Can infections trigger psychotic episodes?
This blog was prompted when I learned of a family that had been riddled with chronic fatigue syndrome (ME/CFS), one of whose members began experiencing psychotic symptoms, and ultimately, full psychotic episodes after being given fludrocortisone. Her severe illness had resulted in her existing in a sensory-deprived environment in which she had little social contact.
This person’s story prompted a dive into the intersection between hallucinations and psychosis, and post-infectious diseases like long COVID and chronic fatigue syndrome (ME/CFS); i.e. could her symptoms have been post-infectious in nature? Neither this person nor her family had any history of mental illness.
The outcome was surprising – the data clearly shows that while the risk is low, infections clearly do increase the risk of coming down with these symptoms. Plus, it turns out that the stimuli overload often experienced by severely ill, which results in them living in low stimuli environments, presents another risk factor.
All in all, the data suggests that at least some people with ME/CFS, long COVID and other post-infectious diseases must be experiencing hallucinations and psychosis as a result of their illness. Hence this blog and the poll at the end of it.
Triggers
The Link Between Infections and Psychosis
A 2021 paper, “Viral respiratory infections and psychosis: A review of the literature and the implications of COVID-19“, demonstrated the effects viruses can have on “neuropsychiatric” symptoms. Many of these symptoms (seizures, attention deficit disorder, cognitive issues, uncontrolled anger, migraine, eating disorders, impaired sleep, easy fatiguability, depression, anxiety, other psychiatric issues) are common in ME/CFS and, in fact, ME/CFS has often been referred to as a “neuropsychiatric disorder”. While that’s clearly not a complete description of the disease, it does demonstrate that many of the symptoms of ME/CFS seem to be brain-related.
The link between pathogens and psychosis dates back hundreds of years.
The 2021 paper indicated that reports of infections triggering neuropsychiatric symptoms date back at least to the 1385 German flu pandemic. Indeed, careful reports of past pandemics have always noted a wide variety of symptoms including depression, insomnia, and psychosis. Karl Menninger’s 1919 detailed case series documented the psychotic symptoms triggered by the Spanish flu. (It also found that the psychotic symptoms usually resolved themselves within 5 years.)
You don’t need a pandemic, though, to understand that infections increase the risk of psychosis. Studies indicate that children born to a mother who had the flu during pregnancy have an increased risk of schizophrenia. Viral infections in neonates, children, and adolescents have all been associated with an increased risk of schizophrenia later in life. The effects of infection on the central nervous system appear to be greatest when they occur during critical neurodevelopmental windows such as childhood and adolescence.
The Coronavirus Connection
The coronaviruses are no stranger to these phenomena. Several coronaviruses prior to SARS-CoV-2 were associated with an increased risk of psychotic disorders. Papers published early in the pandemic predicted that the SARS CoV-2 coronavirus’s neuroinvasive properties, plus its ability to trigger a massive inflammatory response, would cause it to produce psychosis in some cases – and it has.
Numerous case reports of people suddenly experiencing hallucinations or psychosis after coming down with COVID-19 have shown up. One young woman with no history of psychosis began acting erratically, told others that it was time for her to die, and complained of seeing and feeling bugs in her hair. She responded well to olanzapine and apparently recovered.
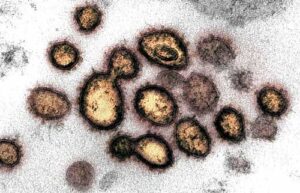
Numerous case reports indicate that a coronavirus infection can, at times, trigger psychotic episodes.
Another young man with no psychiatric history experienced an acute onset of psychotic symptoms (visual and auditory hallucinations, delusions of persecution, and lack of insight) after being affected. He made a gradual recovery and returned to work 12 weeks later.
Shortly after having been hospitalized for COVID-19, another man with no history of psychiatric illness began experiencing visual, visceral, and auditory hallucinations (hearing the voice of God talking to him, feeling demons inside his body), delusional ideas (the apocalypse will come soon, he was on a special mission from God), etc. He had a good response to antipsychotic treatment and was discharged with a diagnosis of acute and transient psychotic disorder.
Another 26-year-old woman with, again, no history of psychiatric disorders, presented with severe psychotic symptoms just days after she had apparently recovered from a mild COVID-19 infection. Her symptoms persisted for approximately two months, after which she was able to discontinue lithium and quetiapine and return to full-time work.
Larger Studies
The coronavirus pandemic has, thankfully, spurred the first detailed, large-scale examinations of the effects of infection on psychosis. Larger studies have confirmed that while the risk is low, COVID-19 infection increases the risk of long-term psychotic disorders. While the rates of common psychiatric disorders increased immediately after the infection in one study, they returned to normal 1-2 months later. Other, more severe neurological problems, however, such as psychotic disorders (as well as dementia, epilepsy, and cognitive issues) remained elevated two years later.
The Effects of Sensory Deprivation and Isolation

Sensory deprivation and isolation can increase the risk of hallucinations.
The sensory deprivation that people with severe ME/CFS can face presents a risk factor for hallucinations. People with severe ME/CFS who are intolerant of sounds and lights live in a world that their brains are poorly adapted to. Our brain is adapted to reacting to stimuli – lots of it – and when those stimuli disappear, it is literally at a loss as to what to do.
After ME/CFS put Dan Moricoli into a coma-like state for months, he found that – particularly when he was under stress – his speech would become alarmingly slurred and his arms would suddenly flap around, sometimes even hitting him in the face. His neurologist believed that the lack of stimulation over time he’d experienced had caused his nervous system to crack up. (Despite his severe symptoms, Dan completely recovered from ME/CFS).
Dan’s reactions to stress bore some similarities to the inability of Whitney Dafoe’s brain to tolerate even the smallest stimuli. He reported:
“I couldn’t tolerate any colors or patterns on them (shirts). I also became sensitive to text like logos or labels on things because it is impossible not to read text that you see; it is something we do instinctually at this age. Reading required more mental energy than I had and caused a mental crash. “
While very severe patients like Whitney must be protected from even low levels of stimuli, it should be noted that it doesn’t take long even for a healthy person kept in those conditions to begin to experience some pretty strange events.
Take Richard Alati’s case. His room was kept in darkness, and few sounds were allowed to intrude, leaving him totally isolated. Alati was not a severely ill ME/CFS patient. He was a professional poker player who’d bet $100,000 that he could survive 30 days alone and in darkness in a small room with a refrigerator and bathroom. He made it 20 days – he’d begun experiencing hallucinations on the 3rd day.
In 2008, clinical psychologist Ian Robbins isolated six healthy people for 48 hours in soundproofed rooms in a former nuclear bunker. The results were predictable – lacking their normal sensory inputs, their brains went a bit crazy. Some suffered from anxiety, extreme emotions, paranoia, and a significant deterioration in their mental functioning. Bizarre hallucinations showed up: people saw thousands of empty oyster shells; zebras; tiny cars, fighter planes buzzing around the room, etc.
Autoimmune Reactions
An autoimmune reactions can produce psychosis. Studies indicate that people with multiple sclerosis and lupus have higher frequencies of neuropsychiatric symptoms, including psychosis. Autoimmune encephalitis (AE), for instance, produces inflammation in the brain that produces neurologic and/or psychiatric symptoms. If a neuropsychiatric form of lupus has been distinguished, one wonders why a more neuropsychiatric form of ME/CFS or long COVID would not exist as well.
Anyone wondering about the ability of an autoimmune reaction to produce dramatic, off-the-charts psychotic symptoms should read Susannah Callahan’s book “Brain on Fire: My Month of Madness“.
Callahan was a young, healthy, news reporter in New York City who came perilously close to being permanently locked in a psychiatric word. MRI, CT and viral assessments were negative, but an alert doctor who did a brain biopsy found that massive numbers of microglial cells were attacking her nerves. She was eventually diagnosed with a recently discovered disease – anti-NMDA receptor autoimmune encephalitis – and was given massive doses of steroids, followed by plasmapheresis and IVIG. She returned to complete health a year later.
Drug Reactions
Odd drug reactions are another potential source of psychosis. Case studies of drug-induced psychosis, in fact, are so prevalent that it almost seems like any drug could produce psychosis in the wrong person.
Fludrocortisone and then later methylphenidate appears to have triggered/exacerbated the psychotic symptoms the young woman with ME/CFS referenced at the beginning of this blog experienced.
Recent reports of drug-induced psychosis include a single dose of ibuprofen that produced tunnel vision and altered consciousness, a rapid zolpidem withdrawal that resulted in hallucinations, and an anticancer drug letrozole that produced hallucinations, a monoclonal antibody (dupilumab) that triggered visual hallucinations, disorientation, cognitive decline, and behavioral changes.
One case report suggested that ingesting large amounts of Coricidin HBP Cough & Cold tablets (Triple-C) (to get high) resulted in psychosis and hallucinations in one person. Clarithromycin apparently caused closed-eye hallucinations in one woman. The list goes on and on… the antiviral acyclovir, the anticonvulsant Lyrica, the antibiotic linezolid, and pseudoephedrine.
Most of these cases are very rare and only occur when the right central nervous system meets the wrong drug. Some drugs, though, can produce hallucinations more regularly. Amantadine, for instance, produced hallucinations in 24% of Parkinson’s patients. The triazole class of antifungal drugs appear to be fairly adept at producing hallucinations and putting patients in a “predelirium” state.
As a whole, antibiotics appear more adept at causing hallucinations than other classes of drugs. Of the rather notorious fluoroquinolone antibiotics, levofloxacin reportedly has a greater tendency to cause “psychosis, auditory, and visual hallucinations”. The antibiotics most frequently associated with hallucinations, though, appear to be cephalosporins and sulfa drugs.
The effect is more common in patients taking multiple medications. “Just why antibiotics cause hallucinations is uncertain,” said Dr. Fraunfelder, “but numerous patient reports document disturbing hallucinations or vivid nightmares associated with taking antibiotics.
Some commonly used drugs in ME/CFS/FM including fludrocortisone, propranolol, atenolol, Eszopiclone, Zolpidem, aspirin, and oxycodone have been reported to trigger hallucinations or other psychotic episodes in small numbers of people.
THE GIST
- Can infections produce psychotic episodes? That was the question that came to mind when I learned of a young woman with severe ME/CFS who began experiencing hallucinations and severe psychotic episodes.
- It turns out that not only does infection have a long history of inducing hallucinations and psychotic episodes in some but the sensory-deprived environments that people with very severe ME/CFS can find themselves in present another risk factor.
- Psychosis can present itself in a variety of ways including hallucination (seeing, hearing, feeling things that aren’t there), delusions (unable to separate fact from fiction), jagged, illogical thought patterns, extreme paranoia and anxiety and others.
- Coronavirus-induced psychosis was predicted and numerous case reports and studies indicate that it has happened. Studies suggest that while the rates of milder psychiatric illnesses such as mood disorders return to normal after two years, the rates of more serious illnesses such as psychosis remain elevated.
- Because our brains were developed to constantly interact with stimuli depriving them of that stimuli leaves them at a loss. Putting even healthy people in an environment devoid of stimuli can rather quickly produce a bizarre variety of hallucinations.
- So many drugs have been reported to induce at least temporary hallucinations and other forms of psychosis that one wonders if any drug is completely exempt from this. Case studies of psychosis from such innocuous drugs as ibuprofen and cold and flu tablets have been published. Some commonly used drugs in ME/CFS/FM including fludrocortisone, propranolol, atenolol, Eszopiclone, Zolpidem, aspirin, and oxycodone have been reported to trigger hallucinations or other psychotic episodes in small numbers of people.
- Many different factors – reduced oxygenation of the brain, direct invasion by a virus, a breach of the blood-brain barrier by immune cells or cytokines, immune dysregulation that results in low-level inflammation – have been posited to trigger psychosis.
- The MOOD Stratification EU research group which focuses on neuroendocrine-immune causes of psychosis believes that immune testing will quickly lead to more personalized and effective treatments for psychosis.
- If you’ve experienced psychosis or personally know someone with ME/CFS, long COVID and/or related diseases please take the Infection, ME/CFS, Long COVID and psychosis poll found at the bottom of the blog. All entries are anonymous.
Causation
An inflammatory model of psychosis has been developed. Reduced oxygenation of the brain – surely a possibility in ME/CFS – could cause a brain disease (encephalopathy) that produces neuropsychiatric symptoms. Direct invasion of the CNS by a virus, or a breach of the blood-brain barrier by immune cells or cytokines from the periphery, could produce an inflammatory state in the brain that destabilizes the microglia. Jarred Younger is currently assessing whether immune cells from the body have made it into the brain in ME/CFS.
An infection and immune activation that causes hypothalamic-pituitary-adrenal (HPA) axis dysregulation (cortisol elevation, problems with dopamine and glutamate neurotransmission) has also been linked to psychosis.
The “MOOD Stratification” EU research program posits that T-cells’ failure to rein in low-grade inflammation triggers an inappropriate stress response that throws the limbic system out of whack. The white matter changes that occur in the brain, in turn, produce mood disorders and the like. This state leaves one prone to post-infectious illnesses and autoimmune disorders.
Treatments
Antihistamines?
Besides antipsychotics, one review suggested trying anti-histamine drugs to combat neuroinflammation. That was interesting given that the one medication that really helped Whitney Dafoe – Abilify – came out of a search for better antihistamines.
Recent rodent studies suggest that Abilify may also “impact insulin, energy sensing, and inflammatory pathways” in the hypothalamus. If Abilify is impacting neuroinflammation, hopefully more effective “Abilifys” are on the horizon as efforts to find more effective neuroinflammation busters have ramped up in several central nervous system diseases.

The Mood Stratification effort in Europe believes immune-based, personalized treatments are around the corner.
The MOOD Stratification research group believes that personalized treatments based upon each person’s immune signatures are not far off. They present fictive cases of four patients experiencing some familiar symptoms (severe fatigue, loss of energy, irritability, sleeping problems, and difficulties with concentrating). They contrasted the treatment options these patients would likely have received in 2016 (SSRI, lithium, amitriptyline, electroconvulsive therapy) and then looked forward to personalized treatments they might receive in 2024.
Immunological testing revealed that an SSRI was appropriate for one, an SSRI plus an anti-inflammatory agent (e.g. anti-TNF) and a T cell enforcing therapy (e.g. low dose IL-2 therapy) looked like it would work for another, an SSRI and an anti-inflammatory agent (e.g. low dose aspirin) was given to the third person, and the last was given an SSRI, lithium, and anti-inflammatory therapy, e.g. anti-TNF.
Health Rising’s ME/CFS and Long-COVID Hallucination and Psychosis Poll
A number of factors – infection, sensory deprivation, isolation, a drug reaction, and infection-induced autoimmunity – could increase the risk of hallucinations and psychosis in post-infectious diseases.
Psychosis, ME/CFS, and Long-COVID Poll
If you’ve experienced these symptoms or personally know someone who has, please take the poll. Please note that your responses are completely confidential.






Your symptom list only allows one answer – is that intentional?
Completely unintentional! Thanks for letting me know. It’s been fixed 🙂
Very interesting. I’ve long felt that my issues are due to inflammation in my brain. I take antihistamines and resveratrol to help.
I had my genome tested and came back with many many markers for schizophrenia, yet we have no family history and I have no symptoms. These were acquired mutations, and I’m convinced it’s related to viral infections that crossed the BBB. The virus brought on my ME/CFS. It was reactivated when I had a COVID vaccine, and I ended up with viral meningitis.
Keep up the great work, Cort!
Wow – acquired mutations related to schizophrenia – probably brought on the infection – that puts a whole different light on things. After I looked at all the “neuropsychiatric” symptoms associated with ME/CFS, I thought why not psychotic symptoms in some people as well.
Psychiatry is more about guesswork and opinion than SciencE IMHO
LIZ
What genome test do you use for this?
I used 23 n me, but put the results through 5 different platforms, Prometheus, self decode, genetic genie, seeking health and I can’t remember the last one. Brain fog!
This article is especially interesting as some research has suggested that aripiprazole successfully acts on schizophrenia in ways that could also help with Long COVID: https://www.frontiersin.org/articles/10.3389/fphar.2021.646701/full
18+ years ago, approximately 3 weeks after experiencing a severe, 3-day, flu-like illness, I was diagnosed with an episode of “Organic Psychosis” and went through a series of testing the next day (Brain MRI’s, EEG, Carotid Ultrasound, etc.). All test findings were negative. In researching my symptoms, I found that they correlated with those symptoms found in “Acute Delirium”, more than symptoms of “Acute Psychosis”. To this day, I still have problems with Cognitive Impairment, that I did not have before that acute, viral illness 18+ years ago.
I do not deny the truth of these findings…just a caution there is still a lot of guesswork going on in untangling the nervous and immune system.
My concern here that lesser psychiatrists will use this to persist with their most harmful and hurtful idea that ME/CFS IS a “persistent delusion”.
They can then lay on the full psychiatric treatment of not listening to the patient and enforcing a regime of psychiatric drugs to which thE ME/CFS Population may be allergic.
I speak of Australia.
Liz, I apologize but I did not try to imply that my acute or long term situation was, or is, a psychiatric condition. More so, over the years my Providers have all pretty much found consensus that my condition is in line with today’s definition of ME/CFS. What I tried to describe was that my initial diagnosis of an acute psychosis quickly sent me down the path of a mental disorder, and the treatment plan was geared towards behavioral medicine treatment for the first few years. I don’t feel that the cognitive impairment I still experience today, is the result of any acute insult I experienced so many years ago (e.g. a stroke, as was my Provider’s first thought to be the source of my acute symptoms).
I hope this clarifies things a bit better. I am not always the greatest with my explanations. 🙂
No worries Mike
Take care
Lix
There is a reason why we use solitary confinement as a punishment – we have long known it’s adverse impact and use it as a deterrent.
Sensory deprivation is used as a form of torture, aimed at breaking down someone’s sense of self and resistance to answering questions.
It’s therefore no surprise at all that people isolated by ME/CFS, FM or other illnesses start to experience psychological symptoms: anyone would, as the 2008 nuclear bunker experiment makes clear.
I am currently taking Ketotifen (Dr. Bonilla/Stanford) and I notice that since taking it, at night, I am having hallucinations of seeing objects that are not there, or something is there but my mind will think it is something else (like a shadow is a animal). These are new, but fortunately mild so I haven’t discontinued the drug. This is the second go round with Ketotifen. Hope springs eternal as Dr. Bonilla prescribed it yet again even though it didn’t help the first time. He has said, more than once, that he recommends a person take an unsuccessful drug for at least a year before judging its effectiveness. !?!
With Abilify, I wasn’t seeing things but could barely think or talk. I became drug stupid even with a very low dose. I do often have exaggerated or unexpected side effects from medications. Usually I don’t naturally have brain fog.
I read a description of ‘highly sensitive people’ and think it fits me. These people experience emotions and reactions (including pain and drug side effects) to a much grater degree than ‘normals.’ Often their ANS is very ‘touchy.’ Also there is evidence that red heads have different drug reactions than others. Although I don’t have red hair proper, (blond with reddish highlights) everybody else on both sides of my family does excepting my father. Perhaps this influences my responses.
And as an aside, I read a study that found reactivated viruses (EBV etc.) were found in fatigue illnesses like ME/CFS rather than inflammation. Sorry but I didn’t take note of the who, when and where of this study but it was not in the U.S. and size was several hundred patients.
Nancy,
I was on Ketotifen for a couple of years. It “does something” (one presumes to do with the mast cells) but does not address anything substantially or permanently for ME/CFS in my experience. I actually found that it masked symptoms and was even counter productive as far as avoiding PEM goes.
Two things – ketotifen didn’t take a year to work for me (more like 60-90 minutes) and I did not have anything like psychotropic side effects. I really think that if possible you should talk with Dr Bonilla again or get another opinion on the suitability of that drug for you.
Lono,
I so appreciate your response. Truth be told, I’ve had a fraught relationship with Dr. Bonilla. I believe he is very well educated and has mostly good intentions, but we don’t communicate well. He frequently cuts me off so I cannot fully communicate my questions or comments or he rapid fires his questions too quickly for me to respond. Many times, because of his accent, I have to ask him to repeat himself. There is a condescending attitude that permeates our encounters. He often seems disorganized. I ask about other treatments and he brushes me off with, ‘It’s not part of the plan.’
When I asked ‘Why ketotifen?’, he replied it’s an anti-inflammatory. Of course I did research and really, that’s not the entire story. I do have Ehlers-Danlos but do not have MCAS symptoms. When I asked for a more in-depth reason he said ‘I’m trying to help you.’
He has given me various medications for these past few years and nothing has helped–nothing. Even pacing is problematic. Next he mentioned some sort of DMARD used for RA in addition to ketotifen. Sometimes I think I should just stop seeing him, but then again I might miss something that really might help.
I’ve had same negative experience with Dr. Bonilla. I left the intake thinking, what was the point of that? He seemed very dismissive of points of view other than his own…
Ray, I appreciate your validation. Sometimes I wonder if I’m just a confrontative person, but with all the mis-guidance I’ve encountered within the medical system, perhaps I’m just overly sensitized.
My other gripe is that he charges Medicare over $900 for each encounter. With the low level of value, I think that the government is being robbed under the pretext of receiving care. And my care does not seem to be individualized.
It’s more like Bonilla is conducting his own research on various medications–like Abilify–which later morphed into a paper which extolled its effectiveness. I was not one of the people who it helped (bad side effects) and so I argued with Bonilla who wanted me to stay on it for many more months so I wouldn’t become part of the negative statistic.
And the way he gathers statistics…I could go on… Needless to say I am not impressed with his acumen–at least in dealing with patients.
I’m surprised that you are commenting on such an old blog. I often think that once a blog is a few months old, then nobody comments and few read them again.
Ray, hope you find some things that work for you!
Some years ago I asked someone about the incidence of degenerative disc disease in people with ME/CFS. There seemed to be no data back then. But recently in the poll involving long Covid one item that could be checked was for spinal stenosis. Well, I have degenerative disc disease. It was diagnosed long before I was officially diagnosed with ME/FM. I’d had it for years and with it was spinal stenosis – twice. I had to have 2 spine surgeries and could have had 3 but I think I experienced a miracle and never had to have the 3rd. I continue to have low back pain but nothing compared with the horrific nerve pain I experienced prior to the 2 surgeries. Is there now an accepted link?
Nancy that’s interesting. I haven’t had covid
but do have long term me/cfs, osteoarthritis and spinal stenosis.
I don’t know if it’s “accepted” but there’s certainly a potential link.
https://www.healthrising.org/blog/2019/05/29/spinal-stenosis-chronic-fatigue-fibromyalgia/
Thanks Cort I must have read the 2019 article but wasn’t aware I had spinal stenosis then. In fact getting to the stage of seeing a neuro surgeon in September has been over the last few years like swimming in mud. Hope I get some answers as I can only just walk a few metres now. FYI, In Australia,; me/cfs/ fibromyalgia, overly mobile joints, osteoarthritis, spinal stenosis.
Adding something here re the psychosis questionnaire I filled it in. I believe my hallucinations, very scary ones were purely caused by amitryptiline and Duloxetine at different times but I seem to be super sensitive to certain medications so was that caused/enhanced by the illness or the drug? Hope this is able to be understood.
I have been diagnosed with ME. I also have spinal stenosis and degenerative disc disease.
I previously posted that I experience ME and spinal stenosis and degenerative disc disease. I should add that my ME seems to possibly be a result of mono but maybe also hormone treatments for infertility. I’ve been sick for 8 years. I began experiencing symptoms of psychosis about four months ago. These symptoms have been frightening and have really added to the already very upsetting debilitation of ME. I am grateful for any research that is being done to add to our understanding of these things. My doctors know almost nothing about ME (just enough for the rheumatologist to diagnose me, but my primary care doctor and psychiatrist had not even heard of it before).
I invite everyone to visit the website of The Neuroimmune Foundation, neuroimmune.org. There truly is a great deal of research happening in the sphere of inflammatory brain disorders. The Neuroimmune Foundation each May hosts the virtual Inflammatory Brain Disorders Conference, which features researchers’ presentations on ME/CFS, POTS, Long Covid, PANDAS/PANS, ASD, and EDS — all conditions linked to neuroimmune processes and many of which, though they have psychiatric presentations/symptoms, are firmly rooted in immune disfunction. The Foundation has also partnered with donors to fund a Fellowship with UCSD to study commonalities/differences and look for avenues for treatment. The Neuroimmune Foundation communicates frequently with the folks at OMF. The past three years of conference presentations can be viewed at neuroimmune.org. I am a firm believer that any insights into any one of these conditions is helpful to all. Though we all wish the science was moving faster, I want to reassure everyone that it is, indeed, moving. And the research increasingly shows that much of what we consider “mental illness” today is immune mediated and will be treated much differently in the future.
Exciting stuff! Thanks Mary for sharing this. 🙂
Agreed! <3
Thank you!!!
Hi Cort, I find it an “awfull topic”. I am not saying that it totally can not happen. But like the poll, you do, not asking how many of us do not have it. It gives no real % of who has it (how many) and who not(how many) on every level of illness. That some of us get depressed, hopelous, is no miracle. How long do we allready ait for real tests and treatments? How many broken promises? And in what circumstances do some of us live? And also, i hope they do not read it in my country because it is still cfs only and get and cbt and falls beliefs, psychosomatic while some people are here fighting so hard to get finally recognition.
I wrote a while ago to the DecodeME study and asked questions. i got the next day answers. By the way they still work together with presicionlife. It is the only largest study worlwide. they gave me also a link of the allready 1700 and a bit of questionaires they had. for the completion of the study, if i remember correcty we need to wait untill summer 2024. In the questionaire there was a verry verry verry small % of psychosis. just like other deseases like addison, etc I can not remember how small, but really not high.
I really hope that psychiatrist do not fall now in other countrys over this blog. and the poll. Like i allready wrote, we are allready here psychosomatic, falls beliefs, etc
i would have liked more to read when finally Nancy Klimas would starts finally her treatment trials? Do you know? Or other treatment and research stuff?
if you would have asked for post traumatic stress syndrome without the “post” because there is still nothing I could have understood. How they (professionals/medicine) treated me, harmed me over decades just like so many other patiets, what i all lost in my life over decades, i just lost “my life” i could have understood it. But this? by the way, how many psychosis patients do not have PEM, etc
the poor GWI vets where also long called psychiatric patients. Serve your country, get ill and then happens that. Luckilly with finances that has now changed as far as I know for research.
ps by the way, with the DecodeME study and cooperations, if there excist allready a med(s), it can go fast. That is what I, many of us need.
Well said Pom..caution here
I assumed that we would only get a few responses – and for a poll we didn’t get many at all – but we do have 56 responses, which is more than I suspected.
I’m not really worried about the CBT interpretation of ME/CFS or ME/CFS being thought of as a psychosomatic disease because psychosis is in another ballpark entirely. Depression is not unusual at all in the context of a chronic illness- any chronic illness – but psychosis is really unusual.
I think it points out the effects a virus or infection can have on the brain. A few people experiencing psychosis as a result of an infection actually made sense to me after I looked into it.
As to the Klimas study – she recently said it was starting. She’s said that before but hopefully it finally is.
https://www.healthrising.org/blog/2023/06/12/moonshot-ebv-chronic-fatigue-syndrome-inim/
Hope not too many of us get these symptoms on top of the rest!
I was wondering when Dr Jarred Younger would get mentioned again – is there any info on how his work is going so far? Last I heard (ages ago) he was weeks away from putting patients through a new imaging system that would say if the immune cells were present in the brain – presumably the study you referred to above. Things seemed to be moving relatively quickly at the time, so I was hoping we’d have some results by now. Any updates available on how it’s going/when we’ll see results? Thanks
if i can, i follow him on fb. I always type jarred younger ME/cfs fb (facebook), I do not know why, but there are 2 fb’s I always see. 1 is updated. he gives there for excample youtube’s, mention things, etc
Great idea Konjin, thanks! Didn’t realise he was on FB, I’ll take a look 🙂
you are welcome!
He is working on this. My guess is that we will hear more about Younger’s findings by the end of the year.
Thanks Cort!
Thank you so much. I cannot begin to tell you how validating this is as my young person with Severe ME/CFS has been struggling with neuro psychiatric symptoms. We’ve not been able to access any medical help in the UK for these additional horrible symptoms. There is fantastic support from the PANS/PANDAS community but this is yet another illness that is so very mis-understood and the NHS won’t even recognise it. The P in PANS/PANDAS is also problematic as it stands for paediatric and yet, there are many patients who are older – the symptoms don’t magically disappear once you reach eighteen!
HHS just issued this last month. https://www.hhs.gov/about/news/2023/06/21/hhs-issues-advisory-mental-health-symptoms-and-conditions-related-long-covid.html#:~:text=Long%20COVID%20can%20have%20devastating,to%20the%20advisory%20issued%20today.
Please everybody..
Psychiatrists round here call ME/CFS ”
“a persistent delusion”
I am alarmed by this debate Cort .
Please Note I admire enormously what you usually do on Health riding blogs.
I think they’re using “delusion” in a different sense than is being used here. In this blog, it’s a more technical term that refers to things like hearing voices from God, believing that aliens are tracking them, or that devices have been implanted in their brains that are making them act in a certain way. Really out there stuff.
I think it’s helpful for people who have experienced these issues or have family members who have to understand that they can be the result of infection or autoimmune response or some other biological factors.
Totally agree..just wary of feeding stuff to the psych group..many are not up with Neuro immune function..just use old assumptions along old psychosomatic lines. also not many psychs an psychiatrists are really across The current excellent research in this area or is this only in Oz.
Delusions don’t start suddenly do they? I ask because I don’t know. But I do know that I went to bed one night nearly 40 years ago perfect happy and healthy with 2 grown sons and a great job. I awoke the next morning with vertigo. I thought it some wierd thing that would go away if I just went about my morning as usual by making my coffee, grabbing something to eat, etc. However, I was so dizzy I could barely walk. I had to hang on to things to get around. I finally gave up and called into work that I was sick with the flu and wouldn’t be in. The vertigo took days to dwindle down to a persistent but mild dizziness and went back to work on Monday.
I was never “normal” again. I read everything I could get my hands on. I knew I was not crazy because I began having so many symptoms I had to start writing them down as I knew I’d have to see a doctor eventually. Seeing a doctor was fruitless. I drank a lot of ice water for the sore throats and coughs (no fever). Those were the first of many symptoms you all here with ME are very familiar with.
After 10 years and a move to Charlotte (my husband’s idea after we both were forced to retire), I found Dr. Lapp. He diagnosed me with ME/CFS and fibromyalgia. Of course, most in the large medical community of Charlotte, NC did NOT think Dr. Lapp was legit. To this day its dismaying to know how many still don’t believe ME/FM is real.
My point here is that when something starts so suddenly and within a week a myriad of symptoms suddenly come about, its not delusional. Its just unknown to many in the medical field who are ignorant of its true nature. I learned that it wasn’t new. There’s a long history of this disease and its many different names.
Yes Nancy..thanks for this affirmation and clarification
I may seem like a research dinosaur but some of this discussion has made me very uneasy.
Just listening to an eminent Parkinsons researcher.
Anti psychotic medication can induce
Parkinsons so if u join the dots.
That’s all folk
..beware of medical politics…liz
In 1984,I was diagnosed with chronic encephalopathy and immune deficiency by two immunologists (one a prominent practicing immunologist and the other a professor of immunology at our local university). They ran extensive immune studies and my results were very scary…a very severe depletion of T cells.
My symptoms seemed to jump around to different parts of my body, so much so that I remember asking my doctor, “Are you sure that I am just not crazy?”.
He said, ” not with immune abnormalities like you have”. Dr. K is decreased, but I wish I could hug him for this reassurance.
I am relatively certain that most ME/CFS patients never had the battery of immune studies that I had so early in the illness.
Fortunately, the severity of my immune suppression improved over time, not so much for the chronic encephalopathy.
Your brain is like any other part of your body and can be affected just like your muscles, pancreas, liver etc. Having brain symptoms shouldn’t be treated as a sign of a psychosomatic illness.
Hi Cort,
I recently came across a study from 1937 which examined the blood volume status of schizophrenics. It found a reduction of 20% in plasma volume and 12.5% in total blood volume, which could very much be what is observed in ME/CFS. (Paper was ‘Observatons on the circulating blood volume in schizophrenia….’ by Haffron and Finkelman). To my knowledge, this is not a question that has been studied since.
Were those really ME/CFS patients whose reduced cerebral blood flow resulted in biologically-driven personality changes that resulted in them being falsely diagnosed with schizophrenia? Or can both conditions lead to low blood volume? Or is something else going on?
I found the study mind-blowing. I’ve never experienced hallucinations or voices but when I am badly ill with ME, I do withdraw socially, have flat emotional affect, and can feel hostile (though try not to act on it).
I found the blog very interesting, thank you.
Wow…What an interesting connection! I had never heard of that and thanks for passing it on :). Being really PEM’d definitely produces psychological changes and one of the three factors that can distinguish PEM in ME/CFS – if I remember them correctly – is low mood.
At times, though, I’ve gotten very ADHD’y, irritable and start saying things I wouldn’t ordinarily say…my normal social filter gets considerably weakened 🙂
You are welcome, Cort! I also find I am ADHD because of this illness and it gets worse when I crash. I manage to control my social filter during PEM but my inner monologue is certainly blunter 😉
Thanks Cort, for this blog. I found it very interesting. I am also one of those who experienced extreme paranoia like anxiety once the illness had really set foot in my brain. Under the current state of research I believe that I have HHV6 brain inflammation episodes because they can be stopped with aciclovir. And I think that the extreme anxiety is a direct consequence of the inflammation of parts of the brain that regulate anxiety. Just as Bupesh Prusty has shown in one of his studies about post-mortem brain tissue of ME/CFS patients.
As a long time meditator I was thankfully prepared for experiences of extreme anxiety and paranoia. Earlier in my life I had already learned to overcome social anxiety and meditation and the teachings of the Tibetan Woman Warrior on how to deal with fear had served me greatly. I can recommend them fully. They can be learned in the books of Pema Chödrön for example.