


Exercise isn’t just about the muscles – the immune system plays a crucial role in cleanup and repair.
The great question for chronic fatigue syndrome and long COVID is: what causes post-exertional malaise (PEM)? The latest study to come out of Nancy Klimas’s Institute for Neuroimmune Medicine – led by Lubov Nathanson (senior author) and directed by Derek J. Van Booven (lead author) – defines PEM as “as a worsening of symptoms following even minor physical or mental exertion”.
The study’s title, “Stress-Induced Transcriptomic Changes in Females with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Reveal Disrupted Immune Signatures“, says it all. They applied a stressor – an exercise session on a bicycle – to women with ME/CFS (given the gender differences showing up, they’re understandably concentrating on women) and then measured how the expression of the genes found in immune cells (T, B, NK, monocytes, dendritic cells) in the blood changed.
We tend to think of the metabolism, blood flows, and the mitochondria when we think of exercise-induced PEM. It’s clear, of course, that ME/CFS is many things – it’s a metabolic disease, an autonomic nervous system disease, a neuroendocrine disease, and an immune disease. We’ll see in this study that the immune system plays a major role in our body’s response to exercise as well – and in ME/CFS, it’s not responding very well.
The study was small and not so small. It was small in numbers (20 ME/CFS / 20 healthy controls), but it dug deep. It used RNA sequencing (RNA-seq) to explore gene expressions at three different time points: baseline before exercise challenge (T0), maximal exertion (T1), and 4 h after maximal exertion (T2).
The results were startling – and not so startling. The genes in the immune cells of the healthy controls responded dramatically to the exercise bout. From prior to the exercise study to the point of maximal exertion, 102 genes significantly changed their level of expression. The healthy controls’ (HC) immune cells were “on”; virtually all of the genes (98) became more expressed.
Not so in the ME/CFS patients. As 102 genes in the HC” immune cells exploded into action, the genes in the immune cells of the ME/CFS patients lay low. They basically sat the exercise bout out – no significant changes in gene expression were found.
That was a pretty startling finding, but it aligns with other recent findings from the Hanson group. A small urine metabolomics study that found an explosion in altered metabolites (n=400) in healthy controls but no significant change in ME/CFS patients’ metabolites 24 hours after exercise later prompted the authors to write:
“Our most unanticipated discovery is the lack of changes in the urine metabolome of ME/CFS patients during recovery while significant changes are induced in controls after CPET, potentially demonstrating the lack of adaptation to severe stress in ME/CFS patients.”
So it was with protein levels as well (!). Germain’s study found exercise triggered a much bigger change in the proteins found in the sedentary, but healthy, controls than in the ME/CFS patients. The healthy controls responded to the rigors of the second exercise test by scrambling their protein mix more. Lacking the same ability to do so, the ME/CFS patients did not.
Immune genes, metabolites, proteins – that’s a pretty heady mix. The problem appears to be less that ME/CFS patients’ systems are responding in strange ways to exercise than that they’re not responding at all. Whatever switch gets turned on in the body to allow humans to tolerate and benefit from exercise – it’s not happening on multiple levels in ME/CFS.
It got even more interesting. The genes in the immune cells that got turned on in the healthy controls turned out to cluster in none other than our old “friend” – natural killer (NK) cells. NK cells are the one messed-up immune cell that’s been identified with ME/CFS from the very beginning. Plus, the number of NK cells in the blood increased during the exercise in the HCs but remained flat in the ME/CFS patients.
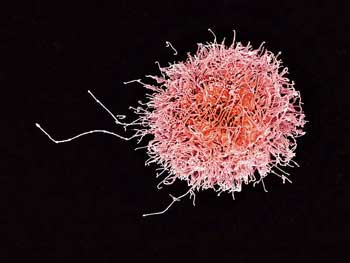
NK cells are supposed to dive into the bloodstream during exercise and participate in cleanup and recovery activities. They didn’t appear to be doing much of either in ME/CFS
We tend to associate the poor cytotoxic or killing abilities of the NK cells in ME/CFS with problems responding to pathogen invasion, but they, to my knowledge, have never been linked with exercise before.
Studies indicate, though, that NK cells are the most responsive immune cell to exercise – and what an interesting coincidence that is! As soon as we start to exercise, our NK cells wake up, become activated and move into the bloodstream on the alert for possible problems. Their levels in the blood increase 2-5xs normal during exercise, and then rapidly fall as soon as the exercise stops. (Because exercise-activated NK cells exhibit an anti-tumor profile, exercise is now being assessed as an adjunct to cancer treatment. )
Interestingly, it’s precisely the feature of the NK cells that’s gotten whacked in ME/CFS – cytotoxicity – that gets amplified during exercise – another interesting coincidence.
After Exercise
The results suggested that exercise-induced oxidative stress may be damaging and killing cells in ME/CFS
The fun continued in the after-exercise recovery period. This time, perhaps struggling to clean up the damage, it was the ME/CFS patients’ immune cells whose gene expression exploded as about 50 percent more of their genes became activated.
The GIST
- It appears that problems with blood flows, oxygen utilization, and energy production combine together to make exercise pretty miserable in ME/CFS. The latest study from Nancy Klimas’s Institute for Neuroimmune Medicine makes it clear, though, we can’t keep the immune system out of the mix. This is, after all, an all-purpose disease.
- This study assessed how the genes of immune cells (T, B, NK, dendritic, monocytes) in people with ME/CFS and healthy controls expressed themselves in response to exercise.
- The genes of the healthy controls expressed themselves well. Over a hundred genes leapt into action during the exercise period. The immune cells of the ME/CFS patients, on the other hand, laid low and were basically MIA during the exercise period. In fact, not one gene met the criteria for activation.
- This strange non-response or very limited response to a pretty darn big stressor like intense exercise has shown up in metabolic and protein studies in ME/CFS. For whatever reason (cellular exhaustion?), major systems in ME/CFS are simply not responding to exercise.
- In the case of the immune cells this study was examining the major “downer” in the study was the inability of our old “friend” natural killer cells (NK cells) to show up. Problems with NK cells showed up early in ME/CFS and they’ve been consistently found.
- In a rather remarkable coincidence (coincidence?), NK cells turn out to be the most exercise-responsive immune cell. During exercise NK cells become activated, and jump into the bloodstream where their levels increased 2-5xs. Unless you have ME/CFS that is. They didn’t “jump” nor did they appear to be become activated.
- These cells apparently troll the bloodstream because exercise inevitably produces some damage as the free radicals leak out of the mitochondria. Studies suggest that in ME/CFS, exercise produces a lot of damage as it produces more free radicals than usual and the antioxidants that keep the free radicals in check are low.
- Because exercise appears to produce leaky gut in ME/CFS as well, NK cells would be needed to combat the bacteria that are showing up in the bloodstream.
- In the after-exercise recovery period, perhaps struggling to clean up the damage, it was the ME/CFS patients’ immune cells whose gene expression exploded as about 50 percent more of their genes became activated. indeed, genes associated with the cellular response to stress and regulation of cellular response to stress that were amongst the most upregulated.
- Plus 4 hours after exercise it appeared that the ME/CFS patient’s immune cells – in contrast to the healthy controls immune cells – were still trying to tamp down inflammation.
- The authors concluded that “after significant exertion, ME/CFS patients are unable to mount the proper defenses to combat cellular stress, leaving their immune cells vulnerable to apoptosis (cell death)”.
- Finally, because herpesviruses can infect natural killer cells, it’s possible that herpesvirus reactivation may play a role in all this.
In contrast, the immune cells in the healthy controls were more prone to turn on genes involved in immune-response signaling and leukocyte activation.
What kind of stress were the ME/CFS patients’ cells facing? Recent studies suggest that high rates of oxidative stress – perhaps produced by malfunctioning mitochondria – could be hammering away at the lipid coatings of cells, releasing free radicals that feed a free radical storm. The authors suggested something similar, writing that:
“after significant exertion, ME/CFS patients are unable to mount the proper defenses to combat cellular stress, leaving their immune cells vulnerable to apoptosis (cell death)”.
The finding of an increased expression of genes involved in “positive regulation of cytokine production” 4 hours after exercise suggested ME/CFS patients’ immune systems were, long after the inflammatory pathways of the healthy controls systems had settled down, still trying to tamp down cytokine production; i.e. low-grade inflammation.
The authors concluded: “These gene expression changes may indicate that dysregulated immune responses are contributing to the PEM that characterizes this disease.”
A Gut-NK Cell-PEM Connection in ME/CFS?
We don’t know what’s happening with NK cells in the gut, but they apparently play a major role in batting down intestinal infections and immune regulation. We do know that exercise in ME/CFS increases leaky gut, which results in the transference of gut bacteria into the bloodstream. Having gut bacteria in the bloodstream is a big no-no and the immune system, including NK cells, jumps to kill and remove the bacteria, that is – if the NK cells are there and functioning.
In ME/CFS, though, it appears they’re not. NK cell numbers neither increased nor became activated during exercise, potentially setting up an intriguing NK-cell-gut-exercise-PEM-ME/CFS connection. People with ME/CFS exercise, their guts leak bacteria into the bloodstream, which NK cells, in particular, fail to clean up quickly, leading to inflammation and PEM.
A Herpesvirus-NK Cell Connection?
Herpesviruses have made waves in both ME/CFS and long COVID recently, and it’s possible that a herpesvirus-NK cell connection could be present. The Epstein-Barr virus can infect NK cells, and one review noted that “increasing evidence indicates that most, if not all, members of the herpesvirus family suppress NK cell activity to some extent”. One study found that a latent CMV infection compromised NK cells’ ability to conduct immune surveillance after exercise.
The authors of the present study noted that reactivated herpes viruses in ME/CFS appear to result in mitochondrial dysfunction (remodeling) that pushes cells toward a hypometabolic (Dauer) state, and suggested that exercise in ME/CFS may be resulting in herpes virus reactivation.
They may be exhausted in fibromyalgia as well. A study suggesting that NK cells are attacking nerve fibers in fibromyalgia also found that they displayed markers of exhaustion.
Summer Donation Drive Update

As a used to be athlete who loved nothing more than to press his body to its limits nothing has struck me more than the huge payback that occurs after even mild exertion. Exercise inevitably brings out the worst in us – both in the lab and in our lives. If the answer is going to pop out its going to pop out in exercise studies more quickly than anyplace else. That’s why I latch onto exercise studies like a bee onto honey. If that makes sense to you support HR in a way that works for you 🙂






Cort, do you know how they defined “maximal exertion”? I don’t seem to find anywhere in their paper. The maximality (is that a word?) of MECFS patients can’t be same as that of HC, and if they are different, then the study could be nonsensical. The immune system/gene expression of MECFS patients may not have responded because their exertion was much lower than that of HC.
They didn’t explicitly say except that they used McCardle’s protocol which “was used as part of larger ongoing studies of biological mechanisms underlying neuroimmune diseases.” – so it may show up in other papers.
As to a reduced maximal exertion in ME/CFS – one would expect that – that’s true. Whether a lesser maximal exertion would affect gene expression I have no idea.
The increased gene expression during the recovery period in the ME/CFS patients would seem to argue that they’d really stressed their bodies – more so, one would think, than the HC’s – even if they couldn’t attain the same maximal exertion. It’s an interesting question.
These tests are intense and I would hope that they would be enough to prompt the immune system to do what it does during exercise.
Thanks for the info. A quick search seems to indicate that Mcardle’s is a metabolic disease. So they may have assumed MECFS is metabolic disorder and applied same methodology.
They should’ve used similarly deconditioned subjects as the control, I think. The outcome could’ve been similar to MECFS patients’ then: less response at T1 due to lower maximality, but violent immune response at T2 to repair the higher damage.
I would think maximal exhertion even if it is at different levels is the key. For instance well trained persons need more excersize than sedentary ones. My guess at least.
Yes, but the question I was raising was about immune/gene response at T1, during the time of exercise. Both group exercised maximally, but MECFS group showed less/no response.
Thanks for this! I am wondering how PEM in ME/CFS differs from fibromyalgia (do we know)??
My understanding was that PEM is unique to ME/CFS. Fibro is a separate ….but often overlapping….disease where exercise is not contraindicated.
Not clinical evidence, but looking back to the year I appeared to transition from FM to CFS, my fatigue before was more general though increasing, more miserable than debilitating. I regret pushing as hard through FM as I did, and wonder if it led to the breakdown of my system that is ME-CFS.
My QUESTION is “Does this study apply to other stresses than maximal physical exertion—mental work, stressful situations or even pushing my limits before resting?
Interestingly I have an opposite experience, although I don’t disagree with the findings, I do believe ME/CFS has immune over activity too as PEM feels like influenza, and that’s an activated immune response. Maybe that’s because PEM comes later? Did they test more than a few days after exercise testing?
Anyway, my recent reasonably successful n=1 experiment started about 5 days ago, as I was forced to do much more exertion than than my safe baseline normal amount, as was shifting rooms. Even though I had a person helping me, I still had to move about beyond what normally triggers ‘Post Exertional Malaise’ PEM for me. So I knew I was in for one hell of a crash.
Other times I did anything near similar to that amount of exertion I was bedridden for up to three months with what feels like endless influenza.
However this time I remembered there was a left over supply of dexamethasone (4mg) that my mother didn’t use. So immediately after the exertion I took one tablet a day, for 5 days.
I normally have quite late onset of PEM, usually between 48 and 72 hours after exertion but the PEM didn’t hit me!
I noticed my baseline level of exertional ability has still dropped, but I’m not godawful sick, and no flu like symptoms,. My brain fog has increased slightly and a slight hangover like sensation came, but this is definitely much better than what normally happens.
So the exertion still has affected me but not to the degree it would have if I hadn’t prophylactically taken dexamethasone.
I’ve tried dexamethasone a couple times in the past but I’ve taken it after PEM itself has begun which I feel is too late, as has no for me benefit then.
I’ve often wondered whether or not we could take some sort of a immune supresor or modulator immediately after (or during) exertion if it would have an affect on preventing PEM.
I have also used Low Dose Naltrexone and NSAIDS immediately after too much exertion and that has had some slight but still noticeable effect in reducing PEM severity.
I am aware that some people with MS/CFS cannot tolerate glucocorticoid steroids like dexamethasone, so wont help them, but maybe some other immune suppressant might?.
Although we have to be aware that these drugs can cause problems when taken long term. My suggestion is more for emergency PEM prevention. i.e. a short course once in a while.
What a great idea! I was trying to think of what treatment possibilities and other than fixing the exercise problem I couldn’t think of any but that totally makes sense to me. trying an immune suppressant / high doses of antioxidants / antivirals to knock down herpes reactivation / NK cell enhancers / after exercise / gut junction enhancers ??? – they all seem like possibilities.
I could see Nancy – giving small groups of patients different things before exercise or after exercise – then taking their blood, monitoring what changes, and seeing what happens. What a great experiment!
Michael Peluso is trying to do something similar in long COVID – giving small groups of patients immune modulators and then testing the heck out of them to try to find something – and learn what’s going on at the same time…
I should add that I also have been taking the same 67.8g dose and ratio of amino acids and NAC as AXA1125. However I’ve had a PEM crash (caused from too much exertion) while on it.
In fact I haven’t noticed much difference on AXA1125 in the month I’ve been taking it.
Although maybe it’s starting to kick in. However I believe taking dexamethasone immediately after too much exertion, but prior to PEM onset, was the game changer.
Could be a combination of them both though
But as you say Cort, the time to be testing medications and concoctions is during and immediately after exertion but prior to PEM. There’s probably a lot of things that suppress PEM, and I find it puzzling why we don’t hear more ideas like this.
For example another idea I had is that cellular exertion releases a molecule that maybe mistakenly seen by the immune system as a foreign pathogen, caused by ‘molecular mimicry’. Maybe this molecule is released in abundance during exertion therefore an immune attack happens.
So I thought I need to flush this rogue molecule out by drinking large amounts of water and peeing heaps for 2 to 3 days after too much exertion, and I found that this method also reduces the severity of PEM.
That’s interesting , B Rob . When I have really bad PEM , I can’t eat but have to drink ridiculous amounts of water until I recover .
Always wondered why but the body does know what it needs !
Thanks .
I have been taking Vegepa capsules since last October and haven’t had a really bad crash since February this year . Early days , but perhaps this is having a similar effect .
I cannot eat with pem either but drink like my life depends on it!
More like you’re inadvertently fasting to heal problems and it’s stacking over time
This maybe fits in with the idea that the HC’s genes were activated during exercise and cleaned the situation up quickly, while ME/CFS persons did not activate at first at all and then began a delayed response? Maybe producing cytocines because of what happened during those hours of delayed response?
And I too was disappointed that they didn’t just continue taking samples for longer. ( My PEM starts to hit me maybe 6-7 hours later or maybe even the next morning.).
Yes, the HC genes appeared to engage in damage control and repair while the ME/CFS patients genes seemed stuck in an inflammatory response. During the recovery period their genes were actually much more active presumably because the ME/CFS patients had been hit much harder.
They did not use sedentary controls unfortunately. That would have been nice but their results jive with Hanson’s studies which did, if I remember correctly, use sedentary controls and showed a similar pattern of an inability to respond to exercise.
After exercise I take light roast weak coffee .I believe this helps so I am wondering if anyone can see how this fits into the above theory..Isn’t it great how much warmer the research is getting to our problems Thanks for yr work Cort.
Liz
Well as far as I know coffee is an adrenal stimulant (releases adrenaline etc.) and increases dopamine; it is also a diuretic that increase discharge of urine via renal activity https://www.brown.edu/campus-life/health/services/promotion/alcohol-other-drugs-other-drugs/caffeine. German sites say it also stimulates circulation including blood flow to the kidneys and brain.
I do not tolerate coffee any more because it overactivates me for a short time then makes me crash. I’ve not tried weak coffee though like you do.
D-Ribose is a much better alternative to coffee. In fact, coffee tends to be very negative where CFS/ME/ Fibro is concerned
Actually, the cleanup in healthy people comes after the exertion in 3 waves, according to an exercise study unrelated to MECFS: 1) the metabolic cleanup that starts 30 minutes after the exercise; 2) Neutrophil activation for debris cleanup that comes in a few hours after the maximal exercise; 3) IL-6 spikes up something like 100 times the next day to repair the damage and the inflammation lasts several days. (PEM that lasts a few days could be an abnormal reaction to a slight elevation after minimal exertion).
So it seems like maybe what is happening is that the HC’s genes clear the situation up right away while the failure of immediate response during exercise for the ME/CFS folks creates problems calling for the cytocine problem and the infuenza-like response? My PEM takes 6-7 hours to manifest itself or maybe even until the next morning after the over-exertion.
I was disappointed too that they didn’t keep taking their samples for longer, after the exercise. They could let the healthy controls go and just stick to following out the ones with PEM. (Who would all be feeling ill by that time, though, so this might be difficult.)
B Rob, that’s a very interesting idea! However, you’re still on it or you just stopped taking it – the real test may come in the next few days as it leaves your system.
I was in tremendous pain after a lumbar fusion a couple of years ago; the surgeon finally prescribed a “pack” of prednisilone – about 5 days, with a heavy frontload dose. I felt like Superman for a few days, then the relief faded with the drug’s departure from my tissues.
Taking something like those drugs prophylactically to prevent PEM seems worthy of more investigation.
Hi Madbegger, I took dexamethasone for 5 days, but I knew to be careful, like resting and avoiding any extra exertion as much as possible for the very reason you mentioned.
It’s a good point you make, as I forgot to mention some people wouldn’t realise they are in for a post steroid crash especially if they were doing more activities. So being aware that when they feel fantastic on steroids, that also should be a warning they may end up exerting too much, causing a secondary PEM crash.
I noticed on day five I did a little too much. And 2 days after I stopped the dexamethasone I felt very flat, I still don’t feel great, but this still far better than a 2 to 3 month PEM crash I was facing.
Another tip when coming off this type of steroid is to have a coldish shower. Start warm but turn down the temperature bit by bit, until a tolerable cold for 30 seconds. (it doesn’t have to be freezing, but cold enough that the body reacts ) The reason for is I found it wakes my adrenal system up after steroids. Like a reboot of the system
Cort, you wrote: in the after-exercise results “it was the ME/CFS patients’ immune cells whose gene expression exploded as about 50 percent more of their genes became activated.” Does that mean our genes were activated 50 per cent more THAN HAPPENED With THE HS’s genes? or that now 50% more of our own genes turned on? I’m confused, and would love to know exactly what happened with the HCs in the after-exercise measurements? (I hope this question makes sense.)
So 4 hours later, did the HC’s return back toward normal and ours finally turned on? Theirs lowered, and ours increased?
Sorry about the confusion. Fifty percent MORE GENES were activated. It was interesting to see many, (many) more genes activated in the recovery period than during the exercise itself. That’s apparently when the real work begins.
“In HCs, 831 genes had significant changes in their level of expression, with 542 being underexpressed (Supplementary Table S2). ME/CFS patients had 1277 genes that were differentially expressed, with 892 of them underexpressed (Supplementary Table S3).”
At the end of the 4 hours the genes associated with stress, inflammation, herpes simplex virus were elevated in ME/CFS while in the HC’s the expression of genes “related to inflammatory signaling in the lymphocytes” was downregulated.
In the end the authors said the “ME/CFS patients are characterized by constant low-grade inflammation” while the HC’s were characterized “immune cells that mediate damage and then repair.”…
Well, good for them! 🙂
after decades of research is what Climax etc. come up with. No shit! Sherlock?
I don’t know what you’re looking for Edwina – for me this study continues the broad theme of showing how exercise affects the body – in this case – the immune system. For the first time it brought NK cells into the exercise equation and it showed that as with the proteins and metabolites that for some reason even the immune cells – which we would not ordinarily equate with exercise problems – even the immune cells cannot rise to the occasion during exercise and they keep pumping out inflammatory mediators even after the exercise is done.
So, yes, Sherlock (:)) there’s actually quite a bit new here. Science moves slowly for sure and while this study does not tell us why exercise it does give us some clues and it scientifically validates the PEM and exercise problems in ME/CFS.
Dude, exactly 🙂 Feels like they’ been doing nothin for the last 10 years/
Except peddling celebrity dietician services!
Why do we pretend that changes in gene expression in PBMCs are strongly indicative of what goes on in the muscle?
I don’t think we can apriori say but it is intriguing that we’re seeing a lack of response to exercise in multiple compartments – immune cell genes, protein production and metabolites. Is it just exhaustion or lack of ATP production on all levels? With regard to the muscles themselves I don’t that anybody has really looked into them. I believe Systrom and the OMF Foundation are doing a muscle biopsy study, though.
Hi Cort,
2 questions.
1) Will a reduction of Epstein-Barr and other herpes viruses improve Chronic Fatigue? And
2) What’s the best way to achieve that reduction?
Thanks, Laurence of Berkeley
That’s the great question. I think it’s certainly a possibility. We haven’t had really good EBV drugs – so we really don’t know. Some may be in the works and it would be really exciting if one were to show up. In the end, though, I’m going to go with what Nancy said – for most people, it’s going to take multiple treatments to hit multiple areas to move most ME/CFS patients back into homeostasis. We just have to figure how what they are.
A friend with post-EBV ME/CFS told me that he felt better on COVID antivirals. Unfortunately, his doctor wouldn’t allow him to take any more than the standard 3-day course. I wonder if anyone’s tested the COVID antivirals on EBV. If they worked, it would be interesting to see the effect on ME/CFS.
Thank you for this. A spot on study and plain speaking article that resounds 100% with me and with many in the community I’m sure. It just makes so much sense.
I was a university hockey player etc (40 years ago) and in recovery during the early years tried to push myself through the illness that I must have fabricated in my mind. It took quite a while to realise that although I didn’t know what was happening, I knew more about me than the experts and I had to have faith in myself.
40 years on I still sometimes say, when maybe someone asks me if I have an injury (I have walked with a cane for support and stability since the beginning and apart from anything else, look drunk if I don’t use one) …that ME/CFS is an illness that I haven’t had for 40 years….never said in bitterness, it’s just how it is and what it is.
So thank you for your work, and for this fine report. Now well into my sixties I am hopeful, interestingly not for some miracle cure but for validation of all those years that I left the Dr’s office and crept home in shame feeling like a sham, an abuser of the system, someone that needed attention, was deficient emotionally and just needed to pull herself together.
Thanks for the Gist as always! Fascinating stuff.
What I like about ME/CFS research is how broad research is already at this point. Though research is underfunded and sample sizes often small, I sometimes think it’s great to have such a variety of biomedical disciplines looking at it at the same time (immunological, virological, epigenetic, genetic, metabolic, cell biology, just yesterday I saw a study discussing circRNAs, etc.). It can be frustrating to have many theories about, but this is actually a strength I think and much better than the field being stuck on one biomedical theory as I believe it happened for Alzheimer for many years. It might amass an incredible puzzle of the body over time.
Yes, indeed – I just saw that circRNA study. I had never heard of circRNA’s before but the exact same thing – a lack of response – showed up – in a different ME/CFS group with a different ME/CFS researcher and in a different compartment! That’s really saying something! That’s when you really start to think – as Herbert said – that we’re getting at some core issues. So good to see 🙂
As I scroll away after studies on ME/CFS I see many studies that mention this or that about similar or the same cells but in other diseases. Unfortunately I cannot read all of them, even skim through.
I also see other diseases that causes exercize intolerance, sometimes also mentioned PEM. And there are alot of fatigue studies within the same area of research.
Therefore, as “our” researcers must have some interaction/knowledge about these areas too. Sorry, I’m pretty new to this still. But yes it is great that we have comparisons with fibro, gwi and all other postviral deseases. Already we see results from connections with postcovid.
Are there similarities with other fatiguing deaseases? To other diseases with PEM or PEM-ish symtoms? For instance hEDS often have exacerbation of symtoms after minor tasks, sometimes they are diagnosed with ME/CFS too, sometimes “only” EDS.
I’m confused overlapping symtoms exists over a range of conditions, and I’m trying to navigate among my own as well as others conditions. And always thinking: There should be som much more cooperation than it is today! Or maybe we just do not know what’s going on.
I know that there has been a fight to have ME singled out as a real, true and disabilitating disease. Because it has needed that, but maybe we need to compare rather than “stick out/up”.
I do not know really if I’m coherent. 😂 But there is so much research out there that seems similar to what’s now done in ME, I want cooperation, comparisons, using each others findings and experiences! NOW!
I have probably written this in swenglish, hope you can understand an bear with me on this. By the way, just contributed a little something to your summer donation drive as an appriciation to the work you do! 💕
This is another very important piece of work! We may finally be getting at the core of ME/CFS. We now have clear evidence that the pathobiological hallmark of ME/CFS is a lack of adaptation to stress. In ME/CFS, there is:
• a metabolic flatline after stress exposure: https://www.mdpi.com/1422-0067/24/4/3685
• a transcriptomic flatline after stress exposure: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9916639/pdf/ijms-24-02698.pdf
• a flatline in circular RNA expression: https://www.sciencedirect.com/science/article/abs/pii/S0378111923004092
• and a lack of adaptation of NK cells after stress exposure: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9916639/pdf/ijms-24-02698.pdf )
Of course, this lack of adaptation to stress also means lack of protection of many tissues, which could easily trigger profound pathology (for instance, ME/CFS patients may be unable to mount the proper defenses to combat cellular stress, allowing for repetitive reactivation of endogenous viruses after exercise, with subsequent mitochondrial and metabolic dysfunction – which in turn will have ill effects on many other tissues and body systems).
But we need to dig deeper here. What may explain the multi-level lack of adaptation to stress? Considering the absent stress response on many biological levels in ME/CFS, a very pivotal and deep regulatory process may have gone bust.
Here we should consider another compelling (and somewhat underappreciated) finding in ME/CFS which shows a messed-up stress response in the CNS. I am talking of Rayhan and Baraniuk´s finding of a paradoxical activation of the Default Mode Network after exercise (this is their paper: “Submaximal Exercise Provokes Increased Activation of the Anterior Default Mode Network During the Resting State as a Biomarker of Postexertional Malaise in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome” : https://pubmed.ncbi.nlm.nih.gov/34975370/).
Why is this important? The regulation of the biological stress response is engrained in the human brain. The brain must change its activity pattern in response to stress to coordinate an appropriate biological adaptation to meet the changing physiological demands. Here the most important switch to be operated is the silencing of the default mode network (=DMN). This network coordinates our resting activities, which evidently need to be scaled back or silenced once we face an external threat.
And this is exactly what happens in healthy people after exercise: the DMN is being switched off and the central threat response networks are being activated. In ME/CFS, however, parts of the DMN are NOT being turned off after stress exposure but are activated instread! So instead of coordinating an effective biological response, our brains stay in the chill mode and signal: do not start adapting. Thus, our bodies are not being prepared for the many challenges and threats that exercise brings along (inflammatory stress, oxidative stress, immune stress etc). Instead, our bodies get whacked without protection, allowing – for instance – for viral reactivation and sending the most vulnerable cell populations of our bodies into dysfunction.
So the many “flatlines” that are now being described on the metabolic, transcriptomic and immunologic level could all relate to a central switch not being operated properly in ME/CFS: the central coordination of the stress response after exercise (we are discussing this in the last part of our paper: https://www.frontiersin.org/articles/10.3389/fncel.2022.888232/full).
This of course opens up more questions: Why is the CNS-adaptation lacking? Why do ME/CFS patients have a paradoxical connectivity of their brain networks? Could this also be a reflection of metabolic/mitochondrial/transcriptomic dysregulation? What´s the hen and what´s the egg? And where does all this start?
Blood supply, maybe?
Max CPET in an almost upright position, venous pooling, less blood and the blood that is available has to, predominantly, go to the legs. What is left for the rest of the body? After exercise other body parts are claiming back their portion of blood? Could that push a pause button? Or a communication backlog?
Anneke, interesting that you should mention posture and blood-pooling. I was astonished at my tolerance for exercise in the form of “deep water running” compared to walking or cycling. I never got significant PEM doing dwr and often really pushed myself. The water pressure would counter the blood-pooling and give better blood flow to the brain presumably. I have come across at least one other fellow sufferer who noticed the same thing.
Perhaps because ME/CFS patients reach higher cortisol and adrenaline levels more quickly during exercise than healthy people? This has a negative effect on the immune system. I don’t know if this can cause a reduced NK cell function.
On the other hand, ME/CFS patients often have low cortisol levels. Due to adrenal exhaustion? Very complex all these findings. I don’t see the starting point for all these systemic disorders either.
I sometimes feel like the adrenergic hyperactivation in ME/CFS (which I assume is the wired but tired feeling) might not be a root symptom but rather consequence of ME/CFS energy impairment. It feels as if with the energy impairment in the body elsewhere, I need to mobilise much more adrenaline to get going (…which equals “pushing” in ME/CFS). It feels as if a car were stuck in 1st gear, so I need to rev the engine much higher to even get it going forward bit. And afterwards, the gas pedal of my system seems to get stuck on high adrenaline.
So, paradoxically, the system seems at the same time both objectively overactivated in terms of high adrenaline, but – in relative terms – underactivated in the sense that I need to mobilise an extra amount of adrenaline in order to get something done. (Yeah I know pushing is bad but there are times where it’s difficult to get out of overexertion because of living situation).
Herbert, I always look forward to your comments . Thanks for the many links and your proposed connection. How can I learn more about the chemical mediators between brain and immune system? I’ve always assumed the brain is a victim of immune response rather than a driver of immune activation.
Poorly written article. Too “comic-book” in the explanation of the findings. Unprofessional.
I understand what you’re saying. I don’t know if anything is going to change though. If the blog was meant for professionals it would look very different but it’s meant to communicate to people with ME/CFS/FM and long COVID. If it loses some cachet amongst professionals because of the way it’s written, I guess that’s an acceptable compromise.
Agree 100%. As the mother of a Severe ME sufferer, I find myself completely out of my depth reading scientific papers on ME. These blogs are a lifeline, offering plain language for complicated science. I’m not dumb. I had a career as a Marketing Director, but I’m not scientific – it’s very different. Posts like this help to give me hope that research which makes sense is happening.
I sincerely and desperately wish to see research on the horrific brain pain caused by light, sound, and cognitive input like listening to someone talking/ processing words. This brain pain, which I see other Severe ME people bemoan as well, has caused far more suffering for my son than PEM, though he’s 100% bed bound. But I have never seen a single study on it.
Yes, I too wish for research into sensory/processing hypersensitivities including uptake of sound, light, information and – I wish this were mentioned more often because it’s one of my most limitating symptoms – sensitivities to odors/fragrance!
I’ve been diagnosed for 16 years, progressively worsening, and often, including tonight I can’t make sense of the gist. Please keep the “comics”!
Thank you so much for how you present these studies, Cort. Over the years that I have continued to decline, I can still manage to gain knowledge from them, even if I have to come back a few times when I’m in PEM. I appreciate the tone and the content.
CFS is bullshit with all its diagnostic “criteria”. I have chronic fatigue for 30 years but no PEM, what should I do? I bet lotsa people like me. Who said there’s one disease and not 100? These researcher won’t do subgroups, why?
Here’s a hypothesis. There’s >100 minor primary immune deficiencies. Various pathogens invade these people’s bodies and make them their home, wreaking havoc. But, to the medical establishment these people are “immune competent”. Where’s the test that shows that? Instead of studying persistent pathogens and immune deficiencies that allowed them to persist in the first place, these researchers are looking for an Occam’s razor. I guess if you solve only 1/100 of the problem you won’t get famous.
Buchstabe Prof. Scheibenbogen,Charite,Berlin,geht von 3-4 Untergruppen aus.Sie sagt,dass es nicht ein Medikament geben wird,dass allen hilft.Deswegen testet sie verschiedene Medikamente.
I like such molecular data fitting the observed disease patterns. I hope they can get funding to do a larger study, involving many more patients, where severity of disease can be related to the levels of gene expression. This should then lead to pinpointing the transcription factors (and their interactors) that are key to the regulation of the response in healthy people, and eventually therapeutic applications.
Also, a meta-analysis study of multiple transcriptomics studies in ME-CFS patients would be of great interest. Can’t wait to see some bio-information getting his/her hands on this.
Thank you so much for sharing this. The results of this study flies in the face of what most doctors have tried to tell me to do for my CFS/ME, EBV and fibro following two dexamethasone epidurals.
At one point a smug orthopedist told me he would not treat some of the injuries from a car accident (pre-epidurals) until I had six months of physical therapy. OMg, I had to quit after four months because I was so fatigued and in pain. Everything got worse. If the therapist did massage or released the fascia and trigger points, I would crash for days and the tps would come right back. I also got progressively weaker during the process. It was so disheartening.
One thing I did discover is gentle swimming in a warm pool It makes a huge difference (at the most minute level of my muscles) which seems to help overall as long as I don’t overdo.
Trying to understand, are you saying you have ME CFS, EBV, and Fibro from epidural injections for previous car accident injuries? It reads like that and is something I have never heard of before, but I like many need pain relief for cervical bulging discs?
@Trudy, your symptoms/response to exercise relate to CCI, etc, spinal constrictions, reducing the flow of cerebro spinal fluid and preventing the clearance of all the toxins, cytokines, chemokines, antibodies in the CSF & lymphatics, I have ME/CFS/FMS AND spinal stenosis, whiplash x3, falling downstairs x 3 crumpling my neck when myhead hit the doorpost. AND head injury., AND 3 epidural child deliveries.Spinal pain & soreness/ tenderness lasted decades from epidurals. I sleep on a princess & the pea, pile of foam matresses, pillows, and duvets. Nothing is soft enough!Not even clouds! I sleep with a neck roll to help prevent the paresthesia in my shoulders, arms ,hands & thumbs.I forgot the torn rotator cuff. tendonitis,both wrists& ulna nerve releases. metatarsalgia, sinusitis, etc etc. I practice the Perrin Technique, which I have adapted over the years , in the shower, using a soft wash cloth well sudsed with shower gel. I find it best to stand as sitting seems to crumple everything and cause more pain. I have also added some gentle leg stretches whilst I am effluaging face, neck, back, arms , leg & around the large colon in the direction of ‘flow’. I finish with hot, then cold then hot again down the back of the head & spine whilst leaning on a suction grab bar,for stabilityand performing neck bends & strecthes for C6& C7 neck stenosis. Sounds energetic? Yes ,but it takes time. I lose my place can end in tears, & rept too many things & miss others . There good & bad days. short & long sessions & often a long lie down in a cotton dressing gown. a la Staci Stevens . Over the long term it has been a good investment of my energy. I use PEA 6 x 500mg capsules in 3 doses daily, nattokinase, 2x daily, serrapeptase 2x daily, Vit c 5-6 g daily, MSM 3x1g daily, lots of other supplements, but these are the ones that have helped the most with pain, Been a PW ME/CFS/FMS EBV etc coming up to 50 years. I cannot tolerate chlorine swimming pools, the effect on the neck & the sinuses, I would love to try a sensory deprivation magnesium sulphate flotation tank, if I could not hear my tinnitis, blood flow thumping & heart bumping in my head & ears.GENTLE Recumbent exercises for cervical & lumbar spine have helped, lie on a pile of strategetically placed soft pillows, use a neck roll and abduct both the feet( push the heel down and pull the toes up, do this for a count of 2 seconds to begin with and increase slowly over time,) Abducting stretches the back muscles down each side of the spine without too much stress except on the ‘back tendons of the ankles’ so that is why start with 2 secs. Do not do situps or scrunchies!! not good for uterovaginal and rectal prolapse !!!! apologies if this comes over as a rant, not supposed to ,hope it offers some tips & support .
Thank you for this Cort, you rock!✌️❤️
Unrelated sorry:
Does anybody else have Rheumatoid Arthritis in conjunction with an ME/CFS diagnosis?
Was just told about the RA today per labs from doctor.
The gift that keeps on giving…🙅♀️
.I’m trying to stay positive….😆
This is such a groundbreaking finding! For the first time in a long time, I’m optimistic that there may be a treatment on the horizon. Thank you Cort, for the amazing reporting on this site. All CFS patients owe you a debt of gratitude.
One of the dryfastingclub members recommended this article and the findings in the exercise control study correlate exactly to what gets healed with dry fasting. If you’re interested in talking to people that have actually improved and healed long covid stop by the dryfastingclub discord. Cort, I’d love to chat with you all about it if you were interested.
Yannick <- healed severe long covid/ME/CFS of 2 years
Does this mean that supplements that would boost NK activity would help? Or would the herpes just infect them as well? How is it possible herpes can infect NK cells when it’s the NK cells that are supposed to kill herpes? If this it true, well, that explains A LOT.