

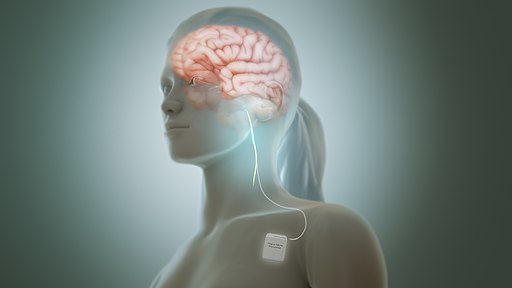
Vagus nerve stimulation shows great promise…When will that promise be fulfilled? (Image by Manu5 – Wikimedia Commons)
If any treatment has promise, vagus nerve stimulation (VNS) does. Through its stimulation of the rest/digest system (the parasympathetic nervous system (PNS)), VNS has the potential to tamp down the fight/flight system that seems to be raging in chronic fatigue syndrome (ME/CFS), fibromyalgia, postural orthostatic tachycardia syndrome (POTS), and quite a few other diseases.
Speaking personally, there are not many modes I’d like to more consistently get into than rest/digest mode. An amped-up flight/fight system and a tamped-down rest/digest system could be affecting everything from( blood flows and coagulation to the immune system, to the gut, and sleep.
Sleep
Take just one major concern – sleep. Numerous studies have found reduced parasympathetic nervous system activity (rest/digest) during sleep. Even the CDC – which was not, back then, exactly known for validating findings – found autonomic hypervigilance (increased HR, reduced HRV, higher norepinephrine, as well as lower aldosterone levels) during sleep in ME/CFS.
“the presence of increased HR and reduced HRV in CFS during sleep coupled with higher norepinephrine levels and lower plasma aldosterone suggest a state of sympathetic ANS predominance and neuroendocrine alterations.”
That was back in 2007! Since then not only have the Aussies (and others) documented those findings but the Aussies have been unable to find anything else that could explain the poor, unrefreshing sleep in ME/CFS.
The 2018 Finnish study, and the 2010, 2011, and 2020 Aussie studies all highlighted the low HRV (sympathetic nervous system dominance) found in ME/CFS during sleep. Similar findings showed up in fibromyalgia in 1998, 2009, 2011, and 2013. It was remarkable to see two studies – one in ME/CFS and one in fibromyalgia – pour through a maze of sleep findings only to conclude that reduced heart rate variability (i.e. reduced vagus nerve, or parasympathetic nervous system activity) was the main factor behind the poor sleep in these diseases.
In 2019, Boissoneault and Staud produced a nice “bifecta” when they showed that lower heart rate variability (read lower parasympathetic nervous activity), in conjunction with lower blood flows to the brain, predicted how fatigued people with ME/CFS were.
Doesn’t this result say it all?
“Autonomic hypervigilance during the deeper, recuperative stages of sleep is associated with poor quality sleep and self-reported wellbeing.”
How could a hypervigilant autonomic nervous system (i.e. an amped-up fight/flight response) during deep sleep be anything but bad? Note that you could be having plenty of slow wave or deep sleep, but if it’s poor deep sleep, it’s probably not doing that much good.
What do we lose by not having good deep sleep? Deep sleep is when the body does much of its repair work. Your immune system rebalances itself, your tissues repair themselves, your cells regenerate, your metabolism readies itself for the next day, and your brain detoxifies itself. It’s no wonder that you might feel “unrefreshed” – a kind word for feeling like you haven’t slept at all – when you wake up in the morning feeling like you’ve been pounded by a 2×4.
Some things (meditation, Tai Chi, exercise in FM) have been shown to improve parasympathetic nervous system functioning, but not everyone wants to take the time to give these a shot and not everyone will benefit, as well. Low-dose trazodone and doxepin elixir can help keep a lid on the fight/fight response during sleep as well, but like any drugs, they don’t help everyone.
We clearly need better options. How does clipping a small electrode to your ear sound?
Vagus Nerve Stimulation
Vagus nerve stimulation presents an enticing possibility. No need to take drugs or engage in hours of meditative activity (meditating, Tai chi): simply attach a small electrode to your ear and let the device do its work. (Surgical implantation of VNS devices is used in epilepsy and worked great in a person with fibromyalgia but is not readily available.)
The transdermal or non-invasive device provides a low-voltage current to a vagus nerve ending in the outer ear. Because 80% of the vagal nerve fibers found in the ear go to the brain, transdermal vagus nerve stimulation mainly affects the brain.
The problem has been that VNS’s promise has not nearly been met. Right now, non-invasive VNS stimulation is less like a medically informed solution than a venture into the wild west of medical devices.
How long to wear one, where to wear one, what intensity of electronic stimulation to use, which device to try – it’s all a mystery, and as we all know – dose-response is a pretty critical factor. Without the right dose (the right amount of electrical stimulation for the right duration over the right period), you’re not going to get the result.
Things are starting to get worked out, though, and the POTS crowd is leading the way. At the 2022 IACFS/ME International Conference, Lauren Stiles – the leader of Dysautonomia International – now in its 10th year (that went fast!) had some good news.
After noting that VNS had helped her a lot, Stiles, who is usually quite conservative in her statements, stated that she believes VNS is going to be a big deal in both POTS and ME/CFS. She believes its ability to reduce inflammation is going to be key.
Some people have found it to be very effective. Others, of course, have not.
The problem has been in figuring how to use the device properly. A step forward was taken in that problem recently with a paper by Vanderbilt and University of Milan researchers, “Transdermal auricular vagus stimulation for the treatment of postural tachycardia syndrome“. The paper addressed “crucial methodological aspects of tVNS”.
The authors focused on studies in a variety of diseases that provided information on the device’s effects on heart rate, blood pressure, heart rate variability, and/or vagal, sympathetic, and inflammatory markers.
Results
Potentially effective
The first conclusion of the overview was that transdermal (non-invasive) vagus nerve stimulation can work. In general, the studies showed that it can lower the heart rate (heart rates are high during sleep in ME/CFS/FM), improve symptoms, and reduce markers of inflammation.
Then it was onto the methodological conclusions.
Using Vagus Nerve Stimulation
The vagus nerve connects the immune system to the brain at the brainstem (Image by Nadezdha fr. Wikimedia Commons)
Right ear only – with the right side of the brain governing “neurocardiovascular-sympathetic interactions”, it’s crucial that the device be attached to the right ear. Although the evidence isn’t as clear, it may be that the best attachment point may also be the cymba conchae rather than the tragus.
Pulse Width, Duration, Frequency
A short pulse width of 130μs produces significantly less overall activation in the human brain than longer pulse widths of 250μs and 500μs.
Several different parameters can be manipulated, making vagus nerve stimulation a complex beast. For instance, vagus nerve stimulation at 25Hz, a 250μs pulse width, with 30 seconds on/30 seconds off, for 4 hours a day is typically used to reduce the number of seizures in patients with epilepsy.
We don’t know which settings work best in POTS, ME/CFS/FM or long COVID, but a start has been made in POTS. Schiffer stimulated the right cymba conchae in 1-hour stimulation blocks, 4x’s a day for 14 days using the Nemos© device (Cerbomed, Germany).
She used a pulse width of 200μs and a squared impulse waveform which caused the stimulator to switch on and off every 30 seconds. She set the stimulation frequency at 25Hz and the electrical current was set to the highest intensity each participant could tolerate without causing discomfort.
A statistically significant reduction (P<0.05) of orthostatic intolerance and gastrointestinal symptoms, as well as a total general reduction in autonomic nervous system symptom scores (COMPASS), was found. Side effects were minimal and no one dropped out.
Four POTS studies underway should tell us more. Some studies are using the NEMOS device while others are using TENS devices that have more flexibility. Stiles said she hoped NEMOS would make a device specifically for ME/CFS/POTS.
The Schiffer study – which appears to have used a regimen similar to epilepsy – may have set an upper limit on the time needed to wear the device (4 hours/day). Stiles said other studies have found much less time was needed to produce a result.
She also said she’s very involved with the RECOVER project and quite frustrated with its unwillingness to add more autonomic neurologists.
Studies Underway
The studies underway should give us much more information on what works and what doesn’t.
POTS
- A University of Oklahoma study using the Parasym (TM) TENS device is assessing its effectiveness in reducing autoantibodies associated with POTS.
- Another University of Oklahoma study will assess the effect vagal stimulation on the tragus of the ear has on antibody suppression, inflammatory inhibition, and symptom improvement in 80 POTS patients.
- Another POTS study is combining VNS with Mestinon.
Fibromyalgia
- Sixty FM patients are participating in a 4 week Massachusetts General Hospital study that started last year.
Long COVID and ME/CFS
- David Putrino’s 6-week trial of people with long COVID who meet the criteria for ME/CFS will apply the Parasym device to the left tragus of the ear. Side effects and symptom improvement will be assessed.
Long COVID
- David Putrino’s 6-week-long placebo controlled, randomized controlled long-COVID trial going on at the Icahn School of Medicine at Mount Sinai will assess cytokines (IL-1, IL-6, IL-10), morning salivary cortisol, c-reactive protein, end-tidal CO2, and many different symptoms, including post-exertional malaise (PEM).
- The Colosat trial will assess the effects of 8 weeks of the Parsym device on pain on 20 patients with long COVID.
- A Casa Colina, California Hospital trial will assess the effects of 7 weeks of the Parasym device on 20 long-COVID patients using neuroimaging, genetics, blood biomarkers, and symptoms, with a focus on brain fog.
Conclusion
Better sleep, immune and gut functioning, etc. could all be a little electrical device away. While vagus nerve stimulation’s promise is not certainly fulfilled, for the first time real progress is being made and with a number of trials underway, we should, over the next couple of years, get a much better idea of these devices’ capabilities and how to best make them work in diseases like ME/CFS, POTS, FM and long COVID. While they don’t tend to be cheap, since they’re a one-time investment, they could be very cost-effective over time.
The results of the NIH’s SPARC (Stimulating Peripheral Activity to Improve Conditions) project will take longer to filter down to available devices, but a major goal of the project is to determine exactly which fibers at which degree of stimulation can be manipulated to produce results. SPARC envisions a world with a lot fewer drugs and many more safe and side-effect free devices that help return us to health.
BIG (Little) End-of-the-Year Drive Update
With over 260 people contributing about 25K, our end-of-the-year drive is roaring away. Thanks very much to everyone who has contributed.

Could we take back the rest and digest with VNS? Let’s hope so!
Health Rising has produced many blogs on vagus nerve stimulation, and if you know anything about it, you may know it from our pages. This blog was particularly exciting because it suggests that a page may be turning with this technology, and instead of fumbling around in the dark trying to use it (I tried it on my left ear…sigh), we should relatively soon have a better idea whether to use it, and if works, how to use it.






I have a theory about vagus nerve stimulation -I think ASMR activates the vagus nerve.
For visual ASMR responders, I think mirror neurons are activated and grooming and care videos stimulate “rest and digest” pathways that date back to cave times. Same with whispering! The only evidence I have for this is the millions of ASMR responders who say it helps them sleep and reduces anxiety, and my own experience as a visual ASMR responder. I often experience what youtube vagus nerve massage videos describe as vagus nerve response while watching ASMR. But I would love to try an electronic device as well, once they are more widely available.
Suzanne, what is ASMR?
Thank you for your observation! That has has inspired a personal exploration .. are you suggesting that there may be personal preferences as to whether it is visual ,sound ,or perhaps kinetic? swimming like it is yoga type thing? Or perhaps address it on all fronts?
This is for Lisa that asked about ASMR .. seems a powerful tool!
“ASMR videos consist of simulating sensory content such as whispering, crisp sounds, slow movements and personal attention. These varied media trigger the ASMR response in many, causing the person to relax, be comforted and even fall asleep.Oct 6, 2022”
My Chriopractor recommended this company that sells VN kit. I am ordering it for myself It is called Rezzimax Pain Tuner Pro II
There’s a Facebook that’s using the Vegas nerve stimulators. Most folks are using a TENS device with much less time then the 4 hours mentioned in the article. They are avoiding the right ear for potential heart issues. I used the right ear once for 3 minutes and I had difficulty swallowing. It was pretty freaky. The tens units are very affordable Maybe $65.
https://m.facebook.com/groups/492041135346672/
The link doesn’t work. What’s the name? I have a TENS unit, and could possibly try this if I knew how. Thanks.
The group’s called A Vagus Adventure AVA – Dawn Wiley. Hope it’s helpful to you 🙂
FB group is called a Vagus Nerve Adventure. Some Tens units are microcurrent units. Here’s a link to one
https://www.tenspros.com/intensity-micro-combo-tens-microcurrent-di9698.html?gclid=CjwKCAiAkfucBhBBEiwAFjbkr8j3IbY2Gg1kYqH0ZJauxI-6He_9jakSsn28iJ-Db0K80j3bhvyP9BoCWjkQAvD_BwE
just search ‘vagus adventure’ or ‘Dawn Wylie’ on FB and you will find it
Oh no! Important correction. We always say it’s the left ear only that we hook up to with an ear clip electrode. Even if you are describing it from someone else’s perspective (ie looking at someones face it’s the ear to your right) most people will read ‘right ear’ and think they should stimulate their right ear. This is potentially dangerous and not the ear used in the studies. Only ever use an earclip electrode with your left ear. The ear on the left side from your own perspective.
I recently started on an AlphaStim(R) device for augmenting my depression/anxiety/CPTSD and associated emotional reactivity. I also have ADHD and probably HFASD. I had to go through two training sessions and 3 mos of follow on visits with my behavioral health team to use it and gauge responsiveness and tolerance.
I potential also have FM, and am interested in VNS for this as well.
I caution individuals that using these devices without trained guidance can potentially be problematic if not dangerous since I had to be trained in how to recognize my tolerance of the generated energy delivery and adjust my device settings accordingly. I am a medical professional and needed training in the proper use of my device, so I find it concerning that some here are saying they have devices purchased online from Amazon and TENS units, etc.
Keep in mind that VNS is working on the largest nerve in the body, one which controls a great deal of our autonomic nervous system functions and with manipulation through these treatment modalities, a wrong move could create dire consequences.
That being said, I wish all who read this well and here’s to finding our way back to balanced lives and mental stability with less, if any pain, and negative impact on our qualities of life.
A tens unit is not the same thing as a micocurrent unit which is what is used in vagus nerve stimulation. Microcurrent units are very reasonable and can be bought on the internet with accessory ear clips. I bought on years ago with clips for less than a hundred.
i used a vagus nerve stimulator that i got off amazon. i used on my earlobes for about 3 weeks, but didn’t notice a change. i guess everyone is different so i dont want to discourage anyone. i have fibromyalgia and the vibrations would get painful. i am now working on nervous system regulation becuase i know i’m in chronic fight/flight/freeze from birth/childhood trauma.
The thing is Aimee is that you have no idea if the settings were correct or if the device you bought is effective for this disease. THe frequency or the pulse width or where you put it on your ear or if you put it on the right ear or maybe you didn’t use it long enough.
That’s why studies which test these devices in this spectrum of diseases are so important – we can actually learn what does and doesn’t work instead of guessing.
Yeah, thankful for the studies. I think I’m going to sit this one out until the studies tell us a bit more about benefits and risks. It’s one thing to have a good theory, another to have a decent phase 3 study on it.
In addition, Cort, it’s the **left** ear that should be used, correct? Hope the info above can be edited.
Aimee, hope you can find some relief.
As Cort’s excellent article pointed out, there is evolving understanding and recommendations
As a review (see 1 below) pointed out, due to risks in different contexts initial FDA approval was for left ear only and for 20-30Hz. The cautious approach was warranted but studies since have started to show it is not the only safe or effective location or range. Studies like (2) below seem to have safe ranges. Some settings can be very dangerous e.g. 50Hz and above, so it necessary to become informed before experimenting.
Regarding left vs right ear
Left ear is less connected to cardiovascular system (especially in dogs) and therefore unhealthy settings can cause less related harm there (but arguably in some cases also be less therapeutic)
Some reviews of studies (such as 1) have pointed out that avoidance of implanted, high frequency or high voltage of right ear stimulation due to risk, acute in dogs, does not make equal sense to generalise to taVNS with lower frequency and amps below discomfort threshold in humans
Regarding general safety
“stimulation frequencies of 50 Hz and above can cause major and irreversible damage to the vagus nerve during VNS”. As per (1) Initially this led to arbitrary 20-30Hz focus but lower frequencies have been shown to be effective too. Studies seem to have had good results between 1-25 Hz
Staying below 5mA and below pain threshold and below 2.5x sensitivity threshold with larger connectors seems to keep it safe and comfortable while still potentially effective. (2)
Some with the microcurrent approach seem to believe you can stay below 0.7 mA (might be less regulated).
Regarding it having no effect
One study (2) showed electrodes at the bottom of the earlobe to have no effect.
The cymba and cavum at and above the ear center are shown to have impact.
Papers
1) “Critical Review of Transcutaneous Vagus Nerve Stimulation: Challenges for Translation to Clinical Practice”
https://www.frontiersin.org/articles/10.3389/fnins.2020.00284/full
2) “Evaluation of different vagus nerve stimulation anatomical
targets in the ear by vagus evoked potential responses”
https://www.researchgate.net/publication/354770095_Evaluation_of_different_vagus_nerve_stimulation_anatomical_targets_in_the_ear_by_vagus_evoked_potential_responses
I tried this also with a tens unit. Did nothing for me. I have fibromyalgia.
I have been using a tns machine for tVNS 3 times daily for nearly a year to the left tragus. Apart from the benefit to my gut mobility which happened within a day or 2, I feel that other benefits have taken longer to develop. So some of the short trials might not see the full benefits. I have seen various positive changes but of course thanks to the vagaries of ME and experimenting with other things, I can’t be sure how much can be credited to tVNS but I plan to continue.
i know several people who got tinitus from it. before i did know that, i bought a vagus nerve tens and luckilly there where instruction warning with it. no metal implant in the boddy! i am operated on my neck with much metal. i asked around because some others do not give this warning in 25% ME group and ones brother, who was with metal operated on his leg (knie i thought) might even not use it from the clinic! so please, be all warned… no metal implants and you can (not everyboddy ofcource but i know several people) got tinitus of it and that you really do not want to have on top. i was verry disapointed but now oh so glad!
I was specifically told to only use the left ear (my left) and using the right could cause heart issues.
Either way it did nothing, tried a whole range of frequencies and locations.
Keen to know what others have tried
Hello,
I’ve also used a VNS device on the left ear for about 1,5month. The earclip was fastened on the tragus. 45 min per day, 25Hz & 250 microseconds. It didn’t do a thing. I have Me-CFS and fibromyalgia.
I am glad that researchers are trying to “connect the dots”. The POTS study combining Vagas nerve stimulation with Mestinon, almost sounds like Dr. David Systrom is on the advisory committee. Many Neurologist specializing in epilepsy have had remarkable success when they wrap the left Vagas nerve with a wire that routinely and briefly stimulates the nerve with a charge from a power source placed beneath the skin. House bound epilepsy patients are often able to work full time, after implantation of the device. Many Orthopods claim that their patients with neck problems often battle depression. Many of these Docs feel that this is because the Vagas nerve is compromised.
Cort, we are so indebted to you. I tried Vagal stimulation years ago using my left ear. I am wondering if right ear stimulation, with a change from the tragus, and some Mestinon added in might be a winner. I never would have obtained this info on my own. Many thanks!
Thanks – We’re seeing a field develop before our eyes. When you look at all the different factors involved I would be surprised if many people had a good result. Most of all, though, I was impressed with Lauren Stiles enthusiasm – she’s quite excited about the possibility – and she’s usually pretty conservative.
Eric,
I wish you an expedited recovery, Knowing personally that brain/ brain stem injuries can take years for recovery.
You mention you are in the UK.
I would first recommend London or perhaps Germany for diagnosis.
Be persistent, insist on a Functional MRI to determine where any weaknesses or injuries are located within the brain and brainstem.
Which is often overlooked and requires additional testing”.
An accurate diagnosis is power in you’re corner. If you happen to be on medications for pain, sleeping or anxiety. Ask your doctor if it is safe to temporarily stop treatment until after the testing to recieve an Accurate diagnosis for your brain and body.
There may be more advanced MRI technology in the UK /Europe than here in the US.
If you are experiencing high blood pressure, metabolic,digestive issues, anxiety (similar to PTSD)
Please read on: Your symptoms may have been caused by a Head and/or spinal cord injury(s).
The Enteric Nervous System,
which is connected with the
sympathetic nervous system runs from the spinal cord to various organs including the gut and are responsible for heart functions and blood pressure.
The Vagas nerve thats runs from the brainstem to the abdomen.
AKA cranial nerve 10 (located on the left side of neck) which is responsible for sending messages between the gut and brain. These three systems make up the brain – gut connection.
PTSD help:
I struggle with severe PTSD when driving. It is a cellular memory response for keeping us safe. Having a hiatus from driving may help diminish. It did for me and the extra walks improves faster healing.
*Years later diagnosed with unknown metabolic issues thyroid, adreanal etc. All connected to the gut and cranial nerve 10, the Vagas nerve.
From an undiagnosed brainstem injury from an automobile collision.
Where I sought help.
Treatment Locations
1.University of Washington
misdiagnosis – concussion *
Refuse to be blocked by a
concussion diagnosis from an
ER doctor.
2.Oregon Health Sciences
University – Beyond Specialty
3.University of California (Davis)
Referred to UCLA
4. University of California ( L.A.)
Dianosis *
Traveled over 4,000 km to UCLA.
How to overcome:
a. Be your best Advocate, go with the best first. Save time and $$$
b. Use your diligence, stay ahead on current and advance treatment(s).
c. Bring a second advocate to listen and take notes.
d.You can quickly advance your healing,
Eric, best to you and Merry Christmas!
I found a TCM manual that illustrated the articular branch on the back of the ear to be stroked downward oblique from where attached to skull towards the first fold. It is a little bit back of mid point of back of the ear where it is attached to head .Very soothing and balancing
I had the VNS machine implant for epilepsy for2 1/2 years and all it did was cause a lot of pain when it went off and cause my voice to sound like I’m gargling when I talk. With that kind of pain when it’s simulated it made it harder to sleep and definitely never anything they’re talking about. It never helped and I had it taken out but the cord is still wrapped around that nerve. Don’t trust this study
Has there been work done with manual stimulation at that spot?
Having read the above comments and articles for vagus nervous system problems I was involved in a Road traffic accident with my head impacting the windscreen in January 2022 since May of this year I’ve started to have spasms in my body and weird pins and needle sensations to my cranial areas .I am Having counselling at the moment and it’s been suggested the damage or the flashbacks I’m experiencing areas very much connected can anyone suggest where to go as I’ve had a ct head scan and nothing obvious has shown up that relates to my symptoms any help would be gratefully appreciated
I’m a male 71 years old living in the UK suffered no broken bones but very bad PTSD as a result of the accident
So sorry Eric, that sounds horrible.
Eric, So sorry to hear about your symptoms. I wish I had an answer, but all I can think of is how important it is to keep searching for a neurologist who has experience and research in traumatic brain injury. It seems that your neurologist should be doing far more than simply doing a CT and dismissing you because that particular test didn’t show anything. I wonder if there’s a research hospital near you that’s connected to a medical school. Sometimes the best thing you can do on an internet search is to Google doctors, their reviews, and their credentials.
Eric, Sorry to hear about your nervous system problems. The Central Nervous System has the ability to repair itself more so than anyone thought just five years ago. (Even in a 71 year old brain.) Docs take an oath at their graduation ceremony to “do no harm”. Your Neurologist may be hoping that with rest and repair, your symptoms will slowly diminish. Many athletes in the U.S. resort to hyperbaric oxygen treatments to get more oxygen to the damaged tissue, even when the Neuro folks can not localize the problem. The Israeli Defense Forces have apparently “healed” significant tissue damage in their IDF troops with HBO treatments. Good luck.
Eric,
I wish you an expedited recovery, Knowing personally that brain/ brain stem injuries can take years for recovery.
You mention you are in the UK.
I would first recommend London or perhaps Germany for diagnosis.
Be persistent, insist on a Functional MRI to determine where any weaknesses or injuries are located within the brain and brainstem.
Which is often overlooked and requires additional testing”.
An accurate diagnosis is power in you’re corner. If you happen to be on medications for pain, sleeping or anxiety. Ask your doctor if it is safe to temporarily stop treatment until after the testing to recieve an Accurate diagnosis for your brain and body.
There may be more advanced MRI technology in the UK /Europe than here in the US.
If you are experiencing high blood pressure, metabolic,digestive issues, anxiety (similar to PTSD)
Please read on: Your symptoms may have been caused by a Head and/or spinal cord injury(s).
The Enteric Nervous System,
which is connected with the
sympathetic nervous system runs from the spinal cord to various organs including the gut and are responsible for heart functions and blood pressure.
The Vagas nerve thats runs from the brainstem to the abdomen.
AKA cranial nerve 10 (located on the left side of neck) which is responsible for sending messages between the gut and brain. These three systems make up the brain – gut connection.
PTSD help:
I struggle with severe PTSD when driving. It is a cellular memory response for keeping us safe. Having a hiatus from driving may help diminish. It did for me and the extra walks improves faster healing.
*Years later diagnosed with unknown metabolic issues thyroid, adreanal etc. All connected to the gut and cranial nerve 10, the Vagas nerve.
From an undiagnosed brainstem injury from an automobile collision.
Where I sought help.
Treatment Locations
1.University of Washington
misdiagnosis – concussion *
Refuse to be blocked by a
concussion diagnosis from an
ER doctor.
2.Oregon Health Sciences
University – Beyond Specialty
3.University of California (Davis)
Referred to UCLA
4. University of California ( L.A.)
Dianosis *
Traveled over 4,000 km to UCLA.
How to overcome:
a. Be your best Advocate, go with the best first. Save time and $$$
b. Use your diligence, stay ahead on current and advance treatment(s).
c. Bring a second advocate to listen and take notes.
d.You can quickly advance your healing,
Eric, best to you and Merry Christmas!
ic,
I wish you an expedited recovery, Knowing personally that brain/ brain stem injuries can take years for recovery.
You mention you are in the UK.
I would first recommend London or perhaps Germany for diagnosis.
Be persistent, insist on a Functional MRI to determine where any weaknesses or injuries are located within the brain and brainstem.
Which is often overlooked and requires additional testing”.
An accurate diagnosis is power in you’re corner. If you happen to be on medications for pain, sleeping or anxiety. Ask your doctor if it is safe to temporarily stop treatment until after the testing to recieve an Accurate acc diagnosis for your brain and body.
There may be more advanced MRI technology in the UK /Europe than here in the US.
If you are experiencing high blood pressure, metabolic,digestive issues, anxiety (similar to PTSD)
Please read on: Your symptoms may have been caused by a Head and/or spinal cord injury(s).
The Enteric Nervous System,
which is connected with the
sympathetic nervous system runs from the spinal cord to various organs including the gut and are responsible for heart functions and blood pressure.
The Vagas nerve thats runs from the brainstem to the abdomen.
AKA cranial nerve 10(located on the left side of neck) which is responsible for sending messages between the gut and brain. These three systems make up the brain – gut connection.
PTSD help:
I struggle with severe PTSD when driving. It is a cellular memory response for keeping on safe. Having a hiatus from driving may help diminish. I did for me and the extra walks improves healing.
*Years later diagnosed with unknown metabolic issues thyroid, adreanal etc. All connected to the gut and cranial nerve 10, the Vagas nerve. From an undiagnosed brainstem injury from an automobile collision.
Treatment Locations
1.University of Washington
misdiagnosis – concussion *
Refuse to be blocked by a
concussion diagnosis.
2.Oregon Health Sciences
University – Beyond Specialty
3.University of California (Davis)
Referred to UCLA
4. University of California ( L.A.)
Dianosis *
Traveled over 4,000 km to UCLA.
a. Be your best Advocate, go with the best first. Save time and $$$
b. Use your diligence, stay ahead on current and advance treatment(s).
c. Bring a second advocate to listen and take notes.
d.You can quickly advance your healing,
Eric, best to you and Merry Christmas!
Thank Q again, all for your thoughtful replies its good to know that I’m not experiencing anything New but getting a different perspective on what for me through counciling and therapy is very enlightening. I think that the most scary part is all my senses have been supercharged since the accident( coming up to my 1st anniversary soon hopefully I’ll not wake up in a tauma unit and find it all been a dream) reality beckons I’m afraid as with the highs and lows could be as you mentioned a long time to recover Thank Q all again Happy and peaceful New year.
This makes me think that you can use the cholinesterase inhibitor Pyridostigmine to enhance the function of vagus nerve, and you can use nimodipine, a selective calcium channel antagonist of cerebral arteries and vessels, to increase the cerebral blood flow.
I think this whole area is so interesting. I haven’t tried a vagus nerve stimulator yet but I have been focusing on trying, successfully 🙂 to calm down my hyper-vigilant sympathetic nervous system, for nearly four years now.
I didn’t realise that being super wired and barely sleeping was having such a negative effect on my whole system. However, I couldn’t tolerate much food at all and I had burnt through my energy stores and was going downhill, at a precipitous rate. So, I had to try something. I’d found Dan Neuffer’s videos online and had ‘read’ his book, in which he emphasises calming down the autonomic nervous system.
By that time though, I had no working memory and could barely think. If one idea entered my mind, then it pushed out any other thoughts; like magnets repelling each other.
A few years ago I also joined a free weekly, global online sound healing meditation group with Nikki Gratrix. It was a friendly and very welcome hour of total relaxation, on a Sunday evening.
Now, I’m doing so much better but I still need to rein in my fight/flight/freeze and I’m continually working on my rest, digest, relax and heal. My life is still very stressful but being perpetually wired doesn’t help.
I call my sympathetic ns ‘Ancient Brain’ and used to have ‘conversations’ with them: “Yes, I’m aware that my life is a complete disaster and I really appreciate you alerting me but you’re not really helping the situation.” I also realised that Ancient Brain doesn’t have a window seat (they’re deep in the brain) and only know what’s going on through what they’re sensing. So despite my life being extremely stressful, I needed to convey to them that I was okay (which was a lie!)
Anyway, I’m not totally serene but I’m not continually wired and I generally sleep really well now and that’s made an enormous difference to everything. I’m aware of various people who use a vagus nerve stimulator and they seem to have benefitted. I’ll definitely try one myself at some point.
Gijs comment reminded me of an important point I wanted to make and then forgot. The No 1 stressor for me is food. If I eat something that my body perceives as a threat, it’ll set off the alarm bells, my HR will soar, I’m wired and I won’t be able to sleep.
For example, a couple of weeks ago, I ate some almonds in the evening and I seemed to have difficulty digesting them. My stomach hurt and I was wide awake until 3am. Many foods can have this effect. This response over-rides any attempt to calm things down. So, I have to avoid whatever it is, that my system sees as a threat.
Still really confused about which ear to stimulate, right or left. The illustration says one thing the post another. Cort please could you clarify. Many thanks for the interesting article.
I’m afraid there’s no clarification possible – we have two opposing views – one from the research paper and one from Parasym…
I have carefully listened to many testimonials of recovery. I was searching for some answers. And I couple this with my own experiences.
The sense I get is that unless you get your thyroid sorted out, even if you ‘recover’, you are in that constant mode of having to ‘calm’ yourself down, of easily getting into the stress response.
I think your observation that your symptoms are closely tied to digestion is golden.
like you Cort, I am also a supporter of dysfunction of the autonomic nervous system and the fight/flight system. It is a mechanism that can explain all complaints. However, I still have a reservation. Does this system come into action because there is a threat or is the system just off track? What is that threat? Is it for compensation? Of what? Or is it in the system itself? The brain. What is interesting to read is that the study you mention shows that the increased autoantobodies are reduced by vns. If this also applies to the autoantibodies found by porfessor Scheibenbogen then you have to ask them how is that possible? A very important finding.
I think you are on the right track, Gijs. When I worked as a licensed biofeedback therapist I was taught that the ANS works like this: the parasympathetic part should be “on “all the time; the sympathetic is only for saving us in emergencies. If we are often anxious (our brain thinks it is an emergency), we gradually train the ANS to stay in “fight-or-flight”. The system no longer has the flexibility of going back to a normal relaxed (parasympathetic) state. And constantly being in the sympathetic state means constant adrenaline in the blood steam which is very bad for us and leads to many of our symptoms. It takes a long time to retrain the ANS back to normal.
The Parasym manual states “The earclip electrode clips to the tragus of the left ear”. So I was surprised to hear that the right ear is recommended. Oh dear, I will have to learn more before daring to try the right ear.
Ha – the paper recommended the concha of the right ear (lol). I did see that some of the studies were using the tragus of the left ear as well. Time will tell – that’s why they do the studies.
Longtime fibi here, finally got a Gammacore scrip, pricey $750 for machine with 20 stims/ day, maybe three months. Then buy renewal rfid card if device helps. This like a rechargeable electric shaver with two electrodes, place on neck on vagus near carotid artery. Interestingly, Indigogo is selling Pulsetto, very clever noninvasive vagus stimulator like Gammacore for stress, anxiety, etc…no mention of pain but maybe worth buying if you can’t get Gammacore. Does it work…took edge off pain immediately on trying for first few days, not as sure now, will need to keep experimenting with it.
2022 Research on ME Neuroglial Failure > https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9124899/
Sleep… I think that it is also necessary to consolidate memories, i.e. to transfer elements in the daily short memory into a long term memory. These info come from my university time when a lot of concepts had to be memorized. But science changes over time… maybe these notions have been debunked since.
Dr Robert Groysman MD also has a facebook group where participants are using TENS units with tragus clips to treat some of the effects of Long Covid.
Dr Groysman also does stellate ganglion block treatments for those who can get to his office.
I was wondering if anyone has experience using the GammaCore, which is usually used to prevent migraines. I used one twice a day for a year (part of a pre-trial experiment that never made it to trial), and it made me feel better for the first six months and then I saw no benefit after that. (You apply it to the vagus nerve on your neck).
I just got one for fibro as I mentioned above. Twice a day is only 10% of the allowed number of zaps, way too few for bad fibro pain IMO. I’m still experimenting with mine. I haven’t seen any published Gammacore studies for fibro.
I use a Med-Fit vagus nerve stimulator, and in the user manual it states that “We recommend you connect the ear clip to the left ear only, as this is where most research studies have placed the ear clip”. However, you state ‘Right ear only – with the right side of the brain governing “neurocardiovascular-sympathetic interactions”, it’s crucial that the device be attached to the right ear.’ – is it a well-established fact that the right side governs these interactions? Do you have a source/link for this, Cort?
Apologies – I didn’t read the article carefully! Of course, you’re drawing on the paper cited above!
What proof is there that this directly acts on the vagus nerve?
It could be working in a completely different way than is being theorized, i.e., it doesn’t ‘stimulate’ the vagus nerve, and it’s not ‘stimulating’ the para-sympathetic system either. It could be acting on depolarizing cells, and getting calcium out of them, and that in turn having other effects, etc. See a paper Cort referenced in a recent pist from a clinic in Japan using depolarizing electric pulses [amongst other therapies] to treat the tight neck muscles and eliminating ME/CFS, TBI, whiplash.
I also don’t comprehend: a state of Me/CFS, where you can’t get out of bed or do much of anything and feeling hopeless – a state of too much ‘parasympathetic’ activity if these are the terms used, why would you then want to stimulate more parasympathetic activity? It sounds nutty to me.
Also, has it ever been considered that the sympathetic system is going into overdrive to counteract a para-sympathetic system that is also in overdrive? Some get a bi-polar like diagnosis…. And that maybe these two are interacting and are not so distinct and separate? And what you want is to stabilize and restore the metabolic functioning (via nutrition and thyroid) so it doesn’t have to keep swinging either way to make-up for energy production loss?
You are right.In some cases is a dominant parasympathetic nervous system and i also wonder if this devices can really balance the autonomic nervous system.As you said both can be high or both can be weak….is not simple at all.I had a pituitary apoplexy that almost killed me and my thyroid is not working anymore and i take cortisol and other hormons…i would be interested in a device that can regulate the autonomic nervous system not only making the parasympathetic one stronger.I would love to chat more with you if possible.
my email is : miculetevalentin@yahoo.com
Your comment is very good and i would love to share some opinions.Thank you
Hi.
I sent you an email.
Just a quick share on the Vagus Nerve from Eva Detko in conversation with-
Dr. Navaz Habib: Of course, and thanks for starting off with this. I really do
think it’s an important place to begin, so I’ll just jump right in. The vagus nerve
is that nerve that we don’t realize has so much of an effect on our body, positive
and negative. When it’s working, obviously, very positive. And when it’s not, it
can have very negative consequences. The reason for that is the vagus nerve is
connected to, and a lot of people don’t believe this until they actually see it, but
it’s connected to essentially every single organ in our thorax, which is our chest
area, and every organ in our abdomen, every digestive organ, every
detoxification organ.
It’s essentially the highway, the information superhighway, getting information
to and from those organs and the brain. And so when we look at its physical
location, where is it located? Well, the vagus nerve spelled VAGUS actually
begins in the cranium. It’s one of the twelve pairs of cranial nerves. So we have
12 nerves that begin in the brain stem, essentially right below the brain, just at
that top area of the spinal cord almost. And those nerves generally will stay
within the face and the neck area, and they’ll stay within the cranium. And the
tenth nerve of those numbered pairs is the vagus nerve. And this is the only
nerve that actually leaves the cranial cavity and goes into other places.
It has so many different effects. It’s called vagus, because the word vagus comes
from the word wandering. So essentially, it goes to so many different places.
This was something that anatomist, when they were studying this couldn’t
believe, that there was a single nerve that came from either side, there’s one on
the left and one on the right, that came down through the carotid sheath, which
was very important, we’ll talk about that in a moment, and it goes down to all
of these different organs and it sends information to and from.
Now when it comes down, out from the brain stem, it goes down through the
neck, and specifically is attached to, or right beside, the carotid artery and the
jugular vein. We have a carotid artery and jugular vein on either side of our
neck. And those are the blood vessels that take blood directly from the heart to
the brain, and back from the brain to the heart. Those are the most important
blood vessels in regards to brain function and the ability for our nervous system
to do its job. And inside that sheath are those two blood vessels, as well as the
3
© 2020. All rights reserved.
vagus nerve. So it really goes to show just how important the vagus nerve truly
is in creating health and actually having optimal function in that nerve.
And actually, prior to going into the neck, it’s going to send a branch to a part
of the ear. It’s going to send branches to the back of the throat, to the vocal
cords, the muscles around the vocal cords. It’s going to send branches as it
comes down into the thorax, to the heart, and to the lungs. And it’s going to
continue on down beside all of these organs, down beside the esophagus and
then pass into the gut, into the abdomen, and it’s going to attach to the
stomach, the small intestine, the large intestine, the pancreas, the liver,
gallbladder, kidneys, spleen. And that’s just how important the vagus nerve
truly is. And that’s just a basic overview of its anatomy.
OPINION
published: 18 January 2021
doi: 10.3389/fmed.2020.606824
Will COVID-19 Lead to Myalgic Encephalomyelitis/Chronic Fatigue Syndrome?
Kormaroff & Bateman
Although uncertain, it is likely that the causes of all post-infectious fatigue
syndromes share with each other and with ME/CFS many
common elements (24). Longitudinal studies of people who
develop COVID-19 may help reveal the biological underpinnings
of many post-infectious fatigue syndromes.
In people with lingering fatigue post-COVID-19—and
without chronic cardiac, pulmonary or renal dysfunction—one
likely explanation for the chronic fatigue is a state of chronic
low-grade neuroinflammation generated by the disease (25).
SARS-CoV-2 can infect the brain, causing neuroinflammation
(26). Moreover, inflammation elsewhere in the body can activate
the innate immune system in the brain via both humoral
and retrograde neural signals, largely involving the vagus
nerve (27, 28). As argued elsewhere (24), neuroinflammation
can produce fatigue through the action of various cytokines,
perhaps acting on a “fatigue nucleus”—a collection of neurons
dedicated to diminishing energy-consuming activities (“sickness
behavior”). Such energy-conserving behavior in an organism
that is infected or injured would help to focus available
energy stores on the process of healing (27, 29). In addition
to activation of a “fatigue nucleus” by neuroinflammation,
a state of chronic, severe fatigue and related symptoms
could also be explained by other abnormalities identified
in ME/CFS: impaired energy production (30), oxidative
stress (31), ion channelopathies (32), and impaired cerebral
perfusion (33).
Note that this extract mentions the Vagus Nerve
and all the other symptoms and processes involved in ME/CFS/Long Covid.
as per my previous comment the vagus nerve is poly vagal, has many effects on many organs & systems, and at least 2 branches operating in the PNS Parasympathetic, Rest & Digest, Ventral Vagus.
And the SNS, Fight Flight Freeze (Dauer) Hypervigilant , Dorsal Vagus.
In ME/CFS LONG COVID The Dorsal Vagus is ON
and the Ventral Vagus, Rest & Digest is OFF
We are constantly running away from the tigers of Infections, Toxins, Inflammation,
& Threats. our Dorsal, SNS is always ON
Our PNS, Ventral Vagus is exhausted, unable to Rest & Digest, & Housekeep, lacking the resources of nutrition, digestion, energy, antioxidants, to supply the necessary constituents for health & healing. We cannot digest, our digestive tract is on a go slow, and accumulating toxins, IBS, etc. We cannot experience refreshing sleep with a hypervigilant SNS, we are constantly wired and tired.
There are various ways of resetting the vagus branch dominance, but we need to be in a good place to start with, and things tend to get worse before they get better. eg. the releasing and detoxing of ROS, NOS, and other chemo reactive species & biologically active agents through strategies like Perrin Technique, even gentle passive mobility exercises, tai chi, cold therapy, deep breathing, box breathing, belly breathing, yoga ( stretching seems to cause a hyperarousal of the nervous system, and also the fascial release of active substances, also stimulation of release from lymph nodes.)
I find PEA calms the Tiger a little, in the mind & Body.
Do not be deceived , we are not in Rest & Digest Mode, more like hiding immobile in a cold empty cave devoid of comfort.
Be kind to yourself, send yourself some loving intentions, & loving gratitude.
Hang on in there.
methyl B12, niacin, vit C vit D withK2, B1, Bcomplex, nigella seeds, quercetin, PEA, Probiotics, CoQ10, PQQ, MSM, Fish OIl, Evening Primrose, Mg Threonate, Mg Glycinate, Himalayan pinksalt, Kcitrate, D ribose, D mannose, Cranberry extract, ALA, etc, brain fog slows & robs.
Seasons Greetings , Shine a Light .
Our microglia, and neuroglia are over extended, hypervigilant and creating more inflammation unable to put out the fire.
From Dr Eva Detko Interviewing Dr Navaz Habib RE VAGUS NERVE OVERVIEW
But what we’re going to do here today is to give people this sort of bird’s eye
view of what this is all about and why we’re doing this summit. So let’s start by
introducing the vagus nerve, telling people what it is, and maybe anatomically
where it is located as well.
Dr. Navaz Habib: Of course, and thanks for starting off with this. I really do
think it’s an important place to begin, so I’ll just jump right in. The vagus nerve
is that nerve that we don’t realize has so much of an effect on our body, positive
and negative. When it’s working, obviously, very positive. And when it’s not, it
can have very negative consequences. The reason for that is the vagus nerve is
connected to, and a lot of people don’t believe this until they actually see it, but
it’s connected to essentially every single organ in our thorax, which is our chest
area, and every organ in our abdomen, every digestive organ, every
detoxification organ.
It’s essentially the highway, the information superhighway, getting information
to and from those organs and the brain. And so when we look at its physical
location, where is it located? Well, the vagus nerve spelled VAGUS actually
begins in the cranium. It’s one of the twelve pairs of cranial nerves. So we have
12 nerves that begin in the brain stem, essentially right below the brain, just at
that top area of the spinal cord almost. And those nerves generally will stay
within the face and the neck area, and they’ll stay within the cranium. And the
tenth nerve of those numbered pairs is the vagus nerve. And this is the only
nerve that actually leaves the cranial cavity and goes into other places.
It has so many different effects. It’s called vagus, because the word vagus comes
from the word wandering. So essentially, it goes to so many different places.
This was something that anatomist, when they were studying this couldn’t
believe, that there was a single nerve that came from either side, there’s one on
the left and one on the right, that came down through the carotid sheath, which
was very important, we’ll talk about that in a moment, and it goes down to all
of these different organs and it sends information to and from.
Now when it comes down, out from the brain stem, it goes down through the
neck, and specifically is attached to, or right beside, the carotid artery and the
jugular vein. We have a carotid artery and jugular vein on either side of our
neck. And those are the blood vessels that take blood directly from the heart to
the brain, and back from the brain to the heart. Those are the most important
blood vessels in regards to brain function and the ability for our nervous system
to do its job. And inside that sheath are those two blood vessels, as well as the
3
© 2020. All rights reserved.
vagus nerve. So it really goes to show just how important the vagus nerve truly
is in creating health and actually having optimal function in that nerve.
And actually, prior to going into the neck, it’s going to send a branch to a part
of the ear. It’s going to send branches to the back of the throat, to the vocal
cords, the muscles around the vocal cords. It’s going to send branches as it
comes down into the thorax, to the heart, and to the lungs. And it’s going to
continue on down beside all of these organs, down beside the esophagus and
then pass into the gut, into the abdomen, and it’s going to attach to the
stomach, the small intestine, the large intestine, the pancreas, the liver,
3
© 2020. All rights reserved.
vagus nerve. So it really goes to show just how important the vagus nerve truly
is in creating health and actually having optimal function in that nerve.
And actually, prior to going into the neck, it’s going to send a branch to a part
of the ear. It’s going to send branches to the back of the throat, to the vocal
cords, the muscles around the vocal cords. It’s going to send branches as it
comes down into the thorax, to the heart, and to the lungs. And it’s going to
continue on down beside all of these organs, down beside the esophagus and
then pass into the gut, into the abdomen, and it’s going to attach to the
stomach, the small intestine, the large intestine, the pancreas, the liver,
gallbladder, kidneys, spleen. And that’s just how important the vagus nerve
truly is. And that’s just a basic overview of its anatomy .
Can you please point me to the Schiffer study? I can’t find it online
I used the Nurosym vagal stimulator for an hour a day for at least two months. I imagined that it had helped a little with my IBS, but my meticulous records show that it had no discernible effect – except on my bank account. However, I also do daily breathing exercises and take pills that, according to my tracker, have a clear effect on my autonomic nervous system. So it’s possible that the Nurosym would have helped me before I started those treatments.
Hello what pills you take ?
Cort, I would like to congratulate you on your masterful report on this subject! I came to read it because you had mentioned the VNS but I had not yet read this.
Because this topic had stuck in my head, then prior to my reading this page I tried to learn the basics on the vagus nerve and what stimulation could do. I want to underline a couple of great points that you made, but add some good news and interpretation. I’ll do it in a separate comment.
What I read which is good news is that there are two ways to stimulate the vagus nerve APART from electrically.
1. deep stomach breathing
2. application of specific essential oils to the bone behind the ear
With the breathing, I should underline your point anout yoga or meditation being possibly prohibitive practices… but they likely include the “deep stomach breathing” which means you stick out your gut
**to pull down on the diaphragm** which already has a built-in good effect on the vagal tone. I need to just quote straight from Wikipedia:
“During inhalation, the intra-thoracic pressure lowers due to the contraction and downward movement of the diaphragm and the expansion of the chest cavity. Atrial pressure is also lowered as a result, causing increased blood flow to the heart, which in turn decreases baroreceptors firing response which diminishes vagal tone.
This causes an increase in heart rate.”
Conclusion 1:
So your inadequate heart preload will be positively affected !!
Conclusion 2:
So POTS may be positively affected by breathing only when heart rate is increased, since we know that low variability is part and parcel of POTS.
And it is bound to ‘preload your brain with extra oxygen as well’. Do breath holding perhaps?
It says that exhalation will then reduce the space in the chest, lowering your heart rate and preventing backflow of blood.
So I’m saying that this
STOMACH BREATHING ALONE will give, basically, vagal tone variability, and no one hates yoga stretches more than I do. I LOVE stretching, just not hardcore yoga stretching.
Your article seems to be saying that a CFS patient and probably Fibro patient is somewhat STUCK in fight-or-flight,
which you explained very well is handled by the Autonomic or Sympathetic nervous system (same)
ANS or SNS. If that is slightly inaccurate about nervous system nomenclature– I find it to be my toughest subject to grasp.
REST & DIGEST;
Okay, so let me underline that point of yours as well.
1. That is what the patient is missing some of (the deep sleep or delta wave state)
I had the strangest thought two days ago: You know when you study too long and your brain turns into a brick? It feels like a heavy stone and you can’t think as well? I do not have CFS, but if I cram without breaks every 50 minutes and push through, say, two hours… it will happen. Or did in highschool. I was a top student. If I got near that sensation I would go and watch 10-15 min of TV.
I would come back MORE brain refreshed than if I just took a break. I was trying to FORCE my brain to not think for a bit.
But what do they say about non-learning TV watching? That it puts your brain into a slow-wave delta state where you are highly suggestible
ie. you don’t filter with intelligence.
Interpret that coincidence how you like, but I returned to the books as LESS of a brickhead as a result.
How we get into Delta wave state, it suggests to me, is not quite so important as THAT we do.
But there is also real phenomenon in sleep study called “microsleeps” which can be connected to falling asleep at the wheel. If we are overtired/underslept… and you know who you are… it’s the autonomic brain trying to tell you something.
Lastly on sleep, let me mention something I read, perhaps here, that will yogic training, then practice, a person can get MORE restoration out of a nap or shorter sleep.
So… forced Delta? Forced loss if vagal tone?
You said yourself, above, that if anything seems like it’s going to treat non-restorative sleep, it is Vagus Nerve Stimulation.
But let me underline why:
because you are FORCING a STUCK nervous system to VARY tone !!
You know, mix it up a bit !
rest and DIGEST:
I hope this is not annoying for anyone.
So we also seem to have either digestive/absorptive problems in CFS/Fibro and other, autoimmune disease.
ACETYLCHOLINE– (Ach)
We know that Buytrate is the intestine’s rocket fuel, while acetate goes into the bloodstream for use in forming Acetylcholine.
You mentioned mestinon in this article. Its purpose is to inhibit Acetylcholinesterase in the synapse with the net result that the ionic channel allowing a muscle to flex stays open longer than it is designed to, and is used for Myasthenia Gravis.
But this is used BOTH
-in the cognitive brain (where brain fog is a problem
and
-at skeletal muscle
To flex and hold a muscle for
1 second
takes 1,000 doses and clearances of ACh
So if it fails early, so will the muscle tire early.
I can’t decide whether Acetylcholine
a) isnt made enough (see gut)
b) is prohibited by this possible local cell hypothroidism
c) is prohibited by a brain on fire since temperature will surely increase.
d) is the target of an autoantibody
or
e) is the victim of the KNOWN autoantibody against acetylcholinesterase reuptake receptors, as in MG disease
But wrt Vagal Tone:
“The vagus nerve acts on the sinoatrial node, slowing its conduction and modulating vagal tone, via the
neurotransmitter ***acetylcholine**”
And this REALLY got me:
In order to test vagal tone if you think there is something wrong with it, you can invasively (press behind the ear)/ use “vagus nerve stimulation by specific manual, breathing or electrical techniques.”
Pressure would be the manual one.
“Noninvasive techniques mainly rely on the investigation of heart rate and heart rate variability.”
All in all the role of the vagus nerve is a very complex subject,
but…
We know:
-that there is a gut-brain axis
-that immune response is mostly handled by the gut, with assistance from endothelial cells (those not removed , for eg. by covid infection)
-that Efferent nerve signals back to the dorsal root ganglia are deficient in Fibro, along with norepinephrine
(Gerald Albrecht)
-That serotonin is sent out from the gut and taken by serotonin transporters in the blood
-that serotonin is a VASOCONSTRICTOR.
Let me end by saying you mentioned aldosterone production levels being low during non-restorative sleep. I must read about why that matters. But I DO know that Aldosterone regulates sodium retention.
And we see kidney dysfunction all the time in long-covid if not CFS. Plus, in hypocortisolism, which can occur after hypercortisolism fatigues the adrenal glands, Aldosterone production takes a big hit.
So I ask you: is Aldosterone level ONLY low during sleep? or ALSO when awake?
Why? Because if you dont retain enough salt, you lose water to flush it out. That’s two electrolyte strikes. If this is chronic, then you may have LOW BLOOD VOLUME. I believe a few members of this site were diagnosed with low blood volume and the same or others with low blood pressure.
Well, with low volume/pressure
2 things happen:
1. You get low CELL volume and you may be sodium deficient when it comes to that ionic channel used in thinking/focus and muscle flex.
2. You heart has no choice but to make up for the low pressure with
HIGH HEARTRATE and little variance from this.
Gosh it’s complicated.
Did you know that when your inhale your heart rate is higher but when you exhale it is lower? or — should be. The idea is that perfusion needs some time to finish, whereas the initial pump does not.
So in the same way that Wim Hof is recommending breath holding for increased oxygen absorption in the lungs, the capillaries need
let’s call it: Heartrate Holding.
Im kind if going in a circle now,
but most importantly:
yes,
I believe you that VNS will help
but
The HRV being not very variable
means perfusion could suffer
and
the vagus nerve controls the heart rate
CORRECTION:
-that Efferent nerve signals back to the dorsal root ganglia are deficient *in SEROTONIN*
in Fibro, along with norepinephrine
(Gerald Albrecht)
It occurs to me, patients have their vagus nerve severed in Gastric Sleeve surgery. This could be disastrous.