

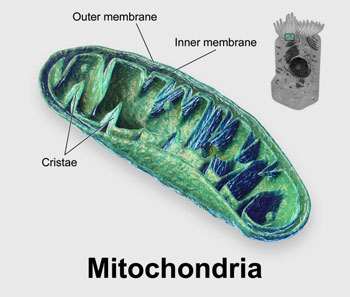
Something appears to be going on with the mitochondria but exactly what is unclear. (from Blausen 2014 Medical Gallery – Wikimedia Commons).
The mitochondria are a big mystery in ME/CFS and fibromyalgia. Plenty of evidence – most of it from small studies, admittedly – suggests the mitochondria are involved. Nailing down exactly what’s gone wrong has not been easy given the variety of possibilities that have shown themselves.
Problems with fatty acid metabolism, shunts propelling oxygen-rich blood away from them, broken antioxidant systems, high levels of intracellular calcium, complex V dysregulation, HHV-6 reactivation/mitochondrial fragmentation, inborn errors of metabolism, and more have been raised. The list seems to go on and on.
In “Elevated ATG13 in serum of patients with ME/CFS stimulates oxidative stress response in microglial cells via activation of the receptor for advanced glycation end products (RAGE)”, the Simmaron Foundation research team just added a new possibility to that list – and a rather fundamental one at that.
Proteins That Clump Together…
First, the Simmaron team looked for evidence of increased protein aggregation, or clumping, in ME/CFS and found it.
We know protein clumping best from the amyloid-b and alpha-syn proteins that clump together in Alzheimer’s. Since protein clumps can interfere with all sorts of cellular activities, the high rates of protein aggregation, or clumping, found in the ME/CFS patients (particularly the females) were interesting, to say the least.
They’re not the only ones to find proteins clumped together in ME/CFS. Nunes recently found amyloid fibrin(ogen) or fibrinaloid microclots in the blood of people ME/CFS, and Pretorius has found them in long COVID as well. (Blog coming up.)
Some indirect evidence of increased protein clumping has shown up as well. A 2005 ME/CFS cerebrospinal fluid proteome study, that highlighted the presence of amyloid proteins, suggested that misfolded proteins embedded in the blood vessels of ME/CFS patients’ brains were causing small leaks.
David Systrom also recently reported that he was working with a group focusing on whether another cleanup mechanism – the TNF-related apoptosis-inducing ligand (TRAIL) – had gone awry in ME/CFS. TRAIL is known for attacking amyloid-ridden nerve and cancer cells. Systrom wonders whether it may also be killing off the small nerve fibers in ME/CFS, FM, and other diseases.
The Gist
- Finding increased levels of aggregated proteins in ME/CFS patients’ serum, the Simmaron researchers assessed whether their cells were having trouble breaking them down via a process called autophagy.
- Autophagy clears unused proteins and old and damaged mitochondria from the cells and is especially important during exercise. When autophagy breaks down, it can impair oxygen consumption and mitochondrial activity, affect immune functioning, turn cells into pro-inflammatory generators, and lead to clumps of proteins that can damage all sorts of processes.
- A variety of tests found high levels of several autophagic factors – most particularly a protein called ATG13. High levels of ATG13 outside in the serum indicate that ATG13 has undergone phosphorylation and has aborted the autophagy process.
- Applying serum from ME/CFS patients and healthy controls to the microglial cells caused the cells given the ME/CFS serum to begin spewing out pro-inflammatory substances.
- Rapamycin and metformin are two drugs that may be able to restore autophagy. Health Rising recently reported on a doctor who recovered from a long-term case of ME/CFS using rapamycin, and metformin has been found to be helpful in chronic pain conditions and has been suggested in fibromyalgia.
Broken Cleanup Process
Next, they looked at why these protein clumps might be forming. ME/CFS patients were either forming more protein clumps than usual, or the protein degradation process in the cell (autophagy) that is supposed to cleanly and efficiently dispose of old proteins and mitochondria was not working well.
A larger sample of 24 patients and healthy controls found that ATG13 – an early marker of autophagy – was elevated in ME/CFS patients’ serum.
That was not a good sign. Finding high levels of ATG13 in the serum indicated that it had been phosphorylated and that the autophagy or cleanup process in the cell had been aborted – resulting in ATG13 being moved outside the cell into the serum.
Next came a big question. Besides the mitochondrial problems it might be causing, could the high levels of ATG13 also be sparking microglial activity and producing neuroinflammation? The Simmaron researchers took a page from what’s becoming a pretty common playbook in ME/CFS and applied serum from some ME/CFS patients and healthy controls to cultured microglial cells.
Lo and behold, the serum from the ME/CFS patients turned on the microglial cells causing them to spew out free radicals and to produce iNOS (nitric oxide) – an inflammatory and neurodegenerative form of nitric oxide – while the serum from the healthy controls did not.
Next, they used an antibody to neutralize the ATG13 in the serum and tested it again. When the ATG13-free serum failed to turn on the microglia to the same extent, they concluded that ATG13 was the culprit.
With that link tied down, they did an in silico (e.g. computer simulation) analysis which suggested that ATG13 was turning on the microglial cells via a receptor called “RAGE”.
Autophagy, Chronic Fatigue Syndrome (ME/CFS), and Fibromyalgia (FM)
Autophagy hasn’t shown up much in ME/CFS. The first time I came across the term autophagy was following an exercise test for a study done at Dr. Klimas’s Nova Southeastern Clinic when the researcher suggested that problems with autophagy may be present.
The interesting thing about the autophagy finding is how fundamental it may be. Autophagy is the process by which cells cleanse themselves of inactive proteins and defective mitochondria.
If the general findings regarding the mitochondria are correct, it makes sense that a lot of damaged and poorly functioning mitochondria may be present in ME/CFS and in need of cleanup. Having an impaired autophagy process is probably somewhat akin to never changing the oil in our car: the valves in our mitochondrial engines become clogged with junk, and our engines sputter.
Problems with autophagy can result in two things that appear to be happening in ME/CFS: lower oxygen consumption and higher rates of free radical production. Poorly functioning mitochondria do more than slow a cell and its functions down, though. If the mitochondria stay dysfunctional long enough, the cells they are embedded in can become senescent, start deteriorating and begin secreting pro-inflammatory cytokines.
Plus, autophagy also becomes quite pronounced in two situations that may be of special interest in ME/CFS: starvation and exercise. “Starvation” could come into play in ME/CFS not because people with ME/CFS are not eating enough but because their cells may be being starved of nutrients. Autophagy is induced by the muscle contractions that occur during exercise and is necessary for maintaining muscle activity. Mice deficient in stress-induced autophagy mice exhibit less endurance during exercise.
Rapamycin Connection?
Health Rising recently presented the story of a physician who has recovered from ME/CFS using rapamycin – a longevity drug and MTOR inhibitor. That was an interesting report given that MTOR activation aborts the autophagy process. The fact that an MTOR inhibitor significantly helped at least one long-term ME/CFS patient suggests that an impaired autophagy process may be present in some people with ME/CFS.
Gunnar Gottschalk noted that they’d love to test the effects of rapamycin in their ME/CFS animal models. In fact, they created a way to neutralize ATG13 in order to do just that.
How about Metformin?
Autophagy has cropped up a couple of times in connection with FM, though. A 2010 study linked mitochondrial problems with increased autophagy and several animal studies suggested an elevated autophagy response may be present in FM.
Metformin – a drug that inhibits MTORC1 via activation of AMP-activated protein kinase (AMPK), thus increasing autophagy, has been shown to reduce chronic pain in several studies. Researchers were able to resurrect AMPK production and mitochondrial production (and presumably autophagy) in FM patients’ connective tissue cells (fibroblasts) through the use of metformin.
If autophagy becomes a “thing” in ME/CFS and long COVID, it wouldn’t be unique in the disease world. Autophagy is a problem in many other diseases including Alzheimer’s and Parkinson’s disease.
Conclusion

Are impaired mitochondrial cleanup processes causing problems in ME/CFS?
Finding increased levels of aggregated proteins in ME/CFS patients’ serum, the Simmaron researchers assessed whether their cells were having trouble breaking them down via a process called autophagy.
Autophagy clears unused proteins and old and damaged mitochondria from the cells and is especially important during exercise. When autophagy breaks down it can impair oxygen consumption and mitochondrial activity, affect immune functioning, turn cells into pro-inflammatory generators, and lead to clumps of proteins that can damage all sorts of processes.
A variety of tests found high levels of several autophagic factors – most particularly a protein called ATG13. High levels of ATG13 outside in the serum indicate that ATG13 has undergone phosphorylation and has aborted the autophagy process.
Applying serum from ME/CFS patients and healthy controls to the microglial cells caused the cells given the ME/CFS serum to begin spewing out pro-inflammatory substances.
Rapamycin and metformin are two drugs that may be able to restore autophagy. Health Rising recently reported on a doctor who recovered from a long-term case of ME/CFS using rapamycin, and metformin has been found to be helpful in chronic pain conditions and has been suggested in fibromyalgia.
Update!’
Check out a rapamycin recovery story
And Simmaron’s ME/CFS rapamycin clinical trial






Has anyone else tried Rapamycin
So do you think this issue with autophagy would be in favour of or against ME patients using ketosis and intermittent fasting to trigger autophagy? I wonder if it would make the autophagy issue worse or provide a reset for a broken biological feature…
I do significantly better on keto with intermittent fasting.
MayB, thanks for replying. I also feel better eating keto. Do you have any tips for successful fasting? I struggle with that!
This is really interesting. I have been reading a lot about slowing and reversing ageing and decreasing protein accumulation/clumping and senescent cells by autophagy is one important factor in that. So nice to see there is a connection.
I am taking fisetin now, it is apparently the most effective:
https://novoslabs.com/frequently-asked-questions/other-supplements/why-do-you-use-fisetin-is-fisetin-better-than-quercetin/
Very interesting….I too am wondering if autophagy would be good or bad. It’s encouraging though to see that some studies are focusing on similar areas.
Very interesting. Remember the Goebel landmark study in fibromyalgia ((https://www.jci.org/articles/view/144201))? Some factor X in the serum of FM-patients apparently activates the glia in the dorsal root ganglia. In their paper they write that they have not been able to identify this factor. Maybe it is ATG13?
Maybe a good idea to check this out.
Oh my – wouldn’t that be something. That Goebel study was so fascinating. What a linkup that would be. I particularly liked this possibility:
“The authors believe that a new kind of autoimmunity – one which does not produce inflammation – is present in fibromyalgia. Instead, the autoimmune processes directly target pain-producing nerves.”
It just makes so much sense. Talk about killing several birds with one stone….
https://www.healthrising.org/blog/2021/07/02/blood-cause-fibromyalgia-autoantibodies/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5723685/
Natural mimetics of rapamycin and metformin. Theory article
Didn’t they identify it as IgG?
“Mice treated with IgG from FMS patients displayed increased sensitivity to noxious mechanical and cold stimulation, and nociceptive fibers in skin-nerve preparations from mice treated with FMS IgG displayed an increased responsiveness to cold and mechanical stimulation.”
Urolithin A has been shown to induce mitophagy. I had heard about it 2 years ago as it was researched at ETH Lausanne. It has recently been commercialized by https://www.timelinenutrition.com/science.
I had been considering Rampamycin but I found Urolitin convincing enough and easier to start with it 5 days ago. I ll be happy to share my experience. Wish me luck !
Good luck! I heard of someone who appears to have done well with it 🙂
Janos
The use of Urolithin A is an exciting and promising approach! Rapidly growing evidence suggests that metabolites of gut microbiota, like Urolithin A and others (called now postbiotics) regulate mitochondrial quality control and functions. Furthermore, microbiota-mitochondria disorders play a crucial role in common neuropsychiatric diseases. (https://pubmed.ncbi.nlm.nih.gov/35978068/)
@Massimo How does the urolithin A feel? Do you have M.E?
Yes, I have ME but too early to tell. I started one months ago. Company says you notice after 3-4 months.
Wow. Stunning. I wonder if lowered activity of Uncoupling Protein 2 (UCP2) is behind the reduction in autophagy and AMPK production.
https://atm.amegroups.com/article/view/59732/html
I’ve seen at least one piece of literature to this effect:
Compared with the wild-type mice, the UCP2 knockout mice exhibited more severe cardiomyocyte injury after CLP, and the AMPK agonist AICAR protected against such injury. Consistent with this result, silencing UCP2 augmented the LPS-induced pathological damage and mitochondrial injury in the H9C2 cells, limited the upregulation of autophagy proteins and reduced AMPK phosphorylation. AICAR protected the cells from morphological changes and mitochondrial membrane potential loss and promoted autophagy. The silencing and overexpression of UCP2 led to correlated changes in the AMPK upstream kinases pLKB1 and CAMKK2.
Besides scenescence, something else also happens when cellular DNA is damaged – it signals latent virus particles within the cell to wake up, ramp up production, burst the cell and spread, looking for cells that are not damaged:
https://phys.org/news/2022-09-microbes-hosts-unknowingly.html
Please take a look at glutathione levels and find the most bioavailable form of glutathione…
Very interesting. Could ATG13 be the factor X lurking in the serum of persons with ME?
Am I right in thinking suppliments like PQQ could be harmful or protective dependjng on the lifespan or stage of lifespan of your mitochondria. having more mitochondria sounds like a great thing but they all must die eventually, is high or low “mitochondrial turnover ” something anyone has aimed for?
Would an impaired autophagy process result in lower than normal levels of protein in the blood? My Comprehensive Metabolic Panel (CMP) always shows a lower-than-normal Total Protein level.
I don’t know but reduced protein synthesis after exercise was a pretty big finding in Hanson’s studies.
That’s an interesting puzzle I want to unravel. The studies indicate that AMPK activity is significantly lowered in ME/CFS. AMPK inhibits protein synthesis yet protein synthesis is diminished. I think there may be some other activity that AMPK does that indirectly and ultimately leads to protein synthesis as opposed to its immediate inhibition of protein synthesis by inhibiting mTORC1.
Brain fog pretty bad right now. Some follow-on thoughts from my previous comment. Is this impaired autophagy process somehow implicated in the ability of the herpes family viruses to hang around in the cells forever and reactivate whenever they feel like it? And what are the implications for the use of mRNA technology for vaccines? After every one of my covid vaccines, I experienced reactivated herpes and/or shingles, plus weeks of fatigue. Maybe normal people are able to clean the vaccine particles out of their cells, while those of us with CFS are not so easily able to do that?
This seems to tie in with the work done by Booth et al, which found blocked translocator proteins in the mitochondrial membranes of a large fraction of patients with ME/CFS. They showed that transfer of ADP and ATP in and out of the mitochondria of neutrophils is impeded.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3403556/
I’m so curious to know if all ME/CFS patients had elevated ATG13 or what %. That could help me decide whether this is something I want to do something with. But the full research is not public.
Funny I had just asked if anyone knew what percentage of patients have the elevated levels! I have been on rapamycin now several weeks and I do believe it is helping me. I have been able to walk outside my house four minutes the past several days and yesterday I got almost 1,400 steps which I haven’t done much of anything, mostly bedbound since February 10th!
Does anyone know the percentage of m.e. patients that are believed to have higher levels of ATG13? I have been on rapamycin for several weeks now and I do believe that I am experiencing benefits. I have been able to walk 4 minutes straight outside my house and yesterday I did just under 1400 steps which I haven’t done since February 10th.