


Creativity and productivity have been the hallmarks of Simmaron’s small research team.
Clinical trials – once a rarity for chronic fatigue syndrome (ME/CFS) – suddenly seem to be popping up all around the place. The Open Medicine Foundation just announced its first two-fer (two drugs tested together) clinical trial, Solve M.E. has funded at least 4 small trials over the past couple of years, and now we have Simmaron’s first clinical trial.
THE GIST
- The Simmaron Research Foundation’s research team of Avik Roy and Gunnar Gottschalk has been making waves with their work on not one but three mouse models for ME/CFS, and their work suggesting that the cellular cleanup process called autophagy has gone awry.
- This time, they and the Simmaron Research Foundation have really outdone themselves, though: they’re about to begin a 100-person trial of Rapamycin (Rapamune) – a possible mitochondrial enhancer.
- The trial’s origin has roots in the research program’s work in mouse and human studies, which found high levels of a compound called ATG 13 which suggested that problems with autophagy existed.
- Problems with autophagy could interfere with many cellular processes, the most significant of which, for our purposes, may be the inhibition of mitochondrial activity and the production of free radicals.
- Studies showing that Rapamycin has been able to extend the lifespan of several organisms have sparked interest in the longevity-enhancing potential of the drug. The drug inhibits the mTORC1 pathway, which in turn inactivates autophagy.
- Last year, Health Rising published a Rapamycin recovery story involving a physician who’d been ill for ten years.
- Simmaron’s non-placebo-controlled pilot trial will include 100 patients under the care of Drs. Kaufman, Chheda, Peterson, and one other doctor to be named soon. The trial, which is expected to last at least 18 months, is designed to provide data needed to get funding for a more rigorous placebo-controlled trial.
Next, they showed, in two papers, that the coronavirus doesn’t actually need to enter the cell to damage it – all it has to do is attach itself to the ACE-2 receptor. That’s a very interesting finding given the apparent ACE-2 dysregulation also found in ME/CFS and POTS which could help explain the reduced blood flows, low blood volume, poor mitochondrial functioning, and others in that disease. They also developed an ACE-2 receptor modulator called the ACIS KEPTIDE and received a patent for it.
They’ve been moving towards fulfilling an immense need in this disease by working on not one or two but three ME/CFS mouse models (for PEM, POTS, and brain fog). They won a Ramsay Award in 2022 and received a rare NIH grant in 2023.
Mouse and Human Studies Lead to Rapamycin Trial
Still, I never anticipated the team would be able to pull off a 100-person clinical trial of one of the most intriguing drugs out there – rapamycin – a possible mitochondrial enhancer.
The rapamycin trial has its roots in Simmaron’s mouse and human studies. Mice were given two compounds, one of which activated the mTORC1 pathway and one that inhibited autophagy – a cellular cleanup process that’s crucial to mitochondrial functioning.
The mice responded by exhibiting high levels of ATG13 – a marker suggesting that problems with autophagy were present – and by looking like they had ME/CFS. Interestingly, the female mice were much more likely to become ill, quickly became fatigued when asked to exercise, and their grip strength declined.
Moving from the mice to humans, the Simmaron team found the same evidence of a breakdown in autophagy (high levels of ATG13) in ME/CFS patients’ serum. When autophagy breaks down, it can impair oxygen consumption and mitochondrial activity, affect immune functioning, turn cells into pro-inflammatory generators, and lead to clumps of proteins that can damage all sorts of cellular processes.
Applying the serum from ME/CFS patients to cultured microglial cells caused the microglial cells to erupt into activity and spew out free radicals and produce iNOS (nitric oxide) – an inflammatory and neurodegenerative form of nitric oxide. Meanwhile, the serum from the healthy controls had no effect on microglial activity.
Next, they used an antibody to neutralize the ATG13 in the serum, and tested it again. When the ATG13-free serum failed to turn on the microglia to the same extent, they concluded that ATG13 was the culprit in the ME/CFS patients’ serum.
That finding set the stage for the trial of an mTORC1 inhibitor called rapamycin in 100 people with ME/CFS. Interestingly, just last year, Health Rising presented the story of a physician who has recovered from ME/CFS using rapamycin (Rapamune).
Rapamycin (Rapamune, Sirolimus)
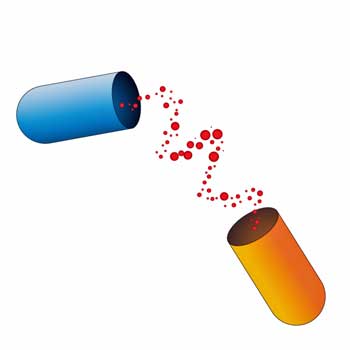
A model of rapamycin latching onto mTORC1 and preventing it from activating.
Touted by some to be a longevity drug, rapamycin (Rapamune) inhibits inflammation by preventing T and B cells from activating.
Like so many other drugs, it has a fascinating backstory. Produced by a bacterium called Streptomyces hygroscopicus, rapamaycin was first isolated back in 1972 from samples gathered on Easter Island of all places. (Its name came from the native name for the island, Rapa Nui, where it was found.) Initially developed as an antifungal agent, researchers soon became more interested in its ability to inactivate the mTORC1 pathway.
The mTORC1 pathway functions as a kind of energy/oxidative stress sensor and is regulated by a number of factors including Rapamycin. The pathway does a number of things, but its main interest for ME/CFS is that it inactivates autophagy – the process through which cells cleanse themselves of old and damaged compounds which would otherwise interfere with mitochondrial production and cellular functioning.
Since declines in autophagy have been associated with aging, Rapamycin’s ability to tamp down the mTORC1 pathway and restore autophagy has made it of much interest to the longevity community.
The mTORC1 complex
Interest in Rapamycin’s longevity properties began in the early 2000s when it was shown to slow aging in worms, yeast, flies, and ultimately mice. Interestingly, Rapamycin appears to both inhibit (reduced TNF/IL-6) and stimulate (increased IL-12 / decreased IL-10) the immune system. The IL-10 inhibition might be helpful in ME/CFS, as a recent study suggested that increased levels of IL-10 may be hampering the acute immune response – allowing bacterial toxins to flourish.
Health Rising’s Rapamycin Recovery Story
Prior to ME/CFS, the doctor’s favorite activity was mountain climbing! Just a year earlier, the 69-year-old had climbed to the top of an 18,000-foot extinct volcano in Chile. He was, as he said, “living life to the fullest.”
An upper respiratory infection, though, knocked him down and seemingly out for good. After working all his life in an intellectually challenging career, he found he could only concentrate for two hours at a time, could not handle household chores and, at times, couldn’t walk a block. His social life was nonexistent. This went on for ten years.
His literature search led him to Rapamycin and he began an N=1 trial. Rapamycin’s inhibition of mTORC1 activity, its potential as a longevity drug, and its potential to reduce lactate production, increase ATP levels, improve cognition, and induce autophagy all recommended the drug.
He’d tried numerous treatments, but upon taking low-dose Rapamycin (6 mg once weekly), he noticed an improvement in three weeks, and by six weeks he was in full remission.
The Rapamycin Trial
Four doctors will assess Rapamycin’s effectiveness in ME/CFS.
A hundred people under the care of David Kaufman MD and Bela Chedda MD at the Center for Complex Diseases, and Daniel Peterson MD at Sierra Internal Medicine (and one more doctor to be named) will be given the drug.
The dosage will be determined by each doctor. Autophagy markers will be taken before the trial, then at the maximum dose, and 30 days at each time point thereafter.
The goal of this non-placebo-controlled pilot trial is to gather enough data to get funding for a larger, more rigorous trial. The trial will assess symptoms and autophagy markers, and probably last from 18 months to 2 years.
Rapamycin has been around a long time and is known to be a safe, affordable drug – meaning should the pilot trial succeed, physicians will likely be willing to give it a try.
- Find out more about Simmaron’s Rapamycin trial here.
Simmaron asks that if you are on Rapamycin and have ME/CFS, or you have been told by your doctor that they plan to start you on Rapamycin, please email them at connect@simmaron.com.
Kudos to the Simmaron Research Foundation for investigating such an intriguing drug!






thanks for the hope Cort!!! fingers crossed!!! any idea how long this trial will take?
6mg/week seems like a far cry from any dosage used for mitochondrial treatment. Googling results were more like 4-8mg/kg everyday. Maybe the trial is hoping for anti-inflammatory/immunosuppressant effect instead?
Actually after learning further I removed the dosage. It seems that the doctors are going to decide the dosage on a patient-patient basis. There is no set dosage for the trial.
100 person study is very large for ME. This is good news and I wish them God speed. I think the results will be positive judging from my own experience. I take metformin, I’m not diabetic, and have seen a 15% improvement. I’m not scientific, but I believe metformin also helps with issue off autophagy.
Roger, what has Metformin helped with? Fatigue?
It has helped me with fatigue and clarity. I still get set back if I overdo it. But if I stay within my energy level then I feel like my baseline is 15% above my pre-metformin. I also have fibromyalgia, so it seems like I’m dealing with that and not ME. For instance, if I have an active day within my energy envelope I feel tired or even very tired, but not fatigued. I get better sleep at night and wake up more refreshed. I have better clarity and less brain fog. When I do get PEM, it’s more like a headache rather than a migraine. Of course if I go beyond my limit I can still crash as this is not a cure only an assist to the body. Again I do not have diabetes, so not sure if it will help if you also have that condition.
Thanks so very much, Roger.
Wondering how much you take? Or how you, or others, mitigate common side effects? I have plenty of other health reasons to take metformin, in addition to longtime ME. But seems I can only tolerate about half the dose Rxd me.
Taking Adderall for severe fatigue, plus too sick/disabled to cook, or fix more substantial food often enough. Unless i eat much more, metformin causes digestive system issues. Including diarrhea and gut pains. But I’ll do about anything to help my intense fatigue. TIA 💖
Hi Cathleen ,
I take 500mg 1x day. Please follow your doctor’s instructions. I also take Acetyl L Carnititine 500 mg once a day. Each person has to find what works best to help them. Good luck and please don’t give up.
thanks!!!
If you’re all looking for autophagy, wouldn’t fasting do that. That’s why the other day I posted on another comment area..
“Ask yourself if your hungry”
If one goes to the flccc website they tell people to intermittent fast.
I am a person that did a 6 day fast and cured my me/cfs only for it to come back again.
I believe it’s why none of us have electricity between our cells, and why many get electrical shocks when touching things.
You should see what happens when I go into a high voltage industrial electrical room.i start loosing my balance very quickly.i think I would die if I stayed in that room.
This reminds me also of when I first began to fall apart way back in ’93….everytime I would enter my home I would break out in a head to toe body rash. I would leave the house and feel my health improve…go back in the house and start feeling my health decline.slept in a tent until it got too cold 🇨🇦eh.Winter came, I lived inside that home and I’ve been STUCK ever since I have uranium, nickel and antimony show up in a urine test I did
A lot of people on 6mg for life extension, the drug has a very long half life
That’s nuts!
I don’t know how anyone could take it daily…
6 mg weekly might already be too high for some.
Same for people who dose high b vitamins. I just don’t get it. It might help some symptoms but it’s got to be screwing something else up, causing other deficiencies etc.
It has never been my experience that high doses of anything don’t cause problems.
I know that is different from medical standards, you really have to question high doses of anything, much less for a prolongued period.
From what I can tell it will be at least 3 months and may go on longer.
thanks!!!
Yes, fasting!
I was 100% bedbound for 12 continuous years unable to even use the toilet or a commode. Around day 40 of a specialized fast, I knew I could sit up in my hospital bed. A few days later I tried standing with a walker as I knew I could do it too. That progressed to taking my first few steps in over a decade. The fast was extremely difficult physically and emotionally and I had to end it on day 70 but I got my walking back a little bit which no diet, supplement, complex treatment or drug had been able to do.
Can you elaborate what type of fasting you did?
I did Masterfast System using Concord grape, binders, herbs, enemas. In USA, it’s similar to Dr Morse’s Grape juice Cleanse.
THat’s not a fast at all.
Many benefit from increasing carbs, specially fruits – you were taking grapes.
If the herbs were eaten feesh, or decoctions – that’s also plenty of clacium and other minerals and vitamins, plus flavones (anti-inflammatory, etc).
You cannot attribute your gains to fasting.
http://www.rapamycin.news has lots of articles about the drug and a discussion forum for people who use it for its anti-aging benefits. It also has a list of verified suppliers who ship to any country without a prescription.
Thank you, Duncan! I’m just about to trial it and wonder if I might be in touch with you for additional info?
” non-placebo-controlled pilot trial”.
Why do not double blinde trial with placebo. I get tired of this kind of studies. The study is two years and the resluts must be replicated in a double blind study after. Then we will be another 2 or 3 years further. Waste of time. If you do science do it good or do it not please!
Why not study 10,000 people like the stroke studies do? Believe me, if the Simmaron Research Foundation had the money to do a placebo-controlled trial; i.e. if they would get the support to do that – they would do it.
I understand your frustration. I would rather have the results yesterday and its crazy how long it takes to do these things but if in two years the trial is successful – and doctors use those results to prescribe rapamycin – and a more comprehensive trial is funded I sincerely doubt that you will consider this a “waste of time”. Would you want it done faster? Of course – but a waste of time – no.
You’re right, wasting time might be putting it a bit too harshly. There is always a shortage of money. If this research shows a positive effect in 2 years’ time, the question is whether additional money will be made available for further research. Studies are often not followed up, especially in ME/CFS. I almost never see a replication or follow-up study. Only psychologists can do that, see CBT/GET -:)
It’s very frustrating. We are getting older and time is ticking. I have lost more than half of my life. And many with me. Or even longer. You too I think. But luckily these doctors are still doing their research and doing their best. I appreciate that.
Thanks, Gijs – It is very frustrating how slowly things go…Very frustrating. And yes ME/CFS has been with me for 2/3rds of my life. I wouldn’t say that I’ve “lost it” but my God how its impacted it.
And yes, the doctors, the people at Simmaron – some of whom have family members who have been severely affected by ME/CFS – they all want it to move more quickly too. They’re out there on the front lines pushing as hard as they can.
yes, I am getting to old on these verry slow studys..My clock is ticking verry loud. and decades of severelly/verry severelly illness has not helped it in any way. And here they will not prescribe it if not large trial double blind placebo controlled study and replicated by many ohers to come to a consensus wich is allmost impossible because of the heterogenity of us. My onlyhope lays still on the decodeME study togetherwith precisionlife for now. fast and precision. And maybe carmen scheibenbogen who is buussy to sort things out why something helps some and othhers not. I hope, to ill, i have forgotten others… If i could buy time, life, it would be better… And where stays nancy klimas never starting trial? a joke!! cynical one…
Konijn, you are an inspiration. Sounds like you have been enduring this illness much longer than I, and in all that time “research science” hasn’t seemed to change its paradigm too much. It is indeed hard to watch them moving so slowly.
I am a layman weighing in here, but I do wonder about ethical issues. In the case of ME/CFS, is there sufficient evidence that a gross amount of negligence has taken place, which has impacted a lot of people? If so, ethically speaking, should the normal procedures of research be amended? (I realize this is also a financial question, which is to say it costs more to change a paradigm or to “move faster.”)
I remember many years ago hearing a NASA person talking about Mars Rovers and how at some point someone came up with a novel question: Instead of being so focused on sending 1 rocket to Mars and taking all the time and spending all the money to make sure 0% goes wrong, why not quickly and for the same money throw together 10 rockets, and let 90% go wrong.
Of course, those were unmanned missions. And, as I said, I am a mere layman.
Why not get a doctor to let you try it? N=1 but who cares? If it proved effective in clinical trials you would have to get some doctor to let you try it anyway. Go for it, I say. I’m going to try this myself.
my gp who comes at my bed would never prescribe it. even not LDN, mestinon, LDA…And as severelly as I am again changing of gp to get also a NO, there am I to ill for. They know where i live nothing about it and it must also be comparable with sleepmeds.
Konijn, you need a new doctor. Ask your gp for a referral to a specialist. You can do this. Don’t hold back, go for it! Make some noise, get on the phone, force the system to change your treatment. Get angry – this kind of thing is not right!
thanks but i lay in my darkened room with my shaakes from pharmacy for food and can only manage 2 hours of help a week and live alone. i do not need a referral, if i could, i could go by myself to specialists (need many, also for other issues) but simply not possible. but thanks for caring!!!
Very interesting. I’m curious if there are other success stories with rapamycin — there must be if they are going to do a trial? I have heard some concerns in the community regarding safety of the drug. Something along the lines of it making the user susceptible to fungal and bacterial infections, etc. The rumor is that Brandon Gilles of X (formerly Twitter) was on rapamycin when he died ….
I imagine that Drs Kaufman, Chheda and Peterson have patients who have tried Rapamycin – they are all up on research – and the fact that they – and one other intriguing doctor who cannot be named yet – are behind this is good news.
hi Cort – I recently came upon Dr Ruhoy and Dr Kaufman’s new Patreon website and found their hour+ discussion on Fatigue profound and their assessment and treatment suggestions hopeful. One thing that disturbs me is that they seem to promote the use of higher dose Oxaloacetate that costs $500 a bottle for 20+day supply. Upon investigating it further it seems that Dr. Kaufman has developed this product himself and seems to be financially conflicted in promoting it. I have found no other trials or producers than theirs. You would think if it had any benefit – others would be all over it and the costs would come down? What do you think? Has anyone tried it?
They really need to be very careful here. There is no published data so far on how ATG-13 levels track longitudinally in individual patients between PEM and non-PEM states. Unless they have a clear understanding of this dynamic their measurements may end up being skewed. Just imagine: if ATG-13 levels indeed fluctuate in individual patients depending on them currently experiencing PEM or not (which I would assume) their measurements would be completely up time of blood draw. A patient may be in reasonably good shape during intitial assessment, then possibly on day 3 of PEM during follow-up – they would then compare apples and oranges.
The problem, unfortunately, is a systematic one: for most “biomarkers” we really have no data how they differ between PEM and non PEM days – one of the reasons we have so many murky results in ME/CFS research.
My suggestion: first do a very thorough assessment of all the “biomarkers” used how they may fluctuate intraindividually between clinical states.
And again because it matters: ME/CFS is a disease with two completely different pathobiological states: PEM and non-PEM. Not taking this into account in research has been one of our greatest obstacles for progress so far.
This is a very good point. Every study should take this into account. PEM could even be on a ‘spectrum’
But it is also problematic because inducing PEM is very invasive for patients (and sometimes even dangerous).
It makes it specially really complicated to research (very) severe patients, although they might be in continuous PEM.
Doctor Peterson is a very experienced doctor in the field of ME/CFS. He has been studying and treating ME/CFS patients for almost his entire life. Since the eighties.
I am very very hesitant to have real hope because we’ve all been screwed before, but it does feel like the tide is finally turning in medicine with all the long covid stuff getting accelerated. I mean, we have multiple real clinical trials going on right now, irregardless of how effective the meds are that gives the disease “realness” in medicine.
Plus the Mayo clinic proceedings… Absolute game changer. Brought it to the ER with me last time I had to go (for a migraine cocktail) and they immediately called in a pharmacist to discuss med sensitivities and gave me a mild sedative (i think some sort of benzo?) to prevent the stress from making everything worse.
Such a completely different story than the time i went to the er with covid and got treated like a silly anxious teenager, it’s so relieving to know i can hand a doctor a couple page summary of CFS and they will realize it’s a legit serious disease. No more panic attacks about not being able to access emergency care!
Previously I had been told “we don’t treat cfs here, go to a different hospital if you have an emergency” by the only available er 🤦 but now they quickly realize there’s info available.
I guess what im saying is maybe it’s gonna be okay. Probably not for a little while but if we even get a bit of progress on the general public opinion problem everything will be approached with empathy and that would be such a big help mental health wise.
Hopefully the sad fact that we’re facing a pandemic of mass disability from covid will turn into the happy fact of cfs getting the notoriety it deserves on the list with other serious diseases like heart disease and cancers (not that I want people to be terrified of cfs but cmon we have worse quality of life than most of the diseases people dread)
What Mayo Clinic proceedings are you referring too ?
https://www.mayoclinicproceedings.org/article/S0025-6196(23)00402-0/fulltext was released recently, it’s *the* definitive basic summary of all things me/cfs
Thank you for bringing this to our attention again!
Thank you !!
What a great result from the Mayo proceedings! Nice 🙂
I just saw a media report that the rates of brain fog and cognitive problems have gone up dramatically over the past couple of years – and they believe its all due to long COVID.
This is fantastic. Not only a promising possibility in itself, but more than that – another treatment trial. More please!
This is from Dave – his comment did not go through yesterday.
“I am wondering if Rapamycin is related to Clarithromycin? I ask because I once took a combo of 3 drugs (for 2 wks) that resolved 100% of my (CFS and Fibro) symptoms (but only until I stopped taking the triple regimen). It consisted of Clarithromycin, Minocycline (or perhaps Tetracycline?), and Bismuth.
This combination had originally been developed to treat H.Pylori (ulcers). I had tested negative for H.Pylori, but took it anyway as a test to eliminate possible bugs causing my symptoms (which had not yet been identified as CFS and Fibro). Intriguing. Notably, these 3 drugs have anti-bacterial, and anti-viral properties (and perhaps anti-fungal too?).
I also noticed that Rapamycin was originally developed as an anti-fungal agent. This also intrigues me, because when I first became clinically ill I was working in a building full of black mold.
Wiki stated that the drug (aka Sirolimus) can also increase insulin resistance and (the risk of?) diabetes (due to its inhibition of TORC2), but that this side effect was prevented in mice by the use of one or two other preventative drugs. If an increased predisposition to diabetes (or other problems) is caused by the drug, I would hope that this is acknowledged and addressed during the process of the trials.
I look forward to the outcome of this trial. I can envision that they may be onto something here.
A profound Thank-You Cort! I don’t know what we’d do without you!
Thanks for this encouragement, Cort, and for all you do to keep us informed! So grateful for you all these years.
Thanks! 🙂
I recall listening to a cbc🇨🇦 radio broadcast about MS.the researchers had a hunch ms was from dead cells not leaving the body
Better keep an eye on your blood sugar and cholesterol while taking this in that manner.
I see that this doctor used 6 mg and that was considered a low dose. I was started at 3 mg, which I thought was the low dose. Though I have very slowly improved weekly up to this week, my 6th week, I have not seen remarkable results. I wonder if taking a little more would help? Anyone out there who has done that? I am thankful that it has helped a little, just still have a long way to go. Thanks.
I top at 3mg weekly. After that, I get a stress response and takes a long time to get out of it.
I also stopped taking it, period. The good effects are sustained.
I started at 1/4 of a tablet and increased dose only after a month of that dose, etc.
That is, a dose that is too big for me will cause the same symptoms I am trying to get rid of.
So perhaps you want to try a lower dose, not higher.
It’s very comforting to know this trial will take place. It may be too late for me in my lifetime, now 75 years of age, but I pray future generations will not have to suffer as I have and still do, for the last 38 years. Good luck and blessings to those on the journey of this trial.
Angela F.
After reading many literature, I believe that the mTOR pathway is abnormally activated in CFS patients, and some studies suggest that the mTOR activity of lymphoblasts can serve as a biomarker of CFS, making this study very valuable.
I was seriously considering trying the rapamycin until I went back and read through all the comments from the blog about Jeremy’s experience. In taking the rapamycin, Robert Lawson indicated that he experienced an HSV2 outbreak, Learner described both EBV and HSV2 outbreaks, and forummember9922 references a research article that states “We determined that treatment of cells with rapamycin, which is an inhibitor of mTORC1 activity, led to a reduction in the ability of [EBV-positive] B cell lines to undergo lytic replication. In contrast, EBV-positive epithelial cell lines underwent higher levels of lytic replication when treated with rapamycin.” Hopefully this new research will take such things into account. My own CFS was clearly due to first an EBV infection, and then later to an even worse CMV infection. The covid mRNA vaccines triggered HSV and shingles episodes, and I am currently dealing with a shingles episode that I believe is part of my long COVID symptoms. Under the circumstances, I’ve decided NOT to try the rapamycin! On another note, it has long been my understanding that women are more prone to CFS (and now long COVID) than men, but it seems that most of the recovery stories I’ve read are from men. Is anyone looking at the question of how and why CFS (et al) differs between the sexes? If there are different mechanisms/characteristics, then it seems quite possible that the treatments/cures will differ also. The research certainly needs to address this.
Hi
Just try at a much lower dose
1/8 or 1/4 of a tablet of 1mg, and then stay at that dose for a while before titrating by the same amount.
People that are reporting side effects ade taking big doses, they just don’t think it is big because medicine trains us to think that grams is big, not mgs. 4 mgs is too much for me.
Hi, if this is probably a medication that will help us to have energy, what is the next step to have this medication?
I’m confused: is the idea that we need to inactivate or tamp down autophagy, or is it that we need to restore autophagy? This article seems to say both things.
Activate autophagy and tamp down the MTORC1 pathway
I am planning to use Rapamycin for at least a month. I will be taking Rapamycin at a dosage of 5mg per week, along with two tablets of Schisandra extract twice a day (BID).
Schisandra extract can inhibit CYP3A4, which can potentially double the bioavailability of Rapamycin, helping me to reduce side effects and lower costs.
I am planning to start this regimen in a few days.
Good luck Andy! Thanks for passing on the Schizandra info – I had no idea. Please let us know how it turns out 🙂
I will report any test results, whether successful or unsuccessful, in the comments section.
I have taken the Schisandra extract tonight and will continue for 3 days, followed by administering the first dose of 5mg Rapamycin.
Thanks! Good luck!
The attempt of using rapamycin can be declared as a failure.
I have taken it for 25 days, but no effect has been observed during the period.
The status is relatively poor during this period. The pain and fatigue are slightly heavier than before, but not obvious. It is unclear whether it is related to this medicine.
There may be no positive effect, and there is no significant side effect.
I haven’t encountered the common adverse reaction of oral ulcer, which is very lucky.
Next, I will try Pyridostigmine (PYD).
Thank you for your attention.
^_^
Sorry to hear that but thanks for letting us know. Mestinon is a good next step! If I remember correctly the OMF is assessing it when used with LDN. 🙂
Andy, I suggest starting at a much lower dose. The more severe your illness, the lower the dose, and work up to a higher dose of a few mgs slowly.
It happens often that someone will say such and such substance wasn’t good for them, caused bad side-effects when it’s the dose that was too high. And what people think is a ‘normal’ dose is already way too high, of most anything.
Experience taught me this.
How do we get in touch with the proper people to be part of the rapamycin trial?
You actually have to be a patient of one of the doctors listed in the trial. Sorry!
Can one become a patient from a distance, and would you be able to give me the phone number or email of any of the doctors?
To my knowledge, these doctors are not accepting new patients and have not for some time now.
Bummer. But thanks for letting me know.
I’m case there’s been a recent change contact info: https://www.centerforcomplexdiseases.com/
I say this in the nicest of ways:
I don’t know who you people are that can take 6 mg of Rapamycin weekly…
I get a stress response at 3 mg, and it takes a long time for things to calm down.
I also had to do so many other things, work on my nutritional and hormonal deficiencies. Rapamycin definitely helped me, I find it hard to understand how people can get just take rapa and not address the other things.
I know people also heal and recover simply addressing nutrition. Amazing.
Not my case at all.
Hi KayT:
Thank you so much for your comments. I really want to try Rapamycin and it makes sense to me to start very low. What is the dose you started at?
I also take Low Dose Naltrexone but very little. Last year I was at 4.5 mg a day and weird things started happening – tendon pain and my hair started following out. I learned on this site that that’s a thing for women and LDN can also lead to muscle wasting. Who knew?
I also take hormone replacement therapy (as I’m 60). That includes estradiol and prometrium.
What nutrition do you do? Auto-immune protocol?
THANK YOU SO MUCH FOR POSTING!
*egads*… Estrogen is a known carcinogen, listed as such by the NIH since 2002. If you are taking it, it would be causing/exacerbating a host of issues, including symptoms of ME/CFS. Ditto for progestins.
I am not familiar with the product Prometrium.
Progesterone should be taken physiologicaly, cycled even if post-menopausal, 2 weeks on/2 off. Is that how you were prescribed to do it?
I started with 1/4 tab of Rapamycin [0.25 mg] and worked my way up 1/4 at a time, staying at the dose for a few weeks before changing it. Until I hit the limit, which is when it would cause a stress response.
I stopped taking it after a while.
I would like to try microdosing an antibiotic from a different group (Rapamycin has a structure that belongs with the macrolides).
Antibiotics were used to treat ‘connective tissue diseases’ by a few doctors some decades ago.
Whenever you try a substance, try a small dose. We think it’s tiny because we are used to seeing 100s of miligrams as normal. So maybe less LDN for you, maybe.
Ray Peat
saved my life
Introducing calcium in my diet had dramatic results, immediately.
[Via milk & dairy, etc]
https://raypeat.com/articles/aging/aging-estrogen-progesterone.shtml
https://raypeat.com/articles/articles/calcium.shtml
Thyroid
Is a hormone
Vitamin D
Is somehwere there too
I thank Cort and friends responsible for the website
For making it possible to receive an email when someone writes months, years later replyong to a comment.
Isn’t that something. Somehow it took us ten years to figure that out (lol)
I am currently trialing Rapamune for ME/CFS. 6mg, once a week for 4 months.
I am 4 weeks in, no changes yet. Will report if I notice any changes.
Sean how are you going ?
Still in the news.
A Compound Discovered on Easter Island Extends Life, Combats Alzheimer’s https://link.theepochtimes.com/mkt_app/health/rapamycin-a-drug-that-may-hold-the-secret-to-life-extension-5623260?utm_source=andshare
Mikhail Blagosklonny on Rapamycin
https://youtu.be/_Abtz2WpKfU?si=0zcvwgVNjgLXsm0Z