

“If you don’t get a good night’s sleep, you’re not going to get well. It really is that simple”. Dr. Rodger Murphee

How to get better sleep. This blog compares recommendations from different health experts.
This is part IV in an ongoing sleep series from Health Rising that attempts to understand why the notoriously bad sleep in chronic fatigue syndrome (ME/CFS), fibromyalgia (FM), long COVID and related diseases occurs and to find ways to fix it.
Unrefreshing or otherwise poor sleep is often the first symptom practitioners try to help in ME/CFS, FM, and related diseases. This blog compares sleep prescriptions from a diverse array of sources – a fibromyalgia doctor, an ME/CFS/FM doctor, a longevity expert, and a neuroscientist – to see what commonalities showed up, what differences existed between them, and hopefully uncover some new approaches to take. (Please note this is a very long blog and you may want to print it out using the print button on the bottom left of the blog.)
The health experts include:
- Dr. Rodger Murphree DC – fibromyalgia and ME/CFS practitioner and author. Blog source – Fibromyalgia and Deep Restorative Sleep – ebook
- Dr. Teitelbaum MD – ME/CFS/FM practitioner and author. Blog source – From Fatigued to Fantastic 4th ed.
- Dr. Peter Attia MD – former surgeon – now a longevity and wellness podcaster. Blog source – Peter Attia’s Sleep Protocol: Supplements, Tools, & Tips – from Brainflow
- Dr. Andrew Huberman PhD – Stanford neuroscientist and podcaster: Blog source – Sleep Toolkit: Tools for Optimizing Sleep and Sleep-wake Timing.
Please note this is a very long blog and you may want to print it out using the print button on the bottom left of the blog.
It should be noted that, except perhaps for Dr. Huberman and Dr. Teitelbaum, this overview does not cover all the prescriptions for sleep from these health experts. Dr. Attia, for instance, has done six podcasts on sleep (!) and this overview simply covers the sleep treatments that a website reported he takes and recommends. Likewise, the sleep prescriptions from Dr. Murphree came from an ebook provided to people who viewed his recent online summit.
Except for the section on Dr. Huberman, which contains a new take on sleep hygiene, this overview also does not explore sleep hygiene – often a crucial element in getting better sleep.
Broad Observations
Almost 50 different sleep aids were suggested. Surprisingly, all four practitioners agreed on only one of them (see table below). Some broad observations:
- Dr. Murphree – who has focused on fibromyalgia – relies entirely on supplements and reports they work well with his patients.
- Despite his long association with supplements, Dr. Teitelbaum focused his sleep chapter almost entirely on sleep drugs and employs a number of them at the same time in low doses to get his patients to sleep. Dr. Teitelbaum was the only practitioner/researcher to advocate using sleep drugs.
- Perhaps not surprisingly, the two newcomers to the scene, Dr. Attia and Dr. Huberman (in particular) advocated for some high-tech solutions (cooling mattresses/pads) and apps to help with sleep. Huberman also advocated for some novel sleep supplements.
The next part of the blog dives into some of the more common suggestions and the second part of the blog covers the protocols proposed by each person.
Sleep Suggestions Table
| Rodger Murphree DO | Jacob Teitelbaum MD | Peter Attia MD | Andrew Huberman | ||
|---|---|---|---|---|---|
| SUPPLEMENTS | |||||
| Vitamins, etc. | |||||
| Melatonin | 3-9 mg sublingual plus 3-9 mg timed release - if waking up in middle of night) | Natures Bounty Dual Spectrum Melatonin 5 mg | Doc Parsleys Sleep Remedy | does not recommend | |
| Magnesium | 500 mgs (chelate) - in CFS/Fibro Mix | Attia has mentioned taking several kinds of magnesium over time (600- 800 mg per day: 2 tablets of SlowMag every morning and 400 mg of Magnesium Oxide by Nature Made at night - but focuses on Jarrow MagMind L-Threonate for sleep. Magnesium bisglycinate (200 mg) is also found in Doc Parsleys Sleep Remedy | 145 mg magnesium threonate 1 hour before bed | ||
| 5-HTP | 300 mgs/400 mgs if taken with food | 200 mg (Revitalizing sleep formula - Enzymatic therapy) | Doc Parsleys Sleep Remedy | ||
| L-trytophan | Murphree believes 5-HTP is much better | Doc Parsleys Sleep Remedy | |||
| Phosphatidylserine | Doc Parsleys Sleep Remedy | ||||
| GABA | (if needed) - in Delta Sleep Formula | Doc Parsleys Sleep Remedy | 2 grams every 3 or 4 days; | ||
| Vit D | Doc Parsleys Sleep Remedy 69 mcg | ||||
| Niacin | Doc Parsleys Sleep Remedy 6.9 mg | ||||
| L-Theanine | (if needed) - in Delta Sleep Formula | 200 mg (Revitalizing sleep formula - Enzymatic therapy) | Doc Parsleys Sleep Remedy | 100-400 mg 1 hour before bed | |
| Apigenen | 50 mg 1 hour before bed | ||||
| Lysine | 2 grams every 3 or 4 days; | ||||
| Myoinositol | 900 mg - every other day | ||||
| Herbs and Herbal Extracts | |||||
| Ashwaganda extract | (if needed) -- in Delta Sleep Formula | ||||
| Valerian extract | (if needed) -- in Delta Sleep Formula | 800 mg ((Revitalizing sleep formula - Enzymatic therapy) | |||
| Passion Flower | (if needed) - in Delta Sleep Formula | 350 mg | |||
| Hops | 120 mg (Revitalizing sleep formula - Enzymatic therapy) | ||||
| Lemon Balm leaf extract | Terric Zzzz | ||||
| Mandarin Zest Oil | Terric Zzzz | ||||
| Ravintsara | Terrific Zzzz | ||||
| Lavender | Terrific Zzzz | ||||
| SLEEP DRUGS (Teitelbaum) | |||||
| First Choices | |||||
| Ambien (zolpidem) | 5-10 mg (top choice) | ||||
| Trazodone (desreyel) | 25-50 mg | ||||
| Neurontin (gabapentin) | 100-600 mg (bedtime) | ||||
| Lyrica (pregabalin) | 50-300 mg (bedtime) | ||||
| Flexeril (cyclobenzaprine) | 2.5-5 mg (bedtime) | ||||
| Over the Counter Antihistamines (Unisom, Benadryl, Dramamine) | 25-50 mg | ||||
| Second Choices | |||||
| Klonopin (clonezepam | 0.5-1 mg | ||||
| Zanaflex (tizanidine) | 4 mg | ||||
| Antidepressants (Teitelbaum - use only one at a time from this list) | |||||
| Sinequan (doxepin) | 5-10 mgs or 10 mg/cc | ||||
| Elavil (amytriptyline) | 10 mg | ||||
| Remeron (mitrazapine) | 15 mg | ||||
| Zyprexa (olanzapine) | 5 mg | ||||
| Seroquel (quetiapine) | 25-50 mg | ||||
| Blankets and Mattress Pads | |||||
| Weighted sleep blanket | Luna brand | ||||
| Cuddle Ewe Mattress Pad | |||||
| Ooler Sleep System | From $450 to over $1300 | ||||
| Eight Sleep Mattress or Mattress cover | From $2200 to $3900 (!); | x | |||
| Light Blockers and Enhancers | |||||
| Blue-light blocking glasses | Gunnar Blue Light Blocking Glasses | x | |||
| Ring Light | Ring lights | ||||
| Drawing Tablet | Drawing tablet | ||||
| Sleep Masks | Alaska Bear Sleep Mask | x | |||
| Apps and Tapes | |||||
| Reveri App | Reveri | ||||
| NSDR | Madefor NSDR | ||||
| Yoga Nidra | x | ||||
| Others | |||||
| Elevating Feet | x | ||||
| Nose breathing | x |
Sleep Aids More Commonly Suggested
L-theanine
- Four of the four experts recommended L-theanine.

The only treatment recommended by all four experts was L-theanine – found in high abundance in green tea.
It’s no wonder that L-theanine was the most common pick. L-theanine, an amino acid found in tea – particularly green tea, has been found to improve sleep in both animal studies, in boys with ADHD (400 mg – taken throughout the day), in healthy men and women, and in people with generalized anxiety disorder. If you’ve taken some caffeine, you might want to boost your L-theanine levels as L-theanine stimulates the same GABA4 receptors that caffeine knocks out – and which are responsible for caffeine’s ability to induce insomnia.
A recent study suggested that future types of L-theanine’s effects may provide even more benefits. A mouse model study -which used a magnesium-L-theanine compound – found the combination was able to increase dopamine, serotonin, melatonin, and antioxidant enzyme levels, reduce glutamate activity and improve sleep latency (the ability to quickly go to sleep), sleep duration, and delta or deep sleep – even when administered in the presence of caffeine (!).
A 2022 placebo-controlled, double-blinded (:)) study found that alpha-S1-casein tryptic hydrolysate (CTH) and L-Theanine increased sleep duration by 45 minutes, improved sleep overall, sleep latency, sleep habitual efficiency, and daytime dysfunction.
(CTH is a milk compound that studies suggest increases GABA activity and may be able to help with sleep, reduce anxiety, improve cognition, and reduce blood pressure and cortisol levels. It is possible to buy hydrolyzed casein but I don’t know if it’s the same product.)
Magnesium may be a natural adjunct to L-theanine as both provide different effects. Both interestingly, however, oppose caffeine’s effects by stimulating the GABA4 receptors.
Magnesium
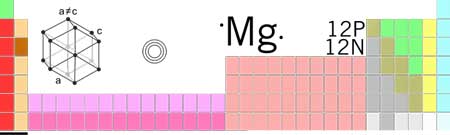
Magnesium – particularly magnesium threonate – was commonly recommended.
Three of the four experts recommended magnesium for sleep. Dr. Teitelbaum was the only practitioner not to recommend magnesium directly but generally does so in regard to other facets of ME/CFS.
Magnesium and Sleep – The study evidence for magnesium and sleep overall is mixed, with some studies showing an effect and others not. Since magnesium is often taken with other supplements, it might be better to assess multi-treatment studies. One interesting study found that a magnesium – melatonin – Vit B Complex (175 mg liposomal magnesium oxide, 10 mg Vit B6, 16 μg Vit B12, melatonin 1 mg, Extrafolate-S 600 μg) taken an hour before bedtime was helpful with insomnia. Another found that Magnesium, B Vitamins, Rhodiola, and Green Tea (L-Theanine) reduced stress levels and daytime functioning.
Magnesium Threonate – Both Attia and Huberman recommended magnesium threonate. Magnesium threonate or magnesium L-threonate is formed when magnesium is combined with threonic acid – a component of vitamin C. Unlike some other forms of magnesium such as magnesium citrate, studies suggest that magnesium threonate may be able to effectively boost magnesium levels in the brain – which needs a lot of magnesium. (It’s not clear if magnesium oxide, orotate, taurate, malate, carbonate, and chloride can easily get into the brain or not.)
Animal studies suggest that magnesium threonate is well absorbed into the brain – which apparently has a very high need for magnesium. According to Be Brain Fit, magnesium threonate over 12 weeks in seniors improved all 4 cognitive domains tested – making them appear 9 years younger than they were. An open-label study also found magnesium threonate effective and well tolerated in ADHD. While much more research is needed – magnesium threonate is one of the least studied formulations – it may be able to help with sleep, cognition, and nerve pain.
Melatonin
- Three of the four practitioners recommended melatonin. Citing melatonin’s wide-reaching effects and the dosages of melatonin in most products that exceed the amount of melatonin created in our body, Huberman worried that taking melatonin chronically over time could be problematic.
Studies – and quite a few have been done – have generally found that melatonin can reduce insomnia, increase sleep duration, and improve sleep quality.
5-HTP
- 5-HTP was recommended by 3 of the 4 health experts, and is Dr. Murphree’s core sleep supplement. (see the Murphree section).
5-HTP is right in the thick of things. Derived from tryptophan, 5-HTP is metabolized into serotonin and melatonin, and according to one overview, plays “a major role both in neurologic and metabolic diseases”. According to the review, 5-HTP may have antidepressant and anti-anxiety effects, and improve sleep, and reduce migraines and the pain in fibromyalgia. Recently, a 5-HTP improved REM sleep and improved sleep quality in a small study of Parkinson’s patients.
GABA
- Three of the four experts recommended GABA supplements.
Sleep drugs often target gamma-Aminobutyric acid or GABA – a calming agent produced by the brain – which studies indicate may be significantly reduced in insomniacs. GABA knocks down excitatory factors such as glutamate and boosts parasympathetic nervous system activity. Like other sleep aids, GABA appears to boost serotonin and melatonin levels.
GABA sleep studies, however, have had decidedly mixed results, however. One mouse study which mixed GABA with L-theanine found the combination restored normal sleep latency and sleep times.
Blue-Light Blocking Glasses
Two of the four experts recommended blue-light blocking glasses.
Research by Harvard University has shown that by exposing our system to artificial blue light from electronic devices after the sun goes down, we actually disrupt our circadian rhythm and experience decreased levels of melatonin. On his blog, Dr. Attia mentions he uses the popular Gunnar brand of blue light-blocking glasses. You can also get Gunnar glasses on Amazon.
Ashwagandha extract
- Two of the four experts recommended Ashwagandha.
It was somewhat surprising that more didn’t, as a recent meta-analysis found of five randomized trials found that Ashwagandha extract (400-600mg) produced a small, but significant, effect on overall sleep and helped most in people with insomnia.
Valerian extract
- Two of the four experts recommended valerian extract.
Valerian extract is commonly used for sleep and calming and probably achieves effects by enhancing serotonin and possibly GABA production and enhancing adenosine signaling. Several studies suggest it may promote deep sleep. A recent meta-analysis and review suggested that while valerian may help with sleep, herbal extracts of valerian that sit on the shelf for a couple of months may lose some potency. Preparations that use the whole root/rhizome may have more reliable effects.
Health Experts’ Recommendations
Dr. Murphree’s Core Sleep Supplement – 5-HTP

Dr. Murphree – who has focused more on FM – finds that 5-HTP works well for most of his patients
Dr. Murphree is VERY high on 5-HTP and recommends it to most of his patients. In fact, he reports that up to 300 mg of 5-HTP (or 400 mg with food) is all most of his fibromyalgia patients need to get a good night’s sleep. He loves 5-HTP because when used properly, it can increase serotonin and melatonin levels, thus improving sleep, digestion, pain, mood, and mental clarity.
Murphree that SSRIs, on the other hand, don’t really help because they don’t help you make serotonin – they just make more of what’s there available. What people with FM and ME/CFS need is more serotonin.
He recommends starting with taking 50 mg 5-HTP 30 minutes before bed on an empty stomach, along with 4 ounces of juice (apple or grape), and increase the dose up to 300 mg (400 mg with food) if needed. If you feel hung over the next day, decrease your dose of 5-HTP.
Warning – a few individuals who attempt to take 5-HTP at night will have an adverse reaction. Individuals with a sluggish liver (usually more pronounced in CFS) may have trouble breaking down 5-HTP fast enough. Instead of making them sleepy, it revs them up and they become more mentally alert. If this happens, simply take 1-2 5-HTP tablets with food 1-2 times a day, and discontinue using it at bedtime on empty stomach.
If 5-HTP doesn’t work within a week, he recommends trying 3 mg of sublingual melatonin. If that doesn’t work, then add his Delta Sleep formula (see below).
The Delta Sleep formula (2-4 capsules/night) contains GABA, L-theanine (500 mg), Ashwagandha (200 mg), valerian (200 mg), and passionflower (100 mg) extracts.
Plus, take magnesium – a natural sedative and muscle relaxer as well as a good multivitamin/mineral supplement. If you’re not having a bowel movement, Murphree recommends increasing magnesium (chelate, citrate, or taurate) by 140-150 mg at dinner each night until you have one.
Waking up in the middle of the night
If you’re taking the 300 mg of 5-HTP at night and melatonin and are still waking up in the middle of the night he recommends taking 3 mg of timed-release melatonin. If that’s not enough, you can even take 3-9 mg of sublingual melatonin before bed plus 3-9 mg of timed-release melatonin. You should start low, though, and only increase if needed.
Dr. Teitelbaum’s Sleep Drug Approach

Dr. Teitelbaum has been treating and studying ME/CFS and FM for decades. He reports that most of his patients require sleep drugs.
Dr. Jacob Teitelbaum MD has been studying, treating, and writing about ME/CFS and FM for several decades. His Fatigued to Fantastic series of books – now in its 4th edition – has been notable for its breadth of treatments and creative approach to ME/CFS/FM.
Dr. Teitelbaum believes that disordered sleep is “one of the key processes that drives CFS/FMS”, and that the most effective way to eliminate fatigue and pain in these diseases “is to get eight to nine hours of solid, deep sleep on a regular basis”. His goal is basically to do whatever it takes to get good sleep.
He also believes that the sleep disruption in ME/CFS and FM is “usually too severe to be dealt with by any single prescription or natural remedy”.
Teitelbaum begins with sleep hygiene and natural remedies but states that most people with ME/CFS/FM will need prescription drugs at least for a time. In the 4th edition of From Fatigued to Fantastic, he lists some supplements, but the chapter on sleep focuses almost entirely on drugs.
Prescription Drug Approach
Teitelbaum does not recommend “many sleeping pills in common use”, like Valium, that worsen deep sleep. With the exception of Klonopin (clonazepam) and Xanax (alprazolam), he highlights the risks of long-term use of addictive benzodiazepines. Both these drugs may improve deep sleep.
Instead of focusing on one sleep medication, Teitelbaum uses low doses of different sleep aids – as many as 3-7 of them – together. Most of the benefits and fewer of the side effects of sleep drugs, he states, appear at the lower doses and they wash out of your body more quickly.
The best way to reduce your level of medication is to stay on the drugs for six months, after which you can usually start to reduce them. Most people can taper off all drugs after about 18 months, while some need to stay on them for years. During stressful times he recommends upping the dose a bit.
The Sleep Drugs
Teitelbaum reports that, with the rare exception of a few people on Ambien who develop depression, he does not see side effects cropping up after long-term use of these drugs.
Main Treatments
Ambien (Zolpidem) – 5-10 mg
Teitelbaum’s first choice – usually effective and well tolerated, effective at helping people fall asleep. Short-acting; if someone wakes up in the night – take 2.5 mg under the tongue. Since rebound insomnia may occur when the drug is stopped suddenly, taper by 2.5 mg every 2 months.
A small double-blinded, placebo-controlled study found that Ambien (10 mg) significantly reduced time to fall asleep, increased sleep time, reduced awakenings, and produced overall improvement in sleep and daytime energy in FM.
Trazodone (Desreyel) 25-50 mg
An antidepressant, usually used in low doses for sleep in ME/CFS and FM. A small percentage of people may need higher dosing.
Trazodone improved global fibromyalgia severity, sleep quality, and depression, as well as pain interference with daily activities in FM. Combining it with Lyrica further enhanced its benefits. Trazodone was also successfully used to stop the hyperarousal that plagues some people with poor sleep. It may also be able to help with neuroinflammation.
Neurontin (Gabapentin) 1-600 mg/bedtime or Lyrica (Pregabalin) 50-300 mg/bedtime
Despite their close chemical relationship, one of these drugs will often be tolerated while the other will not. Teitelbaum usually tries Neurontin first. Both are effective for pain and restless leg syndrome and can markedly improve sleep quality. The main side effects are sedation and dizziness – plus, in Lyrica – weight gain.
Extended-release Neurontin improved the quality and quantity of sleep in one fibromyalgia study.
Flexeril (Cyclobenzaprine) 2-5 mg/bedtime
A muscle relaxant that can be “very effective” for both sleep and reduced pain in FM. A new formulation of Flexeril that may be effective for both sleep and pain is in the last stages of clinical trials.
Over-the-Counter Antihistamines (Unisom, Benadryl, Dramamine) – 25-50 mg
Teitelbaum reports that antihistamines are usually very effective, well tolerated, and only rarely do they aggravate brain fog.
Next Batch
If a person is still not getting good sleep, Teitelbaum tries the next batch of drugs:
- Klonopin (clonezepam) – 0.5-1 mg
- Zanaflex (tizanidine) – 4 mg (do not take with Diflucan (fluconazole).
Other antidepressants – use only 1 at a time:
- Sinequan (doxepin) – 5-10 mg or 10 mg/cc in liquid form; powerful antihistamine; some people get the greatest benefit with < 5mg.
- Elavil (amitriptyline) – 10 mg, may cause weight gain, very good for vulvodynia or nerve pain.
- Remeron (mirtazapine) – 15 mg, may cause sedation but worth a try when nothing else is working.
- Zyprexa (olanzapine) – 5 mg – an antipsychotic which is well tolerated at very low doses and helpful with sleep. Can cause weight gain but does help with deep sleep.
- Seroquel (quetiapine) – 25-50 mgs – similar to Zyprexa
Xyrem (GHB) – is the best deep sleep inducer on the market but is too expensive and difficult to obtain to recommend for most.
Peter Attia MD
For the past 8 years Peter Attia MD has been focusing on longevity. He hosts the popular “The Drive” podcast.
Peter Attia, MD is a big name in longevity circles. Attia got his M.D. at Stanford, spent 5 years as a general surgery resident at Johns Hopkins, then two years as a surgical oncology fellow at the National Cancer Institute, and worked with the consulting company McKinsey and Company. For the last 8 years, Attia has focused on longevity, and for the last 4, he’s been producing a popular podcast called The Drive.
While podcasts that focus on things like strenuous exercise don’t resonate with ME/CFS/FM and long COVID patients, podcasts on things like diet, sleep, heart rate variability, glucose monitoring, rapamycin, metformin, and hydration may all provide insights into factors associated with chronic fatigue syndrome (ME/CFS), fibromyalgia (FM) and long COVID.
For me, Attia (and Huberman, below) are a cut above. They know the science inside and out, and Attia often passes a critical eye on study methodology and rigor. In short, both seem quite trustworthy.
Over the past couple of years, Attia devoted six podcasts to discussing sleep issues with Mathew Walker Ph.D. , the founder and director of the Center for Human Sleep Science, and author of the 2017 book, Why We Sleep: Unlocking the Power of Sleep and Dreams.
In April 2020, a website called Brainflow, which listed Attia’s sleep protocol, provided the data for this blog.
Peter Attia Sleep Supplements
Magnesium
Attia is big on magnesium, supplementing it, apparently, during the day and at night. According to Brainflow, low levels of magnesium can keep your brain from settling down at night, whereas higher levels of magnesium promote a night of deep sleep and have calming effects on the body as well. Attia has said he uses various kinds of magnesium over time, but in one interview, said he prefers magnesium threonate before bedtime for sleep.
Chillisleep OOLER Cooling Sleep System
Attia apparently loves Chillisleep OOLER Cooling Sleep System (which he upgraded to from the Chilipad Sleep System). Various iterations of the sleep system exist ranging from $439 to $1300.
The system was designed around one central fact: we sleep deeper when our environment and our bodies are a bit cooler.
In order to go to sleep, our bodies need to cool down a bit, which is why it’s better to have your room cooler at night. (The optimal bedroom temperature is apparently between 60-67 degrees. Chillisleep says 65-68 degrees is optimal for deep sleep)
It’s also one reason why “The Sleep Diplomat,” Matthew Walker, says that eating less than a couple of hours before bedtime can disturb our sleep. Digestion causes our bodies to heat up a bit.
In the Chillisleep system, temperature-controlled water gets circulated through the Chillisleep cooling pad. Since different people sleep better under different temperatures, you can set your optimal temperature. You can also get a couples system that cools down one side of the bed at different rates than the other side.
If you have the Ooler Chillisleep product, you can even have the temperature of the pad vary over the course of the night. For instance, if you tend to wake in the early morning, you can have the temperature of the pad drop during that time. If you want to wake up at a certain time, you can have the water in the pad heat up.
It’s a pricey product, but it gets good reviews on Amazon and elsewhere, and if you have the cash, it might be worth it.
Andrew Huberman, Ph.D.

Andrew Huberman PhD is a Stanford neuroscientist and podcaster
Andrew Huberman is a neuroscientist and Professor in the Department of Neurobiology at the Stanford University School of Medicine. A McKnight Foundation and Pew Foundation Fellow, he was awarded the Cogan Award in 2017.
Huberman has worked on neural regeneration, on how vision and how we breathe affect performance, and is developing tools to enhance neural plasticity, reduce stress and optimize sleep. He’s been doing his Huberman Lab podcasts since 2021 – and he’s quite popular: in 10 days the Sleep Toolkit: Tools for Optimizing Sleep and Sleep-wake Timing podcast this part of the blog was taken from received over 200K views.
Huberman recently did a podcast with Peter Attia on hormones, fitness, and longevity. Like Attia, Huberman seems quite rigorous and trustworthy.
Except for this section, this blog does not cover sleep hygiene – a potentially important part of getting a good night’s sleep. Huberman has such a different take on sleep hygiene – which he believes starts when you wake up – that it’s being covered here.
Huberman was quite focused on two aspects of getting good sleep that don’t receive as much attention as they might: temperature and light.
In order to go to sleep, your body temperature must drop by 1-3 degrees, and every time your body temperature rises, your levels of cortisol – a stress hormone – increase. Health Rising recently featured a blog on researchers who believe they’ve identified a “hyperarousal” sleep disorder that’s associated with high cortisol levels which, in turn, cause interrupted sleep.
While we probably all know that bright, artificial lights are a no-no at night, Huberman reported that many studies show that getting natural light early in the day, and then late in the day, is quite important as well. He divides the day up into three critical periods.
First Critical Period: approximately the first 3 hours of daylight
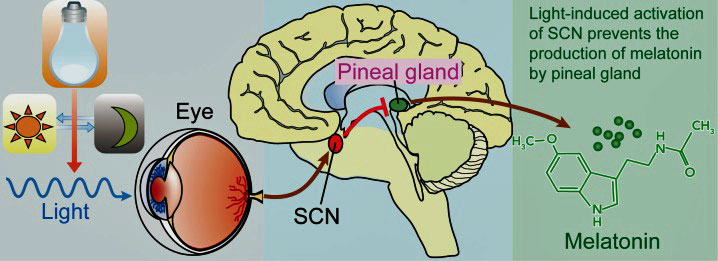
Early morning light boosts cortisol and serotonin and shuts down melatonin production allowing us to wake up.
Getting bright light – ideally from sunlight – early in the morning triggers an increase in cortisol (that’s precisely the time it’s low in ME/CFS) and serotonin levels, and washes out adenosine. Doing so helps the brain/body to wake up and starts a timer which should help you go to sleep at the right time at night. Not being exposed to natural sunlight may also contribute to depression and even possibly dementia.
How much you need depends on your makeup, and the amount of light present, but it generally doesn’t take a lot. Huberman said that on a clear day, about 5 minutes of sun exposure in the early morning should do it. On cloudy days, ten minutes is usually enough and on really overcast days, it may take 20-30 minutes. Even on cloudy days, the light intensity outside is much higher than anything you can produce at home.
It’s much, (much) better to get outside as it takes much longer to trigger the reaction while looking at the sun through windshields or windows. Alex Fergus states you should not wear eyeglasses (block UV light) as well. If you’re bedridden, try to get near a window or open the window and look outside.
- Check out Alex Fergus’s post on early sunlight
If can’t get out or live in a part of the world where it’s really dark, sunlight simulators like ring lights, or a drawing LED tablet, can help.
After that – getting under some cold water – just for 1-3 minutes – will increase your core body temperature, increase your cortisol and get you going. Eating earlier in the day will also trigger an increase in metabolism and heat that will increase wakefulness. Eating a very large meal, though, is going to divert a lot of blood and critical resources away from your brain, etc. and make you feel sleepy.
Caffeine – try to delay caffeine uptake for 90 minutes after waking in order to wash adenosine out of your system; it will delay the afternoon crash. Drinking caffeine after 4 pm can make it difficult to sleep and will disrupt your sleep architecture.
Second Critical Period – middle of the day
Naps are fine; in fact, Huberman himself loves naps. Just don’t nap so long that it disrupts your ability to fall and stay asleep. He suggests trying the Reveri app, yoga nidra, and NSDR scrips to get the best good naps.
Third Critical Period – late afternoon and evening
Getting sunlight in your eyes in the afternoon and early evening hours as the sun starts to descend is actually protective against problems with blue light problems. The different wavelengths of sunlight found as the sun goes down tell your brain/body to start getting ready for sleep.
Bright artificial lights of any color should be avoided at night. In the evening hours, it takes very little bright light to wake up your neurons and eliminate melatonin. Overhead fluorescent lights should not be used at night; instead, use desk lights and dim your lights and dim any screens.
Cooling is the key at night. Taking a 20-30 minute hot bath or sauna in the evening will cool the core of your body down and ready you for sleep. Sleeping in a cool environment is very helpful.
Supplements
Every night: 30-60 minutes before bedtime
- Magnesium threonate – 145 mg – causes gut troubles in about 5% of people.
- Apigenin – 50 mg – is a flavinoid that’s especially abundant in chamomile and alcohol, and appears to have calming effects. According to one site, it should be taken with some fat. Diets high in apigenin were associated with better sleep in one study and enhanced sleep onset and sleep time in a mouse model.
- L-Theanine – 100-400 mg – can give some people vivid dreams.
Huberman believes these supplements are preferable to melatonin.
Every other night – 60-90 minutes before sleep
- Myo-inositol – 900 mg – Huberman reported that myo-inositol enhances ability to fall asleep quickly and go to sleep after waking and also reduces stress and anxiety. Myo-inositol or inositol (or B3) is found in oranges, pears, peaches, beans, brown rice, nuts, seeds, and various other fiber-rich foods and citrus fruits, and may be able to “help balance serotonin, dopamine, and other neurotransmitters”. The highest concentations of myo-inositol occur in the brain.
- A 2022 study found that myo-inositol supplementation (2,000 mg of myo-inositol and 200 μg of folic acid) improved global sleep quality, subjective sleep quality, and sleep duration during pregnancy. Reduced frontal cortex myo-inositol was found in adolescents with poor sleep and depression. Myo-inositol also improved thyroid functioning, and when taken in combination with melatonin, improved glucose metabolism in menopausal women.
He takes these every third or 4th night. Taking them too regularly does not work for him.
- Lysine – 2 grams
- GABA – 2 grams
Others
Apps and Tapes
- Reveri App – Huberman is very high on this self-hypnosis app. Check out Huberman’s podcast with Reveri co-founder Dr. David Speigel. Huberman also recommends doing the Reveri sleep self-hypnosis app (10-15 minutes) 3x a week at any time of day to rewire your nervous system and help you relax faster.
- NSDR – Huberman uses NSDR (check it out on YouTube) to go back to sleep when he wakes up in the middle of the night.
- Yoga Nidra – he also uses Yoga Nidra (also on YouTube) to go back to sleep.
Tools and Breathing
- Eye mask – make sure the room is cool when you use it or it may heat you up.
- Ear plugs.
- Elevating feet – increases the depth of sleep; improves glymphatic flows (can exacerbate acid reflux in some).
- Nose breathing is very helpful – Huberman recommends that you try putting medical tape over your mouth at night. You can also train yourself to nose breathe over time. It’s hard to do at first but opens airways to the skull – allowing you to breathe more easily at night. (See Butyeko breathing.)
Other Sleep Resources From Health Rising
Our ME/CFS and FM Sleep Center contains everything Health Rising has on sleep, including links to sleep research, diagnosis, treatments, and more. Plus check out the overall results from Health Rising’s Mammoth ME/CFS and FM Sleep Survey as well as two adjuncts to it.
- ME/CFS and Fibromyalgia Patients on other sleep Drugs
- ME/CFS and Fibromyalgia Patients on the Drug Combinations That Help Them Sleep
Support Health Rising!







I wonder what happens to these recommendations when you throw sleep apnea into the mix? (Common co-morbidity with ME/CFS).
For instance, gabapentin is a respiratory depressant, and those effects are increased when paired with opioids or other CNS depressants (e.g., anti-anxiety medicines, antidepressants, antihistamines), some of which are recommended here.
I take gabapentin for neuropathy, but I take it in the morning so it’s wearing off by bedtime. It does help me sleep deeply, but I wake up periodically with apnea events.
Thanks for your post, Birdie. I use a CPAP machine for obstructive sleep apnea, and also take Klonopin, which has CNS suppressing properties. I hadn’t considered the implications of this combination. 🙏
From my understanding and experience someone with severe ME could sleep for hours and hours, and still wake up feeling ill and unrefreshed. I believe the cause is far more serious and deep rooted…eg. lack of uptake of oxygen at mitochondrial level.
And the amount of detail in this piece, and supplements measuring required, are both way beyond my abilities.
This blog didn’t deal with causes. I am looking forward to THAT blog. Whenever we find out the cause or causes – that will be a different story entirely – and we’ll know what to target. Hopefully, that will be sooner rather than later. Until then we’re left relying on doctors’ and patients personal experiences.
Inflammation in the brain, nothing new here.
My understanding of this is ,we may “sleep” ,but were not actually going in to the REM 3 REM 4 deep sleep cycles ,and thus not producing the Seretonum we will use for the next day (seretonum being a major player in the Oxygen/mitochondrial pathways)( this is why i take Nortryptileen at the correct time…5 hours before going to sleep…..and just doing that removed 99 percent of the Lactic acid burn feelings i was getting in my body each day especially in the underarm lymth nodes)
Hence we wake up just as tired as when we went to “sleep”
The 5-10 mins Bright sunlight before 9 am is one the body clock cycles we NEED to do each day
At night dim down the lights ,or as ive started doing ,i actuallt switch over to Red lighting
This Medcram youtube lecture has really good info on UV IR and melotonum etc
https://www.youtube.com/watch?v=5YV_iKnzDRg
Birdie I was glad to see mouth taping mentioned – sometimes simply doing that will decrease apneas, as well as sleeping on side.
I agree. I can sleep deeply for 8 hours or more and wake up like someone has given me anesthesia or heavy sedation. I had a sleep study to rule out abnormalities.
I think there is a much larger problem such as glymphatic system malfunctioning. Let’s get past talking about sleep aids and how to get to sleep / stay asleep, No matter how much “good” sleep I get, it’s like my body no longer registers sleep. It’s my most debilitating symptom & I wish someone would study this
If your body is not “registering sleep” then I would submit you’re not getting good sleep – even if you think you are getting enough sleep and your sleep study was OK. Not all sleep studies measure the kinds of problems that occur in ME/CFS. Sleep should above all be refreshing but unrefreshing sleep is the key sleep complaint in ME/CFS.
If I remember correctly sleep studies are getting more sophisticated. Hopefully, they’ll develop enough to pick up everything that’s happening in these diseases during sleep.
I have sleep apnea, more specifically UARS (upper airway resistance syndrome), which is defined as a partial obstruction in breathing whereby the brain arouses too soon and the patient “awakes” (i.e., microawakening) before a full stoppage of breathing (apnea) can take place.
For 7 years, I’d tried in vain to get better sleep quality: trialed 28 drugs; numerous interventions, supplements, etc. I am severe, bedridden for over 5 years. Only recently—in the last couple of months—have I experienced an improvement in my sleep quality, this due to a protocol I’m currently on via Dr. Andrew Heyman (see him mentioned in a past Health Rising article detailing Dr. James Buselli’s partial recovery). This improvement in sleep quality has in turn given me more energy, reduced my fatigue, has allowed me to get out of bed more often, has enabled me to make myself 3 meals per day (previously only able to make lunch maybe 50% of the time), etc.
For me, sleep dysfunction is a big component of my illness. I’d read something about hypothalamic dysfunction and hormone imbalance as being a possible cause for ME/CFS sleep dysfunction. It would be so nice to see researchers focus on this aspect of the disease, as I’m sure a standard for improving sleep quality would benefit quite a lot of patients, which goes without saying, of course.
Congrats Dave! Thanks for sharing that and I hope the progress keeps up 🙂
Just wanted to update your info on Peter Attia. He is a huge proponent of low dose trazodone and takes it every night to increase slow wave sleep (deep sleep). You can find his take on it on his podcast (or clips that are circulating about it) and he just addressed it again on his most recent AMA.
Good to hear! I didn’t know that. 🙂
Thanks Jenn! That’s good to hear, have so much respect for Peter Attia.
i find it al so easy said for an illness where they do not even know the causes, the subgroups, etc and for the 25% ME group, for excample who can even not stand light (overloading), etc
many things i even do not tolerate. And many in the severelly affected group.
my sleep got also way worse when i got way worse until no sleep for 9 days until they gave me something. i think also, it is not a thing “alone”-sleep, it is our illness as a whole, one of the many symptoms.
i would have liked to read what real researchers in this field are thinking about it and are doing about it…
melatonine is here for excample contra indicated with auto-immune desease and auto-immune markers come back and back… i even do not tolerale it… and for excample 2 years in my illness a sudden change of night/day rythm. and temperature, oh my, for menopauzal women…. please let them study the brain, the boddy, these illnesses and come with total solutions and understanding…
I agree, very much. Since there is minimal knowledge about what causes chronic fatigue syndrome etc. how can I rely on the suggestions for sleep, or for anything to help me? It seems like a big crapshoot. My symptoms have gotten better over time, but it helps that I’m retired and don’t have very much stress in my life. I have avoided made making time commitments of any sort. I can’t make plans in the future because I never know if I will have enough energy on that day in the future. Sleeping isn’t a big problem for me although it has gotten worse lately. I’m not sleeping as heavily or as long as I should. Possibly I just don’t need as much sleep as I used to, I don’t know. But I’m really sick of being given a new set of possibilities that may or may not help, but aren’t consistently applied. This is a disease where they don’t know what causes it. Keep that in mind whenever you think you have a solution.
Unfortunately, not a lot of research is being done on sleep in these diseases. We’re left just going on good guesses and relying on doctor’s experiences.
Forget sleep, the whole treatment aspect for ME/CFS is a crap shoot – there are no FDA approved, not many clinical trials and doctors are trying what they find works. I would think THEY would say it’s a crapshoot. In fact, I heard one well-known doctor exclaim in a private conversation that we’re just throwing stuff at the wall and seeing what sticks. So yes, it’s all crapshoot- welcome to the club.
Two sleep drugs are in clinical trials for FM and/or ME/cFS though – TNX-102 and surovexant (?) I think it is.
thank you Cort! i hope with these drugs, that they look at whole the boddy (illness) and not only on sleep.
It’s the same even for ‘simple’ things like high blood pressure and diabetes. They give patients a number of things to try out and figure out which one sticks and which ones don’t. Often the medications will cause ‘side-effects’ for which they’ll.. give you another medication.
This was a key point for me, when I started talking about my health woes, to learn that basically most people have the same issues with the medical system and doctors.
They know very little as to what causes disease and health problems, in general, it seems.
Thank you for these thoughts. Well said!
A kiwifruit an hour before bedtime has helped me to fall asleep. Helped my digestion, too.
(I have had ME for 30+ years)
Thank you Cort, massive effort. The info is there and I guess we cherry pick what works for each of us. There’s no easy formula unfortunately. I’ve tried quite a few things over the years most without benefit and at great expense also I’m reactive badly to many medications. So basically only take blood pressure medication and apply heat and self massage and small careful stretches. I try to not take pain relief though occasionally I get desperate but it doesn’t really help also doctors are very reluctant to prescribe.Take care everyone
Should point out I am now older after a lifetime of this disease at varying levels it does fluctuate and am very bed/ housebound but am fortunate my husband is marvellous and I have no other responsibilities. Feel terribly distressed for those who are younger and those who are struggling.
One thing this blog brought out is that there is no clear roadmap; instead lots of different things to try. If you can get good sleep, though, I imagine its well worth the effort.
And I would try the non-drug/supplement interventions first!
They have been the most effective for me (early morning/late afternoon sun exposure). It took a few months – boy i have never been this sleepy come bed time.
I make no link with any health improvement and sleep. I sleep around 9 hours uniterrupted nightly. And I still wake up feeling very severely ill. That’s what I interpret unrefreshing sleep to mean.
I made an interesting discovery about sleep recently. When I got covid, I was taking antihistamines daily (as part of a protocol). Previously, I could only use compounded, pure diphenhydramine, but I found that my sensitivities had lessened and I could take OTC antihistamines, too. After I (eventually) recovered from covid, I discovered that with antihistamines I was sleeping like a baby! And I felt so much better! But only for a while (about 2 weeks, on average, for each type), and then it completely stopped working. Eventually, I spoke with a functional medicine doc who has a lot of experience with ME & comorbidities. Ah ha! she said. That’s Mast Cell Activation. Because histamine can disrupt the sleep cycle.
Next I did a trial of reducing histamines (DAO enzymes for foods, lots of quercitin, Vit C, resveratrol etc at bedtime for mast cell stabilization…) to test for histamine intolerance – and I felt so much worse! When I spoke to her again, I was so confused and discouraged as I was sure that this meant that it was not this at all. But she said, Yes! We are on the right track! HUH?!! She said that that’s what mast cells do – the antihistamines don’t stop working, but the mast cells just keep dumping more and more histamines! Anyway, she has just started me on a new regime of antihistamines + mast cell stabilizers (incl. ketotifen & LDN). I told her I’d tried LDN a couple of years ago, and it just made me feel worse – but again, it seems I confirmed her hypothesis, as I started LDN at 1.5 mg – she wants me to start at 0.5 mg! And only increase SLOWLY by 0.5 mg each time, to allow my body to adapt (and not piss off my mast cells?!). I’ve only just started, but so far I’ve slept 6-7 hours without waking…. Fingers crossed…..
Really interesting. I think you have a good doctor! Good luck with the regimen. Sleeping 6-7 hours without wakening is so rare for me.
Rare for me too. 6-7 hours would be wonderful!!
Hi Lisa,
May I ask which other products your functional doc put you on along with Ketotifen and LDN?
What reaction did you have LDN when you first tried it that made you stop? I’ve also tried it but felt worse on it.
Thank you!! I am familiar with Drs. Attia and Huberman and follow both Podcasts. I look forward to experimenting with some of the suggestions. FYI, I was diagnosed with ME/CFS summer of 1988 after getting mono and a severe ear infection Christmas 1987. Overall, 34 years later, I’m doing much better, but getting to sleep and staying asleep has been mostly elusive.
Thanks. I’ve picked up some new things. I’ll be trying L-theanine, 5-HTP, and a couple of others.
“Have a cold shower” is bad advice for the me/cfs community who experience recognised thermoregulation difficulties. We’ll still be freezing 3 hours later.
Right. Some people with ME/CFS actually do better with cold showers (I do) – they ramp up the parasympathetic nervous system – but those who can’t thermoregulate should take care.
Thanks Cort for the article! It’s very helpful to have a summary from so many excellent sources!
I’m addicted to Tart Cherry powder right now. I get sometimes 8 hours of Rem sleep for the first time in too many years to mention.
Tart Cherry increases your own production of melatonin as well as providing natural melatonin.
Sometimes I have lactic acid build up in the muscles after taking it but so far NAC has helped with this problem.
I’m curious to know if anyone else is having success with Tart Cherry?
Thanks and thanks for mentioning the tart cherry. I had no idea it could help with melatonin.
I eat cherries for the melatonin, too. Cherry juice and powder have no fiber and are high in sugar, so I eat (usually still frozen) cherries in the evening for dessert (kind of like eating forbidden ice cream — Yum!). I found that it takes 12-16 cherries to be effective, but they definitely help. I still only get 5-6 hours of sleep, but that is more than I get without the cherries. Perhaps I should try increasing my “dose.” I would love to get eight hours as you do. I have never noticed more lactic acid build-up than usual when eating the cherries, but I supplement with 500-1100 mg of NAC daily, so now I know why — thanks!
I felt compelled to comment with some warnings re doc parsley sleep remedy and any others which include 5 Htp, L-Theanine or potentially GABA.
Many people with M.E or Fibromyalgia in particular will be on TRAMADOL, or tricyclic antidepessants like amitryptilline or triptan type migraine medications like sumatriptan/rizatriptan etc.
These will interact with these “natural” supplements mentioned above and potentially cause SEROTONIN SYNDROME which is serious and potentially fatal. Anyone with any kind of seizure activity eg myoclonus should also avoid taking anything which increases serotonin levels.
I do wish these doctors would learn some basic stuff before just dishing out one size fits all remedies for complex probems.
Wasn’t there also recently a research article suggesting that some people with M.E have LOW cortisol levels, rather than high as is assumed? I may be remembering wrong but I think so, So taking some of these products could also exacerbate that by lowering cortisol.
If there was an easy answer to sleep probems in M.E and Fibro, so many people trying so many different protocols would have found it by now. Caution is advised before adding anything new into prescription meds.
Thanks for the warning it’s well-taken and I hope everyone hears it and if strange symptoms crop up they contact their doctors. I would note that these doctors are relying on their long experience with ME/CFS and FM patients. They did actually warn about side-effects they’ve seen pop up in these patients; for instance, gut issues with 5-HTP I think it was and Dr. Teitelbaum warned about depression in a small subset of patients with Ambien. Teitelbaum was the only one to advocate for sleep drugs and he’s been using them for decades in these patients. Since he did not mention serotonin syndrome I hope and assume that it hasn’t shown up in his patients much.
We know there’s low cortisol in morning – what’s not clear is what’s happening at night. The recent hyperarousal study suggests that some people with sleep issues cortisol is increased at night.
I agree there is no easy answer to the sleep problems in ME/CFS/FM – the many different things that health experts suggest indicates that this is a trial and error situation. That’s doesn’t mean, though, that nothing can help. For me – 30 minutes more sleep a night would be great. So would more deep sleep. Anything that moves the needle on any symptom in ME/CFS would be helpful and that’s what this blog and really any treatment blog is about – moving the needle.
Thanks for the reply Cort.
Yes I totally understand people are prepared to try almost anything if it helps – I did too, experimenting on myself like a guinea pig, prepared to take bad consequences in the hope something would help.
Don’t get me wrong Cort, I love your blog and am a regular reader, have been for years and really deeply appreciate all the hard work you put in on our behalf. Especially the get “The Gist” sections for days when reading the whole thing is too much to cope with. So certainly not criticising this blog at all, as it is useful and may be helpful for many people. I have had Fibro 28 years and ME for well over 20 years triggered first with the Fibro by a car accident. I am housebound and ususally not well enough to read the entire article and comment, so apologies if my comment came across as being totally against trying anything. Yes you are so right, anything that moves the needle even a little would be fantastic. I just jumped in as I was really afraid people on certain meds might rush to try some of these things without being aware of the risksand really harm themselves. I know I wasn’t aware of all these things when I first began “experimenting” on myself years ago and I used to be a nurse!
Thanks again for your brilliant website and your endless hard work to help us – I really appreciate it.
And I really appreciate your very generous reply, Maria! Thanks so much 🙂
Doing this blog acquainted me with several things that I, who am in dire need of better sleep, am going to try. I hope others find some as well.
Please don’t apologize for your comment. It’s extremely helpful!
Why We Sleep- good book well written. Room temp around 67 a big takeaway and why.
Increasing fiber in diet may increase deep sleep which is lacking and hard to get based on personal history. Deep sleep based on sleep tracker used over a year seems to be missing most.
Supplements listed all good I would add hops tea and lemon balm. Magnesium gabba melatonin all good from experience.
So what to do about night sweats and pain?
The chill pad wouldn’t work for me as after a night sweat, I get a secondary chill so it’s hot, hot, hot then cold, cold, cold–which is especially bad when one is damp. Happens every hour or so! I’ve tried so many things. Hormones work but I can’t take them now because of past breast cancer.
Then there is the pain, joint pain from EDS. I’m constantly changing positions to try to get comfortable. Norco and the other NSAIDS only partially help.
And then there are these Hyper-POTSy episodes where my ANS speeds up for what ever reason and I wake. And there is my collapsed nasal passage–again thanks to EDS. And don’t forget choking on saliva and other stuff sitting in my esophagus from achalasia. Almost forgot to mention having to pee–it takes me a lot of liquid to swallow meds. No wonder I fall asleep several times during the day before I go to bed!
The docs only recommend a C-Pap. The other issues, no clue.
I have ME / CFS and MCAS. It was the effectiveness of Aleve in helping me sleep–even when I wasn’t in pain–that made believe that disruptions in my sleep are the result of inflammation. These are the things that have helped me the most. I’m writing in case even one is helpful to someone else: magnesium oxide (worked better for me than any other form of magnesium I tried); progesterone cream (tiny doses can also be helpful for men); skullcap, pau d’arco, ginger, cat’s claw. I can’t take these herbs now because their antimicrobial effects stimulate my immune system. But, oh, what wonderful sleep I got with ginger and on day 1 of pau d’arco and cat’s claw.
None of them mentioned high THC cannabis which definitely helps me sleep.
THC never helped me, never did most CBD products, but I’ve been taking
a 66% CBD, 21% CBN, 7% CBG, 6% THC oil for the last few months and saw my sleep improve quite a lot.
The only sleep aide I have found without pushing Serotonin is Klonopin (clonazepam) 0.5 mg. Was Rx’ed 300ea. for years, not one problem. Then the good docs took it away, “benzos are bad for you and you will feel so much better later” Well doc I’m waiting (years) and now I have restless leg also, another use for klonopin. This fall we are to receive the great drug reveal from the FDA “what we meant to say” can’t wait! After YOU killed how many?
I do agree, Ron!
I am so thankful that quitiapine 25mg has been helping me greatly. I am generally getting within the normal range of deep sleep for the first time ever! It’s such a relief. No magic fix for me but a big improvement
Interesting – thanks for letting us know.
This is all very useful.
To go to the subject of blue light, I believe it is also implicated in macular degeneration. I’m trying to avoid blue light for that reason, and use computer glasses.
But what about LED energy-saving light bulbs that we’re being prompted to use these days to save energy? Wouldn’t they also be dangerous to eye health? And if your ambient light is from blue light, wouldn’t that also interfere with the melatonin cycles?
I don’t know about the LED’s but Huberman, in particular, suggested that lights should be dimmed and not overhead at night.
Cort, speaking of computer blue light: have you changed the brightness of this blog? I already have “night light” set on my computer and wear computer glasses and am having trouble reading this blog without squinting. It looks like the background is grey and the print doesn’t have enough contrast. I just wondered if you’d deliberately toned it down. I don’t want to change the settings on my computer just for this one blog. Thanks for any clarification you can give!
I haven’t changed anything on the blog. There is a lot of “action” in it. Maybe try printing it out – the print option works surprisingly well.
One silver lining of ME/CFS for me was that I was sleeping better. Walking a mile in the city was like hiking 10 miles up a mountain and I’d sleep 8-10 hours like a baby. Now that I’m recovering, I’m having a trouble falling and staying asleep, unless I walk miles at a fast clip.
If you are sick and yet unable to sleep, you truly have my sympathy. I can imagine that being one of the worst tortures.
If insomnia is not one of your symptoms though, I’d guess that the usual sleep hygiene and treatment should apply, sans the limitations like sensitivity to light.
I’m one who has a high cortisol level at night–twice the ‘optimum’ range. I think abnormal circadian rhythms are part of my sleep/fatigue problem.
I recently re-discovered Flexeril and it has been helping with extended sleep by countering EDS muscle spasms–maybe worth a try.
And when all else fails, like you Cort, cannabis quiets the overactive midnight mind.
After reading this I purchased some Magnesium Threonate. I had a wonderful sleep the first night but have not slept well for the next two nights. Still too early to tell. However, I am having trouble knowing how much to take. The blog mentions 145g. The tablets I purchased are 600mg magnesium threonate but state that they provide 50mg magnesium. Now, does that mean I should be taking 3 capsules or a quarter of a capsule? To which of those measurements does the 145g apply?
I am answering my own question! I have done some googling and it looks as though it is the ’50mg’ number that is the important one. I found this statement in a blog post by Brainflow. What is confusing, though, is that the amount stated is more than double what Cort has written above.
Dosage of Magnesium Threonate
Huberman recommends taking 300-400mg 30 minutes before bed. It can be a bit confusing when dosing Magnesium Threonate. For example, a supplement may say 2,000mg per serving, but if you look on the back it will say “144mg providing elemental magnesium”. This is the dosage you’re looking for, so 300mg would be two capsules.
More research. You really have to be careful on google. I went back to Huberman’s own post and found 145mg. However, two different sites, supposedly explaining Huberman’s protocol, cited 300mg. Frustrating! Dangerous!
I think magnesium is pretty safe but it is frustrating, I agree.
I use 0,5 -1 mg melatonin, so maybe start low until the personal dose is found?
Have never tried though what would happen if I used more, but probably feeling hung-over on melatonine.
I’ve been recently trying the nighttime gummies (PM Chews) from FABCBD that have me waking up in much less pain! I’m still tracking my sleep stats to see if they are making an impact there. I just checked the ingredients and there are several that are on these lists: L-Theanine, 5-HTP, Melatonin, Ashwagandha, GABA, and of course CBD. I ran out and had to go without them the last two nights, and my pain has been through the roof the last couple of days!
I also track my sleep stats using a Fitbit, and just paying attention to them helps with my sleep health. For example, I get a better sleep score by staying on schedule with the bedtime and awake times I’ve set. This motivates me to stay consistent.
I’m also a big advocate for using a sleep mask. As soon as I put my mask on, my brain knows it’s time for sleeping. It really does make everything darker, and the slight pressure is cozy once you get used to it. It becomes like a hug for your head. 🙂 And my optometrist said that wearing a sleep mask helps with dry eyes, as your eyes can open slightly while sleeping, which dries them out.
And I sleep best in the winter, when I awake and it is 64 degrees in my room. I am much more fitful during warm summer nights.
Thanks for this great writeup!
Thanks, Linda – the best thing I’ve found for sleep – high THC cannabis gummies – are not on these experts list. (l9l)
Trying various supplements over the years, I noticed HTP, reversatrol, and COQ10 have at times seemed to help aid in falling asleep and staying asleep. The prescription meds (nortripiline, gabapentin helped with pain and inflammation but not sleep). Melantonin had no effect. Lorazapam helped but eventually made me less sharp during the daytime. I couldn’t tolerate Ambien, scary. Whats helped me most over the long term is ldn. Its helped calm down the overdrive state and anxiety. Its a wonder drug at least for me. My daily life was unbearable after years of being unable to achieve deep sleep, and I totally understand how Michael Jackson would elect to be hooked up to a propofol drip.
I can recommend the Feel Bright Light which you attach to a baseball hat or visor. It has safe green light. More info on safe green light here, where they sell standing lights:
https://www.sunnexbiotech.com/
The use of magnesium-L-theanine compound sounds helpful but people who have Restless Leg Syndrome be aware: Magnesium-L-Theanine increases Dopamine levels. People with RLS don’t usually need more Dopamine — their Dopamine level can be too high.