

A neuroglial hypothesis of ME/CFS from a pediatrician with ME/CFS and a leading glial cell researcher
Yet another fascinating hypothesis has come our way. Produced by a German researcher/pediatrician/author with chronic fatigue syndrome (ME/CFS) in collaboration with an internationally known glial cell researcher it’s yet another example of how richly the creative juices in our community run. Where else in the medical field are individuals so apt to buckle down, dig into the studies, puzzle things out for themselves – and come up with novel ideas?
Here is Dr. Herbert Renz-Polster’s story:
Dr. Herbert Renz-Polster
Six years ago Dr. Herbert Renz-Polster came down with ME/CFS. This year he published a hypothesis paper on it that’s received more views – almost 12,000 – than 92% of the papers published in that journal.
I am a German pediatrician, trained in the US, first @ Maine Medical Center, then @OHSU, Portland OR, where I did a fellowship in pediatric pulmonology. Back then I published my first scientific paper, on the relationship between mode of delivery and subsequent development of allergies (()). That was back in 2005.
Back in Germany, I worked at an academic public health institute (part of the University of Heidelberg), where we built up a pediatric section. Ten years ago I left academia and worked part-time as a pediatrician but also published popular parenting books, mostly based on evolutionary ethology, which I also explored scientifically.
At the end of 2016, I came down with a severe case of influenza from which I slowly recovered. Three months later after strenuous exercise, I literally crashed to a point where I could only walk a few steps, which brought me to the ER – and later an uneventful work-up with many specialists including neurologists, cardiologists, internists, etc…
Thereafter I had better days with hope and worse days with despair – I knew that I was ill but I did not know from what. To pay the bills I still went to conferences and talks etc. and crashed for days afterward. Eventually, I put 1 and 1 together and finally suspected ME/CFS (which before I had heard of but – to my now never-ending shame – had smugly thought of as “something psychosomatic”).
In the fall of 2017, I had deteriorated to a point that I could not drive a car anymore, couldn´t even tolerate the light of the moon, and spent more and more days in bed, with especially insomnia and anxiety being big issues. I then contacted Prof. Scheibenbogen who saw me at the Charite in Berlin and diagnosed me with ME/CFS.
I then dragged through the months, still working on and off, part-time. With better pacing, a lot of sleep and a lot of support from my wife, grown-up children and twin brother I gradually improved. The pandemic helped a lot because I inadvertently realized how much I really suffered from the talks I gave in other cities and how much each travel set me back. Now I am doing talks only online, which is a smoother ride.
From the beginning of my illness, I researched whatever pieces I could get a hold of on ME/CFS. I wanted to understand what was going on in my body! My feeling was always: yes, my whole body is affected, the immune system is activated, I am low on energy – yet at the deepest level I felt: that a substantial part of all this is in my brain which apparently does not do its business of proper regulation anymore.
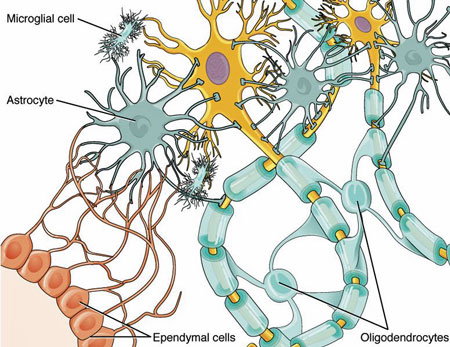
Glial cells in the central nervous system (Version 8.25 from
OpenStax Anatomy and Physiology, Wikimedia Commons)
How often did I say to my wife: “This is in my head!” This deeply felt notion of “something wrong in my head” made me curious about how the pathology of the central nervous system may be connected to all the things I knew about ME/CFS – including the symptoms and the many findings reported in the literature (like mitochondrial dysfunction, endothelial dysfunction, etc.)
So about 2 years ago, when pondering again about how the brain may possibly be involved – or even “cause”? – of so many dysfunctions, I ventured upon a group of cell populations that I didn´t know much about, the glia. What I found out was that CNS function (and dysfunction) is closely tied to the proper work of these cell populations (which include microglia and astrocytes). This got me, and the more I read about these co-regulatory brain cells the more I became convinced that they may play an important role in the whole mess of ME/CFS.
So I started an “Occam razor” project, listing all that is known about ME/CFS (signs, symptoms but also pathomechanisms) and tried to understand for every single entry on that list how it could possibly be explained by glial dysfunction.
I worked on this for a year, then sent it to my cousin who happens to be a veterinary neuropathologist and holds a research chair at the University of Guelph, Canada. We refined the hypothesis and published it as a preprint, aptly termed “Broken Connections – The Evidence for Neuroglial Failure in ME/CFS”.
Shortly thereafter I came across a major publication on the role of glia in COVID 19. As it turned out, the main author, Marie-Eve Tremblay, is one of the leading neuroscientists and glia researchers. I at once understood that she might appreciate our approach, e-mailed her to make her aware of our work – and so, in mid-2021, our collaboration began.
It ended in our publication of “The Pathobiology of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: The Case for Neuroglial Failure” in May 2022. During this time I learned an incredible amount about glial regulation from my collaborators (and I think they learned a lot about ME/CFS from me ;-).
I continue to read every piece of research on ME/CFS and am convinced that we now have a critical mass of knowledge that we will have both biomarkers and therapies in the very near future (my own bet would be on immunomodulatory therapies including BC-007, and “trained immunity” approaches as well as other therapies that may be able to silence activated endogenous viruses (here I am an eager follower of Prusty´s work).
Also, I am now part of the medical advisory board to the German ME/CFS Society, and I now work with my former ME/CFS physician Carmen Scheibenbogen. So the loop has closed in a certain sense and I now benefit from the immense knowledge and insight into super interesting research ideas in this group.
The Paper – A Brief Summary
The Pathobiology of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: The Case for Neuroglial failure by Herbert Renz-Polster*, Marie-Eve Tremblay, Dorothee Bienzle, Joachim E Fischer
Our work on the role of glia in ME/CFS is now published in Frontiers of Cellular Neuroscience. In this publication, we explain why ME/CFS research may benefit from a closer look at the role of neuroglia. The term “neuroglia” or “glia” describes a network of cell populations mainly in the central nervous system which is important for brain health and brain function. At its core, this network constitutes the immune system of the brain.
Why should we take this network into focus in ME/CFS?
Many biological systems are affected in ME/CFS. There is, for example, evidence for immune dysfunction (including autoimmunity), for metabolic, mitochondrial, and possibly peroxisomal dysfunction, for endothelial or vascular dysfunction, for inflammatory activation, and for dysfunction of the autonomous nervous system (and the central nervous system in general).
But it is still unclear how these dysfunctions fit together and how they conspire to cause the symptoms of ME/CFS.
We think that these processes can directly or indirectly affect a very important regulatory system of our biology: the neuroglia, and thus the innate immune system of our central nervous system (CNS). This non-neuronal system is mainly based on cells called microglia, which cooperate with other glial cells, called astrocytes and oligodendrocytes (the latter are responsible for maintaining the myelin sheaths of the nerve cells). The main task of this glial network is to protect the functionality and integrity of the brain. Whenever the health of the brain is challenged this cell population will be called to action. The glial cells are also very important for cooperation with the immune system outside the brain.
In a more detailed look, the neuroglial network plays an important role especially in the regulation of cerebral blood flow, protecting the blood-brain barrier, and maintaining functional connections within the brain. The glial cells are thus very important for motor functions, autonomous regulation, sleep, sensory gating, memory, mood, and cognition – all functions that are to some extent “broken” in ME/CFS. Also, glial cells work in close concert with mast cells.
Therefore, theoretically, the glial network could play an important role in the pathobiology of ME/CFS.
The GIST
- Dr. Renz-Polster’s neuroglial hypothesis of ME/CFS brings us yet another contribution to the ME/CFS field from Germany.
- Dr. Renz-Polster came down with ME/CFS in 2016 when a strenuous workout following a severe case of influenza left him unable to walk more than a few steps at a time.
- With better pacing, a lot of sleep, and a lot of support from my wife, grown-up children, and twin brother he gradually improved.
- Feeling that the brain must be involved he asked himself if damage or perturbations to the immune cells of the brain – the microglia or neuroglia cells – could explain his symptoms.
- He developed a hypothesis and produced a preprint“Broken Connections – The Evidence for Neuroglial Failure in ME/CFS”. Then when an internationally known glial cell expert- Dr. Marie-Eve Tremblay – published a paper on long COVID, he contacted her. Together they published a follow-up paper “The Pathobiology of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: The Case for Neuroglial Failure” which has proved popular.
- The extensive neuroglial (microglial) network plays an important role in many processes in the brain including cerebral blood flows, the blood-brain barrier, motor functioning (movement), autonomic nervous system regulation, sleep, sensory gating (problems with stimuli), memory, mood, and cognition. Plus glial cells work in close concert with mast cells to boot.
- The authors found that post-exertional malaise, reduced brain blood flows, endothelial dysfunction, immune dysfunction, and mitochondrial/metabolic dysfunction could all be explained by glial cell issues.
- So could the brain findings in ME/CFS – the altered connectivity or messaging occurring between different parts of the brain, the difficulty the brain has in sending blood to the correct places, the increased intracranial pressure, the altered cellular metabolism in parts of the brain, and the vagus nerve problems – can all be explained by glial cell dysfunction.
- They propose that the glial cells and the network they’re embedded in have become hyperactive – and are responding to the slightest stimuli – even possibly to stimuli that are evoked doing something seemingly innocuous like reading or watching a movie.
- They noted that glial cells could be producing neuroinflammation but could also simply be interfering with the proper flow of blood across the brain.
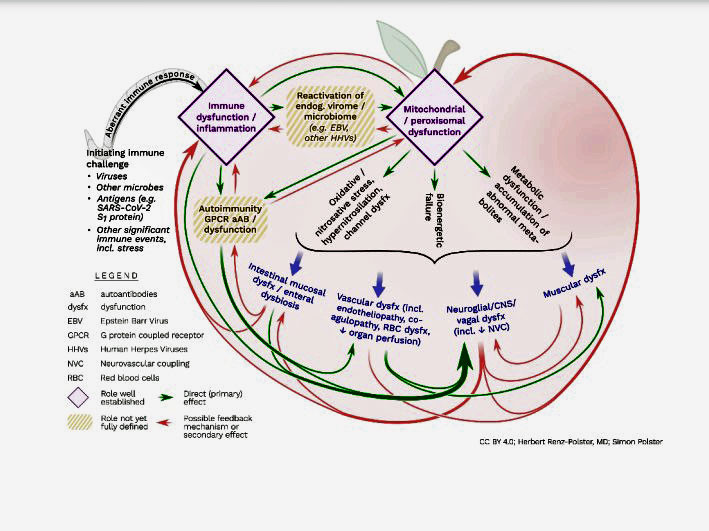
- Finally, they produced an “apple graph” which shows how the many different pieces of ME/CFS may fit together
- Dr. Renz-Polster is convinced that we’re getting closer and believes that we’ll see biomarkers and therapies in the very near future.
Our Work Step by Step
We, therefore, reviewed the whole ME/CFS literature for details about a possible contribution of glia in the many pathways that are dysregulated in ME/CFS. Here, we put the main focus, especially on two features of ME/CFS: post-exertional malaise, and the reduced cerebral blood flow.
We picked these two features for two reasons: both are present in all ME/CFS patients (at least if stringently diagnosed and examined), and they have been exceptionally well studied. Also, they seem to somehow jive together (for example, exercise leads to reduced cerebral blood flow).
What we found is that both of these features can be plausibly explained as a manifestation of malfunctioning glia (some more details below).
We then examined through which ways the other pathobiological features of ME/CFS (e.g., endothelial dysfunction, immune dysfunction, mitochondrial/metabolic dysfunction) could affect the functionality of this biological hub between brain and body. Endothelial dysfunction, for example, can alter the permeability of the blood-brain barrier so that peripheral immune cells can enter the brain and cause inflammation. This in turn activates the glia. Mitochondrial dysfunction (or any other cause of metabolic dysfunction) goes along with abnormal metabolites; these can also activate the glial cells (which are especially vulnerable to many toxic substrates).
The same aggravation can happen from severe inflammation (which also floods the body with abnormal metabolites) or from signals from a revved-up immune system. Autoantibodies, for example, may not only act on the blood vessels but may also directly or indirectly influence the immune system outside and inside the brain (for example, if the blood-brain barrier is not working properly).
Finally, we reviewed the ME/CFS experimental record for evidence from e.g. imaging studies or from laboratory studies (proteomics, transcriptomics, metabolomics, etc.) that may point to glial dysfunction in ME/CFS. Here, we identify and present many findings from different fields and different research teams which suggest that the function of glia may indeed be affected in ME/CFS. For example, all the findings of abnormal brain function in ME/CFS can plausibly be explained as manifestations of glial dysfunction:
- broken neurovascular coupling
- decreased cerebral blood flow
- altered functional connectivity between brain areas
- raised intracranial pressure
- altered cellular metabolism in several brain areas and nuclei
- vagal dysfunction.
The Jekyll and Hyde face of the Glia
In our explanation of why glia may be central in the regulatory disaster of ME/CFS we especially highlight a unique property of this group of cells: they can shift between an “aggravated” (= hyperreactive) and a more “quiescent” state.
- Aggravation happens by any form of stress (including inflammation)
- As already mentioned, glia can also become activated by abnormal metabolites and also by oxidative or nitrosative stress
- If repeatedly or pervasively aggravated, the glial cells become ever more reactive, i.e. prone to overreaction. This creates a vicious circle.
- This also means that the threshold for becoming aggravated can fluctuate and differ over time.
We propose that this flexible response of glia could explain the typical PEM features, i.e., the delayed onset, the typical duration of days (to weeks), and also the different thresholds for PEM between patients. We also think that the central role of glia in PEM could explain why PEM can happen even without any muscular exertion (i.e., alone from thinking hard or from watching a movie).
No “Alternative” Theory

Dr. Marie-Eve Tremblay’s microglial findings have opened new avenues of research.
Our explanations are not meant to replace or contradict the many theories about ME/CFS, like mitochondrial dysfunction, endothelial dysfunction, the role of autoimmunity, the role of reactivation of endogenous microbes, etc.
On the contrary: With our theory, we try to add a layer that may provide a better or finer-grained understanding of the many broken pieces in ME/CFS. Also, this added piece may be valuable when it comes to understanding how some drugs may work for ME/CFS, or which drugs or interventions may be hopeful candidates.
Also, with this work, we were able to benefit from the knowledge of a world expert on glia, Marie-Eve Tremblay, who co-authored this publication (so far ME/CFS research has not had that much access to this field of neuroscience). What she could highlight, for example, was that we may need to think more stringently about the concept of *neuroinflammation* (which some ME/CFS researchers embrace and others dismiss).
Glial dysfunction can be caused by many processes, some of which may not necessarily be inflammatory*. Also, glial dysfunction may not necessarily cause an inflammatory response. For instance, dysfunctional glia may “just” disrupt neurovascular coupling, i.e., the process which matches local perfusion in the different brain areas to local demand. We should probably become less zealotic in this regard.
And, finally, we have used this review of the ME/CFS literature to, again and again, regard ME/CFS from a system’s perspective: how may the pieces fit together? How may they be orchestrated? This gave rise to an “apple graph” which is part of the publication and shows how interwoven and resonant the many aspects of ME/CFS are.
Dr. Renz-Polster has been communicating with Jarred Younger about his hypothesis and neuroinflammation. Dr. Younger’s Solve M.E. Webinar on neuroinflammation and ME/CFS is today from 10-11 pm PDT.
Summer Donation Drive Update
All I know is that the Drive is going well and has exceeded expectations! I will catch up today and will report back shortly. Thanks to the many people who have supported us.:)






Any connection to the basal ganglia or essential tremors?
Great article Cort! Did they say exactly how exertion, especially moving muscles, triggers post exertional malaise through glial cells? I was a little confused about that.
Yes we try to explain this. In ME/CFS we evidently have a pathological response to exertion (muscular exertion included) which may include pathological immune activation, induction of inflammation and associated phenomena like exaggerated nitrosative/oxidate stress, mitochondrial/metabolic dysfunction (the latter may include the production of abnormal metabolites, e.g. in the kynurenine, glutamate, itaconate etc. pathway(s)) or activation of autoimmunity. All of the latter phenomena can affect a) the integritiy of the blood brain barrier and/or b) the functionality of the diverse neuroglial cell populations and thus lead to regulatory dysfunction in the brain.
If you watch the video above with Dr Younger, he explains and illustrates why we have such PEM. It’s at about 14 minutes into it ! Fascinating Zoom session.
Im curious about this to..developed essential tremors in shoulders/neck, hands and hips, along with myoclonic jerks in the last year as CFS got worse
I have the same
@Heidi Maahs I highly doubt it. That dam Gia should know.
Doctor’s comments that he improved during pandemic struck home with me. My only outings were medical appointments & brief errands 2-3 times per week & I leaned in 2020 that was too much. Doing a bit better after cutting back to 1-2 outings/week.
Were pacing & family support only treatment Dr. Renz-Polster credits with his improvement?
Keto has helped a little with my physical endurance, leaving it obvious for me how severely mental activity & stress affect me. I’m trying to be more careful with those now.
Deepest thanks Herbert for your important theorizing and distillation of neuroglial research. I, like others here, am interested on your general thoughts about interventions, pharmaceutical, nutraceutical and otherwise, that may modify micro glial activation.
I have cervical Dystonia as well as ME/CFS. After reading this paper I wondered the same myself…
Danke schön! Does this mean that ME is not necessarily post viral?
There are many Cfs cases reported after accidents, car crashes, operations, vaccines and so on. So yea, highly likely that it isnt only post virus.
The common denominator appears to be events associated with significant immune stimulation. In some (possibly biologically predisposed?) people this may cause persistent biological dysregulation.
ME is often triggered by mental and/or physical stress including a virus, cancer etc.
I’ve never thought it was strictly post-viral myself.
Cort says that he never thought it was strictly post-viral himself but surely Long Covid goes to show that viral illnesses triggering our type of disease with very similar symptoms does show that viruses could be the instigating factor for a very high number of sufferers of ME/CFS.
After all there are so many viruses that we encounter all the time. I seem to remember that back in the 80s and 90s it was mentioned that teachers and health professionals had the highest incidence of ME.
I used to be a teacher btw and was always picking up viruses from the kids that I taught.
For sure – and now long COVID is showing us that we can have an infection that we don’t even know about it which can trigger ME/CFS – so it’s really up in the air. I didn’t have an apparent infectious onset – but now I’m wondering.
Response to the question: Does this mean that ME is not necessarily post viral?
No, definitely not, and this is very important!
We are highlighting the role of glia to better understand the biological basis of the clinical signs and symptoms of ME/CFS (here we especially focus on PEM as this is the most salient feature of ME/CFS). This has nothing to do with the inception question (“What triggers/causes ME/CFS”?).
As to the latter question: We also discuss this question, see figure 2, which is also in the blog. As you see in this graph it is entirely plausible that microbial infection in some people leads to immune dysregulation which then may cause reactivation of endogenous viral reservoirs (like e.g. herpesviruses). The now ongoing and pervasive inflammatory stimulation in the body may set off a cascade of problems, including mitochondrial dysfunction, metabolic dysfunction and autoimmunity – phenomena which in turn can not only sustain the immune dysfunction but can also cause dysfunctions in many tissues: endothelial dysfunction, muscular dysfunction, glial dysfunction… This in turn would explain the organ dysfunctions seen in ME/CFS, like brain dysfunction, autonomous dysfunction, gut dysfunction, cardiovascular dysfunction, muscular dysfunction etc.
I believe anything can cause ME/CFS that throws your body or nerves enough of a curveball to activate an overanxious immune system.
A traumatic experience (either physical or personal), a virus, a vaccine, a car crash and such. I also believe it can come in stages. In my case, it first appeared as a result of child abuse by my grandfather, which put my immune system on edge which I call code yellow. Then with the birth of a child who has never spoken or stood up and gradually increasing deafness, my nervous system advanced to code orange. Finally, 20 yrs ago, after years of Type A overwork and finally a car crash, I reached Code Red, collapsed in a tennis match and was stuck in the corner of my bed for a year, unable to even comb my hair. I made it through the pandemic all alone at home with no car for 28 months, and as someone said above, found myself steadier with the imposed limits. I’ve always said I could “feel something objecting” in my brain if I overexerted. Feeling okay was dangerous, because I’d try to accomplish what I had let go a bit and promptly got worse with PEM. I think you and Dr Younger are on the right track, and I hope our illness is recognized and treated some day. Probably too late for me, being 77, but I’d be happy to leave my brain for you all to use for research if there’s a way to do that. Thank you so much for your efforts on our behalf.
Gia’s Neuro hypotesis can’t be true as she is an American baby care expert.
Martin, I’m sorry but I don’t understand your reasoning.
Cheers,
Gail
Genetic Fallacy
This is great work and seems to be inline with the research going on at MGH in Boston, MA. They are actively recruiting ME/CFS and Chronic Lyme patients in their study titled: “PBR28 with simultaneous MR-PET scanning to measure brain microglia activation in chronic fatigue syndrome and post-treatment Lyme”
I’m a cancer research nurse in Boston and an ME/CFS patient. I’ve been saying to my family and doctors that my brain feels SUPER inflamed. It’s hard to explain. My brain and my gut both feel a mess. My symptoms first displayed as GI related and then morphed into full blown ME/CFS, Dysautonomia, Small Fiber Neuropathy, and MCAS.
Dr. David Systrom told me that my feeling of brain inflammation is likely valid when I met with him 2 months ago for a checkup. He said it’s being investigated by various doctors.
@Rachel. First of all, I am a recovered ME/CFS person. Secondly, just because you are a cancer nurse, does not mean you can understand scientific papers of this sort. And thirdly, just because you FELT your brain inflamed, doesn’t meen it is necessarily so.
You are harming this community with your recent comments. You need to stop.
Martin, Rachel was not responding to your comment. She was making a statement about the article and how it aligns with her personal experience of CFS.
Logically, the question of recovery has nothing to do with the question of the pathobiology of ME/CFS.
Also, logically, if you think only neuroscientists can make comments on a scientific paper published in a neuroscientific journal you should not comment here, should you?
Where is this coming from and what the hell does your comment seek to communicate?
Of course Rachel can understand papers … absurd comment
@Chris. Whatever the cause of ME, it is totally reversible. I should know as I had it and recovered. My brainfog was bad in the early stages and now it is as clear as day. Haven’t had a relapse in over 12 years either.
So happy for you…it socks being stuck
Yea, dont buy it. Ppl who are “clear as day. Haven’t had a relapse in over 12 years either.” arent stalking Cfs homepages 12y later. They live their life. So something doesnt add up here. Plus, you seem very rude and assumptious. Nothing you wrote added something of worth to the discussion
That was out of line, Martin – but please, if you’ve recovered, spill the beans – what worked for you?
Good to hear about that research! Glad to hear that ME/CFS and post-Lyme are being studied together – we need more of that. What is MGH?
MGH is probably Massachusetts General Hospital and that’s possibly Michael VanElzakker PhD’s study. I think his work is very interesting.
I developed ME/CFS 3 years ago from a flu virus and since then have constantly had a peculiar sensation predominantly on the right side of my head above my ear. It’s not painful but feels almost numb, as if i’d been slapped across the face (the only way I can describe it!). I’ve mentioned this to Doctors and my ME/CFS specialist but no one has thought it to be linked. Anyone experience anything similar?
I developed an odd sensation in the same place over the winter, but it comes and goes. Sometimes it twitches. I’ve also had it on the other side. For me it results from taking antifungals, particularly caprylic acid.
SIMON, Yes, I’ve had a dull feeling behind my left ear, a rather large area encompassing the entire left rearward 1/4 of my head/brain.ive had this feeling my entire life.
My mother stated that I was always very subdued and quite growing up.
I failed gr.7 and 9. I just recall in high school algebra I had no clue what the hell they were trying to teach me and I had zero drive to try learning…so I dropped out.
Fast forward to the age of 21 (1981)…I get some weird bug in a hotel room that 2 weeks later caused an ulcer that healed on its own but was left with weird vague symptoms for years that progressively got worse until 1993 KERBOOM!head to toe weird total body rashes everytime I would enter my house….yes I,was one of those people that slept in a tent to prevent the downward spiral in health.then winter came, down I went and never recovered
I had no idea a person could become that ill. When I think back, I honestly believe I went septic.it was as if my entire gut leaked into the rest of my body and all within a weeks time. Two inch lumps all over my upper body.
Decades later I decide on my own to try a single dose of
ivermectin. The dose of ivermectin killed something off…I began to feel better as a whole…nowhere near the person I once was but better.
I’m left with lots of inflammation that does lesson by diet but it’s an extreme diet if I want to feel less inflammation…I mean veggies only and no nightshade which leaves basically nothing to eat. Lots of gut troubles. So BAZZARE.
At the age of 14 I was placed on 1.5 yrs of tetracycline for acne
Hello, I live just outside Boston (Watertown) and have had cfs following lyme for 28 years. Do you know more about this study?
Rachel,
Hello, I live just outside Boston (Watertown) and have had cfs following lyme for 28 years. Do you know more about this study?
Thank you
This reminds me of my long battle with CFS which seems to be in remission for several years now. I distinctly remember the oddest sensation once where the top of my head felt hot. I touched my scalp to see if that was what I was feeling, but it was fine. This hot feeling lasted only a couple of hours and never appeared again. I had no other symptoms associated with it.
I told my primary care doctor about this. He laughed and said there’s no way the top of my brain could cause that sensation because there’s no room in the skull for the brain to swell.
I know my body and know I’ve never felt anything like that before. And those of us who’ve experienced CFS know how strange our brains can become while under its oppressive grip.
Rachel, I have ME/CFS and Lyme+Co-Infections. My first symptoms, predominantly extreme fatigue, arose early in 1981. (Remember “Yuppie Flu?” era?)
I too have that brain-on-fire feeling at times, along with my eyes feeling pressured and hot. Further, radiating immense heat within my body, like a small furnace. It can be quite cool in my bedroom, yet my feet feel enflamed; it is not dictated by the external environment.
Wish I were closer to MG. Are you in the study? I admit, after 4 decades, I devour Cort’s work, yet have given up my youthful quest for a cure in my lifetime. I settle for a form of homeostasis.
Thank you, Hermann, for all of your work. Truly inspiring. Long COVID, Lyme and ME/CFS may be the fortuitous timing needed to crack these all open. Glia cells certainly make sense.
Me too – 1981 – it’s hard to be hopeful of get too excited but somehow nice to know I am not alone
Awww…the ” yuppie flu”
I recall that on the news about some American actress having yuppie flu back in the early 80s.
I had no idea it was what I had also
That’s how long I’ve been strapped in Donna.
I keep coming here in hopes of opening one of Corts pages that says
“STOP THE PRESSES”
@martin Do tell. How did you manage to recover from this when practically no one else has?
@Eddie. Lots of people recover from ME/CFS. Some don’t fully recover and some don’t recover. It is all spectrums of recovery.
Eddie, there are a lot of recovery stories when you look for them. The mainstream medical rhetoric is that you are doomed – you are, to learned helplessness, if you believe them.
Even if recovery looks different for you, takes longer, etc, one can definitely improve quality of life tremendously. Targeting nutrition (hint, ‘healthy’ eating maybe not be as healthy as one think, so explore other ways.) Playing the never crashing game. Etc
I think pain is usually the first thing to recede.
Look up those stories! May they inspire you
All kinds of people recover or find themselves in remission (very well managed symptoms). Vilifying those who are doing much better hardly seems a helpful approach.
I’m not vilifying anyone I’m asking how he did it
@Badpack. I had Post-Viral Fatigue Syndrome not CFs so perhaps I had a different illness to you lot. LOL I also have an interest in ME/CFS so that is why I am perhaps “stalking” these pages as you say. I believe I have added something worthy of the discussion to as now there may be a difference between PVFS and CFS.
Martin, Please keep in mind that the people who read these blog posts are dealing with a wide assortment of symptoms, for which they hope to derive at least a morsel of hope for their future. Your experience with success should be something for which you are grateful, rather than an assumption that all bodies are the same or an opportunity to imply that others are ignorant or doing something wrong. I appreciate every bit of research out there, and although you believe you have the answers because you’re doing better, think about what the author wrote about his own earlier suspicions that CFS was imagined. Might you someday look back with a new set of symptoms or illnesses and regret that same kind of attitude? Compassion means you empathize with others, and never assume they’re just like you.
Beautifully put.
LACS, thanks so much for a beautifully written response to Martin.
What you assume to be a post viral syndrome used to be referred to as post viral neurosthenia back in the early and mid 1980’s. The result of the Yuppie flu as the medical profession so derogatively coined it. There have been many remissions for a group of us with what appears chronic reactivation cycles of dormant viruses
My response was to Martin whose arrogance does not actually merit one
Health Rising has a post
“Microglial Inhibiting Drugs, Supplements, and Botanicals to Combat Neuroinflammation”
which would be a good start if these doctors are correct. My son started on LDN after reading this article. He is finally sleeping and has had an unexpected drop in his thyroid antibodies. We are dealing with mold/mycotoxins but suffer from many of the symptoms of CFS/ME. Thanks, Cort!
@Donna Vogel. Your son most probably has Hypothyroidism not ME/CFS if he has thyroid antibodies. In fact, for a diagnosis of ME/CFS, you have to rule out thyroid diseases.
Martin, this is true and not true.
True: for the diagnosis of ME/CFS you need to rule out other diseases that may explain the signs and symptoms
It is however not true that hypothyroidism would then be an *alternative* diagnosis. People with ME/CFS can have co-morbidities which do *not* rule out ME/CFS if the respective criteria are met (Hashimoto thyroiditis is one of them as is hEDS).
@Herbert Renz-Polster. ME/CFS is probably a secondary hypothyroidism where the T3 cannot get into the cells very easily. There is currently no test to check how much T3 gets into the cells. ME/CFS has exactly the same symptoms as Hypothyroidism. ME/CFS is therefore known and is nothing to do with microglial activation.
One does not preclude the other. I have had both conditions along with fibromyalgia diagnosed in the mid 1980s. Autoantibodies to the thyroid are indicative of Hashimoto’s which was, and continues to be one of my diagnoses.
@ Martin
Here is a nice review article on botanicals and glial cells from last year
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8076853/#:~:text=The%20possible%20interventions%20by%20curcumin%2C%20resveratrol%2C%20cannabidiol%2C%20ginsenosides%2C,Alzheimer%E2%80%99s%2C%20Parkinson%E2%80%99s%20and%20Multiple%20Sclerosis%20for%20microglia-mediated%20therapeutics.
Glad to hear :). I was surprised and please when I made that up – how many potential drugs and supplements there were – which reminds me – I don’t think we’ve gotten the results of Jarred Younger’s botanicals trials.
https://www.healthrising.org/treating-chronic-fatigue-syndrome/drugs/microglial-inhibiting-drugs-combat-neuroinflammation/
I have spent a long time reading everything I could get my hands on to try and find solutions to these problems.
Have this group studied intense vitamin therapies? Or low dose naltrexone therapies? I’m more after the cures as we have spent so much time on probable causes …let’s get into the methods of solutions. We need to live normal lives again before it’s too late!!!
When I saw Dr Bonilla at Stanford last year he mentioned much brain research had been done at Stanford (implying years ago) and they found inflammation in three sections of the brain. I hope Stanford published this work and other researchers are simply building upon it. If scientists aren’t building upon other scientists learnings and combining efforts than that seems a huge waste.
Yes, they did, if memory is correct – it was years ago – it was a fascinating paper because they used new technology and really zeroed in on one part of the brain. It was quite exciting but I believe he was unable to get further funding.
Dr Herbert Renz-Polster’s focus on the microglia is fascinating. I can relate to lots of what they’re discussing and have been really keen to try and understand what’s going on in my brain. Five years after having a very nasty flu (possibly swine flu?) with a very high temperature, I’ve managed to calm my brain down. However I can still wind it up again, if I eat the wrong things and irritate my digestive system. Dr Michael VanElzakker’s work in relation to the vagus nerve picking this up and relaying it to the brainstem, which then alerts the microglia makes sense to me. I’m also really looking forward to watching Dr Jarred Younger’s webinar too, now that the recording is available. And so interesting that the glial cells are involved in blood brain flow etc. I’ll need to read the full article. My brain seems to be constantly shifting in terms of energy levels and my ability to concentrate etc., and it gets worn out fairly quickly with any intense exertion.
Dr Jarred Younger’s Webinar can be watched on Youtube.
‘The recording of “How We Can See ME/CFS Inflammation In The Brain” is now available!’ Solve ME/CFS Initiative.
https://youtu.be/DU0UgWGyi0A
But what can we do about it?
I’ve worked out a lot of things that have helped Gail. I haven’t watched Dr Jarred Younger’s webinar yet though but I’m aware of his previous ideas.
I am convinced there is brain inflammation and brain overheating, and microglia are involved. Abilify has helped me so much and it reduces microglial activation https://pubmed.ncbi.nlm.nih.gov/27614570/ . It lets me do 6 hours of digital art and I can read and write. But if I go over my exertion limit, I still go into a post exertional malaise and can’t do any of that while I’m in it. Abilify makes it milder and helps with the pain, but I’m a cognitive mess. I don’t think it prevents PEM’s for me at all. Neuroinflammation seems like a very bad symptom instead of a cause to me. Why does moving muscles trigger the microglial cells? Why is the exertion threshold so low?
Chris, I have commentend on this question (Why does moving muscles trigger PEM?) above where you first asked it.
Thanks so much for your work Herbert. I am slowly reading the paper and it really is terrific. It covers so much about PEM. Wish I could read faster.
Very interesting paper Cort. Thank you for sharing.
It kind of leaves me asking more questions!
Just what a good paper is supposed to do 🙂
It is interesting how work on ME/CFS often intersects with the work we are doing on prenatal exposures and neurodevelopmental, immunological and endocrine problems later in life.
Recently, researchers at the University of Rochester have found that prenatal dioxin exposure can cause brain changes that result in immune disorders later in childhood. They were also able to repair this damage in the test animals. (NIEHS was one of the funders of this study.)
https://www.urmc.rochester.edu/news/publications/neuroscience/researchers-restore-brain-immune-system-function-after-prenatal-exposure-to-environmental-toxin
Perhaps, those who get ME/CFS were preset to develop this by toxic exposures much earlier in life than any scientist has explored.
Very interesting.
Betty, you may be on to something.
That mosquitoe spray those trucks would spray in our neighborhoods smelled very toxic. I tried to uncover the chemical the city used but it’s locked up pretty tight…I got the run around,and around,and around
I think this is maybe the first true “umbrella hypothesis” for ME/CFS. The beauty in this is that it incorporates a wide range of known onset factors for ME/CFS, and, as it includes explanation of ME/CFS as an interaction of peripheral and central factors, it might also explain why some patients improve on some medications, while others don’t: I assume in this model, depending on the patient’s individual “pathology pattern”, interactions at various points of the system (peripheral or central) might possibly influence the system as a whole.
I think I just saw two new publications going into a similar direction of peripheral immune system signaling inducing microglial reactivity: One is the Long Covid paper explained by Michelle Monje on Twitter, the other is the “Molecular Mechanisms of Neuroinflammation in ME/CFS and Long COVID…” paper by Tate et al.
…as well as incorporates diverse biomedical findings on ME/CFS.
Thank you! To be clear: this is not a *novel* explanation of ME/CFS, it is a detailed summary of which role the neuroglia could play in the pathobiological process using PEM and cerebral blood flow issues as an example. The role of the neuroglial cell populations (esp. microglia) in ME/CFS has been highlighted by several teams again and again, including Michael vanElzakker, Warren Tate, Angus Mckay, Jarred Younger and many others (including many neuroradiologists), and yes, many teams follow this route in Long Covid, too, including Michelle Moje. – We summarize, highlight and comment all of this work in our paper.
I think one of the cool things is how these separate threads and investigations are coming together. We’ll see what the future brings but that’s a great sign in my book.
In the article you shared, the drug Pexidartinib was used in mice to “‘shut-off’ the hyper-responsive microglia and those were replaced by new microglia that functioned normally.” According to another paper, it is an inhibitor of colony-stimulating factor 1 receptor (CSF1-R) (whatever that means :-)…
This was meant to be a reply to Betty Mekdeci’s post.
All those hypotheses, you will get tired of them… I’ve been hearing them for almost 30 years… ME is not 1 disease but has multiple causes… this makes it so difficult to prove it scientifically. How does this compare to manganese , Ron Davis’s new theory. Personally I have no hope that this disease is going to be solved in about 100 years.
All those wasted lives. Very sad.
I just read the paper ! It’s an amazing study and while I certainly couldn’t understand everything I’m impressed with the connectivity of neuroglia and and all the CFS/ME associated malfunctions ! Thank you Dr. Herbert Renz-Poster ! A big thanks to Cort as well for bringing this to our attention !
Many people have used LDN in an attempt to quiet their microglia. Some of them claim mild improvement, others find none at all. I certainly haven’t heard of LDN “curing” anyone’s CFS. Don’t those results suggest the microglia are not at the heart of the dysfunction? Also, didn’t DXM (another microglial suppressor) fail in the same way?
You could also interpret that as the inability of LDN to fully calm down the microglia – that it’s not that good or is not good enough at doing that. The fact that some microglial inhibitors seem to help while others don’t suggest that the microglial issue is a complicated one. Some of this data also comes from animal trials which may not in the end correlate to humans. I would also be surprised if we’re in a take a drug and get over it situation. I would bet on a combination therapy approach.
One must also consider that meds used to calm the micro Glia may also act on other areas that actually stimulate a response…positive or negative.
No pharmaceutical intervention IMHO can target and affect only ONE area. Otherwise some of the pharmaceutical packet inserts would have very short lists of potential side effects….which are actually EFFECTS.
Thus, when some meds seem to help and some dont… we need to be careful of interpreting that outcome.
Micro dosing magic mushrooms does wonders…..and I mean micro…gotta find your sweet spot
Cort, when are you going to do a write up on MM?
It has never been proven that the clinical effects that LDN may or may not have are due to microglial inhibition. LDN is just being thoroughly studied.
Microglia hypothesis for MECFS had been around for quite a while. It is also proven to cause concussion fatigue (a NYT columnist once wrote how he sympathized CFS patients after suffering concussion fatigue for a month) and involved in age related fatigue.
Dopamine is known to down-regulate activated microglia. Unfortunately, there is no easy way to deliver dopamine to the brain. Brain also get quickly habituated with pharmaceutical interventions. The trial with low dose Abilify shows great promise for some people, but the effect quickly evaporated. Some people had bad side effect as well. Maybe Cort could add a link to that HR article.
I find that interesting, because in spite of ME/CFS I tend to go into concentration tunnels which I suspect are hyperfocus which is supposed to involve a dopamine release. It can calm me down temporarily but is not very practical to have with ME/CFS, because it makes me go across energy limits without noticing and crash later. It is amazing how there seems to be more than one energy related pathway in the body…
That’s interesting. Drugs that produce strong feelings of reward do a damn good job at neutralizing all my CFS symptoms. They make it so that I can work out, read; they also stop my mast cell activation. However, staying high all the time is not a good long term strategy.
What drugs give you relief? I have had fatigue symptoms on and off since 2007 with two experiences putting me in the hospital. I’m having one of my worst experiences now….4 1/2 long. Never been able to get a diagnosis and have seen every specialist there is. Bastyr university diagnose me with Epstein barr syndrome because I have high numbers of antibodies. Mainstream western medicine and my doctor’s don’t recognize this. Doctors treat me with depression medicine and don’t believe I have cfs because mine waxes and wains. I live in Seattle and if you know anyone out here that can at least diagnose me that would at least be a start. I’ve read the only 20% of people with cfs actually get a diagnosis.
My wife has had Hashimoto’s, then CFS/ME for 28 years. My current ’cause’ theory is a type of activation of archaic hibernation cells in the brain stem. How does zoology investigate the mechanisms of hibernation?
Mike, there was a ‘dauer’ theory … about the body going into protective hibernation state. Dont recall the doctors name… sure a quick google will turn up some information.
I think Naviaux
Could one confidently state then that ME/CFS has been around forever?
Is this why so many women (in particular) ended up in sanitariums for ‘mental health’ disorders? Hmmmm?
Or can anyone state why in the current age we are seeing so many people predisposed to this condition???
Has something changed? Can we ‘unchange ‘ it?
I always thought that my smartphone made things worse, especially social media. Seeing more and more images and information to process. My health declined a few weeks ago so now I am playing a ‘don’t go on Instagram’ game with myself hahaha. But I do think that that is different: every decade there’s more data to process.
This is a very good question. Many immune related disorders, autoimmune diseases included, have been on the rise over the last several generations. Type 1 Diabetes for example, or Multiple Sclerosis. Possibly ME/CFS? We do not know. Evolutionarily speaking, we humans should be adapted to fight pathogens without many of us falling to the wayside… So it is possible that the rise in autoimmune diseases reflects an immunological “mismatch” in modern times. This is what the “hygiene hypothesis” postulates. A good overview here:
https://www.faustmanlab.org/wp-content/uploads/2020/03/JIM-BCG-induced-metab.pdf
Type 1 Diabetes can now be successfully treated by giving a vaccination with BCG. This is supposed to mimic the commensal bacteria that we carried in us since thousands of years and may boost the immune system. Personally I also think that BCG vaccination and other “trained immunity” approaches should be urgently trialed for ME/CFS.
Herbert Renz-Polster, I thoroughly enjoyed reading this information.
I’m from South Africa.
In January 2022 (after about 3-4 years looking for answers), Dr Janine Raubenheimer (in Pretoria), diagnosed me with CIRS (Chronic Immune Response Syndrome).
It seems to fall within the catagory of ME/CFS.
What made finding a diagnoses challenging, is that I have a few serious conditions, Eg. HIV, Diabetes Type 1, Hypothyroidism, Severe Depression.
We think that the CIRS may have been triggored by prolonged Mold exposure.
Last August 2021 I also survived 9 days in Hospital with Covid Pneumonia.
A month after Covid my Retina tore that was treated with laser. (I mention this, perhaps its all related).
My CD4 Count Oct 2021 was unexplainably high after Covid.
The count was 1545.
I’ve been on ARV’s since 2001.
Became T1D 2013.
Am 62 years of age.
I’m sharing the information since it may offer some leads.
Thank you! This is lot to bear. This could all be a reflection of a immune system gone “wild” indeed. What some physicians diagnose as CIRS may indeed be hard to distinguish from ME/CFS, they may be “two men in the same boat”. Hang in there, and thank you!
Herbert Renz-Polster, thanks for your information, and thanks Cort.
Regarding viral onset, I thought I’d chime in to say that my onset began with a PTSD bout. from the onset date, it took 15 years to diagnose ME/CFS, but I was diagnosed 2 1/2 years in, with Hashimoto’s. Chicken and the egg are always a mind game regarding onset.
I fully recovered briefly 9 years since onset with a really strict diet. I imagine it boosted my immune system enough to dig itself out of the rut. (in the meantime a functional medicine dr discovered about 8 parasitic gut infections.) But then I had another PTSD event, and all the symptoms returned and the diet is now a stick not a carrot. Meaning, I get worse if I eat most anything but I never get better sticking to it, as I did the first time. I imagine the various infections that followed are dominoes that fall: Lyme confections, mold, SIBO…
Of all my ME friends, I’ve got the worst neurological symptoms. Though I have less pain and even fatigue in comparison. The sound flooding is excruciating.
After 24 years, my family, friends and most doctors still don’t believe me (or at least they remain skeptical of the scope of the symptoms of this diagnosis. I would be thrilled just to live in a world where people believe me and are kind.
So sorry Linda, it’s so tough. I sometimes try and imagine how it would be, if people around me believed me and were kind. Such a different experience. We can, at least, try to be kind to each other here, on Health Rising 🙂
It’s another reason why I like Herbert’s paper, as it accomodates also non-viral onset factors or co-factors. It is my opinion that there is a close link between stress and the immune system, and it is also as far as I know a strong epigenetic modulator. You are not alone.
We believe you.
My own father doesn’t believe me.
I wish the non believers would get this just for one week
I have read several articles and books on Psilocybin (magic mushrooms) and how it can rewire the brain. Has any research been done on ME/CFS and Psilocybin? It seems to me that it might help our brain function better. From what I have read, medical-grade Psilocybin is safer than aspirin.
https://www.texasmonthly.com/news-politics/rick-perry-drug-pusher/
It’s being trialed in fibromyalgia.
Check this out – https://www.healthrising.org/blog/2021/12/02/psychedelics-psilocybin-lsd-fibromyalgia-chronic-pain/
🙂
I do magic mushrooms when I need to.
Trust me, they work wonders.
I mostly microdose…and I mean micro.
There are lots of good books written on MM
They are very very safe IMHO
You need to read:
https://www.frontiersin.org/articles/10.3389/fneur.2022.877772/full
Another interesting observation from Warren’s work is a rationale as to why so many (Most) pwme react badly to SSR inhibitors.
This treatment is wrong. Why do you think that people with ME/CFS (properly diagnosed) respond so badly to tricyclics? ME/CFS in the early stages saturates the HT1 receptor with Serotonin causing serotonin resistance. The myriad symptoms in ME are mostly caused by loss of homeostasis – the responsibility of serotonin. The original reason for trialing tricyclics with ME/CFS was incredibly false logic and faulty illness beliefs among the Medical profession that ME/CFS was a form of depression. Some studies showed that some people responded quite well to tricyclics but as you know the diagnostics have been fraught with error often classifying people with a depressive disorder therefore requiring SSR inhibitors.
Ian Hodgson PhD (Otago)
I cant tolerate most drugs even LDN .. antibiotics make mental health, PEM & sleep ability really bad.. symprove probiotics helped on 6m daily intake improve those to allow some sleep and more stable mood.. I cant function at all without Asprin daily.. ie cant even work my phone or communicate.. I have ME, hEDS & CCI, OTC.. symptoms of IIH ..how do the glial cells dysfunction link to ME & hEDS and CCI etc.. have they talked with dr.Fargen? Who is trying to understand why the CSF pressure though normalised with intervention patient will then become symptomatic again.. are they looking at the work dr.Eccles does with people with hypermobility more like to be autistic and contract long covid..? What’s the link between these things and ME and glial dysfunction and connective tissue fragility and genes and gut microbiology and mental health and inability to tolerate or process meds? Are we processing food properly? Are we missing the correct nutrients to protect the body to keep it working and stop the infection? Is that bc of genetics or the microbes being affected by such poor diets and chronic stress? Is the connective tissue fragility part of glial cells going haywire?
I had typical me symptoms intermittently for decades until I learned “the Lightning Process” which teaches us to remain in parasympathetic arousal.
It gave me 7 years of normal energy then the symptoms started to return, starting with difficulty in reading books: nothing longer than a newspaper article.
After 3 years of symptoms deteriorating I realised it wasn’t only me symptoms, eg worse malaise, muscle and bone pain, especially ribs and parasthesia.
I was quickly diagnosed with multiple myeloma which had probably been active for 3 years.
That was 10 years ago.
MM is not curable but it is very treatable and is currently under control with only moderate-severe physical and mental fatigue (and dizziness) as obvious symptoms.
Remaining in parasympathetic mode emotionally definitively alleviates MM symptoms.
Is this congruent with glial dysfunction?
I remember my immunologist, the only guy I trusted, stated to me decades ago that researchers are studying the passages and frontal brain where viruses and infection enter our bodies.