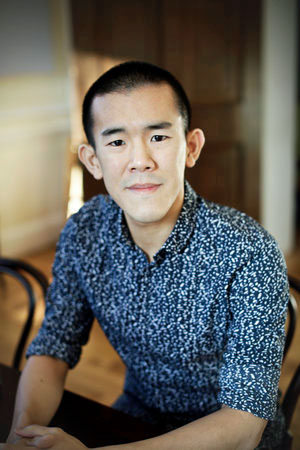
Ed Yong has been racking up the awards writing about the coronavirus pandemic.
Ed Yong, a science writer for the Atlantic, has a talent for getting to the heart of the matter. During the coronavirus pandemic, he’s often seemed a step or two ahead of his colleagues.
His trenchant reporting has landed him a bunch of awards: the Pulitzer Prize in explanatory journalism; the George Polk Award for science reporting; the Victor Cohn Prize for medical science reporting, the Neil and Susan Sheehan Award for investigative journalism; the John P. McGovern Award from the American Medical Writers’ Association; and the AAAS Kavli Science Journalism Award for in-depth reporting.
He’s also the author of two New York Times bestsellers—An Immense World, about the extraordinary sensory worlds of other animals; and I Contain Multitudes, about the partnerships between animals and microbes.
Back in July 2020, Yong was one of the first to report on long COVID and has consistently included ME/CFS in his reporting. In Sept. 2021 he reported that “One of the biggest misconceptions about long COVID is that it is entirely new… (and that) Long COVID shares traits with chronic illnesses including ME/CFS, fibromyalgia, mast cell activation syndrome (MCAS), and dysautonomia including postural tachycardia syndrome (POTS).”
Now he’s taken a big step forward with a major article on ME/CFS and long COVID, “Long COVID Has Forced a Reckoning for One of Medicine’s Most Neglected Diseases“, that highlights ME/CFS. (The ME/CFS article is the number two Atlantic article in popularity right now).
Yong writes that long COVID has “forced a reckoning” for ME/CFS in the medical world. Reckoning – which to my mind has almost biblical overtones – denotes a settling of accounts, a bill coming due. It often occurs when the two parties meet to hash things out but, in this case, the ME/CFS reckoning has been “forced” – basically rammed down an unwilling medical establishment’s throat – by long COVID.
Straight to the heart of the matter, Yong goes. For anyone who thinks long COVID is not largely ME/CFS, Yong reports, using citations, “Many cases of long COVID are effectively ME/CFS by another name.” If the ME/CFS medical community wasn’t already vastly outgunned, it seems like it’s on life support now. Noting that the ME/CFS Clinical Coalition’s website lists just 21 names, of whom at least three have retired, one is dead, and several others are aging, Yong writes:
“American ME/CFS patients may outnumber the population of 15 individual states, but ME/CFS specialists couldn’t fill a Major League Baseball roster.“
Yong then notes that, in some ways, things are actually temporarily getting worse not better. Faced with an onslaught of desperate long-COVID patients, Dr. Kaufman, for instance, is dropping some of his stable ME/CFS patients. With medical appointments getting shorter, it’s getting harder and harder for doctors to understand complex ME/CFS patients who often come backloaded with conditions (POTS, Ehlers Danlos syndrome, MCAS, etc.) that most doctors don’t know anything about.
Yes, progress has been made (Institute of Medicine Report, CDC drops GET, Mayo Clinic guidelines, increased physician awareness), but in the grand scheme of things, the situation is still “intolerable”.
Yong effectively laid out the state of ME/CFS but missed some opportunities as well. He got a subtle but important point wrong when he stated that the NIH committed $1.15 billion to study long COVID. It did no such thing. It would have helped readers understand the fix ME/CFS is in if Yong had informed them that NIH spent virtually nothing on long COVID until Congress gave it $1.15 billion and told it to spend it on long COVID.
Indeed, the NIH is still funding ME/CFS as if long COVID had never happened. Yes, long COVID has been a huge catalyst, but if the ME/CFS doctor community is small, the ME/CFS research community is just as small. Yong never asks how such a small research field is going to adequately test the numerous long-COVID findings that are sure to arise.
Yong’s report on RTHM – an exciting new long-COVID telehealth opportunity, being produced by Ryan Kellogg Ph.D., Jennifer Curtin MD, and Michael Snyder Ph.D., highlights the strange place the ME/CFS community finds itself in. Jennifer Curtin’s mother and brother had ME/CFS and she had it herself for 9 years, yet while RTHM promises to add ME/CFS, it will only see long-COVID patients now and does not yet allow people with ME/CFS to get on its waitlist.
The ME/CFS community is indeed in a strange place. Enormous amounts of resources are flowing to long COVID (yah!), yet the ME/CFS research budget remains stagnant (boo!). Congress gave the NIH $1.15 billion to research long COVID, but the NIH is not allowing any ME/CFS patients in its long-COVID studies. Long-COVID clinics are opening up everywhere, but Yong couldn’t point to one that was treating ME/CFS patients, and some people with ME/CFS are having a harder time seeing the few doctors they have. An exciting telehealth opportunity opens up – only for people with long COVID.
Ultimately, of course, the future bodes well for ME/CFS: virtually every study published seems to further solidify the connection between ME/CFS and long COVID, and RTHM is expected to open its doors to ME/CFS patients in December. Dr. Bateman hopes that in a couple of years 100 times more physicians will have the knowledge they need to provide support for people with ME/CFS.

The reckoning between ME/CFS and the medical community has not yet happened.
But is a “reckoning” for ME/CFS actually taking place? Yong’s article presses the case – the many ME/CFS patients, the few ME/CFS experts, the many ignorant doctors, the low research funding – that a reckoning needs to happen. It’s the first article I’ve seen to tie that to the long-COVID pandemic and is very welcome.
It’s clear, though, that reckoning regarding ME/CFS hasn’t happened – not yet. A reckoning requires that past due bills be acknowledged and made good – leaving all parties satisfied.
While ME/CFS should benefit immensely from the attention to long COVID, a true reckoning will require ME/CFS-specific actions are taken – ME/CFS being part of the medical curriculum, major outreach efforts be taken to inform doctors, major increases in ME/CFS research funding, and funding for clinical trials. These are logical outcomes one would think would flow naturally from a huge post-infectious disease pandemic, but none has happened – yet.
Hopefully, Yong’s excellent article will help spark the long overdue reckoning with the medical establishment the ME/CFS community has been waiting for.






Coincidentally, I had just logged in this morning to provide a link to the outstanding article in The Atlantic, only to find that Cort was, as usual, speedy-fast and efficient in getting to it first. Right after reading the article yesterday about the condition and the medical community’s ignorance about it, I met with an MD who claims to be a disease specialist but when I asked him if he’s heard about ME/CFS, and I told him what it stood for, his blank stare was followed up by an admission that he’d never heard of it. When I went on to explain PEM, this man, who appeared hundreds of pounds over a healthy weight, said, “Well, I have a theory about that. People who exercise a lot sweat too much.” I left the office $40-copay depleted, reminding myself that next time my copay will go to this website. Cort, for all you’ve done for us providing medical information, I hope you know that the validation you provide to readers is priceless. Thank you thank you thank you!!
LAC, I wholeheartedly agree! Thank God for you, Cort. Without the hope and education you impart with your reporting, I don’t know where I would be; not sure that I would be here.
Thanks LAC, Katjim and TAllen 🙂
I totally agree and I have a ME/CFS. PEM, MCAS, POTS, Fibro knowledgeable MD but I met with her today after she returned from a conference and she said there was no new news. We went over everything, lab tests, diet, etc (for over 2 hours) and basically I’m doing everything that can be done. I’ve learned more from Cort and made more progress from findings on this page than any DR. Big doses of Vit B1 &B2 put my ME/CFS in remission but then my MCAS got worse. It’s not all the Drs fault, the research hasn’t been done. Until it is we just keep being our own guinea pigs and hope one of us will come across a cure by accident. Thanks again Cort! Without you we’d all feel hopeless.
The Ed Yong article is excellent. I read it a few weeks ago. It’s encouraging that some places have figured out how parallel the symptoms are.
Cort, You are the BEST! Thank you so much for staying on top of things.
Thanks for your very thoughtful comments on Ed Yong’s article and the state of ME/CFS. I’ve read so many articles on Long Covid that don’t mention ME/CFS, and have therefore been very impressed by Yong’s writing. It just feels like those of us with ME/CFS can’t catch a break. My niece, who has all the symptoms of this illness, has been searching for quite a long time now, for a specialist who can diagnose her. She’s having difficulty finding anyone! A very sad state of affairs.
Dr. Lapp in Charlotte, nc who practiced with dr. Cheney.
I think Dr. Lapp retired a few years ago. BTW, I used to see Dr. Cheney.
I started by seeing Dr Lapp 7 or 8 years ago. He was great. He is retired, and a few years ago was only seeing a very few, previous patients. Tried to get the office to add me back as his patient, but no luck. After my first or second visit, I then saw Dr Black in that office. She was excellent! Not sure where she went, but left around the time Dr Cheney arrived. After my appointment with Dr Cheney I was surprised that he was working in that office. It was a sad day. I haven’t been back. BTW the office staff was amazing!
Health Rising has a program coming up that we hope will help find better doctors. 🙂
That would be extremely useful!
Thank you thank you thank you!!!
Cort, Thanks for providing us with Ed Yong’s publication. You are the best!
Soooooo…is there any good news? I’m so exhausted, sore and tired. Why won’t doctors realize we are barely able to breathe..move..let alone get out of bed?
Sad…but, life goes on.
Thank you, Cort, for your good feedback and for always staying right on top of everything!
It was really due to 3 or 4 people who alerted me to Ed’s article – thanks you guys! That actually happens quite a bit. 🙂
Thanks for reporting on this excellent article Cort. Curious why RHTM isn’t accepting ME/CFS patients on its waitlist? You’d think a woman who suffered with it, and has two children dx’d with it, would PRIORITIZE us!
Yes – I’m confident, though, that RTHM will indeed open up to people with ME/CFS – and probably be one of the first long COVID treatment groups to do that.
One can find that RTHM emerged from Y combinator. One can readily imagine that Long COVID seemed a better bet from a venture capital point of view. Ed’s article will hopefully reach these and other investors.
If you take a look at /r/medicine for Long Covid, Pots, MCAS, Fibromylgia, ME/CFS etc and look at the responses you’ll find that its not so much they aren’t aware of these conditions, its that they are convinced the entire lot are fake illnesses. The problem isn’t one of information, its that they have been trained these illnesses aren’t real and the people presenting with them are faking it. That is a far more problematic situation and its why there has been no turn around at the NIH nor in GPs diagnosing Long Covid alongside these other conditions.
Psychology papers still outnumber biological underpinnings by at least 3 to 1 that I can see, the bulk of papers remain about how amazing exercise and CBT is or how all chronic illness is FMD. That reckoning certainly hasn’t happened yet, things within research and medicine are carrying on as if Long Covid never happened too.
Yes, the journal “Brain” JUST came out with a study on POTS saying it’s psychogenic. Lots of rebuttals, like this one. But, it’s so disheartening and infuriating.
https://academic.oup.com/brain/advance-article-abstract/doi/10.1093/brain/awac348/6713530?login=false
Really amazing – at least that looks like a really good rebuttal.
Syd and Cort, just amazing! It is almost on par with the still being taught notion that Fibro and ME/CFS is just a sleep disorder primarily effecting woman, who have experienced a traumatic event. This is still being taught in some Med Schools. Dr. Maureen Hansen has a slide that she has inserted in many of her presentations that shows the dramatic difference in the micro-flora of an ME/CFS patient compared to a control’s flora. Her comment is now, “This slide certainly illustrates that ME/CFS is, indeed, a psychosomatic disease!” A great “laugh line”, but it illustrates what we are up against!
BrightCandle: excellent points! Thanks!
Actually, THIS is the Yong article, written a couple of weeks earlier that nearly stopped me in my tracks.
The description of the devastating cognitive impairment in long covid patients is exactly what I experience, though I have many more symptoms than he describes. He accurately says the term “brain fog” diminishes the experience. I call it “diminished consciousness” because that’s exactly what it is. It’s a devastation of executive functioning. THIS is the article I sent to my friends and family so they could get a sense of what some of my symptoms are like.
Oops. Hit send too soon. Here’s the link!
https://www.theatlantic.com/health/archive/2022/09/long-covid-brain-fog-symptom-executive-function/671393/
Same! I’d never seen an article that described the devastating mental effects like that one, and I too forwarded it to my family and friends.
OMG – Yong wrote that too. He just keeps popping them out. Amazing article – thanks for sharing that.
I’ve read several reviews of this article and really appreciate the breakthrough that it is, but what no one seems to report is how many of the ME/CFS specialists do not accept insurance of any kind, especially RTHM, which is actually a concierge medicine format that requires a monthly ‘fee’ beyond the posted charges per visit. (And why would a CFS specialist with 3 family members with the illness choose to focus her new practice for Long Covid patients?). This effectively makes treatment by many of the best specialists in the country completely out of reach for most patients, especially those with ME/CFS who are unable to work at all.
I wonder if the Bateman Horne Center is the only one that still takes insurance – which shows how important it is that a campaign that educates primary care doctors about ME/CFS and long COVID takes place. Dr. Bateman hopes that in a couple years a hundred times more doctors get up to date on ME/CFS. Let it be so…
By the way, Dr. Bateman recently announced in her newsletter that she’s cutting back on providing clinical care to focus on educating doctors (i.e., trying to get them to diagnose and treat me/cfs). I really hope this gets more doctors to treat us, but I think this will be challenging given the ongoing shortage of primary care providers.
The Bateman-Horne Center also has an access fee charge (currently $500/year for established patients) — but anyone can apply for a waiver based on income. The fee helps to support education and some research efforts, as I recall. The access fee isn’t covered by insurance; last I heard appointments are covered by a long list of insurance carriers. The BHC is a nonprofit. The insurance paperwork doubtless adds to the clinic overhead.
The BHC clinic also now “prioritizes” patients in the first few years of illness, and treats Long Covid. Hope this all adds up to more info on how to treat post-infective chronic illness.
So you’re on fire and you scream, “I’m on fire!” and people–and not just people, your friends, family, and firefighters, too–pass you by, day after day after day.
Thanks to Ed Yong. Thanks to Cort. Keep fighting, everybody.
You are so right. It’s been despicable. We have been ignored, not believed..even by family and friends..which has been more than depressing. We have been belittled. As I lie in bed feeling so so bad and cry sometimes, I hope, as we all do, to get help. Even the doctors who know it’s true just say they don’t know what to do or say. This has been thirty six years for me. Love to cort and all of us who suffer and the researchers who are trying.
Also, I’m not as enthusiastic as everyone seems to be about the marriage of Long Covid and ME/CFS. My concern is that doctors (and insurance companies) will enthusiastically embrace the Long Covid diagnosis with it’s clear origin story, and continue to marginalize (judge, abandon, criticize, and yes CHANGE THEIR PRACTICES to eliminate) the patients who haven’t had covid.
I know what you mean. I’m very skeptical, as well. There is such a stigma attached to ME/CFS that doesn’t exist–or only minimally exists–for Long Covid. I can hardly believe I’ve had this damn illness for over 20 years and still constantly hear stories about patients being told by their doctors that it’s all in their head. When I see psychologists or psychiatrists writing articles on ME/CFS I want to scream!
Good article. Nice of him to mention the ME/CFS desert in the Midwest. Speaking from the Chicago area (aka the flyover).
Even big Chicago – that speaks volumes….
Thank you Cort! This is what I’ve been trying to say for years. Some viruses can leave permanent damage on some people and whatever name you want to give it, ME, FM, CFS, long Covid, etc, it’s post viral syndrome.
Agreed, Chris. But may I respectfully suggest that it’s post-INFECTION syndrome – viral, fungal, or otherwise. Some of us, for example, had severe candidiasis before developing this awful long-term condition.
Bill, your points of clarification regarding the emanation of this heart-wrenching syndrome, are well spoken. Its important for readers and practitioners to look at the various contributing pathologies responsible for this illness. A point to consider: the causes for the development of this illness continue to be ‘live’ within the affected person’s system. There is little published information to show otherwise. Successful full recovery stories are quite scarce.
Thank you, thank you!! I have struggled since even before my 1991 “official” diagnosis with ME/CFS and fibromyalgia. Doctors told me it was “all in my head,” called it a “wastebasket diagnosis.” Until long COVID began to affect so many people, little research has been undertaken. Maybe, just maybe, now someone will pay closer attention to this debilitating disease! Again, thank you! Blessings!
Excellent article, Cort. THANKS!
My birthday is Sunday, October 2nd. I’ll be 76. I’ve had ME/CFS for 40 years. All those numbers add up to what everyone knows on this website, a chunk of a life stopped in its track.
I guess at my age, this is my normal. Ed Yong’s article in The Atlantic was the gift I needed to thank all my friends and family for their love and bewildered acceptance. I have put my energy into sustaining my relationships and though, more often than not, I let people down by not showing up, this article in this publication gave the ineffable – – authenticity. Thank you once again, Cort.
Linda–I’m happy to see another woman of a certain age here (I’m 75). The Facebook forums I’m on seem to skew very young–mostly women in their 20s. (And how awful to get ME/CFS at such a young age.) I haven’t been able to sustain many of my relationships, apart from the most important one–with my husband of 40 years. Friends have fallen by the wayside. I also had to give up a career I loved, alongside a life I loved.
Jackie, I know! I also had to quit a career I loved because of not being able to process information. I’d been an advertising Creative Director and used to type A life. 3 kids, a blended family, a husband and intense work. I had years of remission during the 4 decades, but the virus was quieted, not gone. I am sad that you have lost friends, and I too have lost some, but wow, we each have 40-year marriages. Our husbands did not abandon us, even if they were/are perplexed. Especially when I have good days and seem to be wholly well again. I’m so sorry for all you had to sacrifice. It’s a profoundly difficult reckoning. Have we not identified with our achievements? Where did we go? How were you diagnosed, Jackie? I had a doctor who was well aware of the CFS cluster in Incline, Nevada and diagnosed me after a bout of Mono/Epstein Barr. However, there was nothing prescribed except rest. Right??? Rest in the midst of life. I fought it a long time and hated the diagnosis. Where did it go? It made me look and feel like a crazy person. I don’t know how people find their way through this disease, I only know that closeness to people I love and giving love and not losing a sense of the world, has saved me. I wish you all the love you can muster. I am mild/moderate now – in a terrible crash however. But I wanted to acknowledge someone who actually remembers The Beatles!
Linda–I’m so sorry you’re in a crash. I hope it’s over soon. Crashes can be so stressful, because we never know when they’ll end. BTW, have you ever tried Abilify (used by Ron Davis’s son)? It’s the first drug that’s helped me in over 20 years. I was diagnosed by a nephrologist at UCLA only 3 months after i became ill, in May 1999. But he neglected to explain the importance of rest and pacing. And never mentioned PEM. So I thought graded exercise would help, and ended up extremely ill. I got ME after a virus, though I did have Epstein-Barr many years before I got ME. A very difficult part of this illness was losing a career I loved as a technical editor. I worked at a research firm with a group of scientists dealing with space programs. We worked closely with JPL and Caltech. Also, my husband and I had just finished getting a book published and working with an architect to get our house built. So I–like you, too, I’m sure–had a very active, full life. I went from that life to being bedridden for a few years, then housebound for many years. During the severe part of my illness, I could only lie on the couch or in my bed, not doing anything. I couldn’t read, watch TV, listen to music, or get on the computer. It was a living hell. I’m so grateful to be doing better now. I think I appreciate my life like no healthy person ever could. I wish you the very best.
There was also an excellent and hopeful article in New Scientist magazine on CFS/ME a couple of weeks ago.
Thank you Cort and others we would never have seen this excellent article here in Australia. Long Covid, me/ cfs exactly the same symptoms in my experience. My brain is definitely affected.
I am very glad that I have found this site and I am very grateful for all the excellent information it provides. Since I am a newcomer, I don’t have much knowledge about the treatment of ME/CFS, but I am trying to catch up. Recently I’ve read here about vascular dilation and nitric oxide. Is there any evidence that taking l arginine to increase nitric oxide would be helpful for PEM?
Thank you so much Cort for yet another great article, I was recently put on CBD drops by my doctor, and they are really helping my ME/FM so much.
UK researcher today > https://www.youtube.com/watch?v=yF4PebYeYpU
I have come to the realization that the medical community is AS corrupt as politics AND big Pharma. It’s just about money changing hands. Nothing is going to be done…unless it leads to a windfall profit for one of these entities.
there is a little known doctor in Central Alberta who has been trying to help his CFS/ME patients, if @Cort wants to, people can pm me for his small clinic’s name
( there is also an Eleanor Stein from Calgary who uses TCR Sport Lab in Calgary for two day C-PETS– or a person can contact TCR Sport directly.)
Sending this from the UK. Thank you so much, Cort, for all your wonderful postings, always guaranteed to provide up-to-date, reliable information. Re. finding a doctor: it’s the same here. Hardly anyone knows anything about ME/cfs, and the Psychs are desperately fighting back after the updating of the NICE guidelines. The one beacon we have found is the wonderful Dr William Weir (who, I think, we found through a letter on this website). He is officially retired from the NHS, but is still soldiering on privately in his support for ME patients (& now Longcovid too). A lovely, kind doctor, who is doing his utmost to keep up with all the latest research & helping as many people as he possibly can. As a result, he’s terribly overstretched: we desperately need more like him.