

Can we please stop pretending that it is?
Note: In the following text I refer to “ME” to mean “ME not caused by Covid”. This is not technically correct, but done for simplicity.

Early on in the pandemic, there was speculation as to if Covid would be another ME causing virus. This has since proved true. Estimates vary, but a large portion of Long Covid is ME and, in the US, Covid has likely resulted in roughly 4-7 million Long Covid ME sufferers joining 2-3 million existing non Covid ME sufferers.
Many folks with ME, myself included, thought that this influx of cases might end up helping those of us with ME who had been here all along. After all, a substantial portion of Long Covid *is* ME.
Several years in though, this hope that Long Covid will help people with ME has turned into a baseless assumption. As things stand, there is substantial evidence that Long Covid is *not* helping people with ME in any systemic, meaningful way. By this I mean, I have yet to see any area where Long Covid is having a demonstrable net positive impact for people with ME. There are single studies, people, and organizations that are benefitting people with ME as a result of Long Covid, but all of these have the problem that, for any single instance of Long Covid benefitting people with ME, there may be another instance where ME is being harmed as a result of Long Covid.
As an example of this, consider that, for every study on ME that happened as a result of Long Covid, there may be one or more studies on ME that didn’t happen, also as a result of Long Covid. This could be due to researchers moving on from ME to Long Covid & then either repeating existing ME studies on Long Covid, for example. I challenge readers to come up with evidence of a single such area where Long Covid is currently having a systemic net benefit for people with ME.
Possible unproven future benefits don’t count. Many people with ME are hanging on by a thread and don’t have time to wait. Personally, I expect my long time partner will leave me soon if my health does not improve in the very near future. I do not have a plan for when that happens. I do not think I am currently capable of living alone and without income. Many other people with ME are in similar or worse boats.
Below, I will present evidence that Long Covid is having either a neutral or negative impact on people with ME in the following areas: Awareness, funding, access to medical resources, and quantity of research.
I don’t say all of this to be depressing. This article is not meant to bring down those who have hope of a better future for people with ME. To the contrary, my goal is to move the community toward that goal of a better future for people with ME, and for that, I think we currently have a situation that warrants acknowledgment and action.
This can end up benefiting both people with Long Covid and people with ME, but only if we first recognize that Long Covid is not currently having any systemic benefits for people with ME & in fact is actively harming people with ME in several ways. Then, we can better fight for the inclusion of ME with Long Covid – in terms of research, funding, awareness, etc. The status quo of complacency is not getting us anywhere. Ultimately, this should benefit people with Long Covid as well as people with ME.
Why this matters:
ME & a large portion of Long Covid are one and the same. Still, assuming Long Covid research will trickle down to help people with ME is aggressively optimistic. If the treatment for Long Covid ends up being a Covid-specific antiviral (not unlikely based on evidence of viral persistence) or is otherwise Covid-specific, then this treatment is unlikely to work on ME triggered by other causes.
One might claim that finding a treatment for Long Covid would still represent a large step forward for people with ME, even if this treatment does not work on ME not caused by Covid, after all, now, we “just” need to find the specific antiviral for every other cause of ME.
Unfortunately, a) Not every case of ME is caused by a virus, and b) I would argue though that, at this point, it could still take 10+ years to get to the point of having treatments for other people with ME.
Many of us do not have this kind of time left. It is also a best case scenario. It is likely that being sick longer will create more treatment challenges. Treatments that would have worked on someone who has been sick for one year may not work, or may only partially work, on someone who has been sick for 10 years. These challenges will not be addressed by Long Covid research that focuses solely on those who have been sick for < 3 years.
If there is something that would help people with ME but not people with Long Covid, it will likely never be tested in people with ME. It will be tested in Long Covid, concluded it does not work and abandoned. (This is similar to the situation in drug research, where most initial research is conducted on male rats. As a result, women may have more or unexpected side effects, and lower efficacy, & if a drug would have worked for women but not men, it will never make it out of animal trials – link).
Additionally, including people with ME in Long Covid research would have benefits for Long Covid patients too. No Long Covid patient has been sick for more than 3 years. ME patients have. By including ME patients in Long Covid research, we can better understand the long-term disease course and predict how Long Covid might behave after patients have been sick for longer. We can then anticipate these changes and possibly prevent them. If, for example, there are certain complications or comorbidities associated w/ Long Covid whose prevalence increases w/ time, we can study these in people with ME now & better anticipate their appearance in people with Long Covid. A better understanding of the disease course over time & the different ways ME can be triggered could also help shed light on disease mechanisms.
Current Effects of Long Covid on People with ME
The current assumption going around is that Long Covid is benefitting people with ME. Below, I present evidence that this is a baseless assumption & that Long Covid is either having neutral or negative effects on ME in several areas.
Awareness
By “awareness” I mean public knowledge of the details, scope and severity of a condition. Having more awareness can lead to more funding & research as well as less gaslighting of those afflicted.
So, is Long Covid increasing awareness of ME?
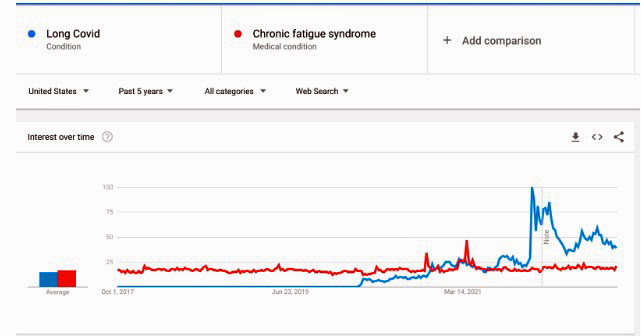
Google search trends
If it were, we might expect that the number of google searches for ME would have some correlation with the number of google searches for Long Covid.
That is not the case. During the pandemic, search interest for Chronic Fatigue Syndrome (CFS) stays stubbornly flat. Surges in search interest for Long Covid show no perceptible impact on CFS search interest. (Note that, I use CFS here instead of ME since CFS is much more common as a search term.)
https://trends.google.com/trends/explore?date=today%205-y&geo=US&q=%2Fg%2F11qm6vy88k,%2Fm%2F0dctd
(There is a tiny bump in search interest for ME that occurs around the beginning of 2022, but this bump occurs immediately after a note about “an improvement to our data collection was applied”, so it is likely an artifact of this rather than actual increased search interest.)
NYTimes Coverage – How often is ME mentioned in Long Covid articles?
Ok, so no more search interest in ME, but maybe more people have heard of it at least? Maybe through reading articles on LC?
To address this, we focus on NYTimes coverage of LC.
To date, the NYTimes has published 362 articles mentioning Long Covid.
Of these articles, 24 (6.5%) also mention CFS, and 14 (3.9%) also mention ME.
Most of these mentions are only in passing, so one could forgive a reader for missing them.
It is perfectly conceivable that a person may read several articles on Long Covid, and not become any more aware of ME.
NYTimes Coverage – Is standalone coverage of ME decreasing as a result of Long Covid?
Additionally, it seems that Long Covid news coverage could actually be *decreasing* ME news coverage. Again, let’s look at the New York Times. from 1980 to the end of 2019, the NYTimes has published 349 articles mentioning CFS, this works out to about 8.7 articles/year, on average. So far, during 2022, there have been 16 articles mentioning CFS, but 14 of these are actually about Long Covid, mostly only mentioning ME/CFS in passing. Thus, the only two articles in NYTimes in 2022 which mentions CFS but not Long Covid are this one and this one.
The first one is about a man with a mysterious illness that involved “strange episodes of utter exhaustion”. ME/CFS was briefly proposed as a possible diagnosis but ultimately was dismissed. The second one is about the challenges of dating for people with chronic illnesses. One of the (many) in the article has CFS, mentioned in passing. (There are also 10 articles from 2022 mentioning ME, all of which are about Long Covid.)
One could imagine that it would feel redundant for the newspaper to cover ME having already covered Long Covid. Hence, the decrease in ME coverage makes sense from that angle. That said, assuming Long Covid is increasing awareness of ME due to mentions of ME in Long Covid articles doesn’t take into account a) the fact that these brief occasional mentions are unlikely to actually increase awareness to any reasonable degree & b) the fact that, for every Long Covid article that mentions ME, there may have been another ME article that was not written as a result.
Silencing of ME in The Atlantic
News coverage of LC is not currently helping to raise awareness of ME. In some cases, it even seems to be making an extremely deliberate effort to avoid mentioning ME.
Take this article from The Atlantic. It attempts to position Long Covid among other, previously known post viral illnesses arguing that “we should try to understand and study [Long Covid] in the context of other long illnesses, not as something that emerged out of nowhere with no comparison or antecedents.” At first glance this seems great – finally, an article that acknowledges other post-viral illnesses! Reading the full article, however, there is a bizarre and glaring omission – neither ME nor CFS are ever mentioned! Instead, the author goes out of their way to avoid mentioning these terms altogether – instead using invented terms like “Long Mono”. “Long Mono” is ME. I have never seen it referred to as “Long Mono” previously.
It is unclear what the goal was here, but it could be a deliberate attempt to silence people with ME – people with ME have been gaslighted & considered fakers or hypochondriacs for so long that, many seem to think the only way for Long Covid to get taken seriously is to separate it from ME. Such a separation is likely to harm both people with ME & people with Long Covid. ME obviously due to the lack of inclusion & continued gaslighting, Long Covid because of the knowledge that will be lost by attempting to define Long Covid ME as an entirely new condition.
Awareness of ME Among People with Long Covid
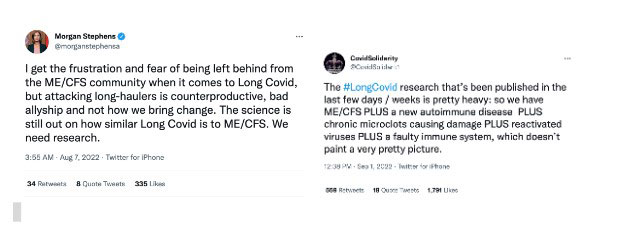
One might think that the influx of people with Long Covid would increase awareness of ME at least among those with Long Covid, but, alas, this too seems to be a mixed bag.
Although some people with Long Covid are good allies to people with ME, others actively work to distance themselves from people with ME in an effort to position Long Covid as more legitimate and more deserving of research and treatments. Such positions serve to actively decrease awareness as they spread misinformation. I routinely see people with Long Covid dismissing ME as “just fatigue” and dismissing the fact that people with ME have all of the same problems and comorbidities as the ME subset of Long Covid. Similarly, they frequently dismiss the fact that a subset of Long Covid *is* ME, claiming that “more research is needed”, or that Long Covid is somehow worse. None of these things are true. ME can have many causes. Covid is one of them. A subset of Long Covid is ME.
It is unclear to me if the positive allyship is outweighing the negative voices or vice versa.
Conclusion
In conclusion, evidence points to Long Covid having a neutral or negative effect on ME awareness, rather than the positive effect that is commonly assumed.
Medical Resources
ME specialists have always been few and far between. [link, link]
ME & the ME subset of Long Covid are the same & even if they weren’t, they have all the same comorbidities (POTS, ME, MCAS, etc), and therefore largely rely on the same networks of doctors and specialists.
With a large influx of Long Covid patients into this network, ME patients are having to wait longer for appointments or are less able to get appointments vs pre-pandemic. This makes sense, as Long Covid patients need these resources as well, but it represents a net loss of resources for people with ME.
Let’s look at what effects long Covid is having on a few of the big-name ME treatment centers in the US:
Stanford CFS Clinic, Palo Alto, Ca
This wait time seems to be growing – As of March 2021, the wait time was reportedly 7 months.
As of August 2021, it was 10 months, or longer if you want to see an MD. (Numbers from Facebook and/or Reddit.)
Stanford has also started a separate PACS clinic [link] that treats Long Covid. Long Covid patients can be treated at the CFS clinic, but CFS patients cannot be treated at the Long Covid clinic.
It does not appear that the CFS clinic has expanded to accommodate the additional demand from Long Covid patients. In fact, the only MD at the CFS clinic, Dr. Hector Bonilla, is listed as a co-director of the PACS clinic. It is unclear if he has reduced his availability at the CFS clinic as a result.
Center For Complex Diseases, Mtn View, Ca
This center has 3 physicians. Their website describes them as “Specializing in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis, Dysautonomia, Long Covid, Mast Cell Activation, Autoimmune Diseases, Chronic Infections”.
The current status of the three physicians who work here, all of which have been with the practice since pre-pandemic days:
-
- Dr. David Kaufman – Reportedly discharged many of his more stable ME patients to make room for Long Covid patients [link]
- Dr. Bela Chheda – Practice full, waitlist full as well.
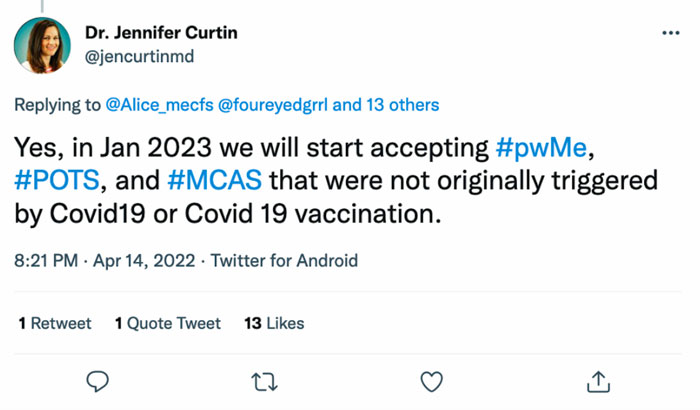
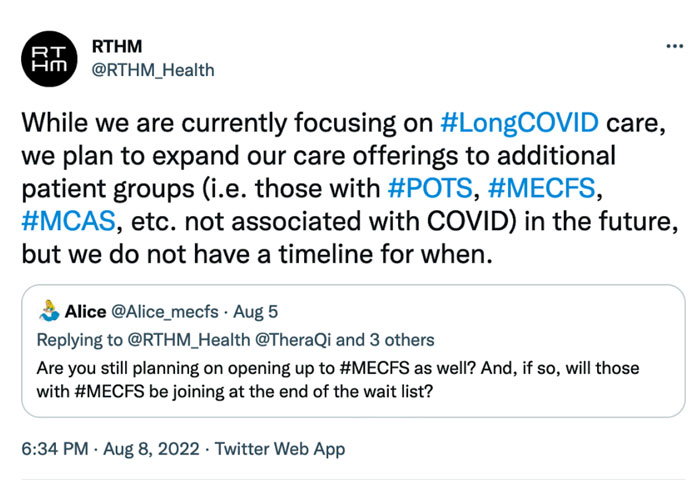
- Dr. Jennifer Curtin – Rumored to be quitting soon, to transfer to working full time at her Long Covid startup. In April, 22, she posted to Twitter that, in “Jan 2023 we will start accepting #pwME, #POTS, and #MCAS that were not originally triggered by Covid19 or Covid 19 vaccination”.
By August 8, 2022, however, the stance had changed. RTHM posted to Twitter that they are “currently focusing on #LongCovid care, we plan to expand our care offerings to additional patient groups […] in the future, but we do not have a timeline for when.” The current status of RTHM only accepting Long Covid patients means that Dr. Curtin leaving her current practice will result in a net loss of care for people with ME.
It is unclear what fraction of patients from the Center for Complex Diseases clinic overall are Long Covid patients. Pre-pandemic, patients on Facebook and Reddit reported wait times for new patient appointments at the clinic as a few months. During 2021, they were reported at ~ 1 year. Now, they are simply not taking new patients and existing patients are losing access to care as a result of Long Covid.
Bateman Horne Center, Salt Lake City, Utah
A subset of Long Covid is ME. Long Covid & ME are currently sharing the same extremely limited network of doctors. Many doctors who previously specialized in ME & related comorbidities are now focusing partly or exclusively on Long Covid. People with Long Covid need care as well, but, other than Ed Young’s recent article in The Atlantic, I have not seen anyone discuss, or even mention, how, much of the care people with Long Covid are getting, is coming directly at the expense of people with ME. This represents a shift of resources away from people with ME. I have not seen any evidence that doctors and clinics moving on from ME to Long Covid are being replaced.
There is no cure for ME or Long Covid, but treatment can help manage symptoms. This treatment often takes the form of a “guess and check” approach, requiring multiple doctor visits to explore different treatment options as well as to manage new or worsening symptoms. Losing access to treatment can mean a worsening course of illness. For some, this worsening can be permanent.
This is resulting in people with ME being less able to access care than they were pre-pandemic. Evidence also suggests that there are substantial resources available to people with Long Covid that are not available to people with ME, but the reverse is not true. Typically any specialist who will see a person with ME will also see a person with Long Covid, but a specialist who will see a person with Long Covid will not necessarily see a person with ME.
Additionally, many people with ME are reporting a worsening of symptoms following Covid infections. Based on wording from RTHM, Bateman Horne Center, and Stanford PACS clinic websites, however, these people would not qualify to receive treatment, because symptoms started before their Covid infections. Thus, these people are forced to wait in line behind all of the other people with Long Covid because they dared to also have ME.
Research
Has the quantity of research on ME/CFS increased as a result of Long Covid?
ME/CFS Paper Counts & Funding
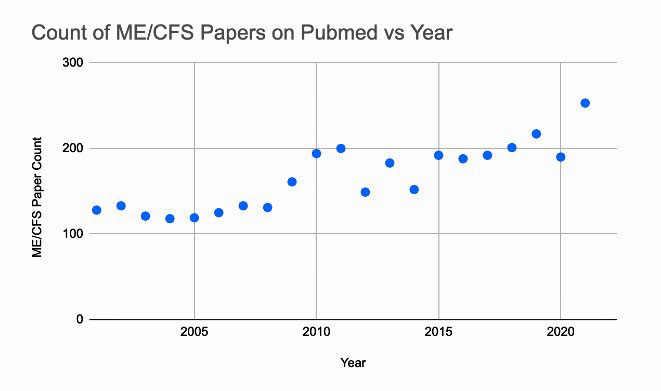
First, we consider the number of PubMed papers that reference ME/CFS in the title.
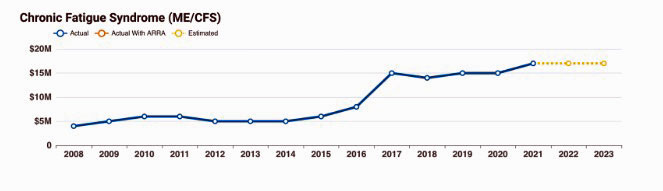
The count of such papers is not increasing as a result of Long Covid, rather, they are closely correlated with NIH funding of ME/CFS research, which, in recent years, has not even kept up with inflation.
In 2021 there was a slight increase in the number of papers over the baseline trend, but this is likely because fewer papers were published in 2020 as a result of Covid.
NIH Funding of ME/CFS:
The Gist
- There is an assumption going around that Long Covid is having all kinds of benefits for people with ME. Unfortunately, these benefits are not supported by evidence.
- Assuming Long Covid research will trickle down to people with ME is aggressively optimistic. Even if ME & a subset of Long Covid are the same illness, a cure for Long Covid could still be covid specific and not apply to people with ME. After such a cure is found, a cure for other forms of ME could still take 10+ years, assuming it gets funded.
- No Long Covid patient has been sick for more than 3 years. ME patients have. By including ME patients in Long Covid research, we can better understand the long term disease course and predict how Long Covid might behave after patients have been sick for longer. We can then anticipate these changes and possibly prevent them.
- The quantity ME specific research hasn’t increased as a result of Long Covid. It correlates strongly with funding for ME research, which hasn’t increased as a result of Long Covid.
- Awareness of ME has not increased as a result of Long Covid. There is no increase in Google searches for ME, and news outlets may actually be replacing coverage of ME with coverage of Long Covid, or otherwise intentionally avoiding discussion of ME in Long Covid articles.
- ME & Long Covid have the same comorbidities and therefore share the same extremely limited network of medical providers. Many providers who previously served the ME community are now focusing partially or exclusively on Long Covid patients. Thus, much of the care people with Long Covid are getting is coming directly at the expense of people with ME.
- We need to acknowledge the current negative impacts Long Covid is having on people with ME & fight to improve the situation. People with ME need to fight for inclusion with Long Covid – in clinics, articles, awareness, research, etc. This is the only way we are going to get the benefits from Long Covid that many assume are already here.
Applicability of Long Covid Research to ME/CFS
So there isn’t any more ME/CFS research as a result of Long Covid, but since a subset of Long Covid & ME are the same thing, Long Covid research should at least lead to benefits for people with ME?
Maybe eventually. Not soon.
To date, I don’t see any significant improvements that have come to people with ME as a result of Long Covid research.
There also seems to be a pattern of researchers who previously studied ME moving on to study Long Covid, thus, this loss needs to be taken into account when considering any potential benefit coming to people with ME as a result of Long Covid research. A study on Long Covid doesn’t represent a benefit to people with ME if that study came at the expense of another study on people with ME.
Additionally, as was mentioned earlier, it is entirely possible that Long Covid research will discover a Covid-specific treatment for Long Covid that is not applicable to people with ME. In this case, Covid research may offer a jumping-off point for ME research, but that ME research may take an additional 10+ years to find treatments for the most common ME causes, and that’s assuming it gets funded.
Most of us don’t have this kind of time to wait.
Additionally, as mentioned earlier, being sick longer is likely to cause additional treatment challenges that will not be addressed by current Long Covid research.
By relying on Long Covid to screen potential treatments for ME, we also may end up missing things that wouldn’t have worked for Long Covid but would work for ME. We will test them on Long Covid, conclude they don’t work, and then move on.
We can’t count on Long Covid research trickling down to benefit people with ME.
We need ME research to be drastically accelerated NOW. People with ME need to fight for this, hard. If we sit back waiting for Long Covid research to benefit people with ME, we will likely be waiting a very long time.
Additionally, we need to acknowledge the current negative impacts Long Covid is having on people with ME & fight to improve the situation. People with ME need to fight for inclusion with Long Covid – in clinics, articles, awareness, research, etc. This is the only way we are going to get the benefits from Long Covid that many assume are already here.
Email: alicekennedy330@gmail.com
Twitter: alice_mecfs
Check out a counterpoint to Alice’s blog.






Wow. I have felt this way for some time, but without the stunning amount of research in this article. For those of us with 30 years of illness, the priority is treatment, treatment, treatment, please. The giddiness with which CFS/ME organizations have embraced long COVID to get money for publicity and research is in practice matched by delays in starting research all over again to define the illness, losing whatever focus they had on what works as treatment. That may help people who get sick later, but likely not the population that needs treatment now.
Thanks Alice!—your research really brings the point home that historical aphasia and disinterest in ME treatment and research has bumped it for the ghoulish prestige of LC.
Thank you! I been feeling as if our status has gone even lower since Covid. We used to be invisible and ignored. Now we are discarded as sick too long to be worth the trouble.
I’ve gotten really tired of seeing these emotional stories about how horrible it is to be sick for a whole six months. Hey folks! there are millions of us that have been sick for decades. Get over yourself and include us in the help.
I’ve just given up hope for any sort of improvement. My health will continue to slowly decline, until some new health issue gives me a big kick, then I’ll be dead. I won’t even rate as a statistic on a government chart because I can’t even find a doctor willing to officially diagnose me.
People with long covid probably don’t want to be associated with ME because they don’t want to believe that they might be sick for decades. They’ll find out otherwise in a decade or so, but we who could have helped them deal with it will be gone.
how is me/cfs treated? 25yrs. and wanting to die…
Thank you. I thought it was me. I foolishly believed after the September 2022 report by Precision and Decode Me that finally help was coming. But every report every article any research grants were certainly not was I expected. Further, after reading this article I have to address my doubts that ME and its counterparts will be swept under the carpet as they have been for all these years. The cost to the economy and more I will not mention because to do so would make my words unresponsible at this present moment. But this article was researched long and hard as only those who suffer understand. I stand with you. Thank you for your truth, integrity and awareness. Well said.
Great article!! Reflects exactly what I’ve been thinking!! Sad… but true!
Very well researched article that shares some of my concerns.
My first concern had been about a red herrings effects. Endothelial and cardiovascular problems that are specific to COVID, in particular. There has been a bumper crop researches on those lately, it seems, and attempts to extrapolate it to ME. Instead of looking long COVID in the context of ME, they are looking ME in the context of long COVID and starting the cycle all over again — the cycles that ME has gone through already with lots of red herrings and whatever was fashionable at the time (XMRV anyone?). We are again feeling the trunk and calling the elephant a snake.
My second concern is that long COVID may turn out to be an ME with a cause, similar to metal/chemical poisoning or CCI. It’s possible that endothelial problems specific to COVID is indeed causing long COVID, and then ME patients without such problem could again be delegitimatized.
In conclusion, I do agree with Alice that long COVID research should be done in the context of ME, not the other way around. Or long COVID should be considered separate from ME till then.
Oh, and kudos to Cort for publishing the view opposite to the popular sentiment.
Thanks – I think Alice has raised some really important points – in particular the lack of ME/CFS-specific funding for research and education of doctors.
I am more optimistic in the long term but I’m still agog at the fact that even after all the interest in long COVID and its clear connection to ME/CFS the NIH kept funding for ME/CFS at the same pitiful level. That really blew my mind.
https://www.healthrising.org/blog/2022/02/19/nih-kicks-chronic-fatigue-syndrome-teeth-regret/
Similarly, the RECOVER Initiative has refused to allow ME/CFS patients entry into its studies. The NIH has said Congress paid to study long COVID not ME/CFS but it could easily rectify this by adding some funding to the RECOVER studies to include people with ME/CFS.
That way as the long COVID findings role out we would immediately know if they applied to ME/CFS. Ditto with the treatment trials. It would put us right in the center of things and make a HUGE difference for this field. That, literally, is all I believe we need.
The RECOVER infrastructure – which was the difficult part – is all set up. It would be so easy to study and track people with ME/CFS. It’s just so galling and really so telling about the NIH that they’re not willing to do this seemingly rather easy thing.
https://www.healthrising.org/blog/2022/04/11/long-covid-memorandum-nih-chronic-fatigue-syndrome/
Things may be changing over there – I suspect they are but as Alice noted – no hard evidence of that. No systematic changes yet for ME/CFS and, as I’ve said ad nauseam, it seems, this field is too small to take advantages of the long COVID research findings in a reasonable amount of time – certainly not in the timeframe that people like Alice need.
I believe the endothelial problems observed in Long Covid are similar to what ME/CFS patients are experiencing with their brain fog and IBS symptoms. No one has ever explained why ME/CFS patients all experience “fibro-fog”. If that nut can be cracked by discovering the cause of fibro-fog in Long Covid patients, I am certain a door will open for ME/CFS treatment. We are constantly wondering what is going on with the mitochondria in ME/CFS. Again, if research money dumped into Long Covid mitochondrial research answers some questions about fatigue, I am certain that data will also help treat ME/CFS. I believe Long Covid is a type of ME/CFS. The symptoms are too similar. Dr. Bateman has a sister with ME/CFS. She darn well knows that the funding for Long Covid will generate lab data that will help with ME/CFS treatment. I also have no problem calling ME/CFS “Long mono”. Even if all cases of ME/CFS are not caused by virus’s, it is more understandable to the general public. People ( political MD’s) at the top of the NIH are standing in the way of ME/CFS research. If the fright of contracting Long Covid and Long mono generate more funding to discover the cause of the symptoms (Fog, POTS, IBS, fatigue, microclots, mitochondria problems) ME/CFS patients will benefit greatly.
Alice’s term “gas lighting” is the perfect way to describe Fauci’s attitude toward ME/CFS.
It’s actually the other way around, I think. The brain fog in ME is long thought to be caused by brain inflammation and Michelle Monje of Stanford demonstrated that the brain fog in long COVID is also caused by microglial inflammation in hippocampus using the COVID mouse model developed by Iwasaki of Yale.
The only way I can think of endothelial damage causing brain fog would be through BBB leak. The BBB leak theory in ME has been looked into and nothing much came out of it as far as I know. Maybe long COVID people will dig it up again and repeat the process rather than making progress.
Long-mono!! Genius. We should’ve thought of this as soon as the term “long-Covid” came out. It would help link the illnesses in social consciousness and especially within medical community.
I can’t prove my nearly-lifelong ME was caused by the mono episode I had as a child (Epstein Barr, etc) but I would have no problem referring to myself as having “Long-Mono” to the docs and specialists I have been trying to get help from for my POTS/ME/FMS who are more ignorant about ME than long-Covid. Even the nicest docs I’ve waited a year now to see don’t want ME patients and try to tell me to go find a specialist. I have to educate and explain and then if they still want to try to help me, jump through several months worth of scheduling appts and testing yet again that I can’t afford or have the time and energy to do, just for the chance of getting the special doc to prescribe an off-label Rx from the MECFS clinicians guide to treatment they don’t care about reading. Maybe if I explain “long-mono” they’ll be more willing.
If microglial inflammation was causing fibro-fog, i would guess that the symptoms would vaccinate greatly. Which they don’t.
“Long Mono” is perfect. Easy for anyone to grasp. Easy for sponsors to understand. Even physicians would be able to diagnose us!
Long Mono” is perfect. Easy for anyone to grasp. Easy for sponsors to understand. Even physicians would be able to diagnose us!
Sorry but I really disagree. Microclots were found due to long covid research and nattokinase was popularized on the /r/covidlonghaulers subreddit. The subreddit has been just as helpful as the CFS subreddit for me. Nattokinase has allowed me to do light exercise like yoga and physio, who knows how long it would have taken to find microclots if it was just CFS. It doesn’t make me feel much less fatigued, just lets me do more.
In addition, the stellate ganglion block was shown to be effective in long covid. I haven’t gotten the SGB but it really fueled my interest in the autonomic nervous system and I’ve had some minor gains by reducing the sympathetic nervous system and boosting the parasympathetic nervous system. It has changed my mindset.
There are so many new drugs that are being studied for long covid, and I’m sure most of them will be beneficial to CFS as well. I saw one post on the longhaulers subreddit that said there were 13 immunotherapy drugs in trials. There are much more research into auto antibodies since long covid arrived.
I feel like a dim light is shining where previously I was in the total dark, I am now seeing clearly many avenues to get better where previously I barely had a clue.
People with long covid are our brothers and sisters, this doesn’t even have to be about me and my results. I thank them for just being there. I almost care more about helping THEM than myself. I don’t understand looking at a group of people who are suffering immensely and saying “you’re not being helpful”.
I feel like this just alienates our allies, allies who know fatigue and may spread awareness and information for the rest of their life.
I do totally understand saying researchers are not integrating CFS into their models enough when doing long covid research, or people are not realizing long covid is a subset of CFS, or some subsets of long covid are not CFS, or doctors are giving more attention to long covid. But I feel like that is small compared to what we are getting.
We are getting so many more possibilities, from the blood and tears of people who are sick, who are practically the same as us, and from heroic researchers who make great efforts, how can we trivialize that? There is nothing trivial about that, this is monumental. To just look at two short years is short sighted.
Even people who are researching AI, I’m grateful for. In 10 years AI will be making huge contributions to curing disease. It is the fall back plan.
Microclots/fibrin deposts – Hughes/Schofield/Berg – Aprehsis has been around for ME for years it is not new.
There is nothing new that I can recall.
@Flip In research, things often have to be rediscovered and reframed many times for them to make an impact. Like, the main algorithm for AI, backpropagation, was discovered in the 1960s but only became wildly popular in 2012, now it is fundamental to the field.
It doesn’t matter if there were hints for microclots earlier, this time people outright said it was a major factor, clearly explained it, and nattokinase was available for any person to buy online for not much money.
@Flip, you are right though, as outlined in this article, hypercoagulation and thickened blood were found as early as the year 2000. It just wasn’t talked about much.
https://www.healthrising.org/blog/2018/08/15/sticky-blood-antiphospholipid-syndrome-pots-chronic-fatigue-syndrome-and-fibromyalgia/
I’m not sure how to do it – but somehow we have to address this issue – that some people -with long COVID are actively working to make sure the long COVID is not linked with ME/CFS and that ME/CFS is not included in long COVID research. We can’t pretend it’s not happening – but we don’t want to overstate it either. I don’t know but I suspect that it’s not causing that many problems overall.
Still it would be helpful to enroll them in the idea that linking ME/CFS to long COVID makes sense, is beneficial to them, and is also morally the right thing to do.
Totally agree with this! PWLC are going through the hell we know so well. Calling ME Long Mono sounds a brilliant idea. Nearly every human has EBV from early infections. Although my ME started with lyme (Borrelia) once Borrelia was vanquished, it is now powered by EBV. We need better antivirals and these will come from the Long Covid research.
This was meant to be aimed at the phenomenon of Long Covid, rather than people with Long Covid, I’m sorry if it came off as being aimed at the latter or came off as alienating as that was not my intention.
@Alice Kennedy I understand, most of your article was good and brought up good facts.
I do think saying “long covid is not helping people with ME” means you have to make the distinction. You could interpret in several ways. Just reading that, I thought of it as the “concept” of long covid, as in the people with it, the researchers, the impact it has on people. Everything involved with long covid.
But you meant to say very specific things, mainly about the “people in charge” rather than anything else. The fault has nothing to do with the virus in this case, but the inappropriate and uneducated reaction to the virus by certain groups of people.
I know your whole post does elaborate on what you actually mean. I was just arguing about wording and being specific, thinking it could be taken the wrong way by some people. I apologize for talking righteously when I was just taking your title and words at face value, out of context of the whole post.
One of the most appalling parts of the discussion is the exclusion from care, as with Bateman and others.
As someone blessed to have access & means to see an ME specialist for 7 years, it deeply grieves me that care is being more limited than ever. When I was first treated, I was told that those who do improve often do so in 4-7 years. Perhaps getting help in this critical phase is part of that decision. Certainly, most of my patient education came in the early years.
Still, as it often takes years to even be diagnosed (probably longer to muster the means for costly & distant treatment) I hope these trends will be reconsidered.
Aside, recently had EBV panel retested & still high, so add me to Long Mono!
THE NIH HAS NEVER CARED OR HELPED CFS/ME. THIS IS INSANE.
I agree COMPLETELY!!!!
I’m actually beginning to wonder if the government has some reason to NOT research ME/CFS. I’m not a conspiracy theorist, but come on!
There was significant knowledge and understanding of ME/CFS (Icelandic Disease) from the late 1940’s into the 1950’s. There were documented outbreaks in military settings.
Yet when the 1980’s Outbreak happened, somehow the government had no recollection of this known illness?? Even though the illness was outlined in Merck Manuals (or similar??) still in circulation at the time.
I used to think ME/CFS simply wasn’t “sexy enough” to garner interest – it doesn’t disfigure or directly cause death (or does it?? NO ONE KNOWS BECAUSE THEY DIDN’T KEEP TRACK)
But as I’m fast approaching 40 years Enduring ME/CFS, and not getting any younger or stronger….some days I can’t help but wonder what it is somebody doesn’t want us to know????
I have little hope for a cure in my lifetime. I’m now more interested in documenting how I decline with age, and if ME/CFS actually does turn out to be directly fatal after all.
If Icelandic Disease had been studied 75 years ago, we might be in a far different place.
I was told by Dr. Cheney that you can die from CFS IN 1986 when I was lucky enough to see him. It can cause lymphoma. And I’m sure many other illnesses. The activation of the sympathetic nervous system is so difficult and most docs know nothing of this. They say you are stressed and to deep breath or do yoga, etc. didn’t stop those feeling for me. Having so so many PVCs and PACs. Heart doc said he could tell I was stressed. For sure, what a brilliant observation. Propanalol, a non selective beta blocker did help but it does lower hear rate as it should but it made mine to slow. What to do? Get a pacemaker to keep heart rate good just to have some relief from the PVC and PACs? I deep breath so much that when I had a chest X-ray radiologist wrote he thought I had COPD which I do not. Everything is crazy. People are tired of hearing how bad I feel. I’m sick of saying it. NIH is partly to blame if not totally to blame. I thought when Francis Collins left it might change but NOT. MY EBV titers are so very high. The herpes group is so destructive. I’m having trouble with my eyes and my eye doctor thinks it might be herpetic eye disease even though I never had any outward symptoms of herpes simplex 1. We all know how we all feel. It’s ruined our lives, our businesses, our friendships, our relations with doctors, etc. Love to all of you and especially to Cort for keeping us informed. Has antivirals helped any of you? Sincerely, hipjaven@gmail.com
How long did you take Nattokinase and in what doses to see results?
@OM 4,000 FU on an empty stomach, It took around 2 weeks before I started being able to do more, and I’ve been taking it for around 2 months. It doesn’t have a crazy huge effect but it has zero side effects for me and works decently.
I’m entirely open to disagreement. I’m just not convinced that these single instances of things being attributed to Long Covid really represent a systemic benefit to people with ME.
Totally agree. I am not certain if I had covid but the doubt was there and I was sent to a long covid breath clinic. I have been hoping that in the event of a ‘cure’ for long covid, then I will be eligible and it might help with the ME. This article implies that it probably would not help.
I’m not qualified to say that it wouldn’t help. I just wouldn’t assume that it will help.
A wonderfully researched article that represents the frustration we all feel especially those that have been ill for many years.
There is, however, an assumption that Long Covid patients are being helped by the influx of research funds.
We have a friend whose brother nearly died of Covid. She works in his company and also became very ill with Covid and has continued to be sick for several years. She is seeing the doctor who treats me for ME/CFS so we are being offered the same treatment options.
Nattokinase is no revelation. The very first medication I was put on in 1984 was a type of blood thinner dextran sulfate (safer than heparin) and only available on an orphan drug status from Germany.
Also go back and look up David Berg’s research on the use of blood thinners in ME/CFS.
The question is “what did my doctor know 38 years ago?”
In my humble opinion, the only reason Covid and HIV have received generous research funds is because they kill people rather rapidly. While ME/CFS patients also die, it is after years of suffering so it doesn’t generate a lot of media or public concern.
Agree with this re: funding is for issues that are killing people quickly
I put my humble opinion next to yours, Betty. In the beginning HIV was predominantly a male disease and in Covid men also got it, many of them well-connected.
But government funding also has to do with the sheer number of new patients, missing workers in the eyes of a government. Long Covid patients can’t work (as much) and don’t pay taxes but are going to cost society a lot in the long term. Better splash out now than be sorry later.
ME/CFS is a more individual disease, easier to ignore.
Thanks for the David Berg info. “Old” research can still be very helpful.
I hate to say it, but this is how I’ve been feeling. I see a whole lot of interest in long covid and long ME sufferers are just as ignored as ever. sad. I hope I am wrong
Deltrus, thank you, I appreciate your (much needed) input to restore a more balanced view!
After so many yrs with ME, & seeing what had repeatedly happened with ME research, I saw this coming when people started jumping on long-covid research as beneficial to ME (& esp as so many ME researchers & Drs started going over to long-covid instead of ME)….I didn’t want to be negative, but I knew it was not likely to be helpful to us overall, & could very well be detrimental to many of us (for many of the reasons stated in the article). And, I hate being right about it – would have LOVED to have been proven wrong, though I am glad to see that some others are finally also seeing this. And, I do feel for those with long-covid – I don’t want them to be left behind either. I’m just so sick of ME being abandoned & left behind over & over & forgotten, etc.
The other thing is that while I’m sure that many with long-covid do in fact have ME as a result, I do not believe that all do…and quite possibly not even most. There are too many reporting symptoms that do not meet the CCC or ICC criteria of ME, & as such, studying only long-covid is NOT the same as studying ME. Plus, there are a lot of triggers for ME, & not all are viral. So, only studying one specific viral trigger potentially leaves out a lot of ME patients. If I’m re-stating some of the article, I’m sorry. Brain fog, pain, & exhaustion are very strong today, so I was not able to be as thorough in my reading of it as I generally am…..but these are issues that have been bothering me for awhile now.
Most studies show ~45%-50% of those with Long Covid have ME, but of course it depends what definition of Long Covid is being used.
Not all, but a very sizable group.
Agree that studying one viral trigger leaves out many with ME.
I was expecting the same outcome as you. ME isn’t new and flashy. I would say that we are yesterday’s news, but we were never news.
I disagree. Research often does not produce results in such a short time frame. I say we can hold on to hope as long Covid research continues. Of course it would be helpful if the research would incorporate people with ME/CFS to strengthen links. Also, we need fresh and innovative ideas from the research community, not just ideas related to previous research on ME/CFS.
My hope and despair has gone up and down over the many years I’ve read articles on health rising. That’s not to say I would stop reading the blog, Cort has always shared many points of view re ME and FM and that reflects a good journalism.
I appreciate the various views on what’s happening re ME vs LC.
It’s certainly obvious to me that LC is getting the focus now but it is good news that ME has been mentioned in several articles.
Aloha Cort,
This is all sad news to me but haven’t we become accustomed to disappointment/lack of care? (I have been sick since 1989)
The thing that actually struck my heart most in this entire article was “Personally, I expect my long time partner will leave me soon if my health does not improve in the very near future.” As if finding partners is not difficult enough in this world, finding one willing to live with a partner whose wheelchair is invisible seems all the more challenging. I can empathize greatly.
On a side note….I have begun treatment for Chronic Inflammatory Response Syndrome (CIRS) with Dr. Andrew Heymans partner Dr. Anil Bajnath at The Virginia Center for Health and Wellness. The overlap of symptoms is too great to ignore. I will let you know how it goes (if I can remember, lol).
How long have you been ill?
Sabina,
Heyman is brilliant, but most of his patients have a chronic immune response to the mycotoxins created by mold.
I’ve been ill for ~10 years, although there was a significant improvement in the middle.
It may be true – ask again in five or ten years, a decent research horizon – but it seems to be the ONLY credible hope we people with ME have right now.
It won’t be fast, and it won’t be efficient, but there are a lot of ME/CFS researchers out there who will USE any long-covid results to push THEIR research to the limits.
I, for one, prefer to have a LITTLE hope. It’s been very dreary otherwise. Not a lot, mind you, a soupcon of hope.
And there is always the possibility of something startling and world-changing happening – if research is going on at all which wasn’t before (like the research that proved H. pilori is the cause of most stomach ulcers).
I can be as realistic about chances, even as pessimistic as you are – but I’m not giving up the hope completely. Or what’s the point for many ME patients who are trying to hang on until something helps us?
Meanwhile, I will finish my mainstream trilogy with an ME/CFS main character, to continue to show what it means to LIVE with this monster.
Always room for some hope.
I just feel that too much hope can sometimes be a bad thing insofar as it discourages action.
The world definitely needs more books and other media with ME characters, short of knowing someone with ME, reading about a character with it might be one of the best ways to gain an understanding.
Alice, A well written, heartfelt article. I feel the same way but somehow hope that maybe some ME patients will benefit from the Long Covid research. On another note, my heart goes out to you regarding your fears for your future. I have been very lucky in that I have a supportive husband, Disability and a disability pension. Without those three things, I would not have made it these 11 years. Even with that, life has not been easy. I can’t imagine what you feel right now. Please know I am pulling for you.
Thank you.
I also hope that I am wrong. I think if there is enough action I may be, I’m just not sure the status quo is enough.
Very well said. Thank you.
I have long Covid — I hope other people with long Covid reading this will really consider what is being said and not get defensive. A lot of people with long Covid read this blog even if they don’t say that they do. It’s important to listen to a variety of views from people in the community especially people with experience of being ill for a long time. I do personally think that ME Will benefit from long Covid, but it also needs to be directly included in discussions, research, media, etc. and not just be an afterthought. Personally I have been frustrated at the lack of speed with which people are realizing and accepting that many people with long Covid have ME. in my eyes, the faster the correct connections are made the faster we will get to treatments that may actually help us all. I will say though, people with long Covid are not really getting very good care either. There are not enough doctors overall and we are “competing“ with each other in the world of long Covid too for medical appointments. It’s complete chaos and disorganization and many of us have just opted to stay home and try to pace ourselves as best we can and try a few supplements and wait for more help to come along. I also want to say that some long Covid advocates understand that they need to play a very long game and will continue to advocate for ME even if a Covid specific treatment such as an antiviral comes out. Many of us have been changed forever by our experience with this illness and there’s no going back. I believe that there are great organizations like a poly bio Who really are including ME in everything they do related to long Covid because that is where they started from. This article will hopefully open some people’s eyes to the dire circumstances and maybe they will become better advocates. I think a lot of people are Stuck in fear and denial. I hope we all get there in the end. I hope we can all be one united group.
Thanks so much Anon – this is the key ” but it also needs to be directly included in discussions, research, media, etc. and not just be an afterthought.”
I don’t think naysayers from the long COVID community are holding us back so much as that long standing institutional biases are. They are the real stumbling block.
Ed Yong penned a great article on the reckoning for ME/CFS and the medical field that long COVID is bringing. The issue is that the medical establishment has not responded. I don’t think Alice would have written this blog if the NIH was including people with ME/CFS in its RECOVER studies or if the NIH had increased ME/CFS funding or if long COVID clinics were embracing ME/CFS.
https://www.healthrising.org/blog/2022/09/28/yong-reckoning-long-covid-chronic-fatigue/
I fully believe that the over time the benefits will filter down – I have little doubt of that but the question is how long? Is it going to be ten years? Or is ME/CFS going to be fully integrated into this explosion of interest and funding and quickly benefit? I really thought efforts would be made to put ME/CFS on a more solid footing.
So I think Alice is right – we have to push for more funding and not wait for it. A blog on our advocacy situation is coming up.
My doc is treating LC and having very good success with Phentermine. He’s says his ME patients don’t seem to respond as well. I’m guessing this could partially be explained because we have been sick longer.
It would be interesting to have data on how people with long Covid also have ME or FM. It would also be interesting to know how many of those that died from Covid also had ME or FM. Maybe if this population is at greater risk, it would encourage researchers to include them in their trials, but I doubt it. We also know that if they come up with a drug, Big Pharma will immediately try to gain approval to use to other populations with similar symptoms.
Even if one were to get into a ME/CFS dedicated clinic, I’m not sure if a person might get helpful treatment. Case in point: I have been attending the Stanford ME/CFS clinic for several years now and at best I’ve been instructed on pacing and at worst I have tried a series of off label medications which have caused more side effects than have helped.
Truth be told, doctors and even researchers really don’t totally understand long-Covid or ME/CFS nor do they know how to truly, effectively treat it. Unfortunately, we, being patients, are at the end of the line in terms of proven treatments–or lack there of. We chase antidotal stories of success, more often than not to end in failure. I know I do.
But I will keep trying. And hoping.
Nancy B I was thinking the same thing. I went to Stanford years ago and all I got was an anti viral that didn’t work, and blood drawn for antibodies to the suspected viruses, which were extremely high but my docs back home only said it means I have a good immune system. So Stanford for me, 8 years ago, was a waste of time/money.
This is fair. It would be interesting to see stats on how many of those with ME or Long Covid are able to get into a dedicated clinic, and, of those, how many improve (& by how much).
I’m sorry about your experience with Stanford CFS clinic. I hope you are able to find something that helps.
Thank you for all of your efforts to publish this. I have been thinking the same. I am disappointed in clinics such as Bateman Horne. Not all ME patients had a viral onset. Now it is all about COVID.
Thanks to Cort for publishing this viewpoint, and in an article with plenty of supporting evidence. In the short term, the author may be right. But it is becoming an accepted belief–as a result of long-COVID–that there is such a thing as mysterious, post-viral illnesses. This is a HUGE leap forward (sadly), and long-COVID has MASSIVE coattails to grab onto. I believe there will be an opening for advocacy for ME/CFS to have greater impact as a result of all the attention/research/$ devoted to long-COVID. ME/CFS will stop being such an abstraction (to some), and people (some) will listen.
I agree Brian, how can long COVID and the funding its received not help tremendously with advocacy, understanding and interest. In the longer term I think we’re in good shape.
This article confirms what I’ve been thinking, so I’ll be interested to see if it is shot down by better evidence. Myself, I was first diagnosed with CFS in 2000, but it only lasted 6 months. Perhaps a better diagnosis might have been ”post viral syndrome.” Over the next 17 years I had two more bouts, each lasting 6-8 weeks. Then March 2020 I got sick with a cold?/the flu?/Covid? (not eligible for testing then), a brief recovery and then yet another bout of ”post viral syndrome” that I have not recovered from yet. My doctor called it “Central Sensitization Syndrome” but after joining a Facebook longhauler group to ask questions, I began to think my illness corresponded to Long Covid. I got a referral to a clinic that dealt with complex chronic conditions and had recently gotten funding to deal with Long Covid. It took me a year to get my first appointment there, but people I knew who were referred there at the same time for Long Covid got their first appointment within weeks. My doctor had identified my problem to the clinic as CSS, which smacked of “all in your head” to me. When I finally got my first appointment at the clinic I argued that I had Long Covid, not CSS. I’m not sure whether they believed me or not, I don’t feel I got the same kind of intensive care that long haulers did. Someone on Facebook suggested I had “gradual onset ME”, which finally turned into the permanent form by my bout of Covid in 2020. At this point whether I have ME or Long Covid is moot, but I feel that if I stick to the Long Covid label I may get better/quicker attention.
@Elizabeth Anne, I’m glad you mentioned that you had three episodes of ‘post viral illness’ before being struck down by full blown ME/CFS. I am the same.
I also had three short episodes of ME/CFS after moderately severe flu infections. Each bout lasted less than a year but more than 6 months and each got more severe and lasted longer than the last. Finally I got sick with the infection that never went away. It’s been 30+ years now.
To me this is a very important piece of evidence–it points to repeated assaults to the immune system that finally kicked it over the edge. I know that most doctors ask about the ‘one primary cause.’ To those who ignore multiple episodes of onset, I think they are overlooking something very important. Thank you for mentioning it.
This is interesting, as I’ve seen some argue that people with ME should refer to themselves by the thing that caused their ME (long Mono, long concussion, for example), in order to have better parity with Long Covid.
Unfortunately, I think it’s pretty common(?) to have situations where the cause may be unknown or a mix of things, so this becomes more or less impossible.
It also seems like a lot of folks with ME are getting a lot worse after covid. Is this Long Covid, or an exacerbation of existing ME? Both?
In some cases ME and Long Covid are more or less indistinguishable, yet there are a lot of efforts to separate them.
The medical profession and public will continue to either reject M.E or vaguely acknowledge it…until they suffer it them selves. However, the L Covid medical research and its productive results will benefit M.E sufferers whether we like it or not.
And certainly as a sufferer of ME since 1986, i am not concerned with where helpful medication, and other fields of treatments comes from , or whether we sufferers gain acknowledgement .
Instead, bring on the super intense research and particularly cellular studies, that may bring new life , especially to children who have ME.
I remember the days when such children were removed from their families and made to exercise, due to mis diagnosis from the Psychiatric profession, with uk Government support.. That was the UK,s way of dealing with ME back in the 1990.s.
So…we have come a long way since those dark days
My experience is that any expectation of sympathy, support and understanding outside of our global society of sufferers, is unlikely . Yet , thanks to L Covid , we will indirectly gain immense steps forward.
Children are still being removed from their families & put into Psych units, made to exercise, etc…….we have NOT come a long way at all re that.
I appreciate the immense frustration behind this article (and yes, thank you Cort for publishing it). I am one of those “OG” long haulers (infected March 2020) who now also has ME/CFS. Early on in my illness, I scoured the internet for answers; that was when I first learned about ME. I had never heard of it prior. I felt intuitively that this is what was happening to me. I was stunned that folks had been sick for decades with such little research or few viable treatments.
There are a few long COVID advocacy groups that have subtly asked patient advocates like myself to steer away from mentioning ME/CFS. I refused outright. What little treatment options we long haulers have had or tried came from our ME brethren. Plus, to me, if it quacks and waddles, it’s a duck. Estimates are that at least 50% of us long haulers have ME/CFS in addition to long COVID. I have all of the classic symptoms of ME and I went for the 2 day CPET with damning results; but I also have bizarre symptoms that are common only among long haulers. So, I know I have both.
I do however have to agree with Deltrus on a few points. I do not feel that the lion’s share of long haulers are dismissing or forgetting about folks with ME. And I don’t think it does us much good to splinter or divide ourselves; those holding the purse strings will just exploit that division. I also think that there really haven’t been any gains yet for long haulers as far as treatment. I take another person’s point here that 2.5 years just isn’t that long in the scheme of research. I also don’t want to be that tone deaf long hauler who implores decades-long sufferers of ME to continue to “just be patient.” I guess my point is that we shouldn’t play Suffering Olympics here, in either direction.
Lastly, I am participating in Fred Friedberg’s hydrogen water study that Cort featured here a few months ago. This is strictly an ME/CFS study centered around possible treatment. And yes – COVID caused me to have ME – but if this study’s findings show a benefit from the treatment, it will lead to larger studies and potentially a treatment to help many (not a cure, but it’s something). So to the author’s point that ME/CFS researchers are all pushing ME aside to get long COVID funding, that’s not entirely accurate (though I do understand that the amounts dedicated to each illness don’t even come close).
These are good points, well said.
One random thought on your mention of having Long Covid + Me –
I think one thing that gets missed a lot about ME is that ME is never (or hardly ever?) “just ME”. It comes with comorbidities. Some of those comorbidities may be unique to the mode of onset.
Covid ME = ME + long covid specific symptoms
Mono ME = ME + mono me specific symptoms
Concussion ME = ME + post concussive symptoms
It’s just that we hardly ever talk about other forms of ME the way we talk about those the ME subset of Long Covid. When talking about Long Covid, all of the comorbidities are talked about together with the ME. With all other ME, we only really talk about the ME, and the onset specific symptoms are discussed separately.
I’m not sure what my point is here, but I guess it is just interesting to see that you say “you have both”, since they are usually all lumped together under Long Covid.
I agree with the sentiment of this author and appreciate her research. Here are my observations:
Long Covid is getting a fair amount of attention, but treatment seems to be in the dark ages for the most part. The Mt. Sinai Long Covid clinic, for example, run by David Putrino, seems to mainly recommend pacing, eating small meals, and gradually increasing exercise as tolerated. Not exactly cutting edge.
The few remaining ME/CFS specialists are harder to reach than ever. The wait time for an appointment at my specialist has gone up dramatically because he has had an influx of Long Covid patients, and believes he can offer more to help recent onset patients than people like me who have been sick a long time (24 years).
I don’t think any new, younger doctors in the mold of Kaufman, Cheney, Bateman, Peterson, and Levine have chosen to specialize in post-infectious illness, including ME, because of the emergence of Long Covid. So that pie is not only shrinking, it’s being divvied up among more patients.
Solve ME and OMF, which get a lot of their non-grant funding from ME patients, are devoting more resources and bandwidth to Long Covid, diluting the attention paid to ME. By definition, Long Covid is a recent-onset illness, so a shift in attention to Long Covid means less attention and resources go to studying long-term ME.
Of course, the world of ME/CFS in terms of recognition, treatment, and research funding been a proverbial wasteland for the last 40 years. Long Covid has not changed the landscape. ME patients remain like an underclass of “untouchables” mostly ignored by the medical and scientific communities. And many of us will continue to die with no explanation why we were plagued for so long with such a life-decimating and grueling illness.
Yeah, because we’ve been ignored for so long, now the resulting length of time we’ve been sick is being used against us as reason that we can’t be helped….nice
Alice has said out loud what has been lurking in my mind about the news that long term ME research and/or treatment centers are veering away from ME and excluding us in favor of Long Covid. But of course, that is where the money is, now.
I hope this does not devolve into a blame game between long-haulers and ME people. This should not be seen as resentment of each other, or defensiveness. The blame belongs to the funding agencies, and to the appropriaters in government or foundations, who are poorly informed about ME. But at the same time, we must look squarely at the facts of the situation if we are to do anything useful.
I am very old, and have had ME for only three years, having developed it after a bad case of flu. It saddens me that there will be nothing forthcoming that help me in the short time I have left. I wish I could be more active in pushing for change, as I have been in the past. But between fatigue and brain fog, this commentary is about the limit for me.
I’m sorry. My hope is that if people are able to acknowledge the status quo, then those who are able can then fight much harder for rapid structural change.
I tend to see pessimism as more optimistic in a way than optimism, if that makes sense, as generally the former leads to more change.
It’s also possible I am entirely wrong, & there is a major breakthrough sooner rather than later. I hope you are able to hold on to some hope.
Considero realista y muy acertado todo el artículo, que viene a decir lo que tantos sospechamos desde el principio de conocerse Long Covid. Pero por ejemplo en mi caso que llevo 15 años con EM/SFC y también con Long Covid desde hace 31 meses, los médicos hacen como que no tiene importancia, ni una enfermedad ni la otra y como mucho, algunos para quitarme de en medio, se atreven a decir que seguramente lo que tengo es un empeoramiento de EM/SFC, y que con eso no pueden hacer nada. Es horrible vivir con SFC/EM pero les aseguro que lo es mucho más, convivir también con Long Covid. Y la desesperanza es diaria y evidente, claro.
Here is a quote from an NIH email I received today about the RECOVER study. I think it presents a valid point:
“Unlike other post-viral conditions, people who experience Long COVID were all infected by the same virus—albeit different variants—at a similar point in time. This creates a unique opportunity for RECOVER researchers to study post-viral conditions in real-time.”
Let’s not throw the baby out with the bath water, just yet at least.
I fail to understand how this rationale is beneficial. Whether we discovered post-viral illness in 1920 or 2020, this doesn’t help identify a treatment. Attempting to define a “new” syndrome detracts resources away from everyone. Together, we would be much stronger. While the newbies reinvent the wheel, the oldies will watch the NIH and CDC replay all their old plays with the same tragic outcomes. History repeats itself unless you learn from mistakes of the past.
I don’t think that’s the point. Many of us know in some ways it’s not a new syndrome. But letting this mass event go unstudied would be insane. We need to harness the lessons learned NOW in order to consider their applicability to all ME/CFS patients. Just my opinion.
Ultimately the “pie” – the number of researchers and doctors interested and knowledgeable about ME/CFS is so much bigger because of long COVID. I’m sure some ME/CFS cohorts are going to show up in long COVID studies – Time will tell but it’s possible that we could see more of those studies than studies with just ME/CFS patients in them.
The question for me is how can we help that process move forward as quickly as possible.
Amy, I was pointing out that the NIH “rationale” you quoted is purely marketing. From a scientific standpoint, it is meaningless.
I will give you an example. People who had onset prior to 2020, but got worse after Covid, do they have ME/CFS or LC?
I do not think NIH is going to be motivated to solve this unless patients and doctors apply more pressure. Separating us into groups decreases our power. We are much stronger together.
Not studying LC would be insane, yes! But so is not studying ME/CFS. NIH has had funding to research ME/CFS for years, but they squandered it. I think they are likely to squander the LC funding, too, unless they change course. They are not going to magically change their ways. Those who have been around the block know this. Putting blind faith in NIH has been disastrous so far. What makes anyone think it’s going to be different now? LC patients are not uniquely ill, we have (SADLY) seen this before. Doing nothing and expecting a different outcome is not wise.
Not all ME patients got sick from a viral illness.
How do you know this. The more heterogeneous the causes, the less reason to research ME alongside LOCO which clearly IS a viral illness. Nobody knows the cause yet but viral is number one favourite.
I don’t know what they are hoping to learn by studying long COVID in “real time” on top of the population data for post viral syndromes that we already have. I can tell you right now that the large majority of long COVID, if it is indeed a post-viral syndrome, will recover within a year. The remaining will get reclassified as ME and they’ll suffer for years or decades with the recovery rate less than 5%.
I wonder what most researchers’ hunches are about whether LC research will transfer well to ME/CFS and other post viral syndromes
As I just replied to above, not all ME patients got sick after a viral illness……those who didn’t are being completely ignored in all this yet again.
Whether or not everyone who came down with ME/CFS did so because of an infection is actually a bit in doubt since we know that some people with long COVID never knew they had COVID.
Tom, have you looked at the November 2021 Mayo Clinical Proceedings for ME/CFS document? I feel like this document is a road sign for the ME/CFS treatment underground railroad.
thanks poppy, i’ll check it out
I don’t think Long Covid is harming ME. I think it’s the best thing to have ever happened for the disease!
The amount of times I’ve seen the term ‘Post Exertional Malaise’ in studies, discussions and advice given to patients, since Long Covid came about is astounding.. That alone is a good thing. As creates interest in ME because PEM is such a unique symptom
Also the researchers who recently found micro clots in Long Covid decided to check ME/CFS too because the symptoms are the same, and they found them! Micro clots in ME is a huge finding caused by Long Covid research
This has opened the eyes of plenty who have seen it. In fact my doctor has just now prescribed me anticoagulants, whether or not they will help is yet to be known. But with these new Long Covid discoveries it is helping the ME cause. Research that finds the pathology of Long Covid will soon follow with drugs, and those drugs are likely to help many people with ME.
It won’t just be antivirals specific to Long Covid because many LC patients don’t have viral persistence.
Seeing a recent MedScape article showing that a large proportion of Long Covid is ME is fantastic in changing the narrative. It’s opening the eyes of once previously sceptical clinicians, researchers and most importantly this will be swaying the minds of funders.
‘Post-COVID Fatigue, Exercise Intolerance Signal ME/CFS’
MedScape
https://www.medscape.com/viewarticle/980536
I think the biggest most positive thing is Long Covid has given many with ME renewed hope!
But with medical science things take time. Although an existing drug could be discovered in the very near future.
If Long Covid hadn’t come about we would still be a forgotten dismissed disease. That’s changed dramatically.
The Google Trends search term ‘Post Exertional Malaise’ has jumped up massively! That search will take people to ME/CFS websites as is a pretty rare symptom limited to mostly ME/CFS
The search term ME/CFS after an initial spike 5 years ago has also slightly increased during the pandemic
This is all good news.
And here’s the thing if you want to be treated fairly along with Long Covid, just say you have it. And reap the rewards. It’s not lying as a large part of Long Covid is ME/CFS. Same same
If anything I see Long Covid as the new name for ME/CFS. Many therapies that benefit Long Covid will benefit ME. The key to getting them when they arrive, is now in the meantime, to make sure you keep telling your doctor you have developed Long Covid. Your doctor can’t prove otherwise either.
Long Covid is simply a name change for ME 🙂
The problems in the blood were NOT found because of LC…..they were found many yrs ago by ME researchers & nothing was done about them….and no, they are not “same same”…..in SOME cases, LC patients do have ME, but not in all (stats are guessing it to be about 50-50)….also not all ME patients got sick after a virus, so their illness is NOT LC.
It is most definitely NOT a name change.
Very interesting, Brandon! Good points.
If you have ME/CFS, try to get your EBV levels checked — there are about 4 or 5 different categories they can test and you should get them all tested. Mine shot up. This is probably worth someone’s knowing, if anyone cared enough to check.
PS What I mean, is after having Covid. The Covid does seem to reactivate issues with ME/CFS patients in a measurable way. Is anyone paying attention to this, in all the one sided attention to Covid?
And further PS, I think the greater interest in Covid is because of the death rates. As far as I know, ME/CFS has been shown to be a disabling disease, but not fatal. People are more impressed by death rates.
I was given Paxlovid when I was infected with covid. The first thing I noticed over the next 10 days or so was that not only was the covid gone, but my ME had really improved. However this would not last. I then got tested for EBV and tested positive. But my Dr refused to prescribe more antivirals, saying the research does not support it.
If it helps, COVID reactivated my EBV, and I’ve been on first famvir and now valtrex for two full years and nothing has changed. My EBV numbers remain off the charts, and no appreciable improvement in my symptoms. So maybe your doctor knows better than mine.
The article states that ME is a subset of Long Covid. But according to my ME specialist it’s the other way around. It’s Long Covid that is a subset of ME. In other words Long Covid is ME that happens to have been caused by Covid rather than other causes, including other viruses.
Hi Geoff – not all COVID long haulers meet the diagnostic criteria for ME. Anecdotally, about half are not meeting the ME diagnostic criteria. So I think either can really be considered a true subset of the other.
Sorry, *neither
Long Covid Is more newly seen as sister disease to HIV. CD4 levels are very low in some pw/LC. I don’t know if this is the case for pw/ME. The clotting mechanism failures are also seen as different. People with LC have issues with strokes, sudden death and possibly even more severe vascular damage. These are several reasons pwLC see themselves differently than pwME and with more severe disease presentation. Viral reservoirs are suspected. Two major complaints I hear are that researchers/treatment should specifically work on viral reservoirs and endothelial/clotting issues ASAP. There is a concern the reservoirs will cause damage (Ex: kidneys) before a window of opportunity for using antivirals.
People w/LC do tend to see themselves as more severely impacted due to what I mentioned previously and see themselves as being infected post acute infection with a more dangerous virus that any post viral ME. The spike protein is a concern in this perspective and the damage the spike is causing.
From what I can see of the stats, there are more people off work with ME/CFS disability than long covid. Whilst the virus itself might be more dangerous (and little attention has been given to the western viruses that have disabled the ME community so I can’t comment on it, it may well be) the mistreatment has harmed people with ME/CFS. The “push on/go away“ or graded exercise therapy Approach & complete absence of any assistance with any symptoms – no POTS testing or anti histamines or even sleep meds for most, in the Uk anyway – has resulted in a highly disabled and HARMED community. Over decades this means that the ME/CFS community has one of the worst qualitIes of life on surveys in any chronic illness. ME/CFS isn’t just Like “long covid but With a lesser, less potent viral cause”, its an horrifically neglected and mistreated illness – .people pressured to do graded exercise therapy & then abandoned when they collapsed. 10, twenty years on, sicker than sick , The worst tube-fed, that’s where many of us are.
This is very useful, Alice. Thank you for the fabulous research and putting it out there.
Speaking for myself as an Indian, the sense of ME/CFS wasn’t there in Indian scenario. Even till date, I haven’t discovered a community or even a small group identifying with ME. Instead, with LC we are stumbling into ME diagnosis that explains decades of pain that was dumped as a mental health disorder. I remember once I insta storied on PEM/PESE. And my Indian friend messaged-shrieked. I had explained what she had suffered a decade.
I am sure in many other Asian/African countries this is happening.
perhaps for the public to get it, our mantra needs to be
“Put us back to work, put us back to life, FIND a cure….FUND a cure!”
this could be my bumper sticker… if i were still driving 🙁
Love this mantra. Imagine all of us saying it together. We could all join online at the same time. Invite the media. Put signs in the yard. So people could see all of us not working and not living.
totally agree with every word!!! was thinking it a long long time…. thanks for this article!!! the thrueth!!!
When you already see the treatment/recovery assistance rolling out for LC sufferers, but nothing, not one thing new for ME/CFS sufferers – then this article sadly and disappointingly seems accurate.
I had such high hopes.
I agree with some of the premise of this article, but not all.
For example, there are some promising treatment trials for long covid which, if successful, could have real value for CFS/ME.
Alice, congratulations, on this important well researched essay. Thank you. This essay is very important for it forces us to think realistically about the situation in the ME community. I have no answers, but your point that TIME is running out for some many, is truly heartbreaking and true. Not sure what the next steps ought to be. Thank you.
Merci pour cet article. Optimiste en 2008, après avoir eu une grippe sévère, puis diagnostiqué EM en 2010, je deviens pessimiste aujourd’hui, partageant votre avis sur l’effet Covid pour l’EM.
A lot of suffering, a lot of frustration, not much hope. I don’t question or make light of any of that. Nor why this blog was written. However, it is hard to agree with everything that was written in this blog though.
Silencing of ME in The Atlantic? There was a Health Rising blog last week about an article in The Atlantic:
https://www.healthrising.org/blog/2022/09/28/yong-reckoning-long-covid-chronic-fatigue/
https://www.theatlantic.com/health/archive/2022/09/mecfs-chronic-fatigue-syndrome-doctors-long-covid/671518/
That article contains numerous references to LC helping ME/CFS. I couldn’t convey them half as well so I won’t bother.
What I will say though is that if 50% of LC turns out to be ME/CFS, when aetiology and clinical biological diagnostic tests are defined for LC, we’ll see how much benefit to ME/CFS there is. I suspect more than anything previously.
There is a lot of social media quoting in this blog. My, perhaps ignorant, reaction to that is resist division – leave it to the algorithms.
A hello from Germany! Here, in the course of the pandemic,
– ME/CFS media reporting has gone from zero to frequent.
– ME/CFS state research funding has gone from zero to the first ever funded project.
– TV channel Arte produced the first ever German (& French) language TV documentary on ME/CFS, referencing the pandemic https://www.youtube.com/watch?v=YYlsgzmjPtU
– A popular German TV doctor has produced content on LongCovid and ME/CFS.
– German biomedical researcher Scheibenbogen has been awarded the Federal Cross of Merit by the Federal president for her ME/CFS and LongCovid research and explicitely also for her fight for more research funding (you could say that one side of the German state is awarding her for fighting from research funding from the other side of state :-D). This award is non-monetary but a big thing.
– In a project, Schreibenbogen is working with representatives of 3 health insurances. While at first glance this seems disappointing as it’s not biomedical research, it is also very important because it raises awareness within the systemic structure.
– Various regional German politicians have started lobbying for ME/CFS.
– The German Association for ME/CFS, in cooperation with Charité University Clinic Berlin, has trained hundreds of doctors in officially accredited free online trainings on LongCovid and ME/CFS, which met with interest due to the Pandemic.
– Many doctors to whom I mentioned the training showed interest in it due to the pandemic.
– The head of a regional psychotherapist union has emerged as a strong advocate for biomedical ME/CFS and has already trained other psychotherapists re. PEM in combined trainings on LongCovid & ME/CFS.
– Though re. ME/CFS the German health ministry remains largely stuck in its old ways, the Minister of Health mostly a disappointment with regard to taking action on ME/CFS (both being additionally restricted by the “freedom”-oriented liberal party in the government coalition who holds the Ministry of Legal Affairs, and the government’s attention distracted by the war next-door and spending-intense energy crisis), still the pandemic marked the first time ever that the existence of ME/CFS (and as a biomedical disease) was acknowledged by the state in public statements (i.e. by the health minister, the federal president,…).
– ME/CFS and LongCovid patient organisations have teamed up and are working with politics.
– German LongCovid and ME/CFS researchers have helped with new WHO LongCovid rehabilitation guidelines that clearly acknowledge PEM.
There is still a long, long way to go, and things are moving too slowly. But I think none of the above progress would have even been conceivable without the pandemic – I think it has raised more awareness for ME/CFS as a biomedical disease than ever before.
There is still a lot of negative – Like in many other countries, public health messaging on LongCovid & ME/CFS is practically non-existent, LongCovid patients are being made worse in activating rehabilitation clinics across the country under the state pension system, and the health ministry is not taking action to prevent this. I am very glad that since last year I already receive a permanent health pension (not based purely on “chronic fatigue syndrome”, but other codes too and a 10-yr health history), as I think the big influx of PostCovid-fatigue is not likely to make it easier to gain a pension with ME/CFS. (And if everyone became sick, could a sick society just become kind of a new normal?) There is a part of the population who is in complete denial of LongCovid, attributing it all to the “genetic vaccine”. We have our own “LongCovid is all psychosomatic” ego-stroking clinic director touring our own equivalent of the Daily Mail and other media for money. (But also, in the course of 3 yrs of the pandemic, some media learned to report about PEM!). I think the health, social security and disability benefits system is still far from what they should be like: That you can openly call ME/CFS by its name and receive the appropriate support; and that not “just” ME/CFS but the reality of suffering and restricted function from any type of systemic or fatigue-type illness are recognised. (I am seeing my post-cancer fatigue neighbour struggling with a lack of recognition in the system just the same).
BUT: If you’d have told me 3 yrs ago that a state minister would be calling ME/CFS by its name as a biomedical illness? That a major newspaper would – with clear reference to ME/CFS – report on how rehabilitation makes the ME/CFS group of LongCovid patients worse? – I’d have thought you are kidding me! And each little step of progress feels like making history and is making me happy! 🙂
In the background, there is also a June 2020 EU resolution for more ME/CFS research funding by the member states, which in turn lead the German Health Ministry to start a 2-year project for assembling the state of research for ME/CFS in Germany. With this background, there is a chance that the pandemic will bring the necessary impulse for change.
There is also the possibility that huge numbers of LongCovid patients will enhance the current state of quasi-denial by the state as they flood the system, and awareness of ME/CFS may ebb again as the pandemic wanes. (I am not convinced of that, though, as it seems multiple Covid infections enhance risk of developing LongCovid).
But I feel that the pandemic has brought about a rise of awareness on ME/CFS that I could not have imagined before Covid. Systems still remain rigid, but I feel as if some change is starting to happen on the ground, with every single doctor who takes part in a training, or starts to see systemic illness in a biomedical light because of seeing it happen to patients post-covid.
Also, the ME/CFS research community is probably unique due to its spirit of openness and cooperation, and new PostCovid researchers become interested in ME/CFS, too. That, together with new research technologies, makes me feel that the silver lining of the pandemic will be progress for ME/CFS, too – not in every single LongCovid research project, but as a whole.
Wow…great story about the changes in Germany. Thanks for taking the time to write it all out. It goes to show that dramatic shifts can take place in a small amount of time.
Haha, I wrote it rather as an account how many small changes may over a long time hopefully add up to a big one. I don’t think people like F. who crashed in spite of precautions after featuring in a media video on severe ME to counteract some LongCovid minimising media features with a good one, or D. who organised the very successful government petition that now documents in all posteriority the need for action for ME/CFS but was met with a disappointing response from the ministry (and deteriorated my own health), or the guys who collected money for the BC007 ME/CFS project and initially lost out to LongCovid would feel as optimistic…But I wrote it also to amp up my mood by focussing on the small but noticeable steps of awareness for ME/CFS that did happen due to the pandemic in Germany, as opposed to a sea of wrongdoing and setbacks, and maybe for the first time, there are also few non-patient people supporting the community.
Realistically, I think LongCovid is where the interest for research funding is now: I fully agree with this blog’s call that benefits for ME/CFS may not come automatically from all LongCovid research and there needs to be as much inclusion of ME/CFS as possible now to benefit from this opportunity – or even the other way round, that ME/CFS research in its own right will have benefits for LongCovid and any future pandemic.
Yes, I agree the reporting is slanted towards post-viral, when many causes exist. I have written to authors a couple of times and effected a few changes in published texts in that regard. To me, in particular the information that gradual onset cases exist matters a lot – because that is my own story, and because knowing this is important to not automatically classify any case without sudden onset as depression.
To some extent I understand the current focus on viral onset, because that’s what can get things moving right now. Because of the similar PEM with different initial ME/CFS triggers, at least my expectation is that research might one day find a common pathomechanism, which may be informed by the post-viral research but in the best case also apply to other triggers. But much about that pathomechanism could be learned from simultaneously comparing ME/CFS patients with non-viral onset!
The answers to ME/CFS may come from an expected place…the Department of Defense’s PACT Act. Starting on November 8th, the VA will begin screening veterans for the effects of toxic exposures if they served near burn pits, the Persian Gulf, Afghanistan and other middle eastern areas of conflict, Vietnam and contaminated military bases.
How does this relate to you? Gulf War Syndrome is almost identical to ME/CFS and has been attributed to toxic exposures.
But, you say, my illness started with a viral infection. I didn’t have a toxic exposure. Are you sure about that? Toxic exposures are ubiquitous in our modern environment.
A toxic exposure that suppresses the immune system can result in the elevation of herpes viruses like EBV, HHV6 A & B, mycoplasma, bacteria, etc.
The DOD has the funds and the clout to develop diagnosis and treatment rapidly.
Betty,
Wow – that will be one to watch. I really believe things are as hopeful now as they’ve ever been for ME/CFS. The PEM GWI link is astonishing. Let’s hope it all comes together – 30 years plus of suffering for those with GWI now.
This is so interesting. Thought about this when I read up on coding gait disorders (I have gait disorder with ME/CFS): Found a medical site describing that a “psychogenic gait disorder” was defined for the first time after World War I trauma in soldiers. Then I thought about the mix of unimaginably high constant emotional and physical stress in WWI and the fog of chemicals they were operating in, and wondered whether post WW “psychogenic gait disorder” was rather part of a wider systemic GWI/ME/CFS type illness.
WWI also was the start of Spanish Flu.
I developed ME/CFS as a result of severe, prolonged emotional stress, not a virus, to the best of my knowledge.
A mi me pasó igual.
Desarrolle el síndrome sin que mediara ningún síntoma ni semanas , ni meses previos.
Siempre que hay una infección alguna sintomatología aparece por leve que esta sea. Pase el covid “asintomático” , me enteré por una PCR en enero 2021 pero a pesar de ser “asintomático” Experimente sudoración nocturna. Por lo tanto no creo en los pacientes asintomáticos, algún sintoma por mínimo que sea han debido tener .
Con el EM Salí bien de mi casa por la tarde y cuando volví lo hice mal
¿Que virus actúa así de forma tan rápida?
He considerado que ese estrés mantenido en el tiempo puedo de alguna manera afectara a mi sistema nervioso, dejando mis amígdalas cerebelosas en estado de hiper excitabilidad como lo que experimentan la gente con Estrés postraumático
He contactado con un anestesiólogo de mi localidad y voy a plantearle la opción de la punción del ganglio estrellado (SGB) al parecer conoce el tema
He leído información al respecto y contactado con algún otro anestesista y la tasa de éxito rinda el 70-80% de resetear el sistema nervioso simpático y apagar la respuesta de huida/lucha (ansiedad y estrés)
Tal vez tu, deberías informarte de ello ya que tu inicio tan poco es viral
Porque puede que lo que tengas sea un Trastorno de estrés postraumático similar al que experimentan los veteranos de guerra o incluso la gente que sufre un accidente de coche.
Y que ese trastorno sea el responsable de tu fatiga al mantener el Estado de estrés de forma Crónica.
Hi Fran, I have entered your text into Google translator. I don’t read Spanish. Yes, a sympathetic nervous system reset would be great for me, too. Please, would report on your stellate ganglion treatment if you pursue it? Gracias!
NPR’s “On Point” has a 47 minute discussion re how ME has helped understand along Covid.
How long ago did it air? (I have trouble with NPR’s search function)
I’ve been ill for over twenty years. I’ve watched breakthroughs come and go. I am more hopeful now than at any point in that twenty years. Nothing has the potential to better understand and treat post-viral syndromes than Long Covid research. It might take another ten years, but it would have taken far longer on the pre-Covid trajectory. It’s easy to pick holes in the way in which Long Covid research has not optimised the links with ME. That will change over time.
I find this article silly, and the evidence presented is weak and subjectively interpreted. So I offer my rebuttal which also contains weak evidence, in order to balance the negativity and alarmism.
It’s purely a numbers thing. The ME community has never been able to muster the fight to break through the scepticism and various adversaries in the medical industry. Most of us are too sick to work, let alone muster the strength and energy to drive the petitioning, protesting and advocacy that other patient communities have used to break through barriers to be seen as a legitimate condition.
LC is addressing this via the rapid increase in patient numbers, and more importantly, by forcing many in the medical and research fields into accepting that LC/ME/CFS is real. It’s turning vast swathes of neutrals and sceptics into allies.
Given that LC and ME/CFS are likely the same thing, even if ME/CFS is left out or discarded by some LC groups, this doesn’t change the fact that any treatments for LC will work for COVID.
Our day is coming! Sure some things are having suboptimal impacts, and we should be doing little things to aid the cause where we are able to. However, if you just look at the numbers and types of new patients, and the growth in awareness and support, it’s clear that COVID is the best thing to ever happen for us. Just try and be patient and celebrate every small win in the meantime.
This blog entry has prompted a lot of discussion, not just whining, which would argue for its usefulness. I find it useful myself and thank Cort for putting it together.
seconded! thanks alice and cort, and everyone disagreeing without being disagreeable. i am more in the hopeful camp, but i think it’s great to have my (our) assumptions challenged 🙂
Hey author, try this blog entry on this very same site from October 2021. Found it with 5 minutes of web search, and some other stuff. Could easily find more but I think maybe you should take your own challenge and go do some proper research.
All the best to you and your partner, but this blog you’ve entry is a total stinker. There are good points in it, but the overall premise is incorrect and doesn’t help those vulnerable community member that may already be feeling overwhelmed.
https://www.healthrising.org/blog/2021/10/30/inspiritol-long-covid-chronic-fatigue-syndrome-me-cfs-and-long-covid/
Updating the progress or lack thereof a year later is extremely useful. A lot has happened since October 2021.
Since ME/CFS is essentially self diagnosed, I can understand why LC sufferers may not want to be associated with us. MILD sufferers who go to work and the gym have no link to my severe status, and don’t seem to experience PEM. Every day new criteria are added to the list by individuals. It makes me doubt my own diagnosis of 10 years. Are LC sufferers similarly graded?
Several years ago, I attended a local ME group Christmas fuddle. They stood, queued, ate themselves silly, talked and complained about how they slept a lot. I had absolutely nothing in common with any of these people.
I feel GPs need to be more ready to diagnose Chronic Fatigue. And leave the ME/CF SYNDROME to far more incapacitated people. That might encourage LCs to join us.
I would disagree that ME/CFS is essentially self-diagnosed. I searched for years for an alternative diagnosis but my doctors insisted to me that ME/CFS was what I had. I found it embarrassing (that’s when it was known as Chronic Fatigue Syndrome) and belittling. Other patients of my main doctor had the same experience as I did.
I can’t find a doctor willing to stay in the room if I say ME/CFS. Mine remains self diagnosed, because no doctor has the decency to look into it. Now I’m too sick to get to a doctor’s office.
I agree. I had exactly that experience. But since there is no diagnostic test, it is wide open to interpretation, even abuse by both patients and GPs. I think the embarrassment you felt is exactly why many LCs don’t want to identify with us. The “diagnosis” has become way too heterogeneous I feel. A syndrome is where all the symptoms consistenty manifest together…like Down’s Syndrome. It’s not open to some symptoms missing, or others a
dded on by individals
ME/CFS is a diagnosis by exclusion, unfortunately the ME/CFS Services; where they exist are in turmoil since the NICE Guidelines review. They used to ask for a panel of blood tests to exclude other chronic dieases. And there was a long wait for an initial appointment , which involves travelling to. And then another 6 month wait for ‘Therapy’,eg’ Compassion Focussed Therapy with a psychotherapist.’ With long waiting lists, with Long Covid Services and NICE Guidelines (which seem to have been hijacked by the PACE ethos of GET etc. ) There is no requirement for a diagnosis for joining a support group, or subscribing to an online community blog, nor should there be. It is difficult enough to get help through the Brain Fog of disbelief as it is. I value very much support groups such as MED (as was) and SMEFG Sheffield ME and Fibromyalgia Group, and other local voluntary groups, especially their online contact and services such as Zoom meetings, one of the few good things to have come out of the pandemic. To be able to join in virtually and watch past Meetings, Talks. Gez Medinger’s is available at sheffieldmyalgiagroup/watch past talks/ Cort’s on FM is on there as well as an interview with Whitney Dafoe’s parents, Janet Dafoe & Ron Davis. among many others.SMEFG also welcomes Long Covid experiencers.
I particularly like to follow Health Rising and Sue Jackson’s blog ? Learning to live with chronic fatigue, They rescued me from despair when I was denied PIP Personal Independence Payments [disability] because of my lack of ability to represent myself fairly. I found them by googling ‘aphasia’ my biggest problem at the time. I didn’t have the vocabulary , through the ‘Brain Fog’ and ‘PEM’ and lack of exposure to other PE ME/CFS/FMS. I really value this Community and the people who contribute, comment, and do all the research and blogging, THANK YOU !!!!!
JR, ce reportage sur l’EM/SFC est magnifique. les essais sur le RITUXIMAD m’ont choquée. Si le traitement n’a pas été accepté dans l’EM/SFC, c’est, non pas parce qu’il n’est pas efficace , car il était sur 3 essais de petite envergure. Mais quand il a été testé en phase 3, par manque de financement, les doses ont été divisés par 2. On voit bien que les 2 chercheurs du CHU de Haukcland sont dépités. Faire autant de recherche pour au final ne pas tester correctement , à des doses insuffisantes la phase 3 !!!
J’invite tous ce qui le peuvent à regarder ce reportage.
Mon EM/SFC s’est déclaré après une intervention chirurgicale sous célioscopie en 2004. Je peux compté les jours où je me suis sentie “normal” depuis.
J’ai oublié de mettre le lien
Die rätselhafte Krankheit – Leben mit ME/CFS | Doku | ARTE
Thanks for that. My German isn’t very good, but I’ll look for it.
I agree with all your comments! (I can read French, but it is years since I have tried to write in French!)
Claudine, je pense qu’il y avait aussi des patients qui se sont detériorés avec le Rituximab (pour le footballeur allemand Olaf Bodden c’était catastrophique et l’a mis en chaise roulante si je me souviens bien, et je pense que Whitney Dafoe ne l’a toléré pas non plus).
I’ve read that there are also patients who deteriorated significantly on Rituximab, if I remember correctly it left German soccer pro Olaf Bodden wheelchair-bound by messing up his immune system, and Whitney Dafoe didn’t tolerate it either.
JR , merci pour cette précision. Je suis navrée pour ces 2 personnes. Je me suis toujours demandée si un traitement EM/SFC sortait, est-ce que je serais capable de le supporter? Déjà que j’ai des effets secondaires avec de simple compléments alimentaires .. mais j’imagine que je ne suis pas la seule .
Merci à toi Cameron de prendre le temps de me lire en Français.
To the point of the Atlantic’s poor coverage, there is one Atlantic writer who wrote well on ME/CFS – sympathetically, and saying that if only more research had been done on ME/CFS instead of leaving us all out in the cold, we’d all as a society be having an easier time with Long Covid now. I believe his name is Ed Yong, science writer for the Atlantic.
Yong was also featured on the Brian Lehrer Show (WNYC) about two weeks ago. I sent Cort an email about both the article and the email. Brian is very supportive of ME, rarely refers to it as CFS, and even can pronounce the full name(!). Yong reiterated the point that people with ME have been overlooked — I think he even used the word tragically, but I’m not sure — for so many years, and if only research had been done for us we’d be in a much better position.
The Brian Lehrer Show reaches a large audience. The interview with Yong was about 30 minutes long and can be found at wnyc.org/shows/ , then look under Brian Lehrer Show. Sorry I don’t know how to copy links to this site (nor does my ancient computer seem to know how!)
To the point of the antivirals, there is an interesting article from 2018 which I found by searching for EMB and antivirals. It has not been updated. Pagano is the lead article (UNC, Chapel Hill). It’s not focussed at ME/CFS but specifically at EBV alone. Goes into various antivirals and concludes that clinical symptoms are not improved but EBV levels in the blood *are* improved. The conclusion is that this is an important area of research that needs to be given much more attention to (ah, so familiar sounding).
I’m going to ask my doctor to try antivirals with me. My EBV levels in all four categories tested shot up after Covid, and my physical condition definitely was worsened (I had Covid, with paxlovid – and rebound covid – in May of this year). The results of a study, to me, don’t mean necessarily that an individual might not respond well.
The Ed Yong article in the Atlantic, that I mentioned above, was about Brain Fog as a misunderstood symptom. He then went into both Long Covid and ME/CFS has having this symptom, and made the sympathetic comments about ME/CFS that I mentioned above.
My previous doctor treated my ME as “Long Mono” because my IgG and M for EBV and CMV were very high. My new doc is clueless. This kind of reversal of fortune will probably destroy the last 10 years of my working life. There really aren’t an infinite number of doctors who treat even Long Covid, much less, any other ME definition.
Can Biden mandate the opening of multiple illness centers in the US that only see ME/CFS patients to execute broadly what’s being learned in research? That’s what we need. The lost productivity to this Illness is staggering. My career was interrupted mid life by this illness and I am waiting day by day to feel well enough to contribute to society again. I read of studies and treatments that I believe could apply to me but I have no way to get the specific testing to know whether to try that specific treatment. Do I have microclots? Do I have preload failure? Is my brain swollen? Do I have cranial instability or such issue caused by my scoliosis? How are my cytokines (beyond what my immunologist measured that look fine)? Do I have an underlying enterovirus? Are there illness flags in my DNA? Even though I am a patient at one of the article mentioned clinics, they do not run you through these tests. They don’t even do tilt table tests (though I know some clinics do).
This is only looking at short term imediate picture. Long term I think it will help us
The medical system does not cure diabetes, thyroid diseases, high blood pressure, arthritis, depression anxiety, endometriosis, kidney disease, cancer, sleep disorders, MS, strokes, lupus, etc etc.
It offers medications that most usually lead to ‘side-effects’or complications. And the ‘diseases’ pile on as they get older. No one has just one diagnosis.
Why would this system produce cures/ sucesful treatment for ME/CFS?
(I do include ‘alternative’ medicine here. Replace supplements instead of medicines in this model, which can be just as harmful and problematic, specially at the very high doses used)
I understand the frustration and anger. Also towards society around us whom doesn’t see we are sick, and often has the opposite of support to offer. This one is a big stinker for health)
The sooner one can get out of this mode of thinking, and start taking control of one’s own health, the sooner you can get better.
This is true for every disease out there, there is someone who figured out a way to get better / recover outside the medical system. Search for them and you will find them.
Hint: a lot revolves around food.