

People with chronic fatigue syndrome (ME/CFS) have often said that they feel like they’ve run a marathon despite the fact that they haven’t done any exercise at all. That idea has never been put to the test in ME/CFS but it recently came close in long COVID.

The study compared circulation in long COVID at rest to runners after they’d exercised to exhaustion.
A recent Polish study “Chronic Fatigue Associated with Post-COVID Syndrome versus Transient Fatigue Caused by High-Intensity Exercise: Are They Comparable in Terms of Vascular Effects?” demonstrates two things: long COVID’s wide reach (it’s reached Poland) and the creative studies that it’s triggering.
The study used a technique called “flow-mediated skin fluorescence (FMSF) which the authors stated was “uniquely suitable” for assessing the microcirculation during periods of low blood flow (transient ischemia). A recent hypothesis proposed that people with long COVID or ME/CFS were in a chronic state of transient ischemia due to inadequate blood flows.
Since the vascular system is put under great stress by exhausting exercise the authors did a rather daring experiment: they used an exercise stressor to determine if the microcirculatory systems of long COVID patients at rest were similar to those in seen in amateur athletes after they’d exercised to exhaustion.
It turns out that high-intensity exercise causes a great deal of stress to the circulatory system. For one, the massive amounts of energy produced come with an equally massive increase in oxidative stress (free radical production). Besides possibly whacking the mitochondria, that oxidative stress can decrease the bioavailability of the main vasodilator of the blood vessels – nitric oxide. The narrowed blood vessels that result would then reduce blood flows.
The non-invasive technique used measures blood flows in the skin. Since the epidermis or top layer of the skin, doesn’t contain any blood vessels oxygen and nutrients are transported to it via diffusion from the blood vessels. Due to this unusual arrangement, the authors reported that assessments of epidermal cell metabolism are “considered a unique and sensitive marker” of early vascular dysfunction and metabolic problems. The approach they used also enabled them to assess the macro (larger blood vessels)
The twist in this study came when the researchers compared the microcirculation of people with long COVID and the healthy controls at baseline to the runners before and immediately after an intense exercise session The runners who participated in this study were supremely healthy having participated in long-distance running, cross-country running, and marathons.
This study, then, compared the microcirculation of people with long COVID at baseline to the microcirculation of runners who’d just been pushed to exhaustion. If the long COVID patients’ microcirculation looked like it had been pushed to the limit without exercise, that would validate the experiences of people with long COVID.
Two parameters were assessed: the NOI (Normoxia Oscillatory Index) and RHR (Reactive Hyperemia Response). The NOI parameter characterizes microcirculatory “oscillations” (a function of activity??) and is particularly sensitive to the effects of high-intensity exercise. The RHR parameter assesses blood vessel function as it relates to the production of nitric oxide (NO) – the main blood vessel vasodilator – in the larger blood vessels.
The authors didn’t employ people with ME/CFS in the study but highlighted the “broad overlap” between the two diseases and referring to Wirth and Scheibenbogen’s ME/CFS hypothesis proposed that both feature problems with calcium dysregulation that in turn affects the adrenergic and muscarinic receptors that regulate blood flows.
Results
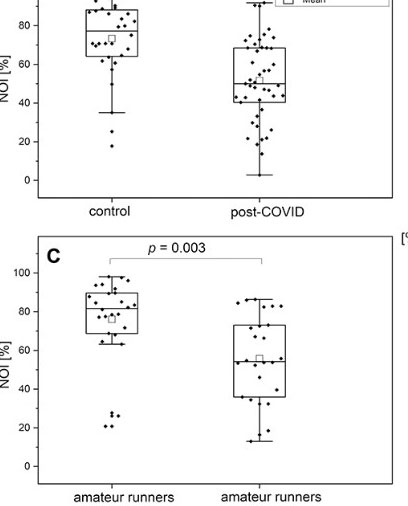
Note the high levels of NO in both the healthy controls and runners before exercise on the left side, and then compare that to the low NO levels in the long COVID patients at baseline and in the runners after exhaustive exercise on the right side.
Both the small and larger blood vessels in long COVID patients – at baseline – looked like they’d just exercised to exhaustion. The long COVID and exhausted runners had near identical microcirculation (NOI) and macrocirculation (RHR) test results. In other words, if you feel like you’ve just run a marathon they may have found a reason for it.
The authors proposed that problems with calcium homeostasis are producing endothelial or blood vessel dysfunction. An interesting study suggests that the opposite may be true as well; that blood vessel problems could be causing mitochondrial issues. The Sept, 2022 study “Flow pattern-dependent mitochondrial dynamics regulates the metabolic profile and inflammatory state of endothelial cells” found that disturbed blood flows increased a bunch of negative factors including mitochondrial free radicals production (mtROS), increased glycolysis (reducing ATP production), endothelial cell activation (inflammation), mitochondrial fragmentation and a hypoxia (low oxygen) factor ( hypoxia-inducible factor 1).
There were some provisos to this study. While the groups appeared to be age-matched they were not gender-matched. The long COVID group was 58% female, the healthy controls were 45% female, and the runners’ group was all male. Given what we’ve learned about gender differences that could make a difference and that needs to be cleared up.
The Gist
- Polish researchers assessed both the micro and macro circulation in healthy controls, runners, and people with long COVID using something called “flow-mediated skin fluorescence (FMSF).
- The twist was that they compared the circulation in people with long COVID and the healthy controls at baseline to the circulation in the runners after they’d exercised to exhaustion.
- Exercising to exhaustion puts the circulatory system under high levels of stress. The increased levels of free radicals produced during energy production can make it difficult for nitric oxide to vasodilate the blood vessels – leaving them narrowed and impairing blood flows.
- The results bore out the old canard in ME/CFS- that having these diseases feels like one has just run a marathon. The exhausted runners and long COVID patients’ at baseline produced near identical readings suggesting that both the macro and microcirculation have been dramatically affected in long COVID.
- The main proviso to this study concerned the all-male makeup of the runners and the 60% female makeup of the long COVID group. Since gender effects can be large, that issue must be dealt with in future studies.
- This study adds another data point to the growing evidence of blood vessel dysfunction in long COVID. The RECOVER Initiative is assessing coagulation factors in its initial assessments. It would be shocking if blood vessel issues weren’t a major emphasis as well.
Conclusion
People with long COVID (or ME/CFS) may feel like they’ve have run a marathon because their blood vessels – both larger and smaller – may actually look like they’ve run a marathon. Rather remarkably, two measures of circulatory blood flows – both micro and macro – were nearly identical in long COVID patients at baseline and in runners after they’d run to exhaustion.
The authors proposed that problems with calcium metabolism aka Wirth and Scheibenbogen’s hypothesis are ultimately causing the blood vessel problems. A recent study, however, suggested that disturbed blood flows may, in turn, be causing mitochondrial problems by reducing ATP production and increasing oxidative stress. Etc.
This study was by no means definitive and seemed rather simple in that it assessed two aspects of a very complex system but it provides another data point suggesting that blood vessel problems play a major role in long COVID (and probably ME/CFS). Overall, while some controversy exists, the blood vessel findings seem to be adding up. The blood vessel research topic was present in ME/CFS but long COVID has really brought it to the fore.
A number of hypotheses have been put forward to try and explain them: damaged adrenergic/muscarinic receptors, shunts that bypass them, micro blood clots, damaged endothelial cells, broken ACE-2 receptors, deformed red blood cells, and probably others
What we really need are big, well-managed studies that can come to a conclusion regarding the blood vessel, and blood clotting issues in long COVID and ME/CFS. That’s where the RECOVER Initiative should theoretically shine at least with long COVID patients. Coagulation factors are part of the standard assessments being done. I’d be shocked if a major effort at understanding the role the blood vessels play in long COVID wasn’t underway.






I’ve had fibromyalgia since 2008. I need to be in one of these trials. It’s an awful way to live.
Hi Sue, Stay tuned for a study that features a fascinating long COVID/fibromyalgia link.
Everytime I feel like giving up, you come along and give me hope. Thanks for the updates on ME/CFS and long covid. Maybe someday we will have some medication that keeps us in remission so that we can live a life that doesn’t include lying in bed most of the day because you have no energy to do anything productive.
Gina,
Cort was sent here to do precisely that!
OK! The primary function of erythrocytes is to deliver oxygen. If ME/CFS was caused by a lack of oxygen delivered to the electron transport chain, HPOT should solve that problem. Dr. Scott Shurr claims that at a pressure of 3 atmospheres, he can deliver as much oxygen in blood serum absent erythrocytes. Throw in even poorly formed erythrocytes, blood serum, and 3 atmospheres of pressure, and we should see a major improvement in oxygen delivery. Which all should lead to less fatigue?? Yes, no, or confused?
Try it out and report back!
If it works, we can all move to an oxygen-filled dome 100 feet under the sea.
@just the facts – Actually, three atmospheres is only 60 feet of water. Dr. Gary Kaplan ( a great D.O. In McLean, Virginia) does incorporate HBOT treatment in his ME/CFS treatment protocol. He’s not a researcher. He is an expert on natural anti-inflammatory supplements/acupuncture/etc.. So, his many patients that do significantly improve have a hard time separating out what helped them the most. Kaplan does not seem to really care at this point, because he is all about “healing”. In the Washington DC area, Gary Kaplan and Andrew Heymen get a great deal of push back from the “NIH do nothings”, and their many DC area disciples.. But, they both have so many happy clients, that the folks who want big Pharma to solve this problem, can’t silence Kaplan and Heymen’s patients. (In full disclosure – I do see Dr. Andrew Heymen, along with my normal MD’s.) I will try HBOT and report back, but it often takes 18 months to see the effects. It is expensive. (Watch one of Joe Namath’s interviews about HBOT and his recovery from concussion inflammation!) Don’t mislead people. We do not need to live under the ocean. Read about the results Israeli physicians are seeing with HBOT!
Rich,
1) I’m suspicious of a treatment that takes 18 months to take effect.
2) I’ve read spotty reports from people who have tried HPOT. (But perhaps it wasn’t tried for long enough, or “deep” enough.)
Hydrogen therapy might be the solution. I’d try that in a second, if I could get a tank of the proper blend (and was assured that it wouldn’t explode).
In the meantime, I’ll set aside some money for my underwater condo – just in case.
I used to scuba dive, often to 100 -130 feet (30 – 40m).
It left me very fatigued and brain foggy, disproportionate to the exertion.
Of course, that was using compressed air, not oxygen. But the experiences often left me wondering why I felt so awful afterwards.
Just the facts. I am with you on all of that. I do know that many Gulf War vets are obtaining free HBOT treatments. They claim that it is helping. Many Israeli patients are also reporting great results.
Glad to hear Gina. An immersion in the research gives me hope, too, that a way out for all of us will be found.
This is actually how I describe what ME/CFS feels like (relative to my state of the illness – moderate). That is, how I used to feel after enduro mountain bike races before I got sick (somewhat equivalent to a marathon).
hi Cort, may i ask you something if it is possible and you want to do it? it is of topic. but for the verry severelly ill ones who hardly can read, have a 1 second memory, etc.
i know (but that is also everything becaue of the obove mentioned things) that there are going to be trials for ME/cfs or even have began, i do not know. make a short list wich ones began on how many people, double blind placebo controlled, etc. and witch ones will begin and when. take for excample nancy klimas, how many years i am waiting and waiting or bateman horne center was it ct38, also so long long waiting. I just ask. if it is possible. i would print it out and hang it on my bed, just to have hope. sorry for of topic!!!
Hi Konjin, I don’t have an easy printout but in January we did do an update on ME/CFS clinical trials underway – at those that are listed in the clinicaltrials.gov database. (Others are surely underway.)
https://www.healthrising.org/blog/2022/02/06/2022-fibromyalgia-chronic-fatigue-syndrome-clinical-trials/
Incredible to get some physical evidence supporting how it actually feels!
This fits with what my Garmin body battery shows – that however well (or not) I recharge overnight, energy is depleted far quicker than in healthy people – I always felt this was due to my body having to work a lot harder than is normal.
Thanks again Cort! I often get a bit emotional reading your research updates but this one in particular hit home
I often describe my ME/CFS as follows, “It feels like I have run a marathon while having the flu, then get hit by a Mack truck driven by a vampire….who then sucks out all my blood”!
I have also told my many Dr’s all these years that it feels like I have no blood coursing through my veins. (Probably due to the vampire).😁
Thanks, Cort for all you do! You are a lifeline for our community!
I’ve wondered about blood flows for decades. It just feels like the blood is not getting through…I’m so glad this area has so quickly gotten so much attention in long COVID.
Interesting to yet again see the adrenergic/muscarinic receptors come up, as they were also found in two Swedish studies in a subset of ME/CFS just a few years ago
The same autoantibodies were also found in 2020 in Long Covid patients by Dr. Wallukat from a German company called “Berlin Cures” (who were first to do research on the drug BC007)
Dr. Wallukat not only found the antibodies to the beta2 adrenergic and the muscarinic M2, he and his team also found antibodies to the angiotensin II AT1, the angiotensin 1-7 MAS and the nociceptin receptor
Dr Wallukat’s team were often able to detect 4 of these 5 autoantibodies in more than 90% of Long COVID patients
So in late 2020 I contacted the ‘Open Medicine Foundation’ (OMF) and other ME/CFS researchers. I mentioned the Swedish study that found autoantibodies to the adrenergic/muscarinic receptors in a subgroup of ME/CFS, and that it was possible the remaining ME/CFS subgroups had a combination of those 3 other autoantibodies found in Long Covid.
(I think the Swedish study was funded by the OMF)
I asked if they knew of any research that looked for the other 3 remaining autoantibodies, in ME/CFS? as this could cover the remaining subgroups of ME/CFS.
The OMF kindly replied saying that as far as they were aware further studies hadn’t been done on ME/CFS sadly due to lack of funding.
I spoke to Berlin Cures, and they wanted to look at ME/CFS but were restricted by lack of funding too.
That was 2 years ago and I still haven’t seen if any researchers have looked to see if other subgroups of ME/CFS have those 3 other autoantibodies that are in Long Covid patients. (We already know 2 exist in ME/CFS)
If the other subgroups of ME/CFS do have some of any combination of those autoantibodies this could be what is causing ME/CFS for the vast majority of patients. It could fill the void in some if not all of the other subgroups.
Thinking about just the adrenal system and muscarinic receptors and the other targets under autoimmune attack would explain a the cascade effect causing a vast array of ME/CFS symptoms. It also would explain subgroups. But no one to date (to my knowledge) has looked.
If these autoantibodies are found, then drug therapies could be quickly used.
It’s highly plausible given that Long Covid is so similar to ME/CFS, so should be a priority to find out. because if it’s true, then funding can be directed into drug therapies.
How hard is it to look?
What I find frustrating is seeing research at the bottom of the cliff, i.e. looking at the result of a cascade of problems that could very possibly have been set off by autoimmune attacks on crucial bodily function targets higher up.
Those are great points, Brendan.
I find 99% of these studies maddening because they find *something* but then don’t explore the next logical step, which they’re already set up to do, or don’t attempt to prove the thing that was inferred by the initial results, or don’t investigate possible interventions suggested by those results (in vivo, in vitro, or in silico)
All the promising work goes fallow – rarely duplicated for confirmation, rarely built upon for full understanding, rarely tested with intervention – as whatever momentum it generated dissipates into that void of bureaucracy that is institutional medical research.
A guerrilla-style lab, funded by Bezos or Musk or Gates, could unravel and cure CFS in a month.
Yes, Give us some Ph.D’s with the guerrilla -style drive of Bezo’s, Musk, or Gates. And, fund Lipken properly.
well, there is a new group that’s very much in that vein, and even partly funded by tech people, i think cort mentioned it recently too. plus with great scientists!
https://techcrunch.com/2022/09/07/new-uk-nonprofit-startup-battles-long-covid-with-the-backing-of-ethereum-co-creator-vitalik-buterin/
Right Rich – hopefully this group – which is dedicated to quick movement – will give us some of that.
https://www.healthrising.org/blog/2022/09/13/lighting-a-spark-major-new-long-covid-initiative-promises-rapid-movement/
Yes, indeed Tom – an exciting group, indeed.
https://www.healthrising.org/blog/2022/09/13/lighting-a-spark-major-new-long-covid-initiative-promises-rapid-movement/
Brendan Rob, this is a fantastic post. We need more guys like you banging on the door demanding answers. I think if we get a true MD/Ph.D at the head of the NIH (not a long in the tooth politician), we will get some answers to these types of questions. I live near NIH. For decades, no one EVER said anything negative about the director. Happily, many of his former residents are now openly discussing the constant verbal abuse they took from him as young physicians. Physicians chosen for a residency program at NIH, are at the top of their Med School class. He’s on his way out, and hopefully non-political, camera shy, researchers interested in “healing” take over. Let’s hope and pray!!!!!
It is taking awhile but I expect we’ll see more research on this. Next up – a blog on a fascinating antibody study in long COVID that has implications for fibromyalgia and ME/CFS.
brendan, you could pass this on to this patient-led group that has 5m available for grants. they prioritize research based on patient ideas priorities
https://t.co/0aS3Nq9gEX
Looks like I spoke too soon as just discovered this video presentation, on autoantibodies in Long Covid and ME/CFS
Even though I suspected autoantibodies, I never knew all people have these existing antibodies that target certain human receptors to turn on or off function. Meaning that a dysregulated immune system is dysregulating crucial bodily functions, like the adrenergic system (amongst others)
I thought the autoantibodies were caused through molecular mimicry. but this could mean it’s something else causing the dysregulation upstream.
Also interesting is these researchers found another subset of Long Covid ME/CFS who have a shorter onset delay of Post Exertional Malaise.
The link is to a short video presentation
Post COVID ME/CFS and the Role of GPCR Antibodies
https://www.youtube.com/watch?v=F7Gj0qKvy2A
“broken ACE-11 receptors,” should be ACE-II/ACE2, I suppose?
Right – not ACE 11 receptors – there aren’t that many of them (lol). Thanks. I really, really hope someone takes a close look at these in ME/CFS as well, of course, in long COVID.
Cort, Thank you so very much for pushing the researchers and then reporting so cogently upon what they have been finding. You are a gem. But clearly $ is an issue and the research occurs so far away from the west coast that I feel utterly helpless about ever being helped by any of it, despite the good news aspect of it. I wish we CFS people could finance several research centers across the U.S. that we could visit and be included in their research. When the job isn’t getting done, I believe one should take the matter into their own hands and jump on the task. The sad thing is that damnable eviscerating lack of energy!!!!!!!!!
No kidding. Long COVID is getting a lot of money but ME/CFS continues on as it is…We’ll benefit from the long COVID research but how long will it take given the small size of the ME/CFS field. If the NIH was including ME/CFS cohorts in its RECOVER Initiative I would feel a lot better.
Do you know if any ME/CFS charities are lobbying for this at all? Thanks for all of your brilliant articles Cort, they really help keep me going!
Another interesting one, thank you Cort.
What would be the treatment for these issues? And is there anything we can experiment with in the mean time? What 27 years and over half my life suffering from this, I would love something to have a positive effect at last.
Certainly the long COVID community is experimenting with a lot of anti-clotting, anti-inflammatory stuff that we’ve never tried. There is some of that in this blog below and I hope to cover the treatments more fully.
https://www.healthrising.org/blog/2022/09/09/ischemia-reperfusion-treatment-long-covid-chronic-fatigue-fibromyalgia/
How is this different or what is it’s advantages over Peripheral Arterial Tonometry (PAT) tests such as EndoPat & Vendys-II.
I wish I knew. 🙂
So what is causing the CONSTANT Fibro-fog? Microclots that have damaged blood flow to the brain? Malformed erythrocytes that can not flow to the end of capillaries? Damaged cell membrane transport of oxygen? Damaged mitochondria that are unable to demand and receive oxygen for the Kreb’s Cycle. I think a decent team of Pathologists with great tissue biopsy samples teamed with several Cytologists could figure this out in short order. But, again no funding. Now, they’ll be forced to fund this research due to long covid. The NIH is pathetic! Geez, Rand Paul, get rid of this guy with his 49 “Honorable Ph.D.’s”, and old hidden e mails from top Virologists.
Dr. Amy Proal thinks out of the box. She recovered from ME/CFS. Get her on board!!!
So for me the issue always goes back to what is the root cause. The capabilities of a virus are ENDLESS as evidenced over history.
Oui, après 18 ans d’ EM/SFC, je pense effectivement à des problèmes de flux sanguins et problème d’ oxygène. j’ai aussi la maladie de Raynaud. J’ai fait un test d’effort avec injection l’année dernière et on a trouvé une petite ischémie à l effort.
Mon ” auto-traitement” actuel est basé sur l’ouverture des capillaires avec les BAINS de SALMANOV, ainsi que le PADMA BASIC ( à très petites doses, car j’ai du mal avec les CA et les médicaments).
Je me laisse 1 an pour voir si il y aura une évolution avec ce traitement…
Encore une fois, merci Cort, tu es toujours là et tu ne baisses pas les bras, tu gardes ton optimisme, et pourtant il y a de quoi devenir dingue avec cette maladie. Tu es notre Braveheart !
Translation:
“Yes, after 18 years of ME/CFS, I am actually thinking about blood flow problems and oxygen problems. I also have Raynaud’s disease. I did a stress test with injection last year and we found a small ischemia during the effort.
My current “self-treatment” is based on opening the capillaries with SALMANOV BATHS, as well as PADMA BASIC (in very small doses, because I have trouble with CAs and medications).
I give myself 1 year to see if there will be an evolution with this treatment…
Again, thank you Cort, you are still here and you do not give up, you keep your optimism, and yet there is enough to go crazy with this disease. You are our Braveheart!”
.
.
“Bonne chance et merci!”
Good luck and thank you!
it is soooo true that even when i am doing nothing laying down ‘flat’– which is most of the time– exhaustion STILL feels like i have run a marathon
thank you Cort for all the marathons you ‘run’ in providing info to us all
Cort, have you seen this?
https://healmindbody.com/chronic-fatigue-syndrome-the-mindbody-perspective/
I have not heard of Immune System Activation of Coagulation or ISAC before. Do you know what these guys are doing? It looks fascinating – the hypoxia/ischemia issue and mindbody approach.