

The eighth in Health Rising’s recent recovery story series brings yet another slant on recovery. We’ve had fast recoveries where someone found “the thing” (Melissa’s spinal patch, Rachel and Adam’s vaccines) that quickly turned things around. There was no magic bullet for Patrick, however.
- A Patch On It: Melissa’s Amazing Cerebral Spinal Fluid Leak ME/CFS Recovery Story – cerebral spinal fluid patch
- Adam’s BCG Vaccination Chronic Fatigue Syndrome (ME/CFS) Recovery Story – BCG vaccine
- Can the Japanese Encephalitis Vaccine Reduce Symptoms of Long COVID? – Vaccine
- Lucie’s Surprisingly Simple Chronic Fatigue Syndrome (ME/CFS) Recovery Story – anti-inflammatory and rehydration
- Up from the Ashes: James’s Severe ME/CFS Recovery/Recovering Story – CIRS-based treatment approach
- A Rapamycin Resurgence: An MD Moves the Needle on his ME/CFS – Rapamycin
- Jason’s Eclectic Mix of Treatments Returns Him to Near Normal Health After 16 Years with ME/CFS – alternative medicine treatments
Patrick was not someone anyone would have ever thought would have gotten ill. A successful, supremely fit professional and father, with a wide variety of interests, Patrick seemed to be living the dream – until a pathogen – perhaps a simple everyday pathogen – knocked him out of the workforce and into bed.
Patrick’s recovery was neither simple nor easy, but it didn’t require anything really exotic either. Finding a good practitioner, exerting discipline with pacing, doing brain retraining exercises, and employing an eclectic blend of treatments (supplements, drugs, vagus nerve stimulation, cold water exposure, etc.) – all figured in Patrick’s slow return to health – and ultimately changed his outlook on life. Thanks to Patrick for telling his story on Health Rising (Cort).
Patrick’s Story
In November 2018, I got sick, probably from a virus, and never thought twice about it. I remained very active at work as a senior partner in a small environmental consulting firm, at home with my wife Raty and our three grown-up kids, and in my many physical activities (e.g., martial arts, ocean swimming, sailing, biathlon, Cross-Fit, biking, running).
My very active life prior to ME/CFS.
However, after a few months of unusual health-related peaks and valleys, I woke up one March Monday morning unable to get out of bed for my swimming practice. That’s when everything changed. I soon had to drastically reduce my work hours and spent more and more time completely exhausted and experiencing unexplained body-wide pain, brain fog, gut dysfunction, fever-like chills, light and sound sensitivity, and insomnia. Every time I felt a little better and tried to resume some form of physical or cognitive activity, all my symptoms got worse. To me, this health crisis became known as “Kryptonitis” (i.e., green kryptonite drains Superman of his strength and severely affects his capacity to function).
I was fairly in tune with my body and mind and knew this was abnormal and serious. Having a science background was helpful. I started identifying and tracking my symptoms and consulting “Dr. Google”. Luckily, my family doctor was also very supportive. Through research, I came across the 2015 Institute of Medicine report, “Beyond ME/CFS”, which includes an in-depth review of this illness and also discovered the powerful documentary, “Unrest”, by Jennifer Brea. Everything resonated with my experience.
In the summer of 2019, I conducted a graded exercise therapy experiment that confirmed my suspicions of post-exertional malaise and, with my family doctor, decided that arranging for a formal 2-day cardiopulmonary exercise test (CPET) at the Workwell Foundation in California would provide me with a gold standard confirmation of this hallmark symptom. In November, six months after the beginning of my illness, I received a formal diagnosis of ME/CFS, with the addition of fibromyalgia following a little later.
I spent my first few years moderately to severely affected (e.g., 30-40 functional ability [2]) and mostly bedbound. With “aggressive” rest, I regained some function (e.g., 50-60% functional ability) but remained mostly housebound. These were very hard times: suffering through symptoms, loss of career and primary source of income, inability to support my family, social isolation, and stigma of living with an invisible disability.
Despite these life-altering challenges, I was blessed with support from Raty, our children, our families, and many close friends. One of these introduced me to “How to Be Sick: A Buddhist-Inspired Guide for the Chronically Ill and their Caregivers” by Toni Bernhard, a lifesaver, literally. I learned to live with ME/CFS with acceptance and whatever serenity I could muster.
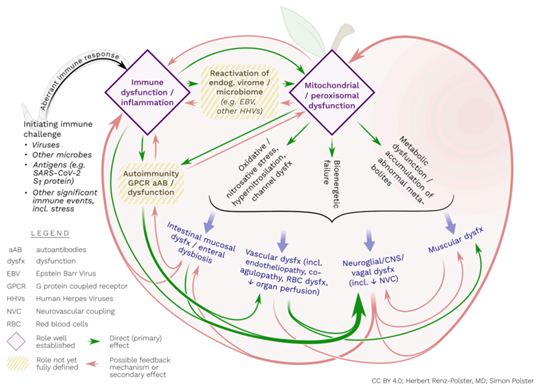
Model from Renz-Polster et al. (2022) showing the possible pathogenic processes in ME/CFS.
With a few exceptions that I would rather forget about, I consider myself very fortunate with my medical team. They were ME/CFS savvy and, despite a lack of cure or approved treatment, I received a lot of help in navigating through my options. Of course, a lot of this process was also self-directed, albeit at a slow pace, and I researched all I could on the complex but fascinating science of ME/CFS, with Health Rising by Cort Johnson being an invaluable resource. The British Columbia ME/FM Society also served as a fantastic source of information and support (e.g., advocacy, legal issues, government assistance, and caregiver resources).
In early 2022, I began learning about neuroplasticity through a brain retraining program run by Dr. Ric Arseneau, an internist located in Vancouver with expertise in ME/CFS, fibromyalgia, and long Covid. In particular, the program helped me better understand the important role of the autonomic nervous system [3] in this illness and realize how I could perhaps have a more proactive approach to my own journey toward well-being and, fingers crossed – recovery.
Eureka Moment
However, it was not until September of that year that I started gaining a lot of traction and momentum in my recovery. My eureka moment was prompted by three separate events:
Encouraged by a friend, I watched the “Race of the Century” on Netflix which tells the tale of the scrappy group of Australians who in 1983 banded together to dethrone the New York Yacht Club and break the longest-running win streak in history, 132 years, in the most prestigious sailing competition in the world. Being a sailor and understanding that trying to beat ME/CFS is also a classic underdog story, this documentary lit a fire in my heart.
- I attended the 2022 Holistic Health Summit for Long Covid and ME/CFS by Lorrie Rivers and was truly inspired by recovery stories, particularly Raelan Agle’s own experience and the treasure trove of recovery interviews that she hosts on YouTube. I also discovered new tools that made a lot of sense to me in my own pursuit of wellness. Examples include: the concept of “beditation” by Lorrie Rivers, decoding fatigue by Alex Howard, Buteyko breathwork by Patrick McKeown, and transcutaneous stimulation of the vagus nerve by Andrea Parker, David Bastians, and Dawn Wiley.
- Through a series of courses and consultations with specialists at the BC Women’s Hospital Complex Chronic Diseases Program, I managed to find a suite of medication and supplements that appeared to address key pieces of the ME/CFS puzzle in my body (e.g., mitochondrial function, neuroinflammation, pain, and gut dysfunction).
It is now June 2023 and, after diligently following my recovery plan for the past 8 months, I no longer experience any ME/CFS (or fibromyalgia) symptoms. And yes, I have conducted a few self-experiments to find out if I was still experiencing post-exertional malaise and, no, it doesn’t appear to be an issue. I even started introducing movement and exercise (very mild and progressively) into my daily routine with none of the negative payback I used to experience.

Successful walking experiment on the west coast of Vancouver Island.
Now, what factors contributed the most to my recovery? Was it one thing, a combination, or stroke of luck? Will this be temporary or permanent? Honestly, I am not sure.
What I do know is that I literally threw everything I could at getting better, including the kitchen sink. At this time, I remain careful and self-disciplined in protecting my gains, and I feel safe and at peace, while trusting my own resilience.
If I hypothesize, I would guess that my change in mindset (starting with my eureka moment in September 2022) was the foundation piece. I became determined to heal and diligently implemented my plan, which was greatly inspired by others who also found success in their recovery. Among the many lessons that I learned from “Decode Your Fatigue” by Alex Howard was that different treatments tend to be more or less effective depending on the stage of recovery that we find ourselves in – what we do and when we do it matters to our body. In that context, I think I found the right pieces of the puzzle at the right time, to give my body a chance to get into a healing state.
Brain retraining was one of the tools that truly helped me reduce the impact of stressors in my daily life by pacifying my overactive autonomic nervous system, and this process was probably facilitated by medication, supplements, and other activities like breathwork, somatic practices, cold water exposure, and vagus nerve stimulation. Taken as a whole, this strategy presumably reversed the “metabolic switch” that kept my body in a pathological state. Ultimately, this is all hypothetical, but regardless, I feel very grateful for all my blessings and I am prepared to “wash, rinse, and repeat” my recovery plan, if necessary.
As a friend recently mentioned to me, ME/CFS is a mysterious illness and with some, recovery is traceable to actions and interventions and for others it just seems like a switch got turned back on. For others, the disease can fluctuate or, at times, deteriorate. The duration and severity of the symptoms may also affect people’s outcomes. Research continues and one day, I hope we understand the disease more fully and have repeatable interventions.
Below are some rough notes on my recovery (e.g., context, mindset, what worked, what didn’t, and key resources). I realize it may seem a bit much, but I found that the devil was in the detail and that both determination and self-discipline, applied in a gentle, self-compassionate way, were essential to my gains.
I am sharing this personal story in the hopes that mapping out my experience might help others.
Patrick
P.S. If I ponder on my current level of activity and what kind of work and exercise I can tolerate, I would say my health is back to its pre-ME/CFS baseline, minus the hyper-fit and overachiever status.
I am determined to learn from this experience. For the time being, I am being careful and continue to rest and apply most actions/interventions that are laid out in my recovery plan. In February, I returned to work about 4 hrs per week and I now maintain what I would consider normal activities of daily life (i.e., normally active at home and outside, with less and less rest required [4]).
I also continue to expand the frequency, duration, and intensity of physical activities. At present, I am doing the GMB Elements program for 15 min twice per week and also do 5 min of basic strength training every other day. I even plan a solo sailing trip in the coming weeks. All this was unthinkable not so long ago.
Assuming my progress continues, I will start taking the training wheels off (e.g., supplements, medication) and re-assess, but I am in no hurry. In the long term, I am not really sure that I want to return to my pre-ME/CFS lifestyle. I am happy to live a “slow, mindful life” and may explore other passions that are more aligned with my metamorphosed self. Time will tell…
Patrick’s Notes on Recovery
My notes are organized into the following sections:
- Onset of illness and stages of recovery
- Context
- Mindset
- What worked and what didn’t
- Key resources (with web links where available).
- Onset of ME/CFS and Stages of Recovery [5]
- End 2018/early 2019: viral infection (perhaps EBV) during a perfect storm of exceptional professional, personal, and physical stress
- 2019: diagnosis and rapid decline in functional ability
- 2020 to June 2021: Stage 1 (Deep Rest); approx. 30-40% functional ability2; unable to work since June 2020
- July 2021 to August 2022: Stage 2 (Tired and Wired); approx. 50-60% functional ability
- September to December 2022: Stage 3 (Reintegration); approx. 70-80% functional ability
- January 2023 to present: Stage 3 (Reintegration); approx. 80-100% functional ability; return to work part-time and gentle/progressive re-introduction of movement and exercise.
- Context [6]
- Supportive wife (primary caregiver) and children, families, and close friends
- Supportive and knowledgeable medical team
- Financial stability.
- Mindset
- Acceptance of uncertainty associated with living with ME/CFS and unshakable trust in my own resilience. Determination and discipline to fully restore my health and emerge as a better version of myself!
- Foster creation of a healing state and a sustained joyful schema (i.e., experience daily events as uplifts rather than hassles; Friedberg et al. 2022)
- Daily morning mantra on personal goals and values; always performed in nature
- Completely stopped tracking symptoms and biometrics (e.g., steps, HR, HRV, stress score, body battery) in November 2022, which offered me freedom to live without constantly (and sometimes obsessively, for me) monitoring my health and worrying about negative outcomes.
- Treatments (i.e., to create and maintain a “healing state” in my body).
Medication
Supplements
- Mitochondrial enhancers: breakfast protein powder, ubiquinol, d-ribose, NAC, acetyl-L-carnitine, B-complex, high dose B1, magnesium
- Gut: Metamucil, enteric-coated peppermint oil
- General: Omega-3, D3, vitamin C
- Discontinued: CBD oil, THC oil, amitriptyline, liposomal glutathione, R-lipoic acid, B2, B12, betaine/HCL, hydrogen water tablets, Banyan Stress Ease (Ashwagandha, Shatavari, Brahmi).
Pacing
- 18-20 hrs per day lying down or lounging, feet up
- Energy envelope for the better part of 4 years: 2,000-3,500 steps, HR < 100 bpm
- Planned rest (“beditation” for a min. 3 hrs/day – lying down device free; “sleep” for a min. of 10 hrs from 9 pm to 7 am)
- Recuperative rest as needed, based on body feedback
- Very limited social interactions, including limited travel to visit family (e.g., aging parents, grandchild) and friends
- Avoid stressful triggers and prioritize myself
- Be aware of my personality traits (achiever, perfectionist, controller, helper) and let go of high energy demands (energy vampires)
- Talk to myself with compassion; mute positive or negative emotions by cultivating calmness and building routine.
Direct vagus nerve stimulation
- Medfit TVNS with Australian tragus clip (daily)
- Beurer ST100 (daily)
- Apollo Neuro (daily).
Mind-body techniques
- BrainChange neuroplasticity scripts [7] (10-20 times per day); importantly, my scripts included goal setting (i.e., identifying rewards of perseverance that served as joyful reminders, rather than stressful targets, of what my life would be after recovery)
- Thought catching/affect labeling
- Mindfulness meditation (Headspace, Balance, Tara Brach) (daily)
- Somatic tracking (Rebekkah LaDyne) (daily, along with neuroplasticity scripts)
- Yoga Nidra (Ally Boothroyd) (daily)
- Buteyko breathwork (Patrick McKeown) (daily)
- Visualizations (daily; some examples include: Magic Book, The Sanctuary.
Movement/exercise
- The dreaded “E” word; this was very important during the Reintegration stage of recovery
- Listen to my body before expanding my limits or returning to baseline; increase frequency, then duration, then intensity (per advice from the BC Women’s Hospital Complex Chronic Diseases Program)
- GMB Mobility program
- Simple strength training
- Walks/hikes.
Others
- Intermittent fasting (9/15), Mediterranean-style diet, mindful eating, and careful hydration (daily)
- No alcohol, caffeine, or dairy products
- Perrin short technique for lymphatic drainage (daily)
- Cold water exposure (daily)
- Massage (weekly)
- SADD lamp (daily)
- Bouncing (daily)
- Optimize time in nature, sunlight (as I slowly became less sensitive).
- Key Resources
- Agle, Raelan. Host of a YouTube Channel on ME/CFS recovery interviews and advice on various aspects of recovery
- Bernhard, Toni. Author of How to Be Sick: A Buddhist-Inspired Guide for the Chronically Ill and their Caregivers
- cfsselfhelp.org. Website with companion book by Dr. Bruce Campbell on pacing, symptom management, and recovery stories
- Friedberg et al. Scientific paper from 2022 on Non-improvements in Chronic Fatigue Syndrome: Relation to Activity Patterns, Uplifts and Hassles, and Autonomic Dysfunction
- Howard, Alex. Author of Decode Your Fatigue, including online companion course and 3-part RESET video series
- Knight, Dakota. Author of A Path to Healing Chronic Illness, self-published in 2021
- LaDyne, Rebekkah. Author of The Mind-Body Stress Reset, Somatic Practices to Reduce Overwhelm and Increase Well-being
- Lyon, Irene. Healing Trauma 3-part video training
- Perrin, Raymond. Author of The Concise Perrin Technique, a Handbook for Patients
- Rivers, Lorrie. Host of the 2022 7-day Holistic Healing Summit on ME/CFS and Long Covid
- Wiley, Dawn. Host of A Vagus Adventure Facebook Group with wealth of information of vagus nerve stimulation.
[1] Based in Comox on Vancouver Island, British Columbia (BC), Canada.
[2] Based on the functional ability scale developed by Action for ME.
[3] ME/CFS is not a psychological illness; it is a disease associated with pathophysiological impacts to numerous body systems (see graph from Renz-Polster et al. 2022). One of these is the autonomic nervous system upon which we can exert some degree of regulatory control (e.g., via structured mindfulness exercises that create new neural pathways through repetition and conditioning).
[4] When sick, I could only tolerate about 4 hours of upright activity per day (either seated or standing) but now I have no post-exertional malaise with 12+ hours of upright activity.
[5] Roughly estimated based on the stages of recovery described in Decode Your Fatigue by Alex Howard.
[6] It would almost be easy to assume that I had a smooth journey and forget the cruel reality of living with moderate/severe ME/CFS: not everyone was supportive, there was a lot of ignorance and dismissal, gaslighting, and I had to drive the medical process most of the time. Also, I tend to be a “glass half full” kind of person and, from a financial perspective, my wife and I were willing to make decisions that reduced financial pressures (e.g., willingness to downsize or move our home, if needed, reduce expenditures to a minimum rather than seek to maintain employment income). Ultimately, I gratefully acknowledge favourable circumstances, but think that our choices, often difficult and requiring self-sacrifice, made a big difference in setting up the right context for my recovery.
[7] Combination of affirming statements and structured mindfulness exercises that, together, reduce the reactivity of the sympathetic nervous system while engaging the parasympathetic nervous system by creating new neural pathways via repetition and conditioning.
Finding the Recovery Stories Helpful?
Please Support Health Rising


 Encouraged by a friend, I watched the “
Encouraged by a friend, I watched the “



The main benefit of this kind of story may be that it brings some confidence to people, and from a medical perspective, it has almost no value. Because the methodological quality of this report is poor, it is usually not considered reliable evidence.It can be seen that the drugs it uses usually have some evidence that has been validated in small-scale clinical trials. So a reasonable speculation is that drugs have provided great help, while other methods without evidence have had poor results.
I think that like any recovery story, it potentially does indeed have medical value. His interventions worked for him and they just might work for someone else. This is no different from how the entire field of ME has pretty much been – trial & error.
This is not a funded study paper: it’s a personal account by someone who has lived in the bewildering world the typical ME patient finds themselves in, except he is one of those relatively few who have made it to the other side.
I’m grateful that he (as well as other recovery story authors) has taken the time to document what worked for him – for our potential benefit. And with his science background & clear writing, he has documented it all in a way anyone can follow and implement, if they so wish.
Thank you Patrick for sharing this very detailed + informative account of your experience + your recovery.
You provide hope, encouragement, and there is so much to your story. 🙏
Don’t let anyone get you down.
Stay positive.
Keep problem solving. 🧩
I am 💯 convinced we need to change the way our 🧠 processes pain + fatigue to overcome this mysterious illness we are afflicted with.
There is no “one size fits all” regimen for ME/CFS/Fibromyalgia.
I firmly believe there are subsets within the parameters of each syndrome.
Some regimens may work.
Others may not.
You are going to receive diverse + wide range opinionated feedback for sharing your personal experience.
Some feedback will be positive.
Some feedback will be negative.
I, for one, applaud you for finding a heart to share. ❤️
I’m at the point now in my own journey of my illness where the self matters less and the community matters more.
Keep on trucking young man. 💪
Well said “Waiting”! You articulated just what I wanted to say in response.
I am inspired by Christopher’s experience and am going to follow it as best as I can in hopes of attaining better health, if not just some better days! Speaking for my myself, I can always use more “tools in my toolbox”.
THANK YOU to Christopher for all the time and energy that was required to write this and for providing so much detail! MUCH APPRECIATED!!!
You are most welcome Martha – good luck on your journey
Cheers Christopher!
Yeah, that is what an anecdote is. Still, you could try it and move on if it doesn’t work. The problem with Patrick’s story is that, unlike Jeremy’s Rapamycin or Melissa’s IH story, it is a bit amorphous. I guess the crux of his story is the “mind set”. Many of the things he lists are dopamine-related (SADD lamp, cold water, positivity, goals, etc). I can personally testify the dopamine’s effect on MECFS, but it’s not something you can easily attain. The effect of things like cold water therapy at home last only a few minutes and hardly made any difference in my experience. I needed something that lasts for days or weeks.
And then there are those like me, who are producing auto antibodies to their own dopamine. The more positive and encouraged and joyful and happy I convinced myself to feel, the more auto antibodies produced causing pain, fatigue, and malaise.
Maybe it’s the stress of trying to convince yourself that is causing the worsening? That is common, I think. You can’t convince your brain into producing dopamine in any case. Dopamine just doesn’t work that way. It has to be external and real.
Happy to hear you recovered. This statement bothered me: “If I hypothesize, I would guess that my change in mindset (starting with my eureka moment in September 2022) was the foundation piece.”
I think if you’re going to make a statement like this, without evidence, you need to fully explain what you mean. Otherwise it sounds like a change in mindset can cure ME, which can lead to patient-blaming or it’s all in their head responses.
I think some of the healing has to do with when you got ME. 2018-2019, when there is much information and possible treatments to be found so you were able to try these things not long after you became ill. For those of us who got sick in the 20th C, there was not much out there. Still, I tried so so much, after my doctor recommended GET, and I went from moderate to severe. Valacyclovir has helped but I’m still severely limited to under 500 steps a day or PEM. I’ve created a life with love & joy & creativity & friendship from my bed.
Here’s my take – both sides of the stress response – the HPA axis and autonomic nervous system – are messed up in ME/CFS and both affect the immune system and all sorts of stuff. So, if you can reduce pressure on these systems that could help. In that sense I fully understand that statement. The stress that was put on those systems must have diminished incredibly.
It doesn’t work for everyone but it really does for some – and yes, doing this kind of work earlier rather than later is probably better -and yes, everyone who gets ME/CFS or long COVID today has more options that people who did even three or five or ten years ago. That said some people – like Ellie Stein MD – who had it for years and years have been dramatically helped by these approaches.
As we’ve seen there are many possible pathways to wellness. We have some different stories coming up. I wish we knew which ones fit who!
Congratulations on creating a life of love and joy and creativity in your circumstances! That is an amazing feat 🙂
I’ve finally made peace with my body, knowing nothing is going to change. I found a rescue dog that loves nothing more than to veg with me on the couch, taking a few steps outside to potty, and to have food ‘tossed’ into his bowl. To him, I am what I am. Hopefully he will outlive me.
I just got a new rescue dog also. She loves to snuggle. I call her my therapy dog. Such a true joy. She loves to eat blueberries.
Thanks Cort!
I’m wondering if there are so many different pathways to healing that there may then be many subsets of ME?
I did a course on mindfulness meditation, somatic therapy and calming the vagus nerve. And while, it definitely helped me to accept and look for the small joys & beauty in my bed life, it hasn’t helped me physically.
Like I wrote Patrick, I’m wary & sensitive about the word “mindset” because, especially in the first ten years, I was told in was all in my head, that it was stress etc.
Thank you for all you do.
Hi Lisa,
Further to Cort’s reply, I just wanted to clarify that the change in mindset led me to research more tools (e.g., beditation, vagus nerve stimulation) and approaches (e.g., decode your fatigue by Alex Howard) and, ultimately, put together a recovery plan (and schedule) which made sense to me. I was not that organized prior to my eureka moment. So I definitely did not want to suggest that my new mindset cured me, rather that it prompted me to setup a more organized way to apply various actions/interventions that made sense to me.
All the best on your journey
Hi Patrick!
I so appreciate your clarification of what you meant about mindset & how it helped you. I’ve been told many, many times “it’s all in your head” so I’m sensitive about it.
It is fantastic that you have healed! Good luck!!
It’s called breaking away from a state of learned helplesness.
You an look up the research, it’s real. The rat sthdies thatbgiveup and die but if they see one that escapes, the wom’t succumb and continue trying to get out.
This is ridiculous. Stop believing the science you are deriving this kind of thinking from.
There are other models of what the immune system is doing, and it is not auto-attacking your body.
This is one way the medical system keeps you in a state of learned helplesness.
Read about the other model – one in which the antibodies are simply activated to heal and clean up tissue. It might inspire you to view your health and illness and how to get better differently, or give you different ideas.
* I realize this comment makes no sense in the order it was published. It’s in response to the comment of autoantibodies to being happy.
“Because the methodological quality of this report is poor, it is usually not considered reliable evidence”
I see this response time and time again when mind/body approaches are used in particular, but if you were to look at virtually every recovery story you could say the same thing. No matter what treatment is used it has not been tested in a study…
Actually there is tons and tons of research that proves the very significant health benefits of body-mind buddhist mindfulness meditation since the 1980ies in every kind of illness. Together with yoga I’ve used it as my most important recovery and wellness tool when I suffered from episodic depression and had my health fully restored. (See The Mindful Way Throgh Depression by leading depression experts Williams, Teasdale, Segal with Kabat-Zinn). Actually every thorough research evaluation for the best recovery tools for serious mental health problems that I know point to a daily yoga and meditation practice as of far greater benefit that psychiatry’s medication and psychotherapy (See The Body Keeps the Score by Bessel van der Kolk, The Evil Hours by David J. Morris)
Now that I suffer from ME/CFS meditation practice has again served me greatly on the physical and emotional plane and I am on a promising path of recovery. Again yoga and mindfulness meditation (next to many others) are my foundational wellness tools.
I think the lack of recognition from the chronically ill stems from the fact that you have to actively engage in it regularly by yourself to benefit. And this is not what most people are looking for as a cure. They want something less demanding with more instand effects.
The Western medical doctors are also not too fond of it it seems to me. Here the problem is that they don’t regard it as a genuine medical intervention that they can administer and cure without their patients doing anything themselves. Western doctors’ self-image as healers also opposes it.
Were you expecting this personal recovery story to be an RCT or meta analysis?
Thanks to Patrick and so glad he has had improvement, and has shared his story.
These “Recovery” stories are interesting and useful (though the approaches are so different It’s really hard to know where to start first (or next)) after reading them.
I’m wonder if “Non-Recovery” stories might be useful, as well. We all hear bits-and-pieces from non-recover-ers, but I wonder what a full write-up–from a positive, informed, engaged person like Patrick–would look like. After all, that is the experience most of us are having.
What can a story like that do for us, one that doesn’t have “recovery” as the climax of the story? I’m thinking there is a way for those kinds of stories to help us, as well.
I love this idea. I did intensive ANS Rewire along with supplements and other modalities for 8 months—I quit work entirely to be able to brain retrain.
My symptoms didn’t even BUDGE. The program was comprehensive, and I couldn’t have been more devoted. But, I did feel extremely gaslit, trying to tell myself pain was just a sensation when it was such a strong and distressing signal something was wrong. (Spoiler alert: it really f’n hurts when your joints are subluxing.)
I wonder if with non-recovery stories on board, we may be able to spot the differences and identify who is a better candidate. I was infuriated that the program didn’t work because a huge part of the program is believing that it will work, so they really hammer that home.
I also see these brain retraining stories weaponized against patients who don’t recover trying them, or who don’t want to try them. (To be clear, I’m not seeing that here.) But I’d love to see more “non-recovery stories!”
Well, I don’t love to see it, I want everyone to recover, but you know what I mean.
It’s a real puzzle isn’t it? I tried Gupta and DNRS and had little success as well. That said I wasn’t nearly as disciplined as Patrick with pacing – which is probably very, very important – and he tried a variety of approaches that I didn’t try.
I do get help for sure from mind/body stuff and I’m keeping up with it. I’m encouraged by Ellie Stein’s long efforts with them which eventually totally paid off – so there’s hope.
I would love it if there was a way to figure out who is the best candidate. As to non-recovery stories, though, I imagine we’d be swamped. I as well as many people have tried so many things that I almost wouldn’t know where to begin. Health Rising is going to have a treatment review site, though – and hopefully that will help.
Hi Cort,
Two additional things come to mind:
1) as Alex Howard mentions, the timing of interventions (relative to someone’s health cycle e.g., crash, tired/wired, somewhat rested, etc.) appears to matter – I made very little, if any, progress with neuroplasticity until, after 8 months of diligent practice, I somehow managed to let my body feel safe and at peace; my experience became top-down (me doing the neuroplasticity scripts) and bottom-up (my body experiencing safety and peace).
2) regarding Brian’s comment about non-recovery, here is a link to the Friedman et al. (2022) paper that you initially referred me to: Non-improvements in Chronic Fatigue Syndrome: Relation to Activity Patterns, Uplifts and Hassles, and Autonomic Dysfunction. I found it very insightful. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9271593/pdf/nihms-1795354.pdf
Thanks Patrick! Very helpful
“I made very little, if any, progress with neuroplasticity until, after 8 months of diligent practice, I somehow managed to let my body feel safe and at peace; my experience became top-down (me doing the neuroplasticity scripts) and bottom-up (my body experiencing safety and peace).”
I’m meditating about an hour and a half a day and have been for about six month. I notice that the meditations are getting deeper- my body has slowed down remarkably during them – even when I don’t feel that great during them – I can tell my body is much more peaceful – and my heartrate variabiity invariaby is ramping up considerably during them. That didn’t use to always happen.
Hopefully, I will eventually get to a place where my body is at peace.
This article seems to want to assume that psychological uplifts are positive. However the viral meningitis that started my CFS journey was caused by a virus that, through molecular mimicry, mimics my own dopamine molecules. The result has been that the better I feel psychologically, the more I will crash. My husband has always said that whenever I say to him, “I feel like I’m almost better, I feel almost well again.” — He knows a big crash will come the next day. Read the work of Dr. Madeline Cunningham who invented the blood test for PANS/PANDAS.
Others’ recovery stories always made me feel like a failure until Dr. Cunningham explained molecular mimicry to me, and that dopamine is one of three molecules viruses have learned to mimic.
One of the molecules, not one of three.
One of the molecules, not three molecules
I feel like I’m almost better, I feel almost well again.” — He knows a big crash will come the next day.
This sounds like you are running on stress hormones.
I found reading Ray Peat’s work very helpful on how to get out of those stressed states.
In conjuction, I also don’t do more than what I can. Doing more than what I can gets those stress hormones going, the ups the downs.
I seem to have this also. Sometimes I won’t be able to go to bed at night so I just stay up the whole night. But I ultimately am going to log close to 10 hours a day of sleep and most the other time is sedentary but on my computer watching youtube something like that. When I do push my self or have no choice but to get things done I will likely get pem. I did try really pushing myself once and that led to months of heightened CFS symptoms.
Sorry you were gaslit…a familiar experience for p/w/ME/CFS. How we see ourselves as people and how well we are doing in our “assignment” in life are hugely important to all people.
The classic form of story called “the hero’s journey” comes to mind. (Think Odysseus…he leaves home, faces challenges, and returns, somehow “changed.”)
Patrick has a “hero journey.” And it is terrific.. (And he meets the definition…he has “changed.”) But I have met a lot of “non-recoverers,” and I have never met tougher people with more character in my life. But because they simply endure (and don’t “change”) they don’t have a “story” and they can’t pursue their assignment. But being a non-recoverer is heroic, too.
It would be wonderful to hear shared stories from the non-recoverers, who are just as heroic as Odysseus or Patrick. Instead, I feel these people have story ripped away from them (gaslighting et. al.) Just because a person hasn’t “changed” by recovering doesn’t mean they haven’t completed the “hero’s journey” in other ways. It is a mistake, IMHO, to make a dichotomy out of these two groups.
I felt I was gaslighting myself! To thine own self (at least) be true.
Thanks for this perspective. I agree, we’re a real tough bunch.
I think you might like Sarah Ramey’s book “the Ladies Handbook to Her Mysterious Illness.” While it’s called “ladies”, it goes in depth into how, men or women, our typical “hero’s journey” must turn into something else when sick.
Thanks for the kind words Brian. In her book, How to Be Sick: A Buddhist-Inspired Guide for the Chronically Ill and their Caregivers, Toni Bernhard describes the practice of khanti, which she describes as the practice of “patient endurance, suggesting that, in addition to being patient (that is, serene and uncomplaining) we actively “endure” (i.e., to survive when faced with difficulties and to experience hardship without giving up). I don’t think it gets more heroic than that!
@Kira,
When I read your comment to the effect that it really f-en hurt when your joints sublux, I thought “ah, sounds like a bit of Ehlers-Danlos here.’ For myself, I’m still not sure if my fatigue is caused by EDS or ME/CFS–or maybe both. It certainly got worse after each viral infection in my life.
Anyway, I recently re-discovered Alan Spanos M.D. who specializes in EDS and he has an article page discussing how many doctors (mis)treat EDS, what has worked for his patients plus other topics.
When I read his comments I really get the idea this guy understands his patients. So, if you think you might also be affected by EDS, or even ME/CFS, or both, I think you might find some solace with his ideas; https://alanspanosmd.com/articles/
I meant to say “Patrick” (not Christopher) in my above submission! Brain Fog!
Patrick, I appreciated this well written recovery story.
Having lived with Me/CFS and Fibromyalgia since 1986 , much of what I have experienced is similar and of course different at the same time. All of us have our own path in this illness. I particularly appreciate the time and energy it takes to document and share your thoughts and experiences. Thank you for that. The other aspect that I like in reading others stories (and yours) is the resources that are provided. Just when I think I’ve heard and read everything possible (wink wink, I know that’s not really possible ) I’m alerted to another person to investigate. A valuable recommendation for me.
I really appreciated how well organized and documented Patrick’s story is. Very helpful 🙂
Thank you Marlene, best of luck on your journey
Dear Patrick, I still have too much brain fog to fully read your account (I hope to do so at some point in the future). But a few things stuck in mind and I would be very grateful if you still see this and might answer:
– About LDA, LDN, Trazodone: I am interested in trying all of those. Did you try all of them in parallel, or separately? Trazodone sounds interesting due to possible effect on hyperarousal – could you add a bit about your dosage, whether you took it at night, and what it did for you?
– I too sometimes work with cognitions to keep mental balance in my situation. I do not do well with any targets or goal visualisation due to the related pressure, and am more trying to live in a kind of day-by-day nirvana. Therefore I’d be really interested to learn more about what you mean by: “rewards of perseverance that served as joyful reminders, rather than stressful targets”?
– I am amazed at your ability to spend 18-20hr per day lying down. How did you do this? I have a really hard time truly resting even for a short time because of hyperarousal/being wired, and because I feel I need more options for what to do during that time that qualifies as true rest. For example I have a couple of relaxation practices but they take up only a chunk of 30 min or so. – Could give an impression of what you did during these 18-20 hrs of lying down? I’d love to have more ideas how to spend time lying down resting but without media consumption. I quite like the word “beditation” – is there a link to beditation practices?
– Thank you for mentioning the names of your vagus nerve stimulation devices! I really want a device, but brain fog and cognitive filtering/decisionmaking impairments make it nearly insurmountable for me to sift through the many options of devices, electrodes, settings and electrode placement variations. Would it be possible for you to add information about what electrodes, settings/programme & electrode placement you used with your device (maybe you followed a specific instruction link yourself?) Then I’d just try and follow your example.
May I conclude by saying that I think you can truly pride yourself in your powers of determination, self-control and personality management to do what you did. Well done :-)! Having trouble to even digest this article, I could never process the resources you did. So also thank you! for sharing in this article, and I will be glad to hear from you.
Dear JR, thank you very much for the kind words. I compiled my answers below, feel free to let me know if I missed anything and please keep in mind that I do not have any medical expertise.
– LDA, LDN, Trazadone: I tried these medications at different times, but they overlapped for about half a year in late 2022, specifically:
(1) I had two distinct trials with LDN. The first was during my lowest/worst period in May 2020. I quickly increased my daily dose from 1.5 mg at night time to 9 mg over the span of about 3 weeks. I was either too poorly or too quick in titrating and could not feel any benefits at that time. Fast forward 2 years and I decided to re-try. This time my symptoms were a little bit better and I was patient in increasing daily dosage. I started with 0.5 mg at night time and over about 8 weeks increased to 4 mg. I think that was successful for me and I currently maintain a dose of 3 mg.
(2) Regarding Trazadone, it was prescribed to me in summer 2020 by a rheumatologist with experience with fibromyalgia (he did not think ME was a real illness despite my diagnosis). I started taking 50 mg daily at bedtime to help with sleep. I took it for several years “just because” and can’t really say whether it was helpful or not. The cost was fairly low and I was reluctant to stop using it in case it was in fact helping. Eventually, I stopped using it completely in fall 2022 and have continued to improve.
(3) I started using LDA during summer 2022 at a dose of 0.5 mg every other day. I am still on that same dose now. At first, I had fairly bad side effects (worsening of most symptoms), however, after about 6-8 weeks those side effects subsided. That coincided with my eureka moment and when I started gaining momentum in my recovery.
– Rewards of perseverance:
As part of the neuroplasticity course that I took we were encouraged to come up with personal rewards of perseverance that bring forth joyful emotions (e.g., I enjoy hiking with my wife as we continue exploring our beautiful island, I fully enjoy quality time with family and friends). The challenge for me was that I sometimes became very disappointed/depressed when these goals remained out of reach. Through reading “Decode Your Fatigue” by Alex Howard, I became aware that some of my go-to personality traits (e.g., overachiever, perfectionist, controller, helper) were actually a source of anxiety and stress, especially when striving for my rewards of perseverance. I had to learn to let go and focus on self-compassion and healing while still visualizing my rewards (i.e., I no longer tried to achieve recovery, rather, I lived day-by-day [like you describe] by adhering to my recovery plan no matter the outcome). This took time, but with mindfulness practice and diarizing, I managed to do so and I continue this practice daily.
– Resting hours:
My 18-20 hrs of rest per day refers to a combination of lying down and lounging (i.e., I basically had a capacity for 4-6 hrs per day of upright activity either standing or siting with feet on the ground). This was a necessity, not a choice at first. As I slowly improved my functional capacity, I maintained the same approximate amount of rest to rebuild my “energy bank account”. I’ve only recently started to reduce my resting periods. As for what to do when resting, that’s a difficult one. Like you I had bad ADD-like symptoms but after a long period of being wired and tired, I decided to slowly get away from my smartphone and shifted to reading books that I had already read. So, for me, reading was a big escape and if my brain got distracted, it didn’t really matter because I already knew the book’s storyline. Beditation is essentially a “non-activity” when I just lie down, meditate or listen to a visualization, and sometimes fall asleep during day time. I don’t think there’s a specific goal aside from resting the body and mind.
– Vagus nerve stimulation: I tried different TENS devices, different attachment points, and different settings before settling on the Apollo, the Medfit TVNS with Australian tragus clip and the Beurer ST100. I use different strategies for each one. For the Apollo, I can wear it all the time and activate the stimulation for short intervals throughout the day, whether resting or not. For the Beurer, which feels like a purring cat on my chest, I use it for 30 min per day during my beditation. For the TENS, I started very slowly with a few minutes at a time, then progressively increased the time (without changing the pulse width and frequency). Once I got used to it and didn’t notice side effects, I trialed different settings. Most of my TENS sessions were timed to coincide with reading or watching videos/TV while lying down or lounging, so no extra effort required on my part. Dawn Wiley’s Adventures in Vagus Facebook Group has a wealth of technical information and support. Overall, the Beurer was the most efficient tool for me and it’s the only device I would get in hindsight.
I hope this is helpful and wish you all the best. Don’t hesitate to let me know if you have further questions!
Hi,
This is an awesome journey you have shared with us all, thank you.
I’m not sure if I missed it, but I would love to know how you stopped or ‘treated’ your insomnia?
Again, thank you for sharing…you have actually reminded me how far I’ve come and to focus on gains, rather than where I think I ‘should be’ or wish to be.
But, having said that, my chronic insomnia plagues me and really hinders me.
Thank you in advance
Sharon 🙂
Hi Sharon,
Thanks for the kind words. I’m so sorry to hear about your chronic insomnia. I used to sleep like a lamb before ME and those restful nights have now returned. Based on timing, insomnia was one of the last symptoms to linger on. It eventually faded away probably as a result of the combined interventions that I used. Having said that, I think I gained a lot from the Headspace (meditation App) course on sleep – it helped me stop resisting insomnia and just feel at peace with the awakeness. I know it sounds crazy but I managed to just lie down without feeling frustrated with the lack of sleep until it eventually found me. I wish you all the best on your journey.
Hi Patrick,
Thank you so much for sharing what worked for you.
Unfortunately that’s not something that’s worked for me :/
I was referred to sleep center at local hospital for horrendous insomnia.There I was instructed to keep a sleep log. When I returned the doctor took one look at it, said your circadian rhythms have dissipated. We are going to reset with light therapy. Every morning at 7 AM I had to go outside on the deck and sit in the sun for 20/30 minutes. Amazingly this worked. When season changed, I was instructed to buy a light box, and use it every morning at 7 AM, same as sitting in sunlight outside in the summer. Eventually the need for light box in winter lessened.If I notice i am still awake in the middle of night, I immediately start using the light box again.This really works for me so am passing along this info in case it might work for someone else. The light box that I use is Northern Lights,which was the brand recommended by sleep center. It has lasted for many years without any problems.
Hi Kat,
Thank you so much for sharing that. I have a red light box…I will have to try and use it! Time permitting… I don’t really have that amount of time every morning for being able to sit in front of a red light box or the sun… But I will definitely try it as often as I can.
Thank is again.
Re. chronic insomnia. The leader of our local ME/CFS group told me about tart cherry juice for insomnia. I didn’t hold out much hope, but thought, oh well, why not give it a try. I took 4 ounces of tart cherry juice an hour before bedtime and suddenly my sleep scores on my FitBit sky-rocketed. I actually had an 89 one night which I have never had before. The other nights have been in the 80’s which I am happy with. When I bought a different brand, it didn’t work so if you want to try this, buy organic tart cherry juice. How does it work? https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5617749/
Hi Betty,
Thank you so much for sharing. I drink tart Cherry juice every night. It worked for 8 weeks…and what an amazing 8 weeks it was…I could do so much more…I got excited and started making plans…and then poof…it stopped working. I still drink it just in case though. I might try pulse dosing it. But this is the story for anything that works for me…it works for a while, and then stops… So frustrating.
Sharkn, I had the same problem when I switched brands of tart cherry juice. Only the organic seemed to work. I wonder if increasing the amount over time would keep the good sleep going.
Very lucky guy to be in the right subgroup to improve
Most of us cant do it this way
Thanks for this account of your recovery. My sleep improved with Melatonin and the Headspace ‘At Night’ meditations (a different one every night and sometimes needed two or more). I notice you are on LDN: this has also helped me enormously. My PEM is much better now although I still get it if I am not careful.
A lot of stuff, and sounds expensive so financial stability must be an important contextual part. I lack all three contextual components so following such a program is out of the question for me. But I am happy for anyone who has found a pathway to full or even partial recovery.
In 2000 I was diagnosed with CFS, and had a supportive doctor but there was little he could offer me by way of treatment. Neither of us had even heard of pacing. However, I achieved full recovery without any kind of treatment plan. I did see a homeopath who prescribed small bottles of water with Latin names. Whether that was the key treatment to my recovery or not, I was highly sceptical but had the money to pay for it and there was nothing else on offer. After a couple of months of treatment the homeopath pronounced me cured, and a couple of months later I was inclined to believe it. Followed by twelve years symptom-free, no pacing no nothing. Just back to my normal life. Then two brief episodes a few years apart, and then Covid in 2020. Three years later I am still down with Long Covid. This time no supportive doctor and on a fixed income. At least I have an income and a mortgage-free home.
I don’t really have a bucket list of things left to do in this lifetime to inspire me, no family depending on me. But I also have no regrets and a positive attitude. I believe life is to be lived however you can that brings satisfaction, contentment and/or joy. That is my focus now.
AnneM, did you do anything else apart the homeopath ? Thanks for sharing
Nope! Didn’t know what else to do! I couldn’t even stay home and rest because my condo was under tarps due to being leaky and the construction noise was too much. Went to work so I could rest!
For what it’s worth, when I first realized I had long Covid I went to a homeopath again, but this time it was little white sugar pills and they didn’t help.
Thank you !
Hi Anne, love your mindset, best of luck on your journey.
Thank you very much Patrick for your detailed account.
May I ask a question :
How long before “discontiunuing” suppelemnts such as Lipoic acid, CBD oil etc ? What were the criteria : decrease of pain, or fatigue, or ….?
Wish further success !
Hi Massimo,
I started detailed monitoring of my symptoms and various metrics (e.g., hours of upright activity, heart rate, heart rate variability, steps) using a Garmin watch and Oura ring from the early beginning and it helped making decisions about terminating medication/supplements. Honestly though, I found that a subjective (how do I feel) approach was probably just as useful to me. I usually tried a new treatment for at least 3 months before deciding if it was helpful or not based. I hope this helps a little.
Thank you Patrick, I find it indeed a very tough decision to terminate something as you have no clear reference, and you keep adding up until you are overloaded…….which does not help healing ! I guess you had the same problem 🙂
Thank you for sharing your story, Patrick! I’m so glad you’re recovered and I love how you’ve laid out the details. It seems so many of us find ourselves in this condition after a time of combined stressors. I hope you never face symptoms again.
I was wondering if you’ve continued with the B1 and diet changes. Mine was related to an intracranial pressure condition so it interests me that those were helpful.
Hi Melissa,
Yes I have continued with high dose B1 (520 mg/d) and diet changes (i.e., intermittent fasting, protein shake for bfast, green smoothie for lunch and Mediterranean or Indonesian dinner, no alcohol). I have no plans on altering this for the time being. Cheers!
Thank you! I’ve had to restrict sodium greatly, avoid processed foods, and find myself intermittent fasting naturally, so this tracks with my experience in high pressure. I hadn’t tried the B1 yet outside of loading up on B1-rich foods, but plan to add it. I appreciate your reply!
Melissa, I’m curious to know how you’re doing since restricting sodium. The only sodium I can tolerate is what occurs naturally in vegetables, not even meat or dairy, definitely nothing processed. Otherwise, brain fog, extreme fatigue, dizziness, headache, head pressure as if my brain is retaining fluids, breathlessness, PEM, etc. Doctors are dumbfounded and I didn’t know anyone else with this until you mentioned it. Care to elaborate? Thanks!
Yes—I would love to elaborate because intracranial hypertension sounds EXACTLY like your case! I have a mild condition probably brought on by stenosis and after an illness raised my pressure, it caused me to leak and get severe. But high intracranial pressure can cause every single symptom you listed and it’s affected greatly by sodium. I’m so excited that this is probably your answer!
Please read my blog post on it here: https://www.healthrising.org/blog/2023/06/01/intracranial-fluid-pressure-chronic-fatigue-syndrome-fibromyalgia-long-covid/
And let me know if you have any questions! I’m so hopeful this helps you!
Melissa, Thank you so much! I will read your blog post and hope to find a solution. Is there one besides eating like a rabbit? And what kind of doctor? We seem to be in a medical desert in most parts of Florida. Thanks again for your help!!!!
Oh…haha…I just realized you’re the same Melissa whose two blog posts I read avidly when they came out, which made me think AHA! That’s it! And especially since I have neck problems that may be blocking drainage? Now the question is what can be done in my neck of the woods. (I live in Tallahassee but can easily go to Jacksonville where medical care is better.)
Yes! It’s amazing how, once we really start looking, all these factors line up perfectly with pressure. That’s why I kept asking so many questions in the pressure posts—hoping people would find their connection.
I’ve heard some less than favorable reviews on the Jacksonville Mayo location but I think it depends highly on which doctor you get. Florida is not the best place to treat leaks for sure but IH might be slightly easier.
For mild conditions the wedge pillow or sleeping on an incline and watching salt and medicines or other triggers may work but for more severe cases they have have several prescriptions that can drop pressure quickly. A person can usually know right away if this helps them. Some cases are more complicated and may need surgery to repair but just knowing what’s causing it is huge to prevent the worst symptoms. And to get the right care.
Your rabbit food comment makes me want to add that sometimes leafy greens can be a trigger (vitamin A can mean pressure symptoms for certain people) so I find myself eating a ton of rice, meat, and potatoes. Nothing processed. And it affects people differently so just look at what you’re doing or eating when you have symptoms (either immediately or within 1-2 days). I hope you can find a doctor to help you with this!
Thank you SOOOOO much, Melissa! I do keep a food and symptom diary for the past 6 months or so and have gradually added new healthy foods, spinach being one of them recently so I’ll pay attention to that. Also, the food diary was for monitoring symptoms of IC but I’ve had about a month of heavy pressure in my head and couldn’t pinpoint a cause other than what I read in your blog posts. I’ll pay better attention now and thanks again!!! Years ago a neurologist told me I might have Menieres Disease which seems to have similar symptoms to IH. In truth, I’ve worn out on traditional medicine, as I’ve found far more answers in online research and comments from the Health Rising community.
I just googled the two together and found several hits including:
“Meniere’s disease is thought to be pathophysiologically due to increased pressure in the endolymphatic spaces leading to distortion of the sensory elements. As the inner ear fluids are in direct and indirect contact with cerebrospinal fluid (CSF), it was hypothesized that changes in CSF hydrodynamics could affect inner ear fluid pressures.”
https://link.springer.com/content/pdf/10.4103/ejo.ejo_5_18.pdf
This sounds like maybe you’ll find answers for all of it! I’ve seen a lot of IC conditions to do with connective tissue disorders too. I know less about that but I had connective tissue issues only when leaking. It’s believed that leaks can damage connective tissue but I’m not sure if high pressure does anything there. It would be amazing if dealing with the pressure could help both issues but perhaps the IC is just an indicator of CTD, which makes high pressure and leaks more likely. (Insert gif of the haggard guy in front of the whiteboard making connections. Lol)
I’m excited for you! I hope it does great things!
Wow, Melissa!!! Thank you thank you thank you!!!
Congratulations for the recovery! That unusual health-related peaks and valleys sounds familiar to me. Mine was more like a few years rather than a few months before it turned chronic, and it turned out to be overtraining syndrome which I only learned in retrospect. I was competing for my black belt in Judo in my ripe old age. My doctor at the time, who was a sports physician, didn’t know about it. People often mistake it for viral illness, because it feels just like a viral illness. Dean Anderson was also a competitive x-country skier in his middle age, I believe, before he fell ill. And Bruce Campbell suffered from what appeared to be overtraining syndrome which managed by cutting back, at least till it became chronic one day.
Ah yes, I remember tracking Cort’s articles on overtraining syndrome very closely (https://www.healthrising.org/blog/2019/09/28/overtraining-syndrome-chronic-fatigue-two-similar-diseases/). There appears to be lots of overlap with ME/CFS. I hope you achieved your judo black belt – quite a feat; I practiced MMA, kali and jo-jutsu.
Thanks Patrick. Hopefully your recovery allows you to eventually return to your pre-ME level of activity too, which would be amazing.
Keep us UTD!
Where could one learn your practice of monitoring HRV to determine whether a supplement might be bad for you? That could be a real help to all of us. Cory, might you do an article on this? Or Patrick, might you consult?
Hi Joyce,
I found this Health Rising article by Hannah to be quite helpful regarding HRV monitoring: https://www.healthrising.org/blog/2021/03/04/hannah-pacing-heart-rate-monitoring-chronic-fatigue-syndrome/. In my case, I built a nice HRV dataset using a Garmin watch and Oura ring; however, over the long-term I could not find any good correlations between my symptoms and HRV. It does not mean they didn’t exist, just that I could not detect them (qualitatively or quantitatively). I ended up stopping my HRV monitoring last fall. Cort – are you still monitoring? Any success in finding correlations, even qualitative?
Thank you Patrick for telling your story and talking about « aggressive rest » . Quite a paradoxical notion but I believe in it. A long time ago when medication was not so advanced, some treatments were simply going to a sanatorium and resting for months.
Thank you Patrick for all of the amazing resources. I’m wondering how to fit all the practices in in a day, but I guess you have to be diligent. Two, how were you able to consult with the Canadian Women’s Center and receive the brain retraining from Canadian doctor? Thanks so much
Hi Tracey,
You’re right, it’s a lot to fit in but most of it is about resting so I found it okay. To get access to the BC Women’s Hospital Complex Chronic Diseases Program or to Dr Arseneau, I believe you need a referral from a BC doctor. The CCDP waitlist is about 2 yrs (horrible for people suffering) but I assume Dr Arseneau’s waitlist would be shorter. I hope this helps a little.
Patrick, thank you for sharing your story. It really resonated with me and was also very inspiring. Everything from your onset and context to your mindset and treatments is similar my own journey in many ways. And while I am not quite as far along as you are – I am 70-75% functional today – I can clearly see the progress and benefits of many of these modalities. With recovery stories like yours and those highlighted by folks like Cort, Raelen Agle or Liz Carlson, I have a lot of hope for the future.
I do have a few questions about your journey (below). Thanks in advance for your thoughts.
(1) Was the direct vagus nerve stimulation integral to your recovery? If so, how did you settle on the combination of devices you leveraged?
(2) Was BrainChange the actual name of the neuroplasticity program you used (can’t find it online)? I have completed ANS REWIRE and DRNS and while they have been helpful, I still have “wood to chop” on this front, and interested in how your program may be similar/different.
(3) What benefit did you see from low dose Abilify?
Hi Brian, this is fantastic, sounds like you’re making great progress. Some responses:
1. I believe it was and the most effective device for me was the Beurer ST100 (see Dawn Wiley’s Adventure in Vagus Fecebook group which has a wealth of info on different methods and settings). I found my Beurer on Amazon UK. I consistently use it for 30 min when I do my daily afternoon “beditation”.
2. I see that Dr Arseneau’s BrainChange program is not currently available; it combines tools from different programs including DRNS and Gupta. I hope he offers it again soon. If not, I was personally considering Alex Howard’s RESET program to top-up my neuroplasticity training, but that’s an individual choice.
3. I started using LDA last summer at a dose of 0.5mg every other day. I am still on that same dose now. At first, I had fairly bad side effects (worsening of most symptoms), however, after about 6-8 weeks those side effects subsided. That coincided with my eureka moment and when I started gaining momentum in my recovery. Therefore, it’s quite possible that LDA was a key piece of the puzzle. However, I acknowledge that my experimental design, with a sample size of 1 and many interventions done together, is definitely not ideal to distinguish LDA effects from those of brain retraining, somatic practices, etc.
I hope this helps and wish you all the best on your journey!
Thanks Patrick! I’ve been poking around on Dawn’s FB site for a while, but had been stuck in a little analysis paralysis with all the different devices, so your feedback is super helpful.
What about the LDN? Maybe it set the stage for wgat came later? 😉
Hi Patrick, thank you for sharing your inspirational story. I have a few questions:
1) What were the big “shifts” for you, where you knew this large number of things were actually working?
2) if you could whittle this list down to three to five most important things, what would they be?
Good questions and I hope I am answering correctly:
1. I had been tracking my symptoms (i.e., daily assessment of 11 symptoms), including my daily functional capacity, since the early onset of ME in 2019 (pre-diagnosis) so I had a fairly good understanding of their temporal trends. That means that in September/October 2022 I was able to notice some slight improvements. Of course, that got me excited and I paid even closer attention to what was happening and noticed consistent improvements in both symptoms and functional capacity as I was implementing my recovery plan. That’s when I knew “big shifts” were occurring.
2. I’m afraid my best guess remains the following: brain retraining (to reduce the impact of stressors in my daily life by pacifying my overactive autonomic nervous system) probably facilitated by medication (LDA, LDN), supplements, and other activities like breathwork, somatic practices, cold water exposure, and vagus nerve stimulation.
I hope this helps – good luck on your journey
Patrick I am so happy for your recovery. I’m so fatigued is it possible to reach out to me? 2017399410 thank you
Dear Nancy, I am so sorry for my delayed response and, most of all, for what you’re going through. I’d be happy to help but I think there are much more qualified resources that may be available to you in the US. In particular, there is an ME/CFS Phone Support Group that can be reached via this link: https://www.facebook.com/groups/MECFSPhoneGroup/about/. I hope this is helpful to you.
Kind regards
Glad you found something that worked! Neurofeedback has been such a helpful part of my health journey! I suffered from Severe me/Cfs and POTS for 25 years and finally found out that mine was caused by major mold and Enviornmental illness and getting rid of toxins and doing hyperberic has been such a major game changer as well as finding out I had a colon issue which required surgery! I truly wish I had known about mold illness and Enviornmental illness years ago! I went to some of the top me/Cfs specialists and none of them brought it up until I waited 2.5 years to see a doctor in Florida. I relocated to Texas to work with an amazing doctor who happens to take Medicare and all is covered except the hyperberic but he spent hours putting all the puzzle pieces together and I just wish more people were told to look into mold and Enviornmental illness as the cause
It sounds like you are still limiting your regular exercise routine out of caution which makes sense but I wonder if you could say more about how much you’ve tested your limits with regards to PEM (an hour of hard aerobic activity like hiking up a hill?). I would also be interested in more on how you managed to travel and do the Workwell exercise test given the initial severity of your symptoms.
It will be interesting to see if you can come off of all or most of the medications and supplements at some point. I would suggest to Cort that maybe you do a follow-up series in a year to see how the people in your recovery stories are doing.
I will say that having a supportive family and caretaker (and no young children or pets to care for), adequate finances (not having to worry about work or getting by on disability and being able to afford treatments), and a supportive and knowledgeable medical team (where you live) is a trifecta that very, very few patients have and I’m glad you acknowledged this was likely key to your recovery (and other recovery stories I’ve read).
My last walking experiment was carried out in April over a 5-day period of which Days 1 and 5 were also travel days (i.e., 3.5 hrs of driving each day, plus walking). On each day I walked 2-3 times for about 1 hr each time. Additional energy expenditures included daily social outings to the local coffee shops and restaurants. After returning home I had no worsening of any symptom: no PEM. Last Fall, this would have been impossible for me.
For my trip to Workwell, I followed their recommendation and arrived a few days early to rest prior to the CPET. It was a very challenging trip and, as expected, resulted in a long crash after all the testing.
I’d be happy to report back at some point.
Thank you for sharing this . I am so pleased for you .
I live in the UK and thought this radio programme might be of interest to some readers , if they can access BBC radio 4 or BBC Sounds .
It’s about mitochondria and ATP .
https://www.bbc.co.uk/sounds/play/m001md34
Positive thoughts to all fellow pwme 😀
Chris .
Thank you Patrick for taking the time to detail your recovery journey for all of us. I have also read through the comments here and appreciate additional information you’ve provided.
I very much agree with your recommendations of Toni Bernhard’s book and Lorrie Rivers’ summit. Her summit led me to Jacob Teitelbaum’s book From Fatigued to Fantastic – corny title, and lots of product-pushing, but lots of great info therein also that I reference to this day when I get various test results or when my FMD recommends new supplements.
I tried the Gupta rewiring program twice in earnest, but other than a boost right in the beginning, it just didn’t do anything for me. I’ve taken Ellie Stein’s Pathways to Improvement program live, and she just opened up the self-paced course for free to those who had previously taken her live course, so I will give that another go at my own pace.
I see that the Beurer ST100 looks very similar to my Sensate device, which I find very helpful in my vagus nerve stim and relaxation efforts. Would you say that adding a TENS device to this regimen was necessary for you?
As for supplements and meds, I am just frustrated. I have tried so many different ones (including those you’ve mentioned here and many others that have appeared on this site), working with a very knowledgeable FMD, and none of them seem to move the needle at all.
I think the big point to a post like yours (and other recovery stories) is that each of our toolbelts will look very different. What I appreciate about a post like yours are all of the hyperlinks (thanks to you and Cort for all of those), which give me some new things to explore and potentially add to my tool belt.
Lastly, I’m intrigued by your late effort to STOP using all your tracking devices. I am so wedded to my FitBit for steps, sleep, HR and HRV info. I can say that I see definite correlations to many of these data sets when I start to tank, or after I’ve crashed. The only thing is that I’m not sure I’ve made the best use of that information to change my current or future behavior. I think I may take it off for a week or two and give my brain a break from it all. Sometimes when we stop obsessing, we give our bodies permission to practice acceptance and rest. Thank you for that!
Hi Amy,
A few notes:
– You might be interested in Rebekkah LaDyne’s book, which was a revelation to me: The Mind-Body Stress Reset, Somatic Practices to Reduce Overwhelm and Increase Well-being
– I tried different TENS devices, different attachment points, and different settings before settling on the Medfit TVNS with Australian tragus clip. I used it for several months while also using my Beurer. Tough to tell the differences in soothing my parasympatheric nervous system, but my guess is that I got more benefit from the Beurer (i.e., clear relaxation response when using it, including apparently improved HRV readings)
– I totally understand your point about tracking devices. In my case, I was just a bit too obsessive and found that I felt anxious when my HRV wouldn’t improve (despite my gut telling me I was feeling better) or when I approached my daily step limits. When I stopped all the tracking, a huge weight lifted off my shoulders and I became more in tune with my body.
All the best!
Dear Patrick, I had a similar question: You mention three vagus nerve stimulation devices. Did you use them all in parallel, or rather tried one after the other? Thank you very much!
Good question. I started with the Apollo Neuro for over a year before adding TENS and later the Beurer. So, I did use all devices in parallel (on a daily basis) for about 6 months until settling on the Beurer as my main tool. If I had to pick just one, the Beurer would be it as I get a much stronger and immediate HRV response.
Thank you, Patrick!
Thanks for sharing your experience! Glad you are doing better! I have had me/cfs for over 20 years and Neurofeedback as def been a helpful tool and was able to see changes in the brain! after all the years of suffering I found out mine was caused primarily from mold and Enviornmental illness wish I knew about this 20 years ago! Hyperberic has been a game changer for me and a clean living place and glutathione. It’s been such a long journey but it is possible to find improvement after 20 plus years and visiting doctors all over the country
That’s great to hear! 🙂
Thanks so much Cort and for providing this always helpful newsletter
Thanks Patrick. To be honest, I try to avoid too many recovery stories as 1. I don’t even know if I really have the same or similar illness as the author and 2. I usually end up with a negative feeling after I read it as it leads to thinking that Ï’m just not trying hard enough. However, with yours my take-aways for myself were that I could put more effort towards getting good sleep vs coping with what I have. If one thing is going to eliminate the chance of a good day it is a crappy night’s sleep. So, I like the idea of shooting for 10 hours of “sleep.” Also, I’ve improved a bit lately (a very rare thing) with starting hydroxychloroquine, but I find that I’m just spending that extra “income” immediately. Truth is when I’m spending 100% It’s probably really costing me 120% over time and it’s resulting in me losing my gains. I like your idea of almost overemphasizing rest in order to allow your body to heal. Good for me to hear. Thanks.
Hi Mark, I’m glad that overemphasizing sleep/rest resonated with you and I really like your analogy to a bank account. I could have done a better job of highlighting this. In fact, during non-resting hours, I also became very mindful of my “energy vampire” personality traits (e.g., overachiever, controller, perfectionist, helper) and made conscious efforts to let go and be serene about things that I was too sick to be in control of.
All the best
In 2005, two doctors won the Nobel Prize for the discovery that ulcers could be caused by H-pylori and treated with antibiotics. Before that, patients were told to reduce stress, drink milk and eat a bland diet.
In 1984, Dr. Luc Montagnier and Dr. Gallo (also shared a Nobel Prize) discovered that HIV caused AIDS. Before that the devastating disease was blamed on lifestyle choices and recreational drug use.
Dr. Anthony Komaroff and Dr. Ian Lipkin have just published a seminal article comparing the symptoms of Long Covid and ME/CFS patients.
“ME/CFS and Long COVID share similar symptoms and biological abnormalities: road map to the literature”
https://www.frontiersin.org/articles/10.3389/fmed.2023.1187163/full
I am glad that Patrick is feeling better, but there really is no longtime cure for him or any of those with the other recovery stories with knowing the cause.
Betty,
Wow. That is one serious article. Thanks for mentioning it. Hopefully this gets traction somewhere at the NIH (via Congress or whatever):
“The goal of this report is to provide a road map to the state of knowledge about the underlying biology of ME/CFS and Long COVID. The often-similar findings suggest that insights into each disorder will have implications for the other. They may also enhance our understanding of evolutionarily preserved biological responses that fight infection and heal injury. We urge that investigators studying the underlying biology of Long COVID take note of the robust findings in ME/CFS that have not yet been investigated in Long COVID: given the many similarities in the underlying biology of the two illnesses, it is likely that pursuing such abnormalities in Long COVID will prove instructive.”
Thank you both for this. Congratulations to you, for your persistence, insight, and fine results (!). Much happiness to you, going forward. Thanks Cort, for providing this benefit to us.
My illness started with a brain infection in 1999. Since 2016, my flares have been about a year long; in bed except for bathroom and food. (Maximum upright about 4 hrs/day, like you.) Like you, I’ve been trying to see anything that makes sense to me, to try, in all 3 arenas: physical, intellectual, and emotional/spiritual.
“Intellectual” is a big component for me, because the initial brain infection left large lesions of white-matter loss (similar to MS, but in a different pattern, I was told). This fiction writer and science editor at Stanford, couldn’t read. And even worse, this highly creative mind lost its creativity. My 2016 scan showed that white-matter loss and atrophy had spread “almost everywhere.”
Surely this had to do with my longer flares, and increased seizures, migraines, sensory issues (with all the senses–sight, hearing, smell, taste, feel), etc. Not to mention brain fog!
So I’ve been tweaking my brain health in all ways too: physical (with diet, exercise, supplements); intellectual (with puzzles, conversation, research projects as deep as I wanted, reading when I could); and emotional/spiritual (various ways, including meditation, which I’d started in the 1970s, doing daily).
What struck me about your approach, was your use of what I might call “profound rest.” I too, had restricted screen time. But I actually aimed for long spells of intellectual fare. I was careful not to over-do; about 2 hours was my max. Being in bed, quietly doing puzzles, research, or conversation, felt so good!
I reasoned that exercising my remaining brain cells was crucial. I do believe that our brains can “re-wire” themselves; I think I’m living proof of this.
But seeing your regime of “profound rest” reminds me that brain activity uses a lot of energy. Recently I’ve wondered if I might be over-exercising the brain; and in tweaking my other remedies, I should also tweak that brain exercise. Rest it more.
Thank you for your example! As with everything else, it’s finding that balance between enough, and too much.
I will increase my meditation time; toss in short meditations throughout the day. And see what happens.
How exciting! (In a calm way, of course.) A new tweak to try. A new insight, among all the details.
Thanks again for sharing your experience. I bet it will help a lot of people, in so many different ways. Probably in ways you couldn’t have imagined.
Hi Fannie,
Best of luck with the increased brain rest! I used to spend my afternoons in bed binging on Netflix – not really a good way to increase my brain health, but it was entertaining. Unfortunately, I think I was using “cognitive ATP” that I did not have in reserve. Becoming device free and practicing “beditation” reduced that draw.
Warm regards
Thank you Patrick for your story of recovery.
I read it with interest and after a 45 year journey with ME/CFS following a Coxsackie B virus I have followed many treatments with plenty of experimentation with the assistance of an amazing GP here in Australia(sadly he died in 2019).
I have noted with interest the parallel treatments we are on which I find helpful also.
Recently after noticing hypoxia during sleep which prompted sleep studies and consultation with a Sleep Specialist who deals with many ME/CFS patients I started using a Cpap machine. I do not have typical sleep apnoea for which this treatment is usually prescribed
To my astonishment the severe early morning panic attacks that have awakened me at about 5am every day for years ceased!
I have had HPA axis dysfunction for many years and recent studies on brainstem involvement intrigued me.
I wonder if anyone else has had a benefit like this Cort.
Thanks again Cort , for bringing such great resources to the community!
Patrick thank you so much for sharing your journey with us. Your attention to detail is much appreciated.
Please could you comment more on your use of LDN, amounts, how long etc. Also, why did you choose Tramazone? What dosage do you take?
Thanks!
Trazadone
Have you read Stasha Gominak’s (neurologist) experiences using vitamin D to treat a plethora of sleep and pain disorders? Machine free!
https://drgominak.com/
Hi JD,
Thank you! And here are some notes on LDN and trazadone:
– I had two distinct trials with LDN. The first was during my lowest/worst period. I quickly increased my daily dose from 1.5mg at night time to 9mg over the span of about 3 weeks. I was either too poorly or too quick in titrating and could not feel any benefits at that time. Fast forward 2 years and I decided to re-try. This time my symptoms were a little bit better and I was patient in increasing daily dosage. I started with 0.5mg at night time and over about 8 weeks increased to 4mg. I think that was successful for me and I currently maintain a dose of 3mg.
– Trazadone is a medication that was prescribed to me by a rheumatologist with experience with fibromyalgia (he did not think ME was a real illness despite my diagnosis). I started taking 50mg daily to help with sleep. I took it for several years “just because” and can’t really say whether it was helpful or not. The cost was fairly low and I was reluctant to stop using it in case it was in fact helping. Eventually, I stopped using it completely about 6 months ago and have continued to improve.
I hope this helps
Thanks for sharing your detailed story Patrick! Wish you all the best.
Do you still take LDN, if so, at what dose? Thanks!
Thank you! Please see my response to JD re: LDN.
Cheers
Oops, didn’t see that. I am currently too on 3mg LDN, for 5 months now. I’m doing (much) better thanks to the medication.
NEW people…listen to Patrick please. I want to congratulate the organizations like SolveME and MEAction as well as the ME/CFS doctors consortium who contributed to this early management and “recovery” story, Dr. Klima’s videos, and Cort’s reporting. Patrick has benefited from early management such as the Workwell Foundation testing and advice. The most difficult part of ME/CFS is finding out that PEM exists and then what your personal energy limit is. Then staying in your limit is a very difficult adjustment for you and your family. In a survey that Cort conducted, this was the number one “wish I had known about it” and thus not caused more damage and the dive into worsening the condition. Whitney Defoe has written about his worsening condition as a result of no knowledge about PEM. I was interested that Patrick’s problem began in 2019 which was a year of great momentum in management of ME/CFS…especially with UnRest. The medications (LDN and LDA) are proving to be worthwhile. Whitney Defoe has recently had some positive changes from LDA. The completeness of Patrick’s program is also very important and the folks below who are minimizing the comprehensive program that he has described are unfortunate additions to this conversation. It is most important that people NEW to this condition see the extensive program needed to optimally manage ME/CFS….correct diagnosis with additional testing onpoint, medication, pacing (exercise restriction), mind/body connections, supplements, training devices and physical aides, etc.)
Keep on ME/CFS community and give feedback about your proper diagnosis/treatments to the doctors who did not help you!
I received news today from SolveME that long covid help communities are beginning to shut down.
This is a story of PROGRESS for the ME/CFS community.
Patrick, I was wondering if you suffered any Dysautonomia, SF Neuropathy or MCAS issues. I may have missed that. Many of us have OI, POTS, etc. Also, you seemed to have handled a lot cognitively. How did you not crash with so much each day to do!! As I explore your story, I am grateful to start with for the excellent and various mind and body relaxation resources. I can not shut my brain off. My HRV RMMSD averages around 20. I read the article on that and recovery, but I fear nerve damage affects my HRV. Also the Elite HRV is just a 2.5 minute snapshot in the morning but a Garmin Watch is too High Tech for me. So far I have been enjoying Ally and Yoga Nidra and listened to the Magic Book last night. I can not for the life of me figure out how to start with a vagus nerve stimulation device, I am so sensitive, and you used three. Guidance?? Thank you so much for your story and the resources. Gratitude.
Hi Cynthia,
Some answers that I hope will shed some light:
– I did not suffer from POTS, MCAS, etc.
– I had bad brain fog and ADD-like symptoms so had a lot of difficulty focusing for any length of time. Once I implemented my plan, I became more cautious with pacing and most of my cognitive activities (e.g., reading ME-related books or research, watching recovery stories) were done while lying down and broken up into small bits of activity interspersed with rest. This means that, in general, it took a long time to accomplish things. As an example, I signed up for unlimited online access to the 2022 Holistic Healing Summit. This allowed me to watch the presentations in short segments over a 6 week period. Same process for books like Decode Your Fatigue.
– Regarding the vagus stimulation, I use different strategies for each one. For the Apollo, I can wear it all the time and activate the stimulation for short intervals throughout the day, whether resting or not. For the Beurer, which feels like a purring cat on my chest, I use it for 30min per day during my beditation. For the TENS, I started very slowly with a few minutes at a time, then progressively increased the time (without changing the pulse width and frequency). Once I got used to it and didn’t notice side effects, I trialed different settings. Most of my TENS sessions were timed to coincide with reading or watching videos/TV while lying down or lounging, so no extra effort required on my part. Dawn Wiley’s Adventures in Vagus Facebook Group has a wealth of information and support.
Please let me know if I missed anything.
Thank you Patrick, not having dysautonomia or OI was a blessing for you. The OI heartrate issues make HRV rather dicey. It could be that is a real hindrance for recovery but still you should be able to at least improve your wired and tired states. I like many others suffer from pretty bad tinnitus which got worse after the Pfizer vaccine. I woke up from it also with my feet on fire. At one point could not stand, ended up in ER. So many variables. If you had to start with one vagus stimulation device that was easiest and considering I must start very low, do you have any thoughts. Again thank you Patrick.
Hi Cynthia, I would say my go-to is the Beurer st100 and I believe that’s also Dawn Wiley’s experience. I’d suggest starting with very short intervals (1-2 min) and see how it feels before increasing the stimulation time. In my case, I use the vibration and heat settings but don’t bother trying to match my breathing rhythm to the vibration. You should be able to find one on Amazon UK. Best of luck!
Is it a vagus nerve device just by virtue of the breath training or does it actually stimulate the vagus nerve. Forgive my lack of understanding. See it in the UK but there are a couple of U.S. sources.
Hi Cynthia, the device sits on your chest and stimulates the thoracic branch of the vagus nerve using infrasonic resonance. A similar device is the Sensate 2 (https://www.getsensate.com/pages/science-of-sensate).
Ah, toning vs stimulation. I found the ear clip itself for TENS version very painful and I have been worried about overstimulation. Sensate vs Beuer if you know? You are inundated with questions. We all want to get better so very much. This illness teaches humility in many ways. Thank you for your generosity of spirit.
It’s my pleasure. Sensate vs Beurer is a great question. I’ve only tried the Beurer, but there’s a Q&A section on the AVA Facebook Group. It seems like they both work in a similar way but Sensate has a patent. Dawn Wiley, the group’s moderator has tried both and reports a better experience (i.e., better HRV response) with the Beurer, which is why I got one.
Thank you very much Janet. In BC, under the leadership of the ME/FM Society, we are working with members of parliament to gain equitable health care for people with ME. In particular, we are trying to prioritize and fund the development of ME-specific billing codes for BC clinicians and the development of continuing medical education credits, modules or incentives for BC physicians, medical students, and other medical professionals to attend training about ME. Early diagnosis, like I managed to get, will hopefully help the “new” people.
Shame on you Cort for promoting what is inherently Lightning Process… What next, a piece on Raelan Agle? Time to stop visiting your blog…
Patrick, thank you so much for sharing your story. I’m envious. Tell me, did you have histamine and/or gluten intolerance along with your other symptoms? Secondly, when you say, “Mediterranean” do you include pasta and cheese and sausages such as pepperoni? No alcohol, for sure, but no milk, no yogurt? What did you use for neuroinflammation? Thanks and the best of the future for you.
Hi Ann,
A few answers:
– I had significant IBS and SIBO, but no gluten intolerance; for a few years I also had bad hives and skin sensitivity but not sure if that had anything to do with histamine intolerance in my case.
– By Mediterranean-style diet I mean lots of fish, white meat, fruits, vegetables, nuts and seeds, and rice (the Indonesian part of our family); we limit processed food as much as possible, but in all honesty we follow a 80-20 rule (we allow ourselves to cheat a little 20% of the time, except for alcohol and dairy).
– Yes I stopped consuming dairy products entirely last fall to see if it would help my IBS (and perhaps other symptoms). Given my overall improvements I’ll stick with it for the time being.
– As for neuroinflammation, my understanding is that LDN and PEA may operate as anti-inflammatory agents in the central nervous system, via action on microglial cells. However, I’m no expert.
All the best
Thank you very much, Patrick. Yes, I take LDN and PEA and find them to be helpful. If you can eat fish and tomatoes, then you are not histamine intolerant! I am beginning to suspect that I am gluten intolerant, but I won’t know until I try it for a few months. Losing my ability to eat any tomato product was a terrible blow to me, but I make Nomato sauce with red peppers and it appears to be ok, at least for now. Thank you and good luck to us all.
OMG I wish I could be as structured in my recovery! Respect. Unfortunately the disease seems to impact my executive functions. I too have made the experience that setting future goals only enhances pressure, so focussing on successes of perseverance instead of stressfult targets makes sense to me.
I guess this recovery scheme (with as much time lying down) is only possible if someone helps to prepare food etc.?
Hello Patrick do you think it would have been possible with out Medication?
Hi Miriam, in my case, it is quite difficult to tell, but my guess is that the LDA and LDN (and key supplements like protein, ubiquinol, D-ribose, NAC) did play a significant role. However, I have listened to many other recovery stories where medication did not seem to be involved.
What a story! I appreciate that you have shared it with us.
The problem is that you tried a bewildering array of trials of various approaches. At no time does it feel like there’s an understanding of the mechanisms of ME. It’s all still a big mystery without a direct path to recovery. Until that changes, I think I have to continue with my life and the coping skills I’ve developed, that minimize serious relapses.
The moment we all are awaiting is the one where this disease makes sense. We need a treatment plan that takes us back to somewhat normal lives.
Thank you for publishing recovery stories. Please continue to do so. They are needed to counteract the learned helplesness created by the medical establishment.
https://youtu.be/Dl1PEIkl1pI
Will do. Personally, I love recovery stories 🙂
I really appreciate you sharing your recovery journey! As someone who has tried a lot of quick fixes over the past 10 years, including Rapamycin and IVIG, I am not realizing there likely isn’t a quick fix, and that small changes and practices over a long period of time are what will lead to improvements. I’m currently working with a good functional practice room, incorporating vagus nerve stimulation, doing brain retraining, meditating, pacing etc. Hoping to one day have a recovery story to share on here like yours!
Looking forward to it Meghan. I have an interview with Dan Neuffer coming up. He says this “and that small changes and practices over a long period of time” is actually the key – and he would know. Good luck 🙂
Congratulations on your recovery, Patrick. What a story.
Here’s my opinion: I think it’s a big crapshoot with ME/CFS and that there is no good way of determining who will recover and who won’t. Mindset could be important, if that’s what’s holding you back, but it also may not be important at all.
I know this is anecdotal, but I sustained a neck injury over 10 years ago, suffering extreme pain for over a year, and, during that time, I couldn’t have been more negative about my chances for recovery; in fact, I thought I’d never play golf again, a sport I loved. Well, I ended up getting completely better and indeed played golf again. This, despite having a negative mindset the entire time.
I think the right combination of medication and supplements can lead to great improvement in an individual with ME/CFS. I think that’s the best chance for a lot of people. But, it’s far from a guarantee, as you all know.
Otherwise, trying to duplicate the myriad treatments and modalities that someone did to recover is far too overwhelming and probably will just lead to a lot of stress and unrealistic expectations.
Be a Guinea pig if you’re able and experiment with medications and supplements, under a doctor’s orders of course, while remaining stoic about the whole thing. That’s a much healthier approach.
Thank you Patrick for this detailed and transparent sharing of your story. You mentioned ‘BrainChange neuroplasticity scripts’ with a hyperlink. I’m having trouble finding where the scripts are located… could you please help with that by responding to this comment?
I have debilitating ME/CFS symptoms as well as severe cognitive impairments due to Long Hauler Covid. 17 months of trying to figure out what helps, what harms and ever so slowly making improvements in activities of daily living and severity of symptoms and PEM crashes.
Your experience is affirming for me – that I’ve been doing the right things, with the right mindsets and attitudes, to as you said “throw everything at it”. I’ve been stalled (or positively put, on a recovery plateau) with improvements in energy and symptoms, for six months. This has been frustrating – though the cognitive impairments saves me from feeling very frustrated… I joined the AVA FB group and getting myself a Vagus nerve stimulation device. I’ll go see my neuroplasticity chiropractor and get a few cold laser treatments done and see if that helps. The three Stellate Ganglion Blocks I’ve had this year helped short term, giving me some capacity/break from the relentless struggle for up to six weeks. But for me it’s not a ‘one and done’ like many LC suffers have experienced.
I really wish you all the best – I completely understand the frustration that comes with plateaus. My experience was definitely not linear, even when I was making the most progress. I just checked and it appears that Dr Arseneau is not offering his course at the moment and the scripts are usually only shared with students since they tend to be quite personal. Below, I put together an outline for a typical script to give you a sense of what they are like. Please keep in mind that there are many different styles that are probably equivalent in their effectiveness. The importance for me was to feel the scripts “viscerally or somatically”, not just in my mind, if that makes sense.
Here is my personal definition of a script to give you some context: combination of affirming statements and structured mindfulness exercises that, together, reduce the reactivity of the sympathetic nervous system while engaging the parasympathetic nervous system by creating new neural pathways via repetition and conditioning.
And here are the key steps that we used:
1. Identify the target symptom, behaviour or thought: brief description that supports affect labelling (i.e., “name it to tame it”)
2. Mindful moment: stop, be present, breathe
3. Wise mind: be aware of past response to the trigger
4. Act opposite: be proactive in changing the response to the trigger
5. Reframe: find out what is under your control (and change it) and what is not under your control (and be serene about it)
6. Rewire: intensify positive emotions (do something joyful), apply mind-body technique (e.g., meditation, breathwork, yoga nidra), and use visualization (e.g., blast from the past or exciting future)
7. Summary statement and validation: revisit highlights of the script
8. Repeat, repeat, repeat
I hope this helps a little. Cheers
This is enormously helpful, thank you for taking the time to write this out! The most positive part of reading your reply for me is that I’ve been on the right track, seeking neural reprocessing for fatigue practices, finding an internal Qigong instructor that teaches online, using Tara Brach’s RAIN somatic scanning ‘script’ and Dr. Daniel Amen’s ‘Killing Automatic Negative Thoughts’ and visualization ‘scripts’ to gently teach my brain that “yes I see we are doing what used to help us early on, thank you for trying to help. And guess what, we can do some other things besides the hyper-reactive, knee jerk, over-the-top sledge hammer on me when I do a bit too much. We can negotiate some non-sledge hammer responses of my brain.
I’ve also continued working with my mind-body psychotherapist who is very helpful.
My LC ME/CFS is extreme because of my 10 year fight to regain my brain and body after a near-death West Nile Virus infection followed by what I now recognize as post acute sequalae WN. So I recognize that though I got on the ‘heal ME/CFS’ train early after LC, my brain/body “knows what to do” which is to totally go haywire and whack out my neuroimmune responses. Sigh.
You and others on this thread really give me hope.
Thank you for writing this Patrick. After 14 months of thrashing around in the dark with long COVID I recognise a lot in your story. I feel as though I am just beginning to accept my illness and put together my own care plan. Your notes have given me a lot to go from and hold on to. All the best.
Good luck, Sophie!
You’re most welcome Sophie and I wish you all the best on your journey! Feel free to reach out if you have any questions in the future.
Please stop sharing stories about non-evidence based ‘brain retraining’
This is a BPS tool which is consistently used to harm patients with ME by minimising it’s biological nature & seriousness.
Sorry KB – I know this is a contentious and difficult area given our past history but it is helping some people – and since that is one of our main goals – we will continue from time to time share it. Of course we will also continue to explore the biological findings – and some exciting ones are coming up.
At some point I think we’ll learn why these approaches help when they do. My guess is that reducing pressure on the stress response axes – both of which are messed up in ME/CFS – and which affect everything from the blood vessels to the immune system to the metabolism – is part of it.
This feels defeating to me rather than encouraging. Because it is clear that in order to recover, you have to fully have the time to recover.
So, only those with financial stability can ever hope to get better.
I am poor, I am soon going to lose my health insurance along with my job, and I have no idea what I am going to do to survive.
I don’t have a family, or a spouse, or children because being ill makes it impossible to have a dating life or maintain relationships.
This story just affirmed to me that I can’t get better under the circumstances I live in and those circumstances cannot change while I am ill. A catch-22.
Hi N/A – tough circumstances for sure but be sure to check out the interview with Dan Neuffer (it’s in 4 parts) where he talks about people with very low resources such as yourself who still managed to recover. It’s still possible.
Hi N/A, as Cort mentions, the interview with Dan Neuffer may provide some help. I also found that Raelan Agle’s conversations with recovered individuals includes a wide range of personal circumstances. Wishing you all the best.
Thank you for this valuable resource and for sharing your story Patrick much of which resonated with me. I hope that you are still doing well with the strategies you are implementing.
I too am in BC and my family doctor is at a loss in terms of what to do with me and my chronic fatigue, which I have had for approximately 10 years (no official diagnosis). She wants to refer me to an internist , but I am thinking about requesting that she refer me to Ric Arseneau even though I am far from the coast. I am also wondering about the BC Chronic Complex Disease Program. Were you referred to both the CCDP and Dr. Arseneau individually or did you consult Dr. Arseneau through the CCDP? Thank you
Hi Marie, thank you so much for your comment. I am glad my story resonated with you. Yes, my recovery seems to be holding very well and I have resumed a physically and cognitively active life, with no need for medication. Having said that, I continue to embrace “slow living” with daily “beditation” and neuroplasticity scripts.
I really hope your health can improve and I can’t say enough good things about Dr Arseneau and his team (Dr McKay, formerly at CCDP, is now on his team). I assume your GP should be able to make a referral directly to Dr Arseneau’s practice and also to the CCDP (they are now independent of each other). I think the CCDP path is also worthwhile. They cover a wealth of resources that can be useful depending on each patient’s circumstances.
Wishing you all the best.
Hi Patrick,
Thank you so much for following up with me; it is greatly appreciated.
Mr family doctor has now referred me to both Dr. Arseneau and the CCDP. For Dr. Arseneau at least it will be a long wait, but I look forward to hopefully getting a plan in place, in lieu of my own “plan” which looks more like whac-a-mole.
That’s great that you continue to improve, and I too wish you all the best.
If I may ask, are you still on low-dose Abilify?
One of the few things that has worked for me is LDN, which is also a microglial inhibiting drug, so I am wondering whether Abilify might additionally be of use to me. Thanks again 🙏
Hi Marie, I no longer take low dose Abilify, but I think it was very helpful when I did. While I have no quantitative data to support this, I think that the combination of brain retraining and medication, particularly low dose Abilify and low dose Naltrexone were definitely beneficial in my recovery.
I’m always happy to answer any questions you may have.
I’ve tried methods from brain retraining videos, and they initially seemed to help. However, I pushed myself too hard with chores I’d wanted to do for years, which resulted in a severe crash that took months to recover from.
I suspect a significant placebo effect is at play in brain retraining. Since both the definition of Chronic Fatigue Syndrome (CFS) and what constitutes recovery can be subjective, it’s possible that what feels like a “cure” is influenced by this. For instance, I feel cured compared to when I lived in a moldy house, but that’s a specific and limited comparison.
While testimonials are a weak form of evidence, I’m still struck by the number of people who claim recovery from CFS through brain retraining. In the past, I viewed this approach as a way for authority figures to dismiss CFS, but now I’m open to the possibility that there might be something to it. It’s important to note, though, that methods similar to brain retraining, like the Sarno method, have largely been dismissed by experts in neuropsychiatry and neurology—meaning they aren’t widely accepted by mainstream medicine. I have other reasons to be skeptical, but I wanted to offer a short concise perspective.