The ME/CFS/FM/POTS/Long COVID Septad – a Treatment Roadmap
From Unraveled A Patreon Broadcast from Dr. Kaufman and Dr. Ilene Ruhoy
The Unraveled Podcasts: two experts discussing complex chronic illnesses over dozens of podcasts.
Dr. David Kaufman MD – A published researcher as well as physician, Dr. Kaufman spent many years immersed in HIV/AIDS research and treatment in New York serving in various Directorships. From 1988 to 2005, he was the prinicipal investigator in 15 HIV/AIDS trials. He has over 35 years of experience in healthcare administration, management, and research, and his clinical experience spans Internal Medicine, HIV, Lyme Disease, and chronic illness.
In 2012, seeking something new, he moved to the San Francisco Bay area and began to focus on chronic fatigue syndrome and allied disorders at the Open Medicine Institute. In 2017, he and Dr. Chheda opened the Center for Complex Diseases focusing on ME/CFS, dysautonomia, autoimmune diseases, chronic infectious diseases, small intestine bacterial overgrowth, and mast cell activation syndrome (MCAS).

Dr. Kaufman – an internist – and Dr. Ruhoy – a neurologist – began a more or less weekly Patreon channel called Unraveled: Understanding Complex Illness in December of last year, in which they discuss disorders like ME/CFS, hypermobility disorder, mast cell activation syndrome, small fiber neuropathy, postural orthostatic tachycardia syndrome (POTS), infections and environmental exposures. The podcasts include some live interactive sessions in which patients/caregivers can ask questions. It’s a rare chance to see two experts who are deeply immersed in these diseases publicly dig into their many different aspects. They state:
“We are two docs from New York now working in Seattle. As New Yorkers, we talk a lot, we talk fast, we interrupt each other, and we have a lot of fun. While we are passionate about our work, we also love to laugh and hope you will laugh with us as you learn”.
When I asked Dr. Kaufman if it was okay to cover some of the podcasts on Health Rising, he said it was, and added this:
“Our goal, our reason for doing this, is to get the word out there and not just to patients but to their families and especially to other physicians. I am quite passionate about the desperate need to recruit more physicians to this work both for ME/CFS and the exploding epidemic of Long Covid. In addition to pulling/luring physicians into this work–which is incredibly challenging and rewarding–I want to help educate primary care physicians since they are–or should be–the backbone and foundation of healthcare in general and particularly for this patient population.”
If it’s appropriate, please share the podcast with your doctor! Those who watch the podcast will surely be encouraged to see two such intelligent and likable doctors discussing them in such an easygoing and informative manner – I certainly was.
These doctors are on the cutting edge. Seeing patients day in and day out, they are, in many ways, ahead of the science. Their unique experience shows up in their framing of the key, interconnected factors present they believe permeate these illnesses. (Note how many of these were hardly in the discussion even for ME/CFS/FM experts ten years ago). Of the seven factors of the Septad, only four (infection, dysautonomia/POTS, autoimmunity, small fiber neuropathy) are being pursued with any vigor at all in ME/CFS research.
These are, of course, their own views, and other doctors may view these diseases differently. Readers should also note that the following is attached to the beginning and end of every podcast.
If I remember correctly, subscribing to the podcast on Patreon costs $9 a month with a discount for a year. (If you’re cash-strapped, you could subscribe for a month once or twice a year and catch up on the podcasts in that way.) Check out the Unraveled podcast here.
The Septad – Podcast #3, January 1st 2023
The Septad (or septet :)) presents a “A classic set of concerns that these patients present with” Dr. Ruhoy
An Origin Story
Dr. Kaufman reported that about 4 years ago, 20 doctors got together to talk about MCAS and set up listserv. Within 2 or 3 months, Andy Maxwell, an East Bay cardiologist – “a totally brilliant guy” – puts an email up asking if every mast cell patient had these characteristics. The light bulb went on and Kaufman realized that his patient had these characteristics…So emerged “the Septad”.
Kaufman stated that the Septad “creates a map that allows the physician…to organize what I’ve heard in a much more usable and actionable way” for patients with chronic illness. The seven all interact – they are all connected and come together to create these diseases.
#1. Hypermobility Syndrome
“What we don’t appreciate enough about connective tissues is that they are everywhere” – Dr. Ruhoy
Kaufman and Ruhoy went way beyond the conventional hypermobility (the thumb bent back to the wrist type of thing). Most of the hypermobility they’re talking about is invisible. The connective tissue that are affected are everywhere – they line our gut, our nerves, our muscles, our brain…They keep our organs in place.
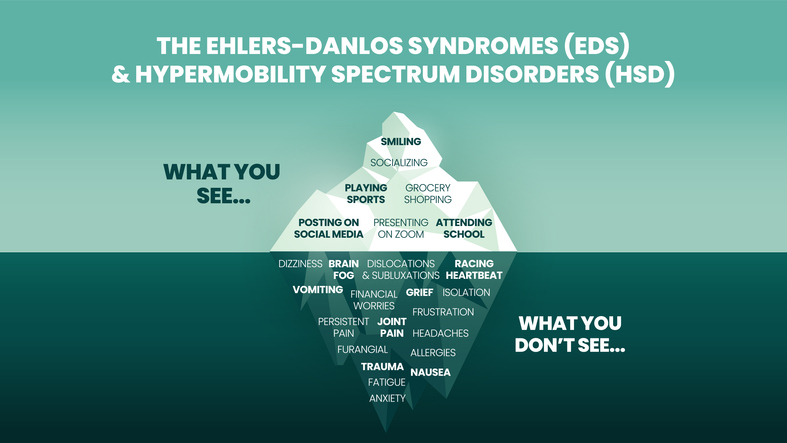
The iceberg model of Ehlers-Danlos Syndromes (EDS) and Hypermobility spectrum disorder (HDS). Joint hypermobility can cause many problems.
Their conception goes way beyond how flexible you are; you don’t have to be really flexible to have a connective tissue problem. The converse is true – being really flexible doesn’t mean that you have a connective tissue disorder either – you can be hypermobile and be completely healthy – check out the gymnasts in the Olympics. (I’ve heard the same is true for POTS. Some people with high heart rates when upright are completely healthy as well).
Being hypermobile only becomes a disease state when the other things (infections, contaminants, etc.) trigger an inflammatory response that targets the connective tissue. It’s the other six things that turn hypermobility into a disease state – and it all starts with inflammation…
#2. Mast Cell Activation Syndrome/Mast Cell Activation Disorder
“Mast cell activation is a critical part of the septad.”
A mast cell that’s ready to pop? While mast cells can emit 1000s of substances, the blue blobs are filled with histamine.
Because connective tissues just happen to be filled with lots of mast cells, the connective tissue issue leads right into the second spoke of the wheel so to speak – mast cells. The skin, gut, nasal mucosa – that are exposed to the environment and stretch and move – are filled with mast cells. They are also part of the innate immune system = first responders. Any kind of traumatic event can call them forth.
Mast cells are an ancient part of our immune system and they don’t produce just histamine. They contain 1000s of chemicals and if they get annoyed, they can dump them all into the bloodstream.
Dr. Kaufman suggested picturing millions of mast cells releasing thousands of chemicals – many of which are pro-inflammatory and some of which damage the connective tissues – throughout your body and you get a picture of how impactful mast cells can be. Mast cell activation, then, “a critical part of the septad”.
For more on mast cells:
#3 Postural Orthostatic Tachycardia Syndrome (POTS)
“I think POTS is one of the greatest drivers of their illness. It’s vastly underrated and misunderstood… and until I fix or manage, I should say, their POTS, I can’t make progress…and I can’t deal with other things. I can’t treat their infection until I get their POTS down.” Dr. Kaufman
Ruhoy remembered when POTS was thought to be a more psychological disorder. Not so anymore. There are several different types of POTS – if your heartbeat only goes up 22 beats, you can still have POTS. If you stand up and your rate goes from 52 to 72 and stays there – that is not normal. Don’t let your doctor tell you that. Your brain is not getting enough oxygen.
Dr. Kaufman really emphasized how important he thinks POTS is:
“I think POTS is so beyond important. If you as a patient say something about POTS and the doctor doesn’t know about it or doesn’t believe in it – you try to finish quickly and get out….there’s no point in continuing.”
As an editorial aside, he said there’s no excuse for an internal medicine, primary care doctor, or neurologist not knowing about POTS in this day and age.
The POTS discussion naturally leads to one on…
#4 Small intestinal bowel overgrowth (SIBO) and Gastroparesis
“I believe that leaky gut and POTS are huge drivers of the disability in our patients.” Dr. Kaufman
The circle continues with Dr. Kaufman’s next “big one” SIBO (and acid reflux), as both are caused by autonomic nervous dysfunction which causes reduced gut motility (the ability to move the food along), which results in dysbiosis (unhealthy gut flora) and SIBO. Reduced gut motility allows the “little bugs”, as Dr. Kaufman put it, to swim up from the colon into the small intestine where they don’t belong.
Dr Kaufman laid it out nicely. The bacteria from the colon enter the rich realm of the small intestine where they metabolize the foods producing substances that help break down the gut wall, causing leaky gut. Once that happens, the “you know what hits the fan”. Lipopolysaccharides from gut bacteria enter the blood, triggering an inflammatory response including a leaky blood-brain barrier and probably mast cell activation. (Note that you can have SIBO without having any gut symptoms.)
Plus, as Dr. Ruhoy pointed out, the small intestine is filled with mast cells – and connective tissues line the gut wall. Kaufman said that he believes that leaky gut and POTS are huge drivers of the disability in his patients.
The origin of the SIBO problem – a gut motility problem caused by autonomic nervous system issues – makes treating SIBO a challenge. Getting rid of the bugs, Dr. Kaufman, asserted, is a “piece of cake”. While it can take months to do that, keeping the SIBO from coming back is the real challenge.
Add in the gut-brain and gut-immune interface that’s also present, and you can see how crucial a player the gut can be.
#5 Autoimmunity
Dr. Kaufman believes autoimmunity drives POTS, which probably figures in the dysautonomia, and the systemic inflammation and complaints that patients have that are often so vague, discomfiting, and challenging. For me, it was great to hear someone provide an explanation for the many weird, almost indescribable symptoms that people with these illnesses experience.
Dr. Ruhoy believes that mast cells recruit other immune cells to the fight – causing the immune system to be very “autoreactive” and producing things like Sjogren’s autoantibodies. Its not that everyone with Sjogren’s Syndrome antibodies has Sjogren’s Syndrome, but their presence constitutes “trouble” – and perhaps could eventually turn into Sjogren’s or other autoimmune illnesses.
Kaufman is a big believer in autoantibodies being related to POTS and uses a German laboratory.
#6 Infection
“If I have a patient who is not getting better, I will start over and look for infection again.” Dr. Kaufman
Dr. Kaufman – It’s critically important to look for evidence of infection. They could be as simple as recurrent strep throat or herpes virus, or tick-born infections. Virtually everyone has EBV, HHV-6, HSV-1, and CMV and sometimes they reactivate. The big rabbit hole of rabbit holes – the tick-borne infections – appear to be like the herpesvirus infections in that they can become reactivated as well.
Once you start looking for virus-triggered chronic illnesses, you can find them. They are nothing new. Dr. Ruhoy noted that many post-infectious neurological disorders exist and mentioned acute disseminated encephalomyelitis (ADEM) – an MS-like condition that occurs 1-3 weeks after an infection, and febrile infection-related epilepsy syndrome (FIRES). These conditions are recognized throughout the medical community because the localized, objective damage they produce has been easy to spot. That’s something that ME/CFS and its allied diseases lack at this point.
Diagnosis continues to be a problem. There are antibodies, for instance, for tick-borne infections, but attaining the gold standard for pathogen detection – using PCR and culture – is very difficult. Herpesviruses are in a bit better shape, but relying on the gold standard – using PCR to find the bug – still means that you can miss people with reactivated herpesviruses using these techniques. The vagueness makes it more difficult for physicians.
Still, Dr. Kaufman said, “If I have a patient who is not getting better, I will start over and look for infection again”.
Small Fiber Neuropathy (SFN)
Small fiber neuropathy (SFN) – damage to the small unmyelinated nerve fibers in our skin, eyes, and many other places – can contribute to dysautonomia, but Dr. Ruhoy focused on pain production. The majority of her patients have SFN. (SFN first showed up in our class of diseases in fibromyalgia. It’s FM’s contribution to ME/CFS, POTS, and long COVID).
Unlike the vagueness that using antibody results entails, the diagnosis of SFN is more straightforward: it’s a histologic diagnosis (structural) made under a microscopic. The pain presentation from SFN is different in these diseases than in other disorders. For one, it’s more diffuse in and does not work its way up from the feet. It’s probably linked to autoimmunity and mast cell activation.
We are dozens of episodes behind…
Take the Poll! Tell us how many of the “Septad” your health care provider is assessing…
THE SEPTAD POLL
Results – I don’t know why the results are not showing but here they are so far. Thus far POTS is getting assessed quite a bit while hypermobility, SIBO, and small fiber neuropathy are not getting assessed much. They are below.
| Yes | No | |
| Hypermobility | 95 (27%) | 259 |
| Mast cell activation | 124 (35%) | 230 |
| POTS/Dysautonomia | 215 (61%) | 139 |
| Small intestinal bowel overgrowth | 89 (25%) | 265 |
| Autoimmunity | 149 (42%) | 205 |
| Infection | 157 (44%) | 197 |
| Small fiber neuropathy | 78 (22%) | 276 |
- Next Up – Craniocervical Instability
- Check out the Unraveled podcast here.
Health Rising is not affiliated with or receive any funding from the Unraveled Patreon series.






The cause of ME is a vascular injury to the brain as proven by Dr Hyde at nightingale.ca
As a 17 year victim of ME/CfS, you’re wrong and so is Dr. What’s his name. I was perfectly normal…no CVA occurred, but I suddenly became weak, sick, and basically feeling like crap. I was a paramedic for 25 years, an ER tech, and a flight medic and have an extensive medical education, and working with doctors for 25 years, you learn a few things. Anyway, I was talking with an old ER nurse and was complaining about my symptoms when she said, Dave, you have mononucleosis (EBV). I found that hard to believe but went to my doctor to have a test done. She found it hard to believe as well but ordered the test anyway. Low and behold, I was EBV positive and that was the beginning of the end. As the disease progressed, I can give you a precise road map of the organs that were effected by the symptoms as the infection progressed down my Vegus nerve, starting with pain of my ear that made it excruciating to touch, then nodes in my neck, loss of voice, asthma type symptoms, cardiac arrhythmia, GERD, and continuing with organs downward in succession to my gut and eventually, my legs being in severe pain…every system that is innervated by the Vegus nerve and each branch as it goes to those organs was effected.
A cerebral vascular accident does not act in that way. I would have had to have a specific vessel issue, followed by a different vessel, followed by a different vessel, and so on. There would have to be some form of paralysis of each successive system or organ, one at a time, or possibly hemiparesys which there was not. No neurologist or whatever the name of a blood vessel specialist is could go along with such a theory. Anatomy and physiology facts do not function in such a way. You can tell your doctor it’s a nice try but is absolutely impossible.
Thanks David, for relaying your story! As someone with medical background it would be great to have your story in our Lives Interrupted program. There’s some about health professionals telling their tale 🙂
https://www.healthrising.org/bm-li-view-stories/
David, do y ou have chronic EBV or ME/CFS? My EBV was negative and yet I still had ME/CFS. Both my EBV and CMV viruses are and were OK but I still had ME/CFS.
Mark, ME/CFS is also known to be caused by any severe (or untreated) viral, bacterial, fungal, infection and likely has a genetic component as well. Trying to find a “cause” may be hard to do because everyone is different in what percipitated their ME/CFS. Long Covid is ME/CFS, as is chronic Lyme, etc. Sorry it’s not the news you wanted to hear. 🙁
I have ME/CFS, but it started by EBV reactivation, and continues to reactivate occasionally. I saw Dr. Montoya (who, unfortunately, is no longer in the picture due to some hyped up BS) And he explained that the virus has infected the milenated fibers that surround the nerves causing inflammation and about everything else. That made complete sense since my issues involved the Vegus nerve and eventually all the nerve branches that come off of it.
Now, there is an antiviral that is semi effective against EBV, but the problem is that those nerves are surrounded by the Dura Mater which is one of the menengies that surround the brain, which in effect, makes the nerves an actual part of the brain. Where the problem with that begins is that we have what is called the blood/brain barrier that is a selective, semi permeable membrane that protects the brain from unwanted substances, one of which is an antiviral. You have the infection in the nerves but the antiviral can’t get to them…well, there is one route but it’s apparently unavailable. That’s why the disease is incurable, there is no way that the medication can get to the infection.
Now, I had this brainstorm idea about how to cure us all. I have a friend who is a Neurosurgeon so I called her and asked if there was a way to inject an antiviral into the Circle of Willis which is a structure within the brain. It seemed like a good idea to me, but her comment back was a clear and non-misunderstandable NO, period. Damned Neurosurgeons anyway, what do they know. Point being that I have it, will always have it, until the day comes, and it won’t be long, when I can’t take it anymore and simply turn myself off. Yes, I have a plan and the means to carry it out.
Good luck David – interesting idea! The brain just has to be involved doesn’t it? I predict that either an antiviral will be found that can get into the brain or something else will be found that can impact the brain. It could even be something that impacts the gut – which then turns down the inflammation in the brain. Or something that tightens up the blood-brain barrier – keeping viruses or immune cells or immune factors from getting in there. We need to keep an eye on the brain.
Is it possible that if we already have a compromised blood brain barrier (as some have suggested) then antivirals would be able to get through anyway, while that damage persists?
Possibly so, I would think.
I was just in a Johns Hopkins study that looked at the blood brain barrier post Covid.
Good to hear!
It’s my belief that a suspect pathway is through the sinus. There IS a way for nasty things to circumvent the blood brain barrier.
I think you will like Michael vanElzakker.He has proposed a vagus nerve infection hypothesis (VNIH) for ME/CFS.
https://me-pedia.org/wiki/Michael_VanElzakker
Yes, I’ve been doing some reading/watching about him and his theories follow pretty close in line with what I experienced as my disease progressed down my left Vegus nerve and it’s branches. I would love to talk with him because I have a very unique and in depth story to tell.
David, I would take what Dr Montoya says with a pinch of salt. NO doctor in the whole world knows what ME/CFS is still today. They are all just hypotheses. There is even a hypothesis that ME/CFS symptoms are hypothyroid symptoms since a lot of people with hypothyroidism say they have ME/CFS too. I know people have tried thyroxine to no avail, but it is still a good hypothesis since viruses can wipe out the thyroid.
Well, call me Switzerland, but I think you’re both right 😉 EBV needs some nerve damage to cling on to and make it worse, imho, which can either be caused by mold or a chemical toxin or a blow over the head, or a combo of things.
Mark, try listening to the podcast — they are quite knowledgeable in this area but don’t think of it as monocausal.
Anyone know whether there is a way to get these as a conventional audio podcast?
I hope this is something Cort is working on! Maybe time to join the Substack family? It’s not perfect but it’s good enough audio to let me listen to info I wouldn’t have the ability to read. 🙂
You can get their podcast on Patreon.
Any idea how? I’m logged into Patreon in a web browser and I’m an Unraveled member but I don’t see anything about a conventional audio podcast. There are lots of videos.
I downloaded the Patreon App & watched/listened to it on my phone.
Does the app let you download the content to play off-line? I don’t always have an internet connection and those are the times when I’m most likely to listen to something.
I’ve just turned off my wifi but it was still going to use mobile data, J.
I just pop in my headphones and listen to it on my computer…what’s happening on screen isn’t that interesting.
I understand that that is possible. That’s not what I’m looking for.
So glad to see tick borne infections is mentioned. My hubby’s doctor tested through Armin labs as they have more specific and sensitive testing than our health care system uses for tick borne diseases. So his “ME/CFS” symptoms are being treated by targeting the positive tick infections he has.
when saying ‘treatment’ it would be good to somehow not make it look so definitive in the title–as there is no treatment that fixes cfs/me, and people reading the headline may get the wrong idea, that it is curable by various treatment(s).
I can see how treatment can get jumbled up with recovery but for them I think its mostly about getting better.
to my ears, patient care plan sounds different than treatment plan.
might be disappointment instead of hope on my part
or possibly fear of the word treatment giving some fodder for more gaslighting of patients
I don’t know. I recognize the concern about gaslighting but on the other than many chronic diseases have treatments but are still chronic. A major goal of the podcast is inform doctors that there are treatments that can help.
In a way it’s actually the perfect title as doctors or patients can look at it, say oh! there’s a treatment roadmap – read the blog and realize that the vast majority of doctors are not assessing these factors and the vast majority of patients are not getting treated for them.
Is it any wonder, then, that so few people get better?
Im not a physician, just someone who’s been suffering CFS for over 40 years now. Reading this news, even the title alone, has the smell, so frequent around us patients, of what we call in Spain “tomadura de pelo”.
A “joke” – a “tease” – why would you say something like that?
Here you have a chance to learn about this disease from some of the top experts in the world and you call it a joke! This is really frustrating. What do you want from a blog?
These doctors – and others they interact with – believe that the septad provides them a treatment roadmap – a way to bring all these factors together into one coherent whole. This is what they say about the septad.
Maybe you want the whole package in one blog? As someone who’s had this for 40 years, I think you know how complex these diseases are.
I don’t know why others are being so negative about this. At least some doctors are trying to help us figure out what’s going on! Im blessed to have started going to a primary care doctor who is trying to get to the bottom of all my symptoms, and have Metrodora also helping me.
They both are trying their best to help me especially with the hyper mobility and POTS issues, like the doctor here said, the dysautonomia needs to be handled. But my doctors response to me asking what they can do about my CFS is that it’s such a complex illness there is such little research and knowledge of treatment.
So what these doctors are doing, wanting to help teach doctors about our complex illnesses means a lot to me. It means they care, and they are actually trying to do something about it. It might be small, but who knows who it could help, every little bit of instruction and education about our illnesses is a step forward, so why be negative about it? I understand being guarded, but I think it’s important to not shove things like this away, how else are we supposed to get help?
“I think it’s important to not shove things like this away, how else are we supposed to get help?”
Great question…Where indeed?
This never ends.
Thus far, of the Septad
Joint hypermobility, small intestinal bowel overgrowth and small fiber neuropathy are the least likely to be assessed. On the bright side POTS is being assessed in about 2/3rds of respondents – that’s pretty good!
May I humbly suggest that it be “orthostatic intolerance syndrome” rather than “POTS”?
And also not “POTS/dysautonomia”?
I know Cort knows the differences, but so many people including doctors have the idea now that dysautonomia is synonymous with POTS and that POTS is the only orthostatic syndrome.
There are many people with dysautonomia who do not have POTS and do not even have an orthostatic syndrome.
In support groups, it’s gone from people being told “There’s nothing wrong with you” to “You don’t have POTS therefore nothing is wrong with you”. The other orthostatic syndromes and the whole rest of dysautonomia is getting eclipsed by POTS.
Kudos to the folks getting the word out there on POTS, but we need to also mention OH, OCHOS, SFN, etc. too.
Agreed – just saying POTS is missing a lot – including those people without POTS but who still have reduced blood flows to the brain – which is apparently just about everyone with ME/CFS who do not have POTS.
I can say that, due to my insistence, the education I have given, and finally some trust that my doctor has built up in me, my POTS and Orthostatic intolerance issues are no longer noticeable by taking dextroamphetamine at a dosage that we are still experimenting with, and my pain levels have also dropped without significant increase in BP numbers. I wear a Samsung Galaxy watch 4(I think) Classic that I sort of installed a modified APK in, that allows we to take a quite accurate BP, if I keep it calibrated. That function has only been available in Korea. I watch my pressure, O2 sat, pulse rate, night time sats, snore detection and sleep quality, quite often throughout the day, and night. I even check orthostatic and pulse rates through the three positions which cause orthostatic changes. It has been a very valuable diagnostic tool and provides data that my doc and I can evaluate. Call me crazy but nobody helped me until I started helping myself and its taken a hell of a lot of time and reading to gain some trust from my doc for her to start believing in my way of thinking. I’m lucky in the sense that I have worked in the medical field for 25 years. But I’m not a doctor, nor do I believe that others should take the steps I have taken because I am only using myself as a lab rat and some of the things I have been able to do are dangerous to say the least. But I’ve been able to have tests done that most GPs would not even think of, and use that data to form my own hypothesis, although I am unable to prove any of them except to myself.
From April, but relevant:
https://www.nature.com/articles/s41579-022-00846-2
“Long COVID: major findings, mechanisms and recommendations”
including remarks on ME/CFS, POTS, MCAS.
Nice!
I’ve just ordered this book, ‘Chronic’ by Steven Phillips MD and Dana Parish. It looks really interesting. I saw that David Putrino PhD showed it on his Twitter/X account.
https://stevenphillipsmd.com/the-book/
These doctors are phenomenally expensive. To see them in person is somewhere around a thousand dollars. It seems to add insult to injury that now they want $9/month to listen to their podcast instead of freely disseminating their wisdom and knowledge to both the patient community and interested doctors. I understand there are costs involved in this kind of endeavor, but this is unusually high for a Patreon where the only offering is the podcast. I would hope that they would reconsider this approach and find a way to offer this information as a charitable gift to the community, either through some targeted sponsorship or tax breaks. They should know as well as anyone the burdens on us as patients. Why add another?
They are working within a broken system and are the trying to do their best in spite of these limitations. I am (very fortunately) a new patient of Dr. Kaufman, and my first visit was 1 1/2 hours. He reviewed my medical history and years of labs prior to the appointment, wrote extensive notes, and ordered labs. One appointment took around 3 hours. Our broken system won’t pay for this type of detailed care that patients like us need. It’s a sad state of affairs.
In my opinion, the Patreon podcast is a way to take advantage of their experience and insights and take that information back to your primary care doctor. It’s very detailed and I can’t always follow the depth of information, but it’s for both patients and doctors trying to learn more about things that they weren’t taught in medical school. Before starting with Dr. Kaufman, my PCP was open to suggestions that I made based on my reading. Dr. Kaufman and Ruhoy also have a Listserv that doctors can participate in to learn more, ask questions, and share information. One could always subscribe for a month, listen to the episodes, and then unsubscribe.
I fully realize that it’s awful that comprehensive medical care isn’t available to all. My hope is that doctors like these find treatments that work and that their knowledge filters out to the medical community. I do know that they are trying.
As always, thank you Cort. I’d be lost without your amazing work.
No, I’m sorry but the “doing the best they can in a broken system” excuse is too little too late at this point. The doctors and other medical professionals must lead the charge for change, rather than point the finger at insurance companies and their reimbursement problems and leave the patients who are increasingly broke and sick to add crushing debt to their burdens.
There actually are doctors out there who provide an in depth podcast for free to their subscribers, knowing full well that their care is out of reach for most people. Peter Attia comes to mind…he is out there giving a master class on a wide range of topics every week (and giving is absolutely the operative word in that sentence..there is no charge to listen).
I was not the biggest fan of the late Dr Lerner, for many reasons, but the fact that he took Medicare (no other insurance) was at least a step towards recognizing this problem. There are other doctors out there making it work with multiple consecutive day appointments to satisfy conventional billing requirements while getting the time and information they need to practice the type of medicine we require.
I can afford to see whoever I chose, lest this come off as bitterness. It’s not, it’s frustration that doctors think it’s OK to wash their hands of the sickest and poorest of us and we all excuse the behavior as a natural consequence somehow instead of demanding that our doctors do something other than just treat those of us who can afford to pay and propagate this appalling two tier system.
Hi, is Dr Kaufman receiving new patients? What did you do to become his patient? I’ve been calling and no one is answering the phone 🙁
Hi Andre – he was accepting new patients when I reached out to the Center for Complex Diseases in June. He asked to review my medical history before accepting me as a patient, and required that the first visit be in person at his Seattle office (I believe his partner is in CA). But I think he also works with bed bound patients so I don’t know if he requires that of everyone. I don’t remember them not answering the phone… Hope it works out for you.
Thank you so much 💜 hope you’re recovering!!
Cort….some time back there was an interview…I think by Kaufman and Ruhoy…they interviewed a doctor with a very difficult last name. He discussed his theories and hypotheses on the Vagus nerve being involved with ME/CFS. But search as I may I cannot find it. I’m searching for his name and contact information if it’s public. Do you have any resources to assist me? Please.
Dave
Hi David, hopefully I will come across it as I do blogs on the talks. I will certainly do one on a vagus nerve talk.
One thing I’d like to see much more of is ADHD and Autism (and possibly other types of neurodivergence) being studied as being linked to this septad, as well. I’ve had symptoms of hypermobility/EDS, immune system disregulation/possible Mast cell activation, gut issues, POTS, and chronic EBV (this one being the only one I’ve actually been diagnosed with) almost my whole life and the only thing that actually brought me to realizing that these conditions exist was through my exploration of what it actually means to have ADHD after I was diagnosed at 22. Physical trainers and therapists talking about the link between ADHD and POTS is the only reason I became introduced to all of this information that describes me to a T.