


Brain-fog: no need to create another term – the original says it all.
“Brain-fog”: it’s another descriptive birthed by the chronic fatigue syndrome (ME/CFS) community that’s been seamlessly by adopted the long-COVID community (you’re welcome!).
The Mayo Clinic – which historically has been no friend at all to ME/CFS but is showing signs of changing – has adopted it (“Brain fog from long COVID-19 “). Ditto with Harvard Health – (“What is COVID-19 brain fog — and how can you clear it?“), Healthline (“What to Know About COVID-19 and Brain Fog“), WebMD (“Fatigue, Brain Fog Most Common in ‘Long COVID“), and others.
A “thank you” is also in order to the massive long-COVID community; a big thank you for validating symptoms like post-exertional malaise and brain fog that languished in our corner of the medical field for decades but thanks to you, and your advocacy and your pain, have become commonplace and believed. Thank you for that!
The answer to a recent study’s question, “Brain fog of post-COVID-19 condition and Chronic Fatigue Syndrome, same medical disorder?” was yes. Sustained attention capacity, processing speed, memory, and ability to learn were primarily affected in both groups.
Note what a nice, coherent package this is: not being able to process information quickly makes it difficult to sustain attention, which impacts memory and the ability to learn. The authors believed that a reduction in the capacity to maintain attention, and a lower processing speed, underlaid all other cognitive complaints in both diseases. (That said, the people with ME/CFS generally had worse cognitive scores than the long-COVID patients.)
But what to do about brain-fog – one of the most troubling symptoms in both diseases? The big clinics, of course, don’t have a clue. With the exception of some stimulants (Vyvanse, methylphenidate), no drugs to my knowledge have been found to help cognition. Methylphenidate plus mitochondrial enhancers did improve cognitive symptoms as well as fatigue, sleep, and pain in a small GWI study. Jon Kaiser, MD – the creator of the protocol – produced a caffeine-plus-mitochondrial supplement for those who don’t want to, or can’t, try the stimulant drug approach. (I don’t know if it’s still available).
Recently, a different approach to cognitive health popped up in a small long-COVID trial.
Co-ultramicronized palmitoylethanolamide/luteolin
Co-ultramicronized palmitoylethanolamide/luteolin (say that three times quickly) is apparently a pretty big thing in Europe but has been dancing on the fringes of the alternative health movement in the U.S. for a decade or so. It showed up in fibromyalgia about 8 years ago (we reported on it) but not much has been heard since.
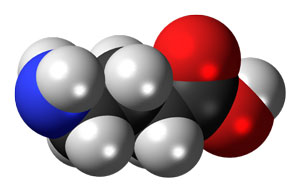
First isolated from soybean lecithin, egg yolk, and peanut meal back in 1954, palmitoylethanolamide, or PEA, is a naturally occurring endocannabinoid produced in our body, apparently in response to inflammation. PEA is not well known in the U.S., but it’s well-studied with over 350 references in PubMed dating back more than fifty years.
The Gist
- A recent study found that the brain fog in long COVID is very similar to that found in chronic fatigue syndrome (ME/CFS).
- Another study examined the effects of PEA-LUT – a food supplement – on GABA functioning in the brain and cognition in long COVID.
- Low GABA levels are associated with insomnia, and anxiety and difficulty turning off the stress response.
- Animal studies and some clinical trials suggest that PEA-LUT may be able to tamp down neuroinflammation and mast cell activation and reduce pain and possibly help in several neurodegenerative diseases.
- PEA-LUT appears to be a “balancer”; its produced locally in the body in response to stress and helps to return the body back to homeostasis. Low PEA-LUT and endocannabinoid levels have been hypothesized to open the door for neuroinflammation.
- The study found that GABA nervous system transmission was low in long COVID and that PEA-LUT increased GABA functioning.
- It did not appear to improve cognition. However, the tests used to measure cognition were not specific to the types of cognitive issues found in a disease like ME/CFS or long COVID. Since specific tests are needed to uncover the cognitive abnormalities in ME/CFS, the researchers may have used the wrong tests. Indeed, although the long-COVID patients experienced cognitive problems, the tests suggested that cognitively they were normal.
- The authors did not assess where the patients experienced symptom improvement.
- PEA-LUT is in a kind of in-between area. It’s certainly gathered some interest and the findings are generally good, but the studies are usually small and often lack real rigor. We lack the kind of large, well put together studies that we can count on.
- Still, PEA-LUT’s potential – tamp down mast cell activation and neuroinflammation – makes it intriguing. It is available on Amazon as Mirica in the U.S. for those who are interested. (Health Rising does not derive any funds from the sale of Mirica.)
- Dr. Michael Murray reports that 300-600 mg a day are recommended, with 600 mg being more effective in pain studies. When taking PEA for depression, try 600 mg twice a day. No side effects are reported.
PEA appears to be produced on demand in areas of local inflammation including, according to its proponents, inflammation in the brain. For instance, glutamate excitotoxicity in the central nervous system appears – in an attempt to calm the neurons down – to trigger the synthesis of PEA in the brain. One review even posits that a reduction in PEA and other endocannabinoids in the brain is what allows neuroinflammation to get out of control.
PEA’s proponents state it can affect two possibly large factors in ME/CFS, long COVID, and other diseases: microglial activation (neuroinflammation) and mast cell activation (via inhibition of histamine and TNF-a release and by blocking cyclooxygenase-2 (COX-2) and inducible nitric oxide synthase (iNOS) synthesis). In PEA-LUT, luteolin – another mast cell stabilizer – is added to PEA as an antioxidant to further keep the mast cells in check and to provide antioxidant benefits.
Websites will sometimes state that PEA is effective in diseases like Parkinson’s and Alzheimer’s, but PEA has not undergone clinical trials in these diseases. It has, however, been found helpful in studies employing Parkinson’s animal models, as well as chronic pain, where its effectiveness appears to lie in its ability to temper mast cell activation and calm down the microglia.
Plus, a retrospective study found that PEA appeared to be helpful as an add-on treatment in FM. Given possibly low endocannabinoid levels in FM, that finding seemed to make some sense. Another long-COVID trial of uncertain rigor found that PEA, plus olfactory training, help improve the ability to smell in long COVID more than olfactory training alone – suggesting that PEA may have reduced neuroinflammation.
Still, the studies – most of which come out of Italy – are relatively crude. Placebo controls are often lacking, and study sizes tend to be small. Some seem a little strange, as well, with physiological assessments being done but no word on PEA-LUTS effects on symptoms.
While none of these studies were strong methodologically, given the low GABAb activity found in long COVID, and PEA’s ability to seemingly improve executive functioning and GABAb activity in dementia – the authors had to ask themselves – why not long COVID, as well?
GABA – the “Anti-Anxiety Neurotransmitter”
This study focused on GABA – the “anti-anxiety neurotransmitter” or “brain relaxant”. If you’ve ever had trouble coming down after a stressful event, it may be due to low GABA levels. Low GABA activity levels are associated with anxiety, depression, insomnia, and mood disorders.
GABA reductions appear to play a role in many central nervous system diseases. It’s even been proposed that an inhibition of the GABA circuit the authors were interested in may cause fatigue. The LICI circuit and the executive functioning associated with it has been found to be impaired in frontal temporal dementia (FTD). A 4-week treatment with PEA-LUT improved executive functioning and LICI activity in FTD.
The Study
The PEA “brain-fog” study used trans magnetic stimulation (TMS) to assess the functioning of the motor cortex in the brain and cognitive functioning.
In this randomized controlled trial, 17 patients received either PEA-LUT (Glialia®, 700 mg + 70 mg, sublingual microgranule formulation, Epitech Group SpA, Saccolongo, Italy) or a placebo for eight weeks. (Glialia® is licensed in Italy as an oral food product for special medical purposes).
In the study PEA-LUT appeared to strengthen GABA pathways that can provide relief from pain, insomnia and depression.
The authors assessed GABA activity by measuring the activity of GABAB circuits (LICI) that studies have found to be depressed in COVID-19 and long-COVID studies. They also evaluated short-latency afferent inhibition (SAI) and long-term potentiation (LTP)-like cortical plasticity (memory). Low levels of both of these measures have been associated with cognitive issues.
Neurophysiological and neuropsychological assessments were given before and at the end of the trial.
Results
The study found markedly reduced markedly LICI (check!) in the long-COVID patients – suggesting that GABA activity was low, possibly resulting in at least mild anxiety, low mood, insomnia, and problems with cognition.
PEA-LUT improved GABA activity (LICI) and LTP-like cortical plasticity – suggesting it might be helpful in improving those symptoms and memory. It did not improve short-latency afferent inhibition.
The author suggested that PEA-LUT had reduced the activation of mast cells, astrocytes, and microglia – thus allowing GABA functioning to improve. They noted that PEA also appears to down-regulate the synthesis of an endocannabinoid, 2-AG, that acts to squelch GABA release.
Despite PEA-LUT’s potentially beneficial effects on the GABA circuits, it did not improve “global measures of cognition” and executive functioning. The author’s blamed themselves for this, suggesting that the data showed that a “ceiling effect” was present; i.e. the testing found that the patients demonstrated too much cognitive ability for any additional effect to be shown.
In fact, according to the tests used, the patients showed almost no cognitive decline at all – scoring 25 out of a possible 30 score on the global cognition test. That suggested that either they had the wrong patients or they used the wrong tests.
Since the patients did exhibit reduced GABA activity, my bet would be on the wrong test scenario. Specific tests are needed to pick up the cognitive issues in ME/CFS. Dr. Cheney, for instance, sent me to a neuropsychologist who knew which specific tests – which were not standard tests – to do.
The Montreal Cognitive Assessment the authors used does provide short assessments of attention and short-term memory but does not assess information processing speed – perhaps the key cognitive problem in ME/CFS. The Frontal Assessment Battery was designed to detect dementia. It’s used in other diseases but is probably not optimal for long COVID or ME/CFS. The authors noted that “more sensitive” cognitive tests might be helpful.
Conclusion
PEA is one of those “in betweeners”. It’s been around for a while and has garnered a good bit of interest in some circles, but it hasn’t been able to get over the hump. The results of laboratory, animal and some human study results have, in general, been encouraging, but the large, methodologically rigorous (and expensive) trials that you can take to the bank are lacking in these diseases. Some larger trials in osteoarthritis and depression, however, have had positive results.
PEA’s ability to possibly improve GABA functioning and reduce neuroinflammation in long-COVID studies plus animal studies showing it can reduce mast cell activation and neuroinflammation suggests it might be helpful. I haven’t tried PEA-LUT, but it is available on Amazon as Mirica in the U.S. for those who are interested.
Dr. Michael Murray reports that 300-600 mg a day are recommended with 600 mg being more effective in pain studies. When taking PEA for depression try 600 mg twice a day. No side-effects are reported. An old website (now off the web) advised trying it for 8 weeks. If you’ve tried it please let us know how you did.
Health Rising does not derive any funds from Amazon sales of PEA-LUT
BIG (Little) Donation Drive Update
Thanks to the over 250 people who have contributed over $21,000 to HR bringing us to over a third of the way to our goal.

If it’s possible it might work we want to check it out
The PEA story exemplifies one of our core goals – to seek out any possibility that might help, then dig into it, and assess its pros and cons. Our first blog on PEA showed up in 2014 – and now 8 years later, here we are again.
A lot of possible treatments don’t get the big studies but still deserve our time and attention…You never know what might work for somebody. With that in mind, we try to dig into everything that makes some sense.






Hi Cort,
Thank you for newsletter.
I was actually wondering if you could do a new piece on the link between Fibromyalgia (possibly, ME/CFS) and adult ADHD?
I have been a suffer for decades and only recently was it suggested to me that I should consider being tested for ADHD.
After a little research I was able to come across quite a lot of information.
I have been seeing my rheumatologist for over a decade but never did it even come up in any if the multitude of visits I attended.
As the correlation seems to be very high, and diagnosis for Fibromyalgia relies on the exclusion of other diseases, why isn’t it standard practice to test fir ADHD.
We seem to be great at masking it!
It would be interesting to read about the experience of anyone who has tried the medication.
I would love to do that. We have a 2018 blog on it – https://www.healthrising.org/blog/2018/01/20/adhd-attention-deficit-hyperactivity-disorder-fibromyalgia/ – but nothing since then. I think its a fascinating connection and I will look around to see if anything new has popped up.
We are going to do another blog on stimulants as well.
Gina, if you have been battling ME/CFS, Fibro, or CIRS, by now you probably have developed ADHD. It is part of the cognitive decline seen in all three conditions. I used to be a Microbiologist at the University of California. But by age 28, I could not focus well enough to work in a lab. I had slowly developed “Fiibrofog”. The Fibrofog has only worsened the past 30 years.
Does anyone know whether Mirica can be obtained in the UK?
There seem to be a variety of PEA/LUT products on Amazon. You can probably find one if you look
Thank you. I found one in particular from New Zealand manufacturer that I want to try, avail on Amazon UK. It combines both PEA and Luteolin.
My understanding is that an important component of PEA/LUT preparations is that they be ultra-micronized for sublingual use, so the PEA crosses the BBB. I just took my first sachet of Glialia® and it is really a LOT of microgranules to have under your tongue so maybe dividing it into two doses a day would work better.
You can get it from their website (https://youngnutra.com/collections) shipping costs £15 though.
Thank you for your reply. I went to their website and read all the info on their products. It was helpful as a guide. I decided to purchas a similar product made in New Zealand that is sold on Amazon in the UK, and delivery free with my Prime account as well as a discount if you order it on a subscription with repeat deliveries. I do hope I will see results as I need to cut back on over the counter meds I take for pain.
Do you mind sharing the New Zealand brand you found please?
I have ME/CFS by way of long COVID. My functional medicine doc had me try PEA several months back for a few months, but I had no improvement. We’re all so different though; I hope it will help some.
PEA can be quite costly. But another supplement of promise that works on gaba A but also inflammation, antiviral and anti bacterial potential is both Chinese and American scullcap. It can take repeated dosing over time for benefits to acrue.
I have found PEA, along with LDN, has helped reduce my brain fog and neuropathy symptoms. I take a micronized PEA in 600 mg capsules that is available in Canada. Recommended by my ND and ME Specialist MD.
I tried PEA after having read some articles that it could help with microglial inflammation. I found that it did help a little with brain fog. Not a cure, but I’m going to continue (every little bit helps!).
PEA is one of the supplements that I take because it seems like a good idea, given that it may reduce mast cell activation. The only negative I’ve observed is to my pocketbook. Unfortunately, I’m not conscious of any benefit either.
I tied PEA for pain but it just made the pain worse and I did try it twice just to make sure and did try to do the low and slow approach. I still have the bottle in the cupboard so may give it another go just in case. Trouble is we are all so different, what works for one doesn’t work for another.
Thank you Cort for addressing the issue of neuropsychological testing !
This seems to be tricky indeed. In a very thorough study of LongCovid patients ((https://www.nature.com/articles/s41380-022-01632-5)) the only test that really showed a difference and correlated with their neuroimaging findings was a test called “Rey-Osterrieth Complex Figure Test (ROCF) Copy”:
“We observed significant cognitive impairment only in the ROCF, a drawing task test used to assess visuospatial abilities, executive functions and memory.”
This is interesting because so many LC and ME/CFS patients report changes in the coordination between vision and spatial orientation and “doing things”.
So this may really be a test to include in studies.
“The maintained attention assessment in patients affected by Myalgic encephalomyelitis/chronic fatigue syndrome: a reliable biomarker?” – 2021
https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-021-03153-1
“In spite of the plethora of symptoms showed usually by these patients often neurological manifestations are specially relevant and among them cognitive disorders have been described playing a central role [7, 8]. A meta-analysis concluded that the cognitive deficit is a primary finding independently of emotional state of patients. The deficit depends mainly on the compromise of attention, memory and reaction time. There isn´t motor deficit, vocabulary, reasoning and global functioning [9].”
“Regarding maintained attention test, there were significant statistically differences in the Global Index of Attention and Perception (GIAP) between CFS/ME and control groups, but not among women and men with the syndrome. Attention records were mainly low (52%), very low (18%) and not evaluable (6%), this last by abandonment due to very high fatigability experimented by some sick. ”
“Fatigue evaluation show highly significant differences between both groups in any situation (Table 1). Comparing the evolution of this fatigability after the administration of the Toulouse-Piéron test is remarkable the highly significant differences (p < 0.001) reported by CFS/EM- group (women as well as men) stand out compared to the no difference reported by the control group (Table 2).
"Perception of effort referred by CFS/EM patients was significantly higher than for control participants (p < 0.001). In addition, comparing gender in that group women showed higher levels than men (p < 0.05; Table 1).
"Some patients (N = 15) provided a psychiatric diagnosis of reactive depression. It should be noted that, there were not differences in GIAP between these patients and the rest (N = 69; p = 0.116)."
"General cognition remains preserved in most patients, only a small group of them shows a significant mild cognitive impairment. Maintained attention is clearly deficient, showing a marked fatigability after the Toulouse-Piéron test. The effort was perceived as very hard by both gender, but higher by women."
@feralboy
Yes, precisely. My POTS was hypoglycemia.
Something to be aware of: stress hormones can prevent blood glucose levels from dropping low. The heart rate and temperature provide more info, and your own symptoms. Measure any parameter when you are symptomatic. Fasting blood glucose only tells you what fasting blood glucose is.
Maybe because the people doing the POTS investigation are not endocrinologist, blood glucose isnnot measured in the tilt table test. They do measure catecholamimes, if norepinephrene shoots up too high = hyperPOTS diagnosis.
Though if one’s water is shifting from blood into tissues/interstitial space when one comes to standing [I would have had to pee within minutes of being upright], I’m not sure what are they measuring in that test: have hormone levels in the blood changed or is it the blood volume that has changed? There is the problem of osmolality vs osmolarity in all blood tests done clinically
Though I don’t know that most endocrinologists today have the necessary knowledge either: I think of those who get into a severe state/losing weight too quickly/not being able to eat, needing tubes feeding them to keep them alive etc, are most likely suffering from the wasting disease – diabetes. Wikipedia has a decent history of diabetes; it’s only recently that it has come to signify high blood glucose levels
Now how to get yerself out the pickle? For me, getting my D levels up was like night and day, from one day to the next. Ray Peat’s work gave me the framework for how to understand my particular nutritional [macro and micro] and hormonal needs. My ‘ME/CFS’ has actually been pellagra. Everyone has their needs to figure out.
The two very specific things usually mentioned as affected in ME/CFS cognitive function are word recall and simple maths problem solving.
This is pretty easy to test.
Did you know that the first two very specific symptoms that are appear when glucose starts dropping are word recall and solving simple maths problems?
In fact, this is how they came up with the diagnostic guidelines for less than 70 mg/dL, because that is when these two symptoms appear, before the other more physical ones.
There is a site that documented the conversations had by thebdidderent people involved in setting the guidelines. I don’t have access to it now to link it here.
They’ve even came up with the term neuroglycopenia… because they don’t understand what blood glucose really represents/means.
As in your blood levels are fine, but your brain doesn’t have enough glucose, and thus, energy.
It’s really not rocket science…
Hey M,
I’m not sure what you’re implying – that ME/CFS brain fog or dysfunction is related to blood glucose, or CSF glucose, or poor neuronal glucose metabolism?
Those ideas are all intriguing. I looked up neuroglycopenia and the symptoms surely do include facets of what I experience:
“…a slowing of thought processes and a gradual blunting of consciousness with a retention of awareness, although amnesia for the episode is common…malaise, feeling detached from the environment, restlessness associated with hunger, nervousness that may lead to panic…insidious changes in personality, memory, and behavior that may be misconstrued as dementia”
Now I want to order a blood glucose meter.
It’s 2024. I recently Learned that cancer patients receiving chemo or radio theraoy have something they term ‘chemo/radio brain’
There is a doctor that advocatea trying out a grain-free diet to see if that is causing the Alzeheimer and other cognitive degeneration. For people whom this works, they have something called ‘grain brain’
People with homocystinuria, whom have problems with certain proteins (but really, who doesn’t ..?) have something called ‘protein brain’.
Guess what they all are ascribed too? Mental fog and slowness, problems recalling names and words.
Brain fog.
There’s also cancer treatment fatigue – a fatigue different from all fatigues because even if you rested you don’t feel rested…
Many patients with chronic and ‘auto-immune’ diseases describe waking up with the feeling that a truck drove them over.
It’s too bad doctors think they are each distinct from each other, each caused by their own particular diagnosis.
I wonder if you’ll get this message as it’s now Feb. 2024. I was shocked to read this — I have been hypoglycemic since forever and have never known why! My doctors just ignore it because they don’t know why. I don’t have any specialists anymore except an endo. I’m a good researcher, but if you any direction for me I would appreciate it so much!
Hi Kristine – I’m happy Cort and site friends set up the email ping-back system.
“When sugar isn’t available in the diet, stored glycogen will provide some glucose (usually for a few hours, up to a day), but as that is depleted, protein will be metabolized to provide sugar. If protein is eaten without carbohydrate, it will stimulate insulin secretion, lowering blood sugar and activating the stress response, leading to the secretion of adrenalin, cortisol, growth hormone, prolactin, and other hormones. The adrenalin will mobilize glycogen from the liver, and (along with other hormones) will mobilize fatty acids, mainly from fat cells. Cortisol will activate the conversion of protein to amino acids, and then to fat and sugar, for use as energy.”
“The amount of glucose in liver cells regulates the enzyme that converts T4 to T3. This means that hypoglycemia or diabetes (in which glucose doesn’t enter cells efficiently) will cause hypothyroidism, when T4 can’t be converted into T3. When a person is fasting, at first the liver’s glycogen stores will provide glucose to maintain T3 production. When the glycogen is depleted, the body resorts to the dissolution of tissue to provide energy. The mobilized fatty acids interfere with the use of glucose, and certain amino acids suppress the thyroid gland. Eating carbohydrate (especially fruits) can allow the liver to resume its production of T3.”
Many free articles on his site and books on the Internet Free Archive. “Nutrition for Women” is one.
Your doctors are ignorant and incompetent.
They put your health in danger, creating a lot of needless suffering and loss of quality of life.
Thank you so much for your response! You are right; my doctors are rather uneducated in this arena. I have researched things about my various conditions and corrected at least two of them on more than one occasion. I believe my primary has a love/hate relationship with me. We get along well, however, and she knows that I research everything that comes my way:) Right at this moment I’m in my second LBS attack of the day and must go eat right now before I …Yep, I just had to eat glucose tablets, two eggs and a GF waffle with peanut butter. I was shaking violently and my boyfriend had to help. I’m used to living in Minneapolis and/or Naples, FL where there is excellent medical care, but now I live in a more rural area and can’t afford to travel to see the specialists I need. I will look up “Nutrition for Women.” I will also send your comment to my primary and endo if you think that may help. As I said, my docs have had no comment on my hypoglycemia, if they even believe me. Again, thank you. I need all the help I can get right now;)
You can do this on your own. I did, and many others have and continue to.
Doctors usually don’t like to have their authority questioned. One doesn’t need the added stress of dealing with the medical system when one is already very sick. ‘Treatment’ can, and usually does, cause further harm.
I also had such crashes of low blood sugar that I couldn’t feed myself and needed someone else to do it for me.
Note the snippet I included above, regarding leucine triggering more insulin secretion, and thus lowering blood sugar.
What you ate to bring your blood sugar up was full of leucine, and very little sugar/carbs.
Fruits are an excellent source of sugar.
Also note in the snippet that if you don’t give your body sugar it will make it first from your protein, and then dissolve your muscles and tissues to provide it.
You can start stabilizing your blood sugar and lowering your stress hormomes by what you eat. You may need additional things. I had low levels of D, and bringing it up helped stabilize my sugar.
https://raypeat.com/articles/articles/sugar-issues.shtml
Yes, I have found that Amazon sells PEA – I just have to find the right one. Your information is like gold. I just ate breakfast for the first time in years; it had always caused me to be more hungry before lunch than I cared to be. I mixed VERY low-sugar Greek yogurt with almond milk, almond creamer, homemade granola (oatmeal, walnuts, maple syrup… I don’t remember what else she puts in), a few dark chocolate chips and a banana. I’m not a big fruit eater but I do eat kiwi fruit for digestion and bananas. I could stomach apples if I cook them but I’ve read they are not good for me. Maybe that is “the cure being worse than the medicine,” ha, ha! Or however that saying goes! My D level is fine but I take D with K2-Mk7. We have a lot of dark days – a lot! I will study leucine and read your link. No need to contact my doctors as one wouldn’t answer and my primary would say that this was beyond her expertise.
Thank you – more than I can say!
I know that Cort would give you my email address — I am also pretty sure I am asking too much. I am lost in your explanations even though I’m a good researcher. Please…just ignore me if this is too much. And, I thank you so much for your info!
Krissy Anderson
It’s all in his articles and books. There are radio shows / podcasrs that had him as guests for years / episodes tol.
Ray Peat
Saved my life
The ‘ME/CFS’ hellhole
Thanks!
I think some of us know to be careful with stimulants.
I have become hypersensitive to stimulants like coffee, cocoa or alcohol. They often make me much more functional, and this can be nice to feel more “normal” for a time or for getting things done. But same as an adrenaline high, they will mask exertional limits and carry me over them, resulting in a crash, and before that, hyperarousal of the nervous system with sleeplessness. (I suspect some connection to adrenal function, as all these substances were listed as adrenal stimulants in a book about adrenal fatigue). To me they seem to work like medication-aided pushing ;), i.e. make the candle burn to its end faster, so I remain doubtful that stimulants are a general solution to ME/CFS.
By the way, I recently tried Ativan and suspect that via improving my focus, concentration and noise shielding, it possibly comes with a similar risk of overexertion.
In a study with stimulants, it would be both important to look at PEM episodes following stimulation and also at long-term experiences (in my own experience, for example with mild ME/CFS, it can still be possible to keep pushing oneself over a consecutive period of say three weeks by remaining in a high state of stress/arousal of the nervous system).
JR, if I did not have access to Amphetamines, I would be unemployed!!!
I am glad to hear Amphetamines help you! May I ask what they do for you?
Maybe my comment on “stimulants” was too general, because I would think every stimulant is the same. I once tried ADHD medication and it did calm me down and helped with focus, though I still felt it might make me overexert. I would very much like to try it again, because if it reduces stress, this will free up some energy and maybe with some more attention to pacing it could make a positive difference! Unfortunately, prescriptions of Methylphenidate are highly regulated in Germany and so far I did not have the energy to undergo the comprehensive ADHD screening required ;-). I think offlabel prescription is theoretically possible but very improbable in practice because doctors are vaguely afraid of getting into trouble or don’t want to have a lot of extra work justifying their offlabel prescription. But thanks for reminding me of this – maybe I should give this ADHD diagnosis another go.
Sorry, typo in previous post – I would think that not every stimulant is the same.
JR, Fortunately, I have never had a “serious” problem with post- exertional malaise. My physicians guess that I fit into the “Fibromyalgia or CIRS camp” more than ME/CFS. Personally, after tens of thousands of hours of research, I believe all three are caused by inflammation in the hippocampus. They are not certain how Modafinil works, but most Neurologists start their fatigue patients on this med. They can move to something like Adderall if need be. But, you need to take long “therapeutic holidays”, or Amphetamines like Adderall will cause a crash. In the book “Blitzed”, the author (a Neurologist) speculates the real reason Guderian, von Manstein, and Rommel’s tank crews did not make it to Dunkirk in time. In the case of Heinz Guderian, his troops had not slept for three days due to amphetamines, and were now experiencing “the crash”. The few Wehrmacht tankers/dive bombers/infantry that made it through the 5 years following the “Battle of France”, felt that the high doses of amphetamines did damage to their central nervous system!!!
JR, I just further digested your comments: “Methylphenidate is highly regulated in Germany”, and “it is an off label use of an ADHD drug”. Methylphenidate is highly regulated here too, but it one of the most employed arrows in the chronic fatigue Docs black bag. (Same with Modafinil and LDN. You need to try these meds!) What is considered seriously “off label’ here, that some chronic fatigue Docs are wary of prescribing is Xyrem. I have a close friend who can not get restorative sleep without Xyrem. She does NOT have Narcolepsy. So, the Xyrem is being used “off label” by her ME/CFS Neurologist. But, she can work now, and enjoy her family. Your comments about the German government’s control of medications scares me to death. We MUST stop this mindset from migrating here, and only permit our amazingly dedicated and educated physicians to make these decisions. I have news for the heavy handed lawyers in DC: “Your law degree is a glorified masters degree in “arguing”. That’s why we call you “sharks”. Our physicians are vastly more knowledgeable in their extremely complex craft than the manipulative “sharks”. Most attorneys I know would never score high enough on the MCAT to get in to Med School, let alone finish an Internal Medicine Residency at one of our teaching hospitals. Unfortunately, we all still complain about our Docs too much. I plead guilty!!!
Thank you for taking the time to reply! How interesting what you write.
To avoid a misunderstanding, I’d like to clear up some things about what you call government control of medications, also indulging in some interesting history:
Metylphenidate in Germany is in a class of drugs regulated by the narcotics law that unfortunately are also being misued as recreational drugs/narcotics or have a high addictive potential such as benzodiazepines or opioids.
The initial German narcotics law was introduced in 1929 as a condition of the 1919 WW1 Versailles Peace Treaty that Germany ratify the US-initiated 1912 international opium convention. If I remember a historical programme right, it was also introduced in reaction to the then generous use of narcotics such as opium, heroine and cocaine as curatives. After this law, they could still be used as medications but prescription only. Today’s narcotics law prohibits trading of true narcotics, but still regulates the prescription of narcotics that also have therapeutic uses.
It probably did not help the case of methylphenidate (Ritalin) that acording to Wikipedia, it was named after a tennis player (Marguerite = Rita) who used it for doping ;D.
I once called up the responsible office and they explained to me that besides its approved indication for ADHD, methylphenidate can still be prescribed off-label with reasoning provided by GP. But my GP for example is spooked by anything narcotics and has so little time for extra work that she prefers not to do any narcotics prescriptions at all.
There are also some medications under this law (such as benzodiazepines) which my GP cannot bill under the free healthcare system, but I think a speciality doctor can, or can be still prescribed by my GP as a private prescription.
Now I just found that Ritalin abuse is also classified/regulated by the controlled substances law of the US. So why is it easier to prescribe in the US? So I guess that details of regulation differ, or maybe because 90% of Germans are covered by the public free healthcare insurance system whose uniform billing rules probably make off-label prescriptions more the exception than the rule, but also ensure direct implementation of narcotics regulations.
So although German narcotics law unfortunately results in a barrier to medical off-label uses of methylphenidate in Germany, it is also the reason why there is no opioid crisis in Germany.
I personally wish off-label was more established here as you say.
For German readers: Modafinil (a stimulant) mentioned by Rich is not BtM (narcotics) regulated any more since 2008.
I also tried a stimulant, first Coffee and then Ritalin for a while. I had a similar response to what you described. It felt good to be able to focus better. However, it triggered overactive digestion and gave me a feeling of being ‘on edge’.
I also think being understimulated can cause a feeling of malaise. It can cause me to just not want to do anything, which affects my mood.
These days, I try to regulate my level of stimulation through activities. Lately, I’ve allowed myself to do 30 min of a fun project in Excel once or twice a day to stimulate my mind. Other things that have been good stimulation were a practice of writing.
It’s a fine balance.
We have a stadium full of ME/CFS and MS patients who are certain that LDN helps with cognition by supposedly reducing microglial inflammation. I believe that Dr. Younger is correct in his hypothesis concerning LDN. ANYTHING that will reduce microglial inflammation should be studied intensely. The LDN we are purchasing from compounding pharmacies is a racemic mixture. The NIH would not fund Dr. Younger’s plan to remove the inactive mirror image in LDN, and then administer the active mirror image to patients. Any Chem grad student could purify the LDN, but funding is needed for patient trials. These decisions by the NIH are almost criminal. If they will not fund sensible LDN research, I doubt anything will come of PEA. But, if PEA does, indeed, reduce microglial inflammation, everyone should give it a shot.
I too read about it and tried Mirica ( original). I can’t say I noticed a difference. On further research I realized that in studies a
micronized or ultra micronized form ( better absorbed) of PEA was used. I just restarted with a powdered form of ultra micronized PEA from Elavation Turpenes . I had contacted Young Nutraceuticals (Mirica) and they confirmed their product was not micronized. However the new advanced form of Mirica contains Levegen with Luteolin a novel form made with Lipisperse technology for increased absorption.
did the PEA from Elavation Turpenes help you? with what condition if i may ask? ME/cfs, long covid, FM, ..? what doses is needed and how much , how often a day? Are you takng it for a long time before it worked? before, after meals? thanks a lot!
I just started 3 weeks ago….. The daily dose is I/4teaspoon. Because I’m supplement sensitive I started with sprinkles …now I’m up to 1/8 tsp. I’m going to give it 3 months as least. It can be taken 1 to 3 times a day as directed by a physician…..with plenty of water.. I have severe CFS , orthostatic intolerance , and severe CNS symptoms . I feel like my body/ brain is on fire. I mentioned it to my functional doctor and he’s all in !
Hi Carolyn- I went to
https://www.elevationterpenes.com/products/ultra-micronized-palmitoylethanolamide-powder-99-pure-lab-tested-pea
They are listing the PEA product as “2021 New Stock”. It’s shown as sold out. That 2021 as new threw me a little.
Can you confirm this is what you purchased?
Are you having any better outcome with this product?
Thanks for sharing your experience.
Hi Birdie…. I just started 3weeks ago at half the dose. I have to go slow with supplements. I’m going to give it a good 3 months to see if it helps.
Yes…that’s the correct product. I hope it’s helpful.
Hi Carolyn,
How did you go with micronised PEA?
That’s the right thing. It may be helping a bit but it’s hard to tell which supplement to give credit to !
Thank you, Cort for reporting on something new to try. Neuroinflammation and mast cell disorder have always been core symptoms for me. I tried LDN, but it made me horribly dizzy even at tiny doses. I ordered PEA this morning and will give it a try. I also reordered cell signaling factors from The Cheney Institute which holds the patent to sell these. I was helped a great deal by CSFs although I know others were not.
Betty, you probably needed to start on a “super low dose” of LDN (a grain of sand). Then, over many months slowly increase the dosage. Many folks have problems with LDN “initially”.
Betty, unfortunately, the compounding pharmacy will not “tablet” a “super low dose” like .01mg. You would need to grind a 1mg tablet yourself. Read the book “LDN’, and give it a year to 18 months. Opioid abusers are usually administered 50mg. That would kill me. I’m serious! I had to start at .05 mg before bed, and then worked up to 4.5 milligrams over 18 months. Yes, i felt strange, but I had read the book. Read some of Dr.Younger’s papers from Stanford, and now The University of Alabama. He is a brilliant Ph.D Neurobiologist. He is now using his skills to study inflammation in the PET scans of ME/CFS patients. Glad I’m on LDN.
I have tried LDN many ways. At first I did what they said and took 1.5 mg. It made all my symptoms worse and I felt terrible. So I opened up the capsule and used, as you say, a sprinkle. I worked my way up to 3 mg over 3 months and still didn’t feel good. It really bothered my stomach. So I got my compounding pharmacist to make a topical creme with it. That worked and I went up to 6mg which works amazingly well for me, taken at bedtime. Until I started developing a rash wherever I rubbed in the topical. Rats. I was then alerted to the possibility that I was reacting to the excipients in the creme.
Then I read somewhere that you can get the 50mg tablets (cheap!) and grind them up in a mortar and pestle, dilute the powder with distilled water in an amount calculated to give you a certain dose, and let it sit to settle out. You get a layer of white crud on the bottom and your water on top. Naltrexone is water soluble, so all of it is in the water and not in the crud. Use a graduated eye dropper to draw up what you want.
But whatever you do, don’t take much to begin with! You have to go slow with this. But it’s worth it. Ask your health care provider to give you a prescription for Naltrexone 50mg tablets.
I take two 50mg tablets, grind them up, dilute with 16cc (16ml) of distilled water, put it into a bottle with a graduated eyedropper in it and let it sit in the fridge overnight. Then I use the dropper to measure 1cc (1ml) of the clear liquid on the top. That gives me 6mg of Naltrexone. I put it into a glass of water and drink it at bedtime and put the bottle back in the fridge. It’s a bit bitter, but if you use a whole cup of water, it is hardly noticeable. I usually get 15 doses without sucking up the white crud at the bottom into the eyedropper. If you want a different dose, you’ll have to do a bit of arithemetic, or use my recipe as a base and give yourself 1 drop to begin, keep it up for a week, then 2 drops for a week, then 3 drops, etc. Work your way up and see how you feel. It will give you wild dreams at first, but that goes away. Actually, I liked those dreams, they were so vivid!
This stuff is fundamental for me. All else goes in on top. I couldn’t live without it. If someone were to come to me and ask where to start, I would say, “Find a health care provider who will write you a prescription for Naltrexone 50mg tablets.”
For more information Go to the LDN Research Trust in the UK:
https://ldnresearchtrust.org/
PEA (PEACure) three times daily helped me with EDS pain prior to Covid. It was about as effective as ibuprofen. During Covid PEA became difficult to find, so I stopped taking it. Meanwhile, I started LDN. Eventually I ordered more PEA and found that it didn’t benefit me as much with LDN. LDN is much cheaper than PEA so I just take LDN now.
Sorry, typo in previous post – I would think that not every stimulant is the same.
I’ve tried PEA 600mg for months but can’t say I’ve noticed anything significantly different since taking it. But I’ve had some pretty serious PEMs these last months, so maybe that may have been masking things. I’ll keep taking it a while longer, just because of its potential benefit (over taking nothing).
Btw the product I use (NerixX) is a combination product with alpha lipoic acid. Some extra anti-oxidant didn’t seem like too bad an idea to me.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8157570/
This is a pretty good summary of PEA effects. Pretty interesting!
Long ago my daughter (CFS) tried PEA. Just from a regular supplement company–no other ingredients. She also was using prescribed antidepressants as I recall. PEA did have some effect on her brain, but she didn’t like that effect. Might have been different if she’d started low and slow or hadn’t had other meds that may have complicated it. I think I tried it first and thought it would be safe to experiment with. No real effect on me (not as bad CFS) as I recall. I definitely think her reaction had to do with cannabinoid receptors.
“Palmitoylethanolamide for sleep disturbance. A double-blind, randomised, placebo-controlled interventional study”
https://sleep.biomedcentral.com/articles/10.1186/s41606-021-00065-3
“Results:
“At week 8, PEA supplementation reduced sleep onset latency, time to feel completely awake and improved cognition on waking. After 8 weeks, both groups improved their sleep quality and quantity scores similarly. There was no difference between groups at baseline or week 8 for sleep quantity or quality as measured from actigraphy or sleep diaries.
“Conclusion:
“These findings support PEA as a potential sleeping aid capable of reducing sleep onset time and improving cognition on waking.”
Huh?! There was no difference between groups at baseline or week 8, yet the study supports its use as a sleep aid?
Metagenics has a hemp and PEA combo that my formerly ME/CFS and now FM 20 y/o daughter took for a couple of years, on the advice of her functional medicine doc. She gradually reduced her PEM symptoms over that same period (primarily bedbound for about 3 yrs prior) but hard to know if the PEA was the helper or some of her other myriad supplements and meds. In any case she decided to stop that supplement and her health seems to be maintaining ok.
I really like PEA, but it doesn’t do a thing for my brain fog. I use it for pain relief, but you have to take a lot of it and it has to be ultra-micronized. I take 800mg three times a day with meals. I have had no side effects. It works on the ACE-2 sites like CBD. Look for it in bulk powder and put it into capsules yourself. Try e-bay. I think capsules of PEA should be in everyone’s medicine cabinet for pain instead of tylenol or asprin.
But don’t take PEA if you are taking THC. They compete for the ACE-2 sites and you’ll feel really whacked out for hours afterwards. No problem with CBD, though.
The thing that works best for my brain fog is NMN (nicotinamide mononeucleotide) which is an anti-senescent. I take 1 gram of the powder in my tea every morning. No side effects. Less brain fog. More energy but does not cause me to over-exert.
Thanks for the info.
Sorry, I should have labelled myself “Ann1”
You can buy PEA on Amazon in the UK here: https://www.amazon.co.uk/Palmitoylethanolamide-Capsules-Certificate-Analysis-Supplement/dp/B09N1P1GXK/ref=sr_1_5?crid=3KLJFTW08ZA5X&keywords=PEA-LUT&qid=1671163250&sprefix=pea-lut%2Caps%2C81&sr=8-5
I’ve just ordered some, it will be interesting to see if it works, for £26/3 month’s supply, it’s worth the risk!
When I was involved in some ME research at University College London, they were very interested to find out I’d had Chicken Pox 3 times (it’s a type of herpes infection), only 0.1% of the population have it more than once.
I had bought PEA from Life Extension before reading this article and took the 600 mg dose since a few days. No effects but no side effects. It certainly is not micronized, so I’ll try again.
Thera are many research papers on neuroinflammation and PEA so it looks really interesting and I’ ll try different forms (Levagen, Myrica etc).
I would be interested in exchanging experiences with others trying it. How do we organize ourselves as a forum if interested ? Cort, could you help in this maybe ?
came down with a mystery illness in1979,,,,at 37 years of age,,,,,,by mid eighties i believed it to be me/cfs,,,, ..i strongly but generally believe cfs hits females and m,e, hits men…..i have tried and experimented with every regime known to mankind…nothing but nothing helps …i am now 82 yo ,,,,,me/cfs with age is getting impossible……….sorry i cant be of more help to others kev
This is a fantastic deep dive into the potential of PEA and luteolin for Long COVID, ME/CFS, and fibromyalgia! The detailed breakdown of their anti-inflammatory and neuroprotective effects is truly insightful. It’s great to see emerging research on natural compounds that may offer relief. Thanks for sharing such valuable information!
Thank you for this incredibly informative and well-researched post! I really appreciate how you broke down the science behind PEA and luteolin in such an understandable way. It’s encouraging to see potential treatments being explored for complex conditions like Long COVID, ME/CFS, and fibromyalgia. The personal insights and the connection to real-world patient experiences really add depth. Looking forward to more updates as research progresses!
Thank you for this insightful and well-researched article! I really appreciate how clearly you explained the potential role of PEA in addressing symptoms related to Long COVID, ME/CFS, and fibromyalgia. It’s encouraging to see emerging options explored with both scientific context and practical perspectives. Blogs like this are invaluable for those of us looking to better understand complex conditions and the ongoing research around them.
Llevo 21 años con sfc/en después de citomegalovirus .. estoy con pregabalina hace dos años 75mg.. estoy dejando.. quiero tomar algo.. natural.. PEA.. voy a probar.. primero melena de león.. o los dos juntos?.. tengo FM.. también.. dolicomegacolon.. y TAG.. la ansiedad creo me la dió los antidepresivos.. tengo terreno antidepresivos desde joven.. gracias
Google translate
I have been living with CFS/ME for 21 years after cytomegalovirus.. I have been taking pregabalin for two years at 75mg.. I am tapering off.. I want to take something.. natural.. PEA.. I am going to try.. first lion’s mane.. or both together?.. I also have FM.. dolichomesocolon.. and TAG.. I think the anxiety was caused by the antidepressants.. I have a history of antidepressants since I was young.. thank you.
New Translations Available
English
I have been living with CFS/ME for 21 years after cytomegalovirus.. I have been taking pregabalin for two years at 75mg.. I am tapering off.. I want to take something.. natural.. PEA.. I am going to try.. first lion’s mane.. or both together?.. I also have FM.. dolichomesocolon.. and TAG.. I think the anxiety was caused by the antidepressants.. I have a history of antidepressants since I was young.. thank you.