they are linking into Goebel’s recent work.
Can anyone see from the supplementary tables if they screened thoroughly for Sjogren’s Syndrome in the FMS patients?
Thanks as always for the excellent work and clear explanation Cort
After reading this and suffering for so long it has given me hope, i believe this is the issue, and i tried predmisolone which has reduced my pain by 80% i had pain in every single muscle and joint and was basically house bound. now my muscles no longer have pain, i still have some knee pain and neck pain. but i am no longer house bound.