

This blog asks if it’s possible to reduce the PEM period by doing things other than resting. It’s a long blog – you may want to print it out using the print button on the bottom left of the blog.

Small amounts of exertion (let alone getting on an exercise bike!) typically result in large increases in symptoms.
About 5 years ago, Health Rising did a post on possible post-exertional malaise (PEM) busters. Since then we’ve learned more about PEM, and people have tried more things, so it seemed like time for an update.
For those who don’t know, post-exertional malaise (PEM) is kind of like “it” in chronic fatigue syndrome (ME/CFS). PEM is so prevalent – and unusual – that the term didn’t even exist in the medical lexicon until the ME/CFS community spoke it into existence. PEM refers to a dramatic and unusual exacerbation of symptoms brought on by small amounts of exertion (potentially any kind of exertion, including physical, mental, emotional) that usually peaks a day or two after the exertion has occurred.
We don’t know what causes it, but thanks to some excellent recent work from the Hanson group, in particular – which has been assessing what happens before and after exercise at the molecular level – we’re learning a lot about it. The Hanson group’s recent proteomic and metabolomic findings jive with ME/CFS patients’ experiences: that is, while they found that some abnormalities crop up during the actual exercise session, the really big hit – the really large abnormalities – come after the exercise is over.
That points a big arrow at the recovery mechanisms that return the body to normality, or homeostasis. It also suggests that, if we want to reduce a PEM hit, while we certainly want to boost our ability to exercise, what we may really want to do is to boost our ability to recover from it.
Exertion – exercise, in particular – comes at a cost. As the muscles lengthen in response to the exercise, microtears are produced that the body must heal and “fill in” afterward. (It’s the filling-in process that creates larger muscles.) Along with the immense amount of energy produced comes greatly increased production of reactive oxygen and other species (free radicals) that the body must find a way to mop up. Many other factors most certainly also come into play. Studies of overtraining syndrome have found that hormones certainly do.
Layman’s Speculations
Uninformed with any real knowledge about what actually happens during the post-exertion period, I nevertheless offer some ideas. 🙂

Recent studies suggest that the repair processes that should kick in after exercise aren’t.
Body doesn’t ramp down – there’s some evidence that the body has trouble turning itself off, thus possibly keeping the healing process from kicking in as quickly as it should and allowing the damage to spread. Perhaps a signal, or signals, that tell the body to come off its exertional state don’t get fully produced, or are not responded to, leaving the body in a kind of jacked up and ultimately exhausted state.
The usual repair mechanisms are simply broken – the repair mechanisms don’t kick in, allowing the inflammation produced as an inevitable result of exercise to feed on itself – producing more and more symptoms until the body finally brings it at least somewhat under control.
An exercise trigger is present – while not as many proteomic and metabolomic abnormalities show up during the exercise period as in the post-exercise period, it’s possible that something produced during the exercise period throws the repair system off balance or overwhelms the healing process. High levels of oxidative stress that start an inflammatory cascade would certainly fit the bill. A South African group recently proposed that a hypoxic situation that results in an ongoing ischemia-reperfusion injury may be present.
The NIH’s Exercise Initiative should tell us much about what’s going on during exercise and allow us eventually to target places where the exertion and repair processes have gone awry. Until then, we’re guessing and probably using hammers, whereas in the future we’ll be using scalpels.
Targeting the Post-Exertional Malaise Period With Treatments
“I think the overall story now is people with PEM should be exploring anti-inflammatory approaches in different ways, especially those agents demonstrated to cross the blood-brain barrier. On the research side, we should be running clinical trials on various anti-inflammatories for PEM, and ME/CFS more broadly.” Jarred Younger
There doesn’t seem to be much of an effort yet to develop treatments that specifically target the post-exertion phase. Right now we mostly have one treatment – rest.
The next part of this blog will use a recent, excellent video on PEM from Dr. Yelman at the Bateman Horne Center as a foundation to review what we know has gone wrong in the post-exercise period, and my speculations on potential treatments that could be initiated or more likely boosted during the PEM phase to reduce it. Your help is requested in coming up with more treatment possibilities.
After that will come reports of PEM reducers that have worked in ME/CFS/FM community – at least for some people – followed by further ideas from outside the ME/CFS/FM community.
The Post-Exertional Malaise Hits in ME/CFS – and the Treatment Targets They Present
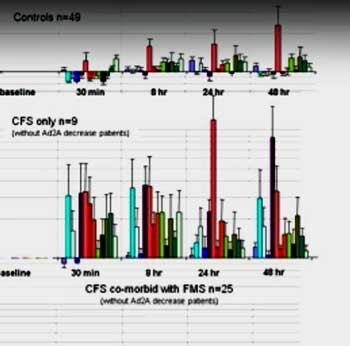
The most famous graph in ME/CFS history. Check out the huge difference in the metabolic/immune gene expression in the post-exercise period between the healthy controls top and the ME/CFS patients (second from top).
Massive Upregulation in Adrenergic and Metabolic Receptors – Yelman referred to still one of the most startling graphs and studies I’ve ever seen regarding ME/CFS. It concerned the massive upregulation in the gene expression of adrenergic and metabolic receptors that Alan Light found after exercise in ME/CFS in 2011.
The finding suggested that exercise was hitting the two sides of the stress response – the autonomic nervous system and HPA axis – hard, and producing high levels of metabolites associated with muscle injury. Follow-up studies highlighted the role of alpha 2 adrenergic receptors – which affect blood flows through the blood vessels – and a glucocorticoid receptor – which could affect cortisol sensitivity – during the post-exercise period.
(These findings foreshadow what we’re seeing in long COVID – problems with blood flows and cortisol. With regard to cortisol, it appears that the normal cortisol response is also lost in overtraining syndrome as well.)
- Possible Treatment Approach – boost cortisol, enhance blood vessel functioning via blood volume enhancers, and anticoagulants, change breathing patterns to support the parasympathetic side of the autonomic nervous system, take drugs that normalize ANS functioning such as Mestinon, propanolol etc., when appropriate pre and post-exercise???
Cognitive Issues – Gelman also referred to Dane Cook’s exercise study which showed that, in contrast to healthy controls – who got “smarter” after exercise, ME/CFS patients’ cognitive problems worsened and were accompanied by changes in brain activity not seen in the healthy controls. Gelman suggested that an uptick in microglial activation and neuroinflammation could be causing these problems.
- Possible Treatment Approach – emphasize knocking down neuroinflammation with increased use of anti-inflammatories including supplements and drugs like etanercept, antioxidants such as intranasal glutathione, turmeric, etc. Try nootropics?
Lactate Accumulations – High levels of lactate (a very unusual finding, Gelman noted) were found in a part of the brain called the anterior cingulate cortex (ACC) in ME/CFS. The ACC has been intimately tied to the sickness response (flu-like symptoms, fatigue, etc.) that the brain produces during an infection. PET scans and ME-spectroscopy studies also suggest neuroinflammation is present in ME/CFS. Plus, BOLD studies suggest reduced blood flows to the brain as well as elevated activity in the prefrontal cortex.
- Possible Treatment Response – focus on reducing lactate levels with supplements, breathing techniques, stretching, increase blood flows to the brain, knock down neuroinflammation.
Activation of the dorsal midbrain after exercise could be affecting things like attention, mood (ever feel depressed while in a PEM state?), threat (hypervigilance), pain, sensory processing (problems with light, sound, smell), cognition, sleep, autonomic nervous system functioning and others.
- Treatment Approach – ???
Some other findings not mentioned by Yellman include:
Leaky guts spark inflammation
- Possible Treatment Approach – increase probiotics, prebiotics, and butyrate enhancers including fermented foods if you can handle them, mop up toxins with charcoal.
An inhibition or even loss of the normal metabolic response to exercise linked with peroxisome and fatty acid metabolism problems
- Possible Treatment Approach – mitochondrial enhancers (CoQ10, acetyl-carnitine, D-ribose, oxaloacetate, etc., muscle repair supplements and herbs, stay away from long chain fatty acid foods and focus on medium chain fatty acid foods such as MCT oil.
Viral Reactivation – Epstein-Barr virus reactivation has been found in several long COVID studies.
- Possible Treatment Response – increase antivirals, herbs, and supplements ( Ashwagandha, licorice, St. John’s wort, lemon balm, ginseng, and holy basil, Monolaurin: 1800 mg twice daily; Olive Leaf: 1000-1500 mg twice daily, L-Lysine: 1000-1500 mg twice daily; Cat’s Claw tincture: 30-60 drops twice daily).
Known PEM Busters For ME/CFS

Some people have found things that allowed them to return to normal; i.e. their ME/CFS baseline, more quickly.
Now that all this speculation has occurred, let’s see what the ME/CFS community reports helps to reduce PEM. Note that since we don’t know how to treat it well – Yelman stated there is nothing that definitively speeds up recovery from PEM – the first and best PEM buster is simply to avoid getting into it. Pacing is key. The turtle is the Bateman Horne Center’s mascot. More on avoiding PEM – and whether you’re doing all you can do to keep it to a minimum – later.
Yelman reported two things the Bateman Horne Center has found that can help with PEM in some patients.
Low dose naltrexone (4.5 mg or less) – It’s well known that LDN suppresses microglial activation and that is what the BHC believes is happening.
Dextromethorphan (cough syrup! – standard dose) – Dextromethorphan is an NMDA receptor antagonist that Gelman stated may also assist with the autonomic nervous system. It’s used directly before or right after an exertional event.
Several years ago, Jarred Younger reported that several studies have shown that dextromethorphan affects microglial cells in a different way than LDN does and proposed that it might work for those who didn’t get relief from LDN. Younger warned that taking it at 200 mg or higher could have dissociative and even hallucinogenic effects, and indeed, a 2006 FM study that used over that amount reported positive results in 35% of patients but negative ones in 40%.
Younger’s 15-week 2021 pilot clinical trial used a small dose (10 mg at morning and night) that would not affect central nervous system functioning but which, he hoped, would calm the microglial cells that he believes are causing neuroinflammation in a small study of fibromyalgia patients. General pain and maximal pain were reduced over the entire study period, but analyses indicated this was true only in the first part of the study – bringing up the specter of the placebo effect.
Dr. Bateman and Yelman are finding that it helps. It’s not unusual for a study to fail but for some people to benefit from the treatment that didn’t in the broadest sense hold up.
Tylenol as a PEM Buster – Christyne’s Experience
Tylenol may shorten PEM duration via TRPV1 reducing neuroinflammation from microglia
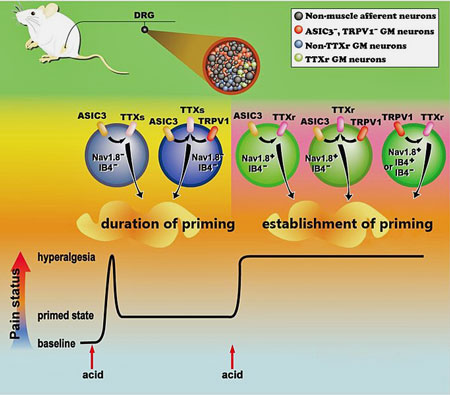
TRPV1 and ASICs prime the pain receptors for action in a mouse model of FM (Wikimedia Commons: Chen et. al 2014 Molecular Pain)
I watched Dr. Jarred Younger’s video describing inflammation and increased temperature in ME brains, Dr. Jarred Younger Presents: How We Can See ME/CFS Inflammation In the Brain – YouTube . As a result, I had a new experience with post-exertional malaise.
I have had PEM episodes monthly or so for years, and they’ve always lasted 5-10 (miserable) days. So I thought I would try taking a maximum dose of Tylenol (acetaminophen) anytime I had a low-grade fever, especially during PEMs. I was shocked to find my monthly PEMs shortened to 1 to 2 days for the first time in 14 years! and I had much less brain fog.
I wasn’t sure that the fever reduction would account for such a big effect, so I searched for a connection between brain inflammation and Tylenol in the literature. Recently it has been found that rather than impacting COX, acetaminophen impacts TRPV1, and TRPV1 impacts neuroinflammation from the microglia!
Dr. Renz-Polster et, al. describe the impact of neuroinflammation and microglial reactivity in ME/CFS and post-exertional malaise in their recent hypothesis paper, The Pathobiology of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: The Case for Neuroglial Failure. They propose that “PEM may reflect a stress-induced aggravation of CNS inflammation or neuroglial dysfunction”, (in addition to endothelial cell and mitochondrial dysfunction). Dr. Renz-Polster pointed out a paper Differences in Metabolite-Detecting, Adrenergic, and Immune… : Psychosomatic Medicine (lww.com), where TRPV1 mRNA was shown to increase more in ME/CFS patients than in controls after an exercise challenge.
That suggested that trying to reduce inflammation could be helpful. In a note to me, Dr. Younger agreed, stating:
“I think the overall story now is people with PEM should be exploring anti-inflammatory approaches in different ways, especially those agents demonstrated to cross the blood-brain barrier. On the research side, we should be running clinical trials on various anti-inflammatories for PEM, and ME/CFS more broadly.”
That provided some possible scientific justification for my experiences with Tylenol preventing and/or shortening the duration of my PEM. The question is, have other people used Tylenol for pain relief, unknowingly preventing or shortening PEMs?
Because PEMs happen the next day or more after exertion, it can be tricky recognizing cause and effect. I wonder, though, if others have found that Tylenol prevents or shortens PEMs in their experience. At the moment, I’m a sample of 1.
Now, I monitor my temperature and take Tylenol for a fever over 99F, which happens about every other day. If I plan to do something that I know is over my exertion threshold, I take a maximum dose beforehand and a maximum dose after. I follow the dosing limits, spacing them out over the recommended times on the bottle because Tylenol can be dangerous for your liver if you take too much. If I develop a fever after these doses, I’ll take another at the appropriate time.
I had a really long doctor’s appointment (3 hours in their office), that would normally put me into a bad PEM. But with the Tylenol, I didn’t get one at all! I was just a little more tired for a day, but no tachycardias, brain fog, memory loss, difficulty speaking, staggering, full body pain, diarrhea, etc.
I was so relieved! I have been able to stay upright longer than my typical 15 minutes per 1 ½ hours since I started this approach. But, of course, I got excited and pushed it by staying upright after my back and neck were getting tired. I managed to trigger a post-exertional malaise.
So I started Tylenol as soon as it started, and the tachycardia and brain symptoms only lasted a half day! Again, so relieved! Only a day in bed instead of a week. Now I’m being more careful with increasing my upright time, but it is increasing. I can’t walk very far, but my walking distance has doubled so far, with Tylenol. I haven’t had any PEMs since.
I will continue taking the Tylenol when I need it, but I have also started Mestinon (pyridostigmine) after hearing Dr. Systrom’s talk about its use for preventing PEMs to the point that patients can tolerate reclined graded exercise therapy.
My rheumatologist agreed to try it with me when I brought him Dr. Systrom’s recent paper on Mestinon. Neurovascular Dysregulation and Acute Exercise Intolerance in ME/CFS: A Randomized, Placebo-Controlled Trial of Pyridostigmine – PubMed (nih.gov). I hope the two treatments together are going to make a big difference for me. This is the first time in a long time that I have some real hope for improving this disease.
Reducing Lactate Accumulations After Exertion
“Hip” came up with the following protocol he devised after assessing athletic performance studies:
-
- Creatine hydrochloride (2 grams) – This study shows that the supplement creatine reduces blood levels of lactate from exercise. And this study found creatine increases muscle recovery after injury.
- Citrulline (1000 mg) – This study found citrulline reduces lactate levels produced by exercise.
- Branched-chain amino acids (BCAA) (5 grams) – This study found that BCAA reduces lactate levels produced by exercise (and this study found that by inhibiting the L-system transporter, BCAA suppressed the uptake of tryptophan, thereby alleviating fatigue).
- CoQ10 (800 mg) – This study found that co-enzyme Q10 reduces lactate levels produced by exercise (in myotonic dystrophy). And this study found Q10 improves muscle endurance. Hip finds taking 500 mg before an activity really helps.
- Sodium bicarbonate (¼ teaspoon (1.5 grams)) – This study suggests that sodium bicarbonate (bicarbonate of soda) can help neutralize lactate circulating in the blood.
- Catalase – 600 mg (taken after exercise)
- D-ribose – (5 grams three times daily) – One person reported: “I gave the d ribose a go and I am now on 10-30g a day. This seemed to drop the severity of the episodes for me. Before taking it I would be laid up for around 3 – 4 days. Now it’s 12 – 24 hrs recovery time when I overdo it.“
Some people find that short-term use of Ativan can get them through difficult situations
Ativan (Lorazepam)
Some people find that short-term use of Ativan can work wonders when they need to get through a difficult situation. Ativan is a benzodiazepine-based sedative-hypnotic that one book stated has a “relatively clean side effect profile”. Primarily used to treat anxiety it calms the central nervous system down by enhancing GABA activity. Dr. Paul Cheney once famously said something to the effect that if he could just put ME/CFS patients in a coma state to calm their central nervous systems down he thought that would work wonders. That’s what Ativan appears to do – for short periods of time. (It can only be taken for short periods of time.)
Mental Exertion
- Prednisone – at a dose of 20 mg or so taken 4 hours before the event. Some ME/CFS patients have vouched this works very effectively and reliably (though others report ill effects from this corticosteroid drug). See this thread. But also see the warning in this post (which cautions against using prednisone for any extended period of time, and warns that the PEM protective effects do not work for the whole day, they seem to wear off after about 6 to 8 hours).
Brendan’s PEM Buster
Brendan says the below regime drastically reduces his chances of getting PEM. He takes this combination only within a 48 hour window of exertion.
-
-
- Anti-inflammatories taken before and after exertion plus an antihistamine, and curcumin (taken together and repeated every 4 hours for a day or two).
- Also a teaspoon of baking soda in a glass of water morning and night.
-
Note: he recommends the anti-inflammatory always be taken with food.
Breathing Better
Calming breathing techniques can also help.
We also have evidence that the breathing is off during exercise, and generally, and that people with ME/CFS are bringing in too much air either by hyperventilating or breathing too deeply. That reduces CO2 levels which, in turn, can constrict the blood vessels, thus impairing blood flows to the brain and muscles, as well as other things.
- Possible treatment approaches – Better breathing patterns during and after exertion to bring up CO2 levels and increase blood flows to the tissues and brain; practice nose-breathing, watch breath holding, emphasize exhalations, try Buteyko breathing, Wim Hoff, ???
Blood Volume Enhancement
Making extra efforts to increase blood volume before and after exercise makes sense given the low blood volume found in ME/CFS. Several people reported in the last survey that enhancing blood volume, whether by adding salt, drinking electrolyte drinks, or increasing water intake, helped with their PEM. Check out one person who improved her ability to exercise by using saline IVs.
Stretching
Stretching has helped me recently in the PEM period, and I have a blog on this coming up. Because stretching increases blood flows to the muscles, reduces lactic acid, and relieves painful, contracted muscles, stretching during the PEM period, in particular, seems like a no-brainer for most of us. Several people reported in reply to the last blog that stretching/yoga was helpful.
Other reports from the ME/CFS/FM community
Other PEM inhibitors reported in the last blog:
- Mitochondrial supplementation – pre-dosing with NAC, AMP, NADH and B Complex and glutathione intramuscular (self) injection, and creatine, D-Ribose, acetyl-l-carnitine and COQ10 as oral supplements.
- Staying calm.
- Oxygen therapy.
Other Ideas From Outside the ME/CFS Community
Enhancing Muscle Repair
How about enhancing muscle repair? Various websites tout supplements and herbs, often different supplements, as a way to increase muscle repair – in healthy people. ME/CFS patients are, of course, a different bag, but people with ME/CFS have found that some of these can help.
Frogfuel suggests
-
-
- Tumeric to reduce inflammation.
- Tart cherry extract to reduce inflammation and uric acid buildup.
- Medium-chain triglycerides (MCT) fatty acids to reduce lactic acid buildup.
- Collagen peptides to construct new connective tissues.
-
Muscle and Fitness suggests
-
-
- Creatinine monohydrate to boost ATP production in the muscles and help them regenerate.
- Whey protein powder “to provide the basic building blocks needed to repair and rebuild damaged muscle mass.”
- Branched-chain amino acids (BCAAs) that are “important for muscle growth and recovery because they help reduce exercise-induced muscle damage.”
- Formula XI, which contains creatine monohydrate, beta-alanine, betaine, L-Ornithine, D-Ribose.
-
Rootbabes.com recommends these herbs:
-
-
- Tumeric – to fight inflammation.
- Green tea – helps to process carbs and may be able to increase muscle mass. Possible Rapamycin analogue.
- Ashwaganda – may be able to increase oxygen consumption and build muscle mass and strength.
- Boswellia – is used in Ayurvedic medicine to increase blood flows to the connective tissues.
- Eleuthero (Siberian ginseng) – may increase oxygen uptake and decrease lactic acid.
- MACA – muscle-building properties.
- Rhodiola – increased endurance.
- American Ginseng – improve oxygen uptake, reduce lactic acid, reduce inflammation.
-
Cold Immersion
Wim Hoff has made putting yourself in cold, sometimes very cold, temperature a hot … err … topic. Brief periods of cold immersion, whether in the shower, the bath (ice baths!), in a cryotherapy chamber, or by plunging into the nearest freezing body of water, is often combined with breath training, meditation, and yoga to increase blood flows, improve oxygenation, kick in the parasympathetic nervous system and produce, believe it or not, a calming effect. One small fibromyalgia cryotherapy study found that it improved quality of life.
Andrew Huberman Ph.d. reported that A meta-analysis of cold-water immersion effects on recovery after exercise found that it “can be a highly effective recovery tool” and recommends that it be done 6-8 hours after exertion.
Question
What have you found helped during the post-exercise period to get that nasty period of PEM over with as quickly as possible? Please let us know in the comments.
Did the blog spark any new ideas? If so, please support Health Rising and keep the information coming.






I’ve accidentally stumbled on Fenofibrate being a PEM buster for me, on both the time scales I experience pay (intra-day and multi-day). It seems to shorten crashes & even reverse baseline lowering that I noticed was starting to creep in (shorter upright time to head sensations).
The couple of times that I have remembered to take it before a bigger activity, it seems to have helped avoid or limit
It’s hard to be sure of course. I had a run of better luck with it, and so I now don’t dare to have a crash without it.
But it is a well-known, widely-available, widely tolerated drug, so I wanted to share.
It’s possible this aligns with the recent reperfusion hypothesis of PEM from the micro-clots folks. PPAR agonists (including Fenofibrate) have been used as protection from reperfusion injury:
https://en.wikipedia.org/wiki/Reperfusion_injury#Reperfusion_protection_in_obligate_hibernators
Thanks – that’s exactly the kind the thing I was hoping would spring up. Kell and Pretorius recently published a review suggesting that ME/CFS and long COVID are reperfusion diseases. I’m about to dig into it. 🙂
Do you think they may be a type of angina Cort?
Viyer05 can you comment on the dosing of Fenofibrate that you’ve tried and which dose you’ve found most helpful for you? Thanks!
Regarding the Tylenol pen buster. Years ago when I could semi function, I had a girlfriend. We had partied and the pem kicked in the following morning. It was bad.
I asked her if she had some pain killers. Unbeknownst to me instead of paracetamol, she gave me some really strong post operative pain killers she had left over from an operation.
I went from having all the classic pem problems, pots etc to feeling amazing. Stopped the pen in its tracks.
It definitely shit down the signals in the head and the inflammation.
I thought, if I could have this everyday, I could live a normal life.
God bless the queen btw
fascinating! just reading the wiki article on reperfusion injury is ringing all kinds of bells for me. seems to link with a number of hot topics in mecfs, and cold exposure shown to help. i have experienced a toe wound that wouldn’t heal as well, which could be explained by this. https://en.wikipedia.org/wiki/Reperfusion_injury
How much do you take per day? Thank you. Debbie
“Body doesn’t ramp down” – I used to try to analogize this to my treating physicians and I stopped making this complaint because of the looks I get from “Sports Medicine” Physicians who are perfectly healthy and never experienced any adversity from what we are looking to treat. I digress, this symptom is the single most obvious symptom I’ve always had, I would exercise and my Heart Rate would stay elevated for at least 48 hours in which I could not sleep or relax. I would then have some sort of arrhythmia or bump in my heart and my heart rate would drop to the low 60s and I then felt I could rest. Another 2 days and I could exercise again. One day in my 40s I no longer got that bump/arrhythmia and my Heart Rate stayed elevated eventually being diagnosed with POTS. There is something to this symptom and although beta blockers slowed my Heart Rate, the rest of my body didn’t feel that relaxation and recovery as before. I find it very interesting because, in the 29 years that I’ve been trying to find a treatment and properly explain my symptoms, this is the first time I’ve seen it in print. Thanks, at least this is encouraging. (PS: Yes I did have a cardiac workup, echo, cath lab, halter monitors, etc. But I could never get them to give me a 30-day monitor workup, always a 24-hour workup which is not enough to produce the arrhythmia in question.
Curley60 – my rule of thumb these days is, never go to a doctor who is perfectly healthy! My best results invariably come from finding a doctor who has the same illnesses I’m dealing with. “Specializes in …” frequently turns out to be code for, “I suffer from this too”. I use the same rule for physical therapists, trainers, etc. It’s caused a marked improvement in the relevance of the listening, and the care I get.
Dear Ron, from September 5, 2022,
Your post about never going to a doctor who is perfectly healthy rings very wise and true. I appreciated your insights.
You sound like a seasoned elder.
Thank you.
Try tachycardia is reflex from impaired venous return. Phenylephrine or midodrine can help
You could add Beta Alanine to the Lactate treatment options, Beta Alanine is a great acidity buffer used in gym training allowing athletes to extend their training sessions. You get a brief weird tingly sensation upon dosing but it disappears quickly, but it’s effects can be quite noticeable.
I get horrible post-MENTAL exertion fatigue (brain crashes after I pay attention/think hard for more than ~20 mins) to the point I can’t read or process info or write. And resting doesn’t seem to help. I’m down for the day. Only an overnight sleep helps, if it does.
Might the supps recommended for the cognitive issues after physical exercise be useful in this scenario?
Hi,
I feel better after been prescribed L carnitine, Q 10 and B12. I have the same issue with mental , now better. Still very hard to speak on the phone though.Brahmi, also, helps with the brain fog. Antihistaminics, said my doctor, may help with brain fog,so he is now going to double the dosis. Take care!
Thank you!
MCT oil. Nutrition that supports the brain avacado nuts olives ..oils really help me sustain brain activity . Speech. Cognitive . …
Thanks! I already take some in the morning. Approx. 1 tsp. So glad it helps you.
Hi Syd,
I find dosing myself with half to one teaspoon of D Ribose from Now reduces my PEM brain fog a lot. Best taken before exertion, but helps if taken during PEM too. When I’m more fit, it can help me prevent PEM altogether
Annabelle
Thanks, Annabelle! I’ll retry it. (I tried it in the past and though I know it’s not supposed to, I felt like it messed with my gut. But that was a long while ago.)
SOOO glad it helps you. Woohoo!!
Same! I work in academia and this is crushing me. D-ribose has saved me, but I still get very bad PEM for both physical and entail effort. I can’t do much at all for at least 48 hrs (starting 8-36 hours following exertion), and in bad cases it can take a week or two or even three to stabilize. I travel to East Africa for work yearly and my trips home across 10 time zones cause horrible crashes no matter what I do. Any thoughts on that? Same when I get sick. I don’t follow the same trajectory as others.
Overtraining syndrome victim here. Triggered by months of pushing myself with intense aerobic and weight lifting. Struggled for years after my mystery flu.
My first insight was to focus on anaerobic exercise like weight lifting which had much lighter pem than post-aerobic. You are still exercising and enhancing aerobic capacity.
Walking every day, no matter what. Walking is the red line we do not retreat from.
I found that if I could get a good night of restful sleep after gym it would stop PEM in its tracks. Poor sleep is the key catalyst of a bad PEM and we all know it’s hard to sleep with PEM
Adaptogens helped with restful sleep and set me on a path. Chamomile. Valerian root, Theanine etc. CBD helped the best. Drops worked , but vaporising cbd flowers had the best effect. CBD is also legal in Uk.
I then tried actual weed. I hadn’t smoked weed in 20 years. I found that it worked the best. It would stop pem , increase appetite and give me the restful restorative sleep. You need to do it at least 3 hours before bed because interestingly it will keep you up with your thoughts running amok.
Marijuana, dare I say , has basically allowed me to get in the best shape of my life while keeping PEM under control.
After a while as I enhanced my capacity, as long as I didn’t push myself too hard, I wouldn’t even need to dose myself and I could recover next day.
As soon as I stop gym routine for a few weeks , I would just get PEM again and I need to get marijuana in the game again.
I wish I could get medical grade thc/cbd pill legally so I didn’t have to buy illegally and damage my lungs potentially. Im worried about buying illegal edibles because of potentially bad production methods. Flowers seem the least bad option.
I’m amazed at the effect THC has on my ability to exercise. Pain is a big part of my problem.
Dr. Sarah Myhill, MD’s treatment protocols of the EBV-caused epigenetic Kreb cycle and mitochondrial changes to the cells that result in a broken ATP production cycle may help. She has a great UK-based website and a couple of books out.
Following the late virologist Dr. Martin Lerner, MD’s c. 1995 supplementation program for improving ATP production also helps; almost all ones out now are based on it. Only change is to replace half the L-Carnitine dosage with it’s precursor (and anti-viral) Lysine, since Carnitine feeds the bad viruses, too.
Then a ‘clean’ anti-inflammatory/anti-viral diet (same thing!) and anti-viral supplements, herbs, and teas, such as Lemon Balm. Cutting out gluten, dairy, processed sugars & oils, and GMOs is #1.
‘Bad’ viruses excrete toxins, so don’t feed them. The HHV-family is the biggest offender, and it now has dozens of variants of each strain, with HHV-4 & HHV-6 being the most common worldwide. Knowing the exact strain really doesn’t matter, since every adult now carries HHV-4 and 80% carry HHV-6. Neutral or ‘Good’ viruses are generally not a problem,
Eliminate all synthetic chemicals (which the liver doesn’t recognize & process properly) and toxic heavy metals in your diet, cosmetics, and medicines. Fillers in pills and carriers in injections (especially preservatives & polysorbate emulsifiers that will now get into the brain) is a common source. Silica dioxide (silica) is OK. Natural ‘nano’ sources of minerals and electrolytes from organically-grown plants (grown in healthy soil and spring water) are OK.
How many toxins does your body have? Just look down. Can you do a bodybuilder’s ‘Vacuum’ pose? A yogi’s Lion pose? Do you have a fatty liver and a rounded upper belly? Does your stomach stick out? Some extra chub? The amount of toxins is directly proportional to excess body fat since that is where the liver-filter tags the unrecognizable/unprocessable toxins for storage, and why fat-burning diets make you feel like crap and do not work long-term.
It is also why ‘Patent’ Rx/OTC medicines will never cure anything, as anyone who has had cancer knows. 95% of cancers are viral+ toxin based. Ditto with any so-called ‘auto-immune’ or ‘idiopathic’ chronic disease.
The cure is basically all the same. That is what Western Medicine practitioners do not want the general public to know or be able to do (hence Good Health being an uphill battle). After the recent C19 disaster, it put society on the path to discover that and change that, so some Good will come from it.
A diet high in polyphenols (colorful veggies & wild berries), blood-cleansing water-soluable fiber and active enzymes (raw/uncooked) and with a lean & ‘clean’ protein source (pork, GMO or non-fermented soy, or farmed fish being the worst) will slowly sweep out those toxins.
Note that eggs & milk are high in baby-growing hormones (no matter what the source), and make the ‘bad’ viruses grow much faster, which is why they are often used to grow the viruses for vaccine products. They must be eliminated first if you are not a baby and are highly inflamed (chronically achy and tired).
They may be added back later ‘as tolerated’ when you get better. 🙂
Thanks for such a thoughtful reply
Same happens to me- I can read fairly tough to read articles like medical articles for about a 1/2 hour, then my brain goes mush and refuses to cooperate, and I just can’t concentrate trade any lo ger. It is maddening. It b3comes like trying to read a book while having a bad flu where you feel miserable, and you can’t think clearly.
CO-Q 10, Citruline, l-Carnatine, Alpa Lipoic Acid, and bentfotiamine are all not doing anything for me to help. Magnesium will help a little- but nothing to write home about.
I’ve read that ATP (I beleive it is, or something that has to do with atp) is invovled somehow, that as we work, our atp gets damaged, and our bodies can’t replace it fast enough like normal peoples bodies can. It takes our bodies several days to do what a normal body can do in hours, ie replace the damaged atp properly. I suspect also that we have chronically low atp stores, so our mitochondria are unable to be fed the fuel they need to properly run our bodies at normal speed. I might be a little off on this, but I do remember the article talking about the “fuel” not reaching out mitochondria correctly, so it’s like running a car with a malfunctioning carburetor, ie the fuel is prevented from reaching g the energy factory mitochondria correctly. I also remember so etching about the body not able to clear the damaged atp very well, which also prevents new atp from being able to reach its destination correctly.
As I said, I might be a bit wrong, but the basics are there- my mush mind got pretty tired trying to understand it all- but a search for “PEM and ATP” might yield some info
Thank you for the reply! I’m so sorry you’re dealing with this, as well. It’s awful, awful. I also think ATP is a big part of the issue. I was just exploring urothin a. NO clue if this is helpful, but I know it’s supposed to help with mitochondria, for those it does help. I’m also thinking about tiny doses of methylene blue. I have lots of other things going on, like a csf leak, so I have to be careful.
I hope you find something that helps you.
oops: I meant urolithin a 🙂
Thanks Syd- I will check that urolithin a out for sure- i had seen videos about methylene blue- but decided against trying it- but can’t remember why now-
Keep us posted!
I have PEM episodes that are triggered by genital herpes reactivation. Exercise will set off the herpes tingles and then PEM will follow. I already take 2000 mg of Valtrex pd but the herpes is still very active. Two weeks ago I discovered that cool red laser irradiation of the spots where the herpes attacks can reduce the severity and number of attacks. I have been using a home laser and it is actually helping the PEM and general low level fatigue. Went for a 700 metre swim yesterday which normally would leave me with some degree of PEM the following day, but I feel fine!
Wow that’s cool. What kind of laser do you use? I immediately thought of the cat toy kind, but I bet that’s not what you meant
What laser are you using, please?
https://luminancered.com/products/genital-treatment-device-luminance-red
I have used pacing to prevent/minimize PEM but occasionally get a whopping crash from an unexpected emotional hit that tips me into the same scenario of severe PEM symptoms. The last one happened several months ago. After a week of misery in bed I did my monthly injection of Repatha which was prescribed by my cardiologist for familial hypercholesterolemia. (The standard dose is one injection twice a month but I stretch it to once a month due to its cost). I started to bounce back almost immediately from full blown POTS that raised my HR to over 120 just getting up to water my house plants back to my normal walking tolerance of about 30 minutes. Repatha is a monoclonal antibody designed to grab on to and take out of circulation the PCSK9 protein which people with familial hypercholesterolemia genetically over produce. PCSK9 raises blood cholesterol by latching on to and blocking cell receptors that normally link to cholesterol allowing it to re-enter liver cells as part of normal cholesterol circulation. My theory is that the cholesterol molecule is similar to cortisol (cholesterol is the precursor to cortisol synthesis in the adrenals) and PCSK9 may also be blocking the uptake of normal circulating cortisol into cells resulting in the exhaustion symptoms typical of low cortisol with normal blood cortisol levels. Also PCSK9 would also block cholesterol entering the adrenals and affect synthesis of cortisol as well as aldosterone. Low aldosterone affects the renin-angiotensin system, sodium is lost through the kidneys, aggravating POTS which worsens PEM. Hence getting rid of PCSK9 with Repatha improved my symptoms. My thoughts on this theory apply to my experience and may not apply to everyone. There are many subsets in ME.
I am on a daily dose of anti-inflammatories (Naproxen 250 mg twice a day) and 12.5 mg of Benadryl every night. The naproxen has a side effect of retaining water and salt. Which is perfect yo keep the enormous amount of salted water that I drink daily. It keeps my pressure in a good position because I am not peeing everything that I drink ! :-).
Otherwise, my pressure is too low. With all this, my PEM last about 6-8 hours on Tuesday afternoon, very prévisible, after spending my weekend gardening heavily. I am about to celebrate 4 years of success with this easy treatment, I hope at least one person could benefit from it.
Lucie, What does the Benadryl do for you? And can you tell how you prepare your salt water?
Benadryl helps with sleep and allergies. Dr Nancy Klimas spoke about it in one Cort’s blogs. She specifically referred to antihistaminics from first generation, like Benadryl . In another article that I can not find back, a doctor who was also diagnosed with mecfs had observed that his allergies were increasing along with other symptoms (brain fog, fatigue, etc)
Salt water: I prepare daily a jug of 2.5 litres of filtered water. I add about one big tablespoon of salt to it. I carry a smaller bottle of it with me when I am out. I leave two glasses around the house to help me think to drink.
At the beginning of this “treatment” I was most of the time drinking the whole thing. Now I probably drink about two thirds. But seeing what’s left in the jug to be drunk helps me gage my daily consumption. In very hot days it Is a very helpful reminder. I barely sweat, therefore the heat really hits me and the water at that time is crucial.
side effects from Naproxen, not sure if Ponstan will do same with less side effects? ( personal experience)
Also…a stomach protector…forgot the name that I take daily
Please share the name of your stomach protector. I would like to take Naproxen but it hurts my stomach.
It is called pantoprazol
An interesting observation for me is that I also suffer from an antiflammatory form of arthritis and 50% when I over exert I get a CFS/POTS crash and 50% I get an arthritis flare within 24 to 48 hours.
I firmly believe it’s an inflammatory response because of this
Lansoprazole or Omeprazole. I’m on 30mg Lansoprazole every morning to protect my stomach from the rest of the meds I take.
The problem I had with Omeprazole was that after a number of years the joints in my hands started aching. I thought it was arthritis but then I read a paper online which said Omeprazole can give you ‘lupus-like aching of the joints! I stopped gradually (not easy because of rebound effect) and the aching in my hands went..hope thats helpful for someone.
Found your blog informative.
I use turmeric with meals sometimes, and will try it after exercise. Calming the nervous system is another good idea I will try. Thanks for doing all the research.
Glad you are taking stomach protector. I gave myself acid reflux after taking naproxen, maybe 250 or 350 a night, for many many years.
Yeah, that need to be clarified. Exercise intolerance refers to post-exercise inability to recover, not inability to exercise.
Post-exercise problem actually comes in waves. 30 minutes after, I conk out and have to take a short nap. Then, a few hours later, depending on the intensity of the exercise, I may keel over again for a couple of hours. Then finally comes the PEM the next day. Not sure if that is unique to me or other people have similar experience.
My PEM buster: traveling. It’s as if the excitement/stress works as a fire retardant, and I’m fully recovered when I’m on the road. But I still succumb to PEM when I’m back home and settle into routine life. My PEM now only lasts a day or two though, not days or weeks as it used to.
yes When I go away I get a boost of energy and life is so much better! But when I come
home it takes a day to ‘come down’ and then I am hit with PEM.This lasts minimum a week . Some times I think its worth it but other times I wish I’d stayed home.
Exactly the same for me. The more time zones I cross, the worse the effect. Sometimes 2-3 weeks if I travel really far.
Similar! I can also sometimes pull myself together if I need to (like I have to teach a class, nobody would ever know), but then I crash again even harder for longer. I have not found a magic bullet but d-ribose and electrolytes and salt help.
My son (teenager, mecfs, pots, mcas, housebound) has had zero PEM episodes in 10 months since we started him on oxaloacetate. Originally 1000mg/day, now down to 500mg/day with same benefit. He can go out for a medical appointment without crashing for 2-5 days afterwards! He couldn’t increase exercise for a long time but adding quercetin on top of his other mcas meds has increased his ability to exercise, still with zero PEM.
Sadly oxaloacetate hasn’t had the same PEM-busting effect for me (mecfs, mcas, housebound). So far the only pem ‘treatment’ that works for me is heart rate pacing (hr<100) to stop going into pem in the first place.
Aside re pem symptoms: like Cort, I stagger when in bad PEM.
Hi Andrew,
Sorry to hear your PEM hasn’t responded to your son’s treatments.
I wonder if you could share the dose and timing of the quercetin supplement he takes. Thanks
Re quercetin, 1000mg/day seems to be the usual dose. (Just check a lower dose first in case allergic). We started at 100mg, son got clear benefit so we up to 1500mg which gave a bit more benefit. Tried 2000mg but didn’t get anything extra from that.
What brand oxaloacetate?
Bene Gene is the only one I know of.
So what’s the consensus? 🙂
24 hour fasting is by far the most effective way for me to deal with PEM. Strangely, fasting has no noticeable positive effects on normal days.
Slow Controlled breathing (2 b/mn) is the second most efficient method, but need to breath so sometime during several hours to see any impact.
Cold bath is incredibly effective at getting rid of brain fog but its effect is so short lived ( few minutes) it’s not worth the effort.
I seem to have managed to increase what I am able to do, largely by what Dr Yellman outlines in his video. It can be very boring. 🙁 I’m also a great fan of Jarred Younger PhD, Michael VanElzakker PhD and Amy Proal PhD and so many others. So I’ve focused on an anti-inflammatory approach with my diet. Tried to improve my gut & healthy microbiome etc. Calming my sympathetic nervous system dominance and actively trying to regularly enhance my parasympathetic nervous system as much as possible. And improving my restorative sleep has been key.
Everything for me is connected. My ANS and my immune system are continually in communication (via vagus nerve?) So I can set off my fight/flight/freeze response, if I eat something that my digestive system doesn’t like. Calming down starts with not eating the wrong thing (which is most food). Also if I do too much, that also leads to me becoming wired, which affects my sleep, which makes me more wired and around I go.
If I’ve done too much I feel like a sinking ship and my brain feels like a dredger, scraping along the sediment at the bottom of a waterway. I do think there seems to be a lack of blood flow. I feel like I’m trying to squeeze the last bit of juice out. And I also find it difficult to evaluate what’s happening – I sort of feel driven to continuing whatever it is I’m trying to achieve.
Another aspect of PEM, that I think is usually discussed as a secondary consideration, is mental and emotional exertion. I would experience these, more than physical exertion and so often feel a bit of a fraud. I think these use an enormous amount of energy, both in short bursts and in a more prolonged way.
I’m constantly working on these areas and I’m always trying, at least, to stay just back from the edge, in every aspect of my life. I often wonder about the enormous toll that the lack of recognition and support has had on people with ME/CFS and now Long Covid? Apart from the frightening symptoms I’ve had over the years, the highest stress has come from not being believed and being harrassed and mocked instead. And stress is highly energy intensive.
I know benzodiazephines are not recommended in long periods of time, as they make a bad addicction, and the body adjusts to the dosis.
Still I think it’s important to keep searching for what makes ativan work.
I was “dead” in undescribable pain, extreemly POTS-hit, hypersensitive, and exhausted, for years. Benzos reduced my hypersensitivity my pain, and my brainfog a great deal.
Now the effect wears off. I wonder, though, if I could increase dose, what would happen. If Ativan is “my insuline” (it certanly felt that way), could I get a lot better by increasing? Except from audition, I have had zero side-effects (I do not tolerate other drugs well).
– I would gladly take the “coma” Garner suggests for some weeks if possible, and see what could happen after extreem rest:)
Our psychiatrist says the “addiction” to benzos is the body’s adapting to it, thus, people will up the dosage. He advised when it stops working, taper back down until off (yes, uncomfortable it will be). Then try a very low dose and it should work again. Do not keep increasing dosage! You have to let the receptors “clear” to be able to bind again. Many addictions are like this and can be dangerous to keep upping the dose when what used to work doesn’t. But also difficult to go back to the dose that was helping because that might be too much once your body has re-set.
Good God don’t increase your benzo usage. I’m 99% sure benzo tolerance withdrawal (aka toxicicity) was the massive chemical trigger that began my nightmare down the road of mecfs.
I agree Tracey Ann, mental and emotional exertion takes its toll just the same as physical. When my son was ill, school was worse for him than a short play at football..something his teachers never believed.
And yes, doing too much leads me to being wired and so can’t fall asleep. Diazepam used to work well for me but they stopped working so now I take a sleeping pill (no more than 3 a week). I have 2 I can use so when 1 starts to lose effect I change to the other. This has worked for several years now.I’m not happy about it but it’s that or stay awake all night!
I’m so sorry your son’s teachers didn’t believe him Lynne. Heartbreaking. My brain stops working properly, faster than other parts of me.
And I think sleep is so important and can be so elusive. I’m glad you’ve found a way that works for you. 🙂
In the last year I have found 2 treatments that have helped me greatly. Both I first heard about here on health rising, thank you so much for your endless research Cort. And Happy Birthday!
I have had great improvement with PEM by using Transcutaneous Vagus Nerve Stimulation (tVNS) using a programmable medfit tens machine as demonstrated by Dawn Whiley on AVA on Facebook https://www.facebook.com/groups/492041135346672/permalink/664134551470662/
It seems to do a lot of the things you said in this article as it calms down and balances the nervous system so it doesn’t use as much energy on “nervous energy” before and during activity and puts you in a calm state to be able to recover and repair quicker afterwards. It doesn’t help me with sleep though so I have to use it no later than 6pm. I’ve had M.E. for 38 years and this is one thing that has really helped me in all this time.
The other treatment that I started just under a year ago that has really helped me with PEM is high dose thiamine hydrochloride, making sure I take its cofactors magnesium and b complex as well. This has greatly improved my stamina from being housebound and feeling very ill every minute of every day. To being able to go out once a week and just generally feeling like me again and like I’m living again and not just existing. I think these two treatments are working well together for me.
With both these treatments and any treatments it is essential for PWME to start extremely low and very gradually build up over months.
Is thiamine hydrochloride called thiamine HCL?
Tracey, I see you. I have had a similar experience in the professional realm.
Also your descriptions are very similar to how I have talked about PEM (mental and physical instigated) with my husband.
Absolutely! I find that mental and physical exertion affect me as badly or worse than physical. My life is full of stressors I can’t control, and then being invalidated and not being believed only adds to it.
I find the really tricky thing about mental & emotional pacing is the inability to quantify. I can wear gadgets that help with pacing physical exertion, but that doesn’t help at all with all the energy expended by my brain. On top of trying to get some minimal work done, I’ve had almost daily prolonged panic attacks since a life-changing event a year ago, and that consumes a vast amount of energy my wearables can’t measure because as long as I’m physically at rest, my HR is unaffected.
It’s so difficult Wanda. I find that prolonged stress, that I have little control over, completely wipes me out. I’ve tried to streamline my life as much as possible but there’s so much we can’t control.
I hear you! I do the streamlining too but unfortunately it’s a drop in the bucket compared to the beyond-control stuff.
hi Cort, I have wondered what happened to the Light’s? I thought, can be wrong, they had a mouse model of ME/cfs? or at least where really really bussy with ME/cfs… did not hear anything from them for long time now… do you know?
That’s a great question. After all those interesting papers they just disappeared. The last published paper I see is from 2017.
Agreed. That was some of the most exciting research I’ve seen — and some of the best to show other physicians the difference between ME/CFS and other illnesses. The visual aids were striking.
Hello,
Can I ask why long chain fatty acids are contra indicated?
I have always felt that omega 3 supplements made me feel worse so very interested to know.
Thanks
Problems with long chain fatty acids have cropped up in a couple of studies in both FM and ME/CFS. The peroxisomes that process them may be affected as well as transport mechanisms into the mitochondria.
oh thats interesting..I take Omega 3 because it’s meant to help cognitive skills…maybe I shouldn’t…?
My daughter’s experience may well be an exception, but we have found regular lymphatic drainage to eliminate the poisoned feeling she used to get a day or two after exercise. We have found that increases in exertion (whether physical or mental) lead to increases in interstitial fluid and a corresponding need to manually drain the fluid into her lymph nodes.
My suspicion is that the excess fluid, if left too long, causes hypoxic conditions that generate at least one strand of the (potentially multi-pronged) phenomenon we label post-exertional malaise. Through manual drainage (we have evolved to use a technique very similar to dry brushing), and stimulation of the lymphatic system to increase lymphatic flow, we substantially reduce the potential for these hypoxic conditions to emerge. As I have written elsewhere (https://pubmed.ncbi.nlm.nih.gov/35073915/) I suspect this is related to vascular hyperpermeability, which seems to be at the core of many ME/CFS and LC symptoms.
In theory, the leakage of protein-rich fluid from permeable blood vessels could also irritate the glial cells. See generally https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9278212/
My daughter has hEDS and ME/CFS in a relapse / recovery paradigm. I hope to write more about the relapse/recovery cycle soon.
Do you do the lymphatic drainage yourself, or do you have a local practitioner? When I I’ve found someone who knew what they were doing to do lymphatic drainage, I found it helped, too, but I can’t find anyone right now. If you learned to do it yourself, do you have any resources to share?
Tamesin — I responded, though for some reason it’s not showing up right under your question.
Wearing a cooling vest during exercise really helped me reduce PEM after, I just wanted to mention!
I just do the maximum dosage of BCCAs immediately after any exertion thats enough to cause significant and lasting PEM ( not just a brief increase in specific symptoms ),
also I never do it for mental exhaustion / brain fog, only physical which could include many things. It consistently works, sometimes I also take NAC or vitamin C in certain specific situations where I feel a certain way.
BCCAs?
BCCAs?
Sorry, side note — why are long chain fatty acids bad for us? We should be avoiding fish? Missed that somewhere. (Really allergic to MCT, so that won’t be for me.)
Sorry — didn’t see that this question was already asked when I read through the comments. Darn brain fog.
I do it for my daughter daily. Sometimes, when she has been particularly active I might do it more often. When I am away she uses dry brushing, which I think is a great place to start for people doing it on their own. She also does drainage herself during the day when needed — particularly face and neck when she has had particular mental exertion. These videos can be a helpful intro. https://youtu.be/KjljIFpuEQU and https://youtu.be/1YnVb9Ie-r0 . Only additions I would make are importance of activating or massaging the lymph nodes before starting (otherwise they can get engorged). Also, worth doing back of neck and back as well. We also do scalp massage, then drain down the spine (straight down). A good PT can help you learn other techniques as well. Good luck!
Thanks for the links!
one thing has always worked well for me in post exersion recovery
ie
2 yrs ago i installed the underfloor insulation under my house
first day i took under a couple rolls ,got thru one roll and crashed the next 2 days in the dark on the sofa
then i upped my Nortryptillen by half a tablet a day while i was finishing off the rest of the house ie 25 mg to say 40mg each day
i could then manage to crawl around and do a couple rolls a day till all done with no crashing inbetween
every time i know ive overworked ie this year was total repaint of half the house inside pre new carpet
each day i remebered to take the extra half tab of Nortryp id be ok to continue the next day couple days i forgot and crashed for several days
Seretonin plays a huge role in the oxygen/energy pathways to every cell
something on same area possibly DROP all the crappy seed oils ie HIGH omega 6 which is a strong inflamation issue
ideal ratio is like 1-4 omega3 to omega 6 but most modern foods have the ratio like 1-25 1-50 plus
Hi!!!
I used to take 275mg Naproxen, 2x/day and 50mg Tramadol, sometimes.
At the last PEM, i took 7,5mg Mestinon and it was fantastic for me.
Some people can avoid PEM and crashes with licorice extract and adrenal supplements. Cortical extract drops have not really been available since the pandemic – the FDA might have cracked down on them because they help people, not sure – but if I do too much and feel a crash coming on, taking extra licorice extract drops can often definitely ward it off. That has reliably worked for me on a number of occasions.
Sometimes licorice can also facilitate recovery from crashes. Aside from effects on cortisol, licorice is also very strongly anti-viral, and that perhaps could be the mechanism behind its anti-fatigue properties. Either way, a crash that ordinarily might last a week or longer can often be truncated to a couple of days with enough licorice.
The one caveat is that it’s important to monitor blood pressure while on licorice longer-term.
Great idea.
Another thing to monitor if on licorice long term is potassium levels. (Easily remedied by taking potassium supps.)
Great call out! Licorice tanks my potassium.
I know this study looked at healthy people, but I still think it’s super interesting to consider.
With my severe PMEM (post-MENTAL exertion malaise), I’ve always wondered is my brain depleting something?? Am I over-producing something??
This study addresses this, specifically: “A lot of the existing work had gone into the assumption that fatigue occurs because you deplete a resource of some kind,” says Matthew Apps, a cognitive neuroscientist at the University of Birmingham in England, who was not involved in this work. “I think it’s really exciting that there might be a different model whereby the accumulation of materials in the brain may stop it from functioning properly—and that might actually be what leads to the consequences of fatigue on your behavior.”
This “different model” asserts mental fatigue might be from overproducing glutamate. There are lots of supplements that can help, at least in part, mitigate glutamate’s negative impacts. (Of course, we need some glutamate.)
https://www.scientificamerican.com/article/why-thinking-hard-wears-you-out/?utm_term=Autofeed&utm_medium=Social&utm_source=Facebook#Echobox=1660249402
That seems like a very interesting idea Syd. I’ll definitely have a look at that 🙂
Creatine monohydrate is a great PEM buster for me. I use it both before and after excertion. Electrolytes and magnesium are important as well. And breathwork to calm down this overactive/imbalanced autonomic nervous system. 🙂 The best PEM buster is of course to prevent it from happening!
hello Cort,
i’m a french guy and i don’t know if you have seen it but a french girl has interviewed dr Patterson about long covid and his treatment:
if interessed:
https://www.youtube.com/watch?v=XKNUc7_s30U&t=545s
There are definitely people who report an advantage from paracetamol.
I’ve heard people say that they can watch TV longer for instance.
I would suggest looking into its pharmacology and besides the ones pointed out, there seems to be a serotonin effect.
I know, because when you do a serotonin urine test, you are asked to leave that out 😉
Everyone be really careful and inform themselves well about the potential of Tylenol (in Germany, it is called Paracetamol) for liver damage. I don’t have the facts in mind, but remember that the dosage beyond which liver damage can happen is not astronomically high and can also vary in individuals (pls check info for yourself, but for example this Swiss case of acute liver failure https://medicalforum.ch/de/detail/doi/smf.2018.03257 took 2 mg one day and 8 mg the other, and in Germany, just one tablet contains already 500mg), earliest stage of liver damage may be overlooked as it need not necessarily produce symptoms, and here https://www.msdmanuals.com/de-de/heim/verletzungen-und-vergiftung/vergiftung/vergiftung-mit-paracetamol it says there can also be a cumulative toxic effect from many smaller doses over a certain time.
The clinical antidote in case of liver damage seems to be high doses of intravenous acetylcysteine which neutralises a toxic tylenol metabolite.
If you take it regularly, Cort, you could maybe now and then have Tylenol blood levels done as well as liver parameters to be on the safe side?
Sometimes what I call “Power sleeping” during the day helps: When totally “wired-up” or in a beginning crash, I sometimes try to regulate down the nervous system and heart rate with medication (like trimipramine) – yesterday it even worked without meds using a series of nervous system downregulation techniques (first, a quick nerve calming finger massage as per Suzie Baxters video from the channel recommended by Dr. Asad Khan (works also using fingernails for me instead of an accupressure ring) https://www.youtube.com/watch?v=UQN2a03bW_Y which made me yawn, then a tapping technique called Emotional freedom technique (EFT) which made me yawn more, then my go-to 20min-muscle relaxation exercise. I can’t remember but may have also added in some slow breathing or “circular” breathing i.e. “up the back, down the front”), then fell asleep from afternoon to 9:30 pm. (This is remarkable for me, as during the day I am never tired just deeply exhausted). It temporarily messes up sleep rhythm but I think it helps.
I also took 2 ibuprofen before this in the hope it might be anti-inflammatory, but that’s just my hope not tested method.
Cort, there are multiple studies that point toward ribose possibly causing dementia/memory loss. Would you mind adding a note about this in your article? I worry about how many ME patients take it without ever hearing about this. It makes a huge difference for me, but I stopped taking it because the risk seemed too plausible to me from what I read about it. Some people might find the trade-off worth it, but it worries me that so many patients take ribose without having all the information they need to make an informed choice.
I had a bad case of bronchitis earlier this summer and used dextromethorphan to ease the coughing. “Coincidentally” I was less fatigued, brain fog disappeared and I h ad no FM pain. After I recovered from the bronchitis and stopped using Dextromethorphan the CFS/FM symptoms returned. As I am taking mitochondrial support supplements, I decided to search for anything that would help brain inflammation. I tried Dextromethorphan (15 mg 2x daily) and am much more functional and have no more pain. I am also using Quercetin to help with allergies as opposed to a daily antihistamine. My thinking on that being that antihistamines block histamine receptions which are there for the normal function of histamine in the tissue. Quercetin blocks the release of histamine from the mast cell which is the dysfunctional part of allergy responses I am weaning myself off of antihistamines and using one dose of Quercetin. (400 mg) with Bromelain. It seems to be working pretty well. Additionally Quercetin is anti-inflammatory I did try Tylenol but did not have the same benefit as Dextromethorphan, though I may try it again at some point.
I do deep breathing with a long exhale, which helps with the “wired”, and also, for me, settles my gut.
Tylenol seems to do something for me. It doesn’t stop me from pem but if I take before bed it seems to make me recover a bit more from pem. I have fibromyalgia pem though. B4 this when I took it I did notice a slight association with better symptoms but thought it was a coincidence as I recovered from pem anyway
Please don’t recommend Wim Hof breathing! The exercises lower CO2 A LOT and thus impair oxygen absorption and thus energy production. People have fainted and even died from these exercises (well not the exercises directly, but they fainted and then drowned).
PS: awesome to see the ‘Notify me via e-mail if anyone answers my comment’!
Just like many other treatments many have been helped by it, some hindered. The drowning was by people who use the method in water, which was dumb and Wim Hof never recommended that.
when its successfully healing I get ripples of heat and sweat.
When the body cannot heal from the exertion I dont get any heat. What I get is no symptoms if I sit perfectly still doing no exertion. Then if I move my solar plexus area goes nuts. Straining feelings like its trying to sort something out by resorting to extrmee means in that area. No matter how many days I sit still the sitaution doesnt change.
If I ignore the raging solar plexus & get up the disability increases long term. MY body is trying to do something & if science could identify what I think it would be groundbreaking. The sensations are so intense that there must be a very clear indicator of biological activity in the body.
For me the 1st point of call would be to identify what the liver is doing. If there was a way to monitor what the liver is producing in reaction to activity to see if there is an abnormalty
A really good effort. The emphasis on muscles isnt right. Ive had severe ME 25 years and my body isnt trying to repair muscles. When I talk to people or read a book I get symptoms. Thinking and sensory adtivity cause post exertional malaise when the condition becomes severe. I cannot even listen to someone talking without getting payback. So its not muscle damage.
When I do activity first I get heat in my torso like a furnace. I get giddiness and irritability. Then I get sensations just below the base of the sternum around the solar plexus which feel like my body is straining to do something.. Sometimes it feels like starvation (even if Ive just eaten) sometimes like straining sometimes ice cold and sometimes like fear. When it feels like fear my mind is blank. Theres no conceptual fears so I think it is my body being in some sort of emergency mode. I get flusih symptoms starting at this point.
When Im coming out of this state the raging heat returns in my torso. (like massive hot flushes. When its healing I get a rippling sensation on my skin with sweating and heat. I wake up and find this happening whilst Im not fully awake. It stops when I wake up.
When my body is successfully healing I get ripples of heat and sweat.
When the body cannot heal from the exertion I dont get any heat. What I get is no symptoms if I sit perfectly still doing no exertion. Then if I move my ,solar plexus area goes nuts. Straining feelings like its trying to sort something out by resorting to extreme means in that area. No matter how many days I sit still the situation doesnt change.
If I ignore the raging solar plexus & do small activities, the disability increases long term. My body is trying to do something & if science could identify what I think it would be groundbreaking. The sensations are so intense that there must be a very clear indicator of biological activity in the body.
For me the 1st point of call would be to identify what the liver is doing. If there was a way to monitor what the liver is producing in reaction to activity to see if there is an abnormalty
I really wish this blog had prioritized what works the best and what doesn’t (and divided pharmacueticals into a separate list). This blog post seems maybe promising but overwhelming. Who could possibly do all of these things??
The problem is we don’t know what works best. None of these have been studied unfortunately. Hopefully we’ll have more and better information over time as long COVID gets more study. Thanks for the idea to divide the drugs into a separate category. It’s kind of meant to be a chose one and give it a try.
After reading this a few times, I have to thank you very much. I am brand new to these potential solutions to long covid. So this is very overwhelming. But I see now that you are just telling us what the research has shown and then what’s helped some people. I guess that’s the best we can do right now.
Unfortunately, for me, many supplements are causing insomnia, just like exercise does.
I’m a distance runner. I’ve been a distance runner for almost 25 years. I was extremely fit for my age when I contracted covid. I was also vaccinated. I have never tested positive but the symptoms have been undeniable and profound, for me anyway.
I seriously think I’ve contracted covid at least 6 times. Mild symptoms every time, during the initial infection, like headache, chills, sore throat, stuffy nose, etc. But I also get this vibrating feeling at night and insomnia. I’ve learned that I definitely can’t run through that initial infection (which is what I tried the first time).
Anyway, I’ve developed serious reflux / gastro issues that they tell me were caused by nerve damage. The antacids that I must take basically destroy your immune system. So every time I go anywhere and anyone is sick, I get sick again. And I’m very very careful. But still. If I totally isolate, after fully recovering, I’m fine until I go around any sick people again.
But every time I catch what I think is covid, I develop *serious* exercise intolerance. Like I can still run, but then afterward my symptoms come raging back. And the worst is then I can’t sleep. At all.
Every time I have covid, I go through this for weeks. *Thankfully* every time — I guess through self-imposed body awareness and just an absolute refusal to stop exercising — within a few weeks I am able to walk a little, maybe lift weights a little, then slowly walk faster, then eventually get back to normal running. I would say that entire process takes me about a (very scary and frustrating) month.
The reflux has never gone away and I’m trying extensive treatments for that.
Most recently, I got sick at the hairdressers. That was 2.5 weeks ago. Right now, I can’t even tolerate a mild to medium pace (extremely easy) 40 min walk. That caused me to crash yesterday and not sleep at all last night (*but see below).
(Usually if I crash — I’m fine again the next day — as long as I don’t repeat the exercise.(
I feel fine with other daily activities though I seem not working much, while trying to fully recover. I do stuff around the house and feel fine.
Right now, after yesterday’s crash, I’m walking at a 1.0 pace on my treadmill, for 30 min. I’ve been able to tolerate that. Really that’s just for digestion. I guess it’s some “exercise” but no different than walking around my house. Very very slow. Heart rate 73.
If this doesn’t cause a reaction (and it hasn’t been), maybe tomorrow I’ll slightly increase the pace and go from there. I might also try a few sets of light weight training.
One thing that helped last night — from comments on this blog that I was reading into the night — at 2:30 am, I took 2 NAC. That put me to sleep fairly quickly.
I woke up again at 6. Took another NAC at 7. Slept until 9:30. Problem was the second NAC caused reflux — probably bc it’s a supplement on an empty stomach at that point — and my nighttime antacids had worn off by that time. So I took my morning dose. That helped but didn’t completely stop the acid
So that was a good find but not something I want to keep needing to do. I’m trying to stop all acid 100% to let that valve heal.
My friend today suggested sublingual glutathione, which I just ordered. Maybe that will help the acid problem.
I can’t tolerate many supplements. This has been a new thing since contracting covid. NAC is usually fine. So I’m going to slowly try other suggestions.
I’m not willing to take pharma drugs. Things never go well for me when I do. They just cause other problems, for me.
Anyway thank you very much for this great resource! I plan to continue following and hopeful to hear good news going forward.
Good luck, Tina – our hearts are with you! Sorry to hear about the acid reflux. Nasty stuff! Darn. Have you tried gabapentin – I just read a blog where gabapentin was used to recover autonomic nervous system functioning and help with acid reflux. Continue to be very careful with the exercise. It’s very hard for athletic people to adjust to that. You might want to check out Michael Gallagher’s story – he was an ultramarathoner who came down with ME/CFS.
https://www.healthrising.org/blog/2022/06/28/getting-run-down-by-me-cfs-a-memoir-summer-reading-i/
Oh I forgot to mention. I eat a 100% plant based diet, and that’s 80% whole foods. The only processed food is soy milk (edensoy), pure raw almond butter, tofu, ezekial sprouted bread, and a new item is pumfu (100% pumpkin seed mashed basically).
Plant based diets are anti inflammatory.
I believe that has helped me recover and get back to exercise.
However this latest time — I’m getting scared. Recovery seems to be taking longer though I’ve never actually kept records (until now, so that I’ll know for sure if this happens again).
I’ve also resigned myself to the fact that I’ll need to wear an N95 mask to ANY indoor events.
Anyway at the moment I’m just praying that I’ll recover again and get back to running. I cannot imagine a life without running. And I’m not totally sure that’s going to happen this time (meaning recover enough to be able to run again).
NAD+ IV infusions stopped 2 months of rolling PEM (aka pure hell.)
When speaking of Benadryl it is important to specify the active ingredient. It is a generic brand name for many tings and in different countries and at different times the active ingredient may be different
I have always felt (for 40 years now) that there was something wrong with the process of the body turning what we eat into fuel- or the cells somehow not utilizing the fuel properly. It was like a rechargeable battery where a night’s sleep would only recharge to about 1/4-1/2 or so, and then the body would be out of ‘juice’ early in the afternoon- and woudl need sleep to recharge for the rest of the night till bedtime- only problem is that sleeping is unrefreshing- I would always suffer 2 days after doing anything like exercise- i woudl just crash hard- and feel weak, dizzy, nauseous, brain fog woudl worsen, muscles weakness big time- somethings it was so bad, if i really over did things, that i wasn’t sure that i woudl be alright after collapsing in bed and feeling really out of it-
anyway- back to the fuel issue- something isn’t right- muscles do not recover like they should- and crashing really takes a toll- and it’s always 2 days after hard work- i woudl be fine the next day after work, but then the following day, i woudl wake up feeling like a truck had run over me-
I read that PEM might possibly prevent ATP from working properly- that the body’s cells die off and can’t be replaced properly for several days like happens with normally healthy people-
supposedly high dose B-1 or Benfotiamine are a help to PEM- I haven’t noticed any change on it yet though- been taking about 1 week- there are a number of clinical trials and reports on it-