Sleep Series

We’re on Pt. 2 of our sleep series
This is the 2nd in a series of (at least) 4 blogs on sleep.
Health Rising’s Sleep Series
- Pt. I – Dr. Bruck Interview – Bronc kicked the series off with an interview of Dr. Bruck – a retired sleep researcher whose son has ME/CFS.
- Pt. II – Ruhoy and Kaufman on Sleep – an overview of a fascinating talk by two long-term ME/CFS/FM and chronic illness experts: Dr. David Kaufman and Dr. Illene Ruhoy on sleep on their Unraveled Patreon podcast.
- Pt. III – A new sleep drug for fibromyalgia? A look at Tomnya – a sleep/pain drug Tonix Pharmaceuticals is submitting for FDA approval.
- Pt. IV – an interview with Dr. Mullington, a long-time sleep researcher and ME/CFS expert who, courtesy of the Open Medicine Foundation, is using cutting-edge technology to further understand sleep in ME/CFS.
The Unraveled Patreon Podcasts

Two experts on ME/CFS and other complex chronic diseases share their insights
This is our 4th in a series of blogs on Dr. Ruhoy’s and Dr. Kaufman’s ongoing series of podcasts on understanding and treating ME/CFS/FM/long COVID and allied disorders.
Ruhoy and Kaufman are on podcast number 56 (!) and Health Rising will only be able to cover a fraction of them. Their Patreon podcasts offer a unique opportunity to watch two ME/CFS/FM experts dig into how they understand and treat these diseases. Questions are allowed – and responded to – and they frequently have live Q&A sessions. At $9 a month Unraveled is the best deal in town.
Please note that all podcasts come with the standard disclaimer – the podcasts are informational purposes only, do not indicate that a doctor-patient relationship has been established, everyone should check with their doctor first before following any recommendations, etc.
(I added the paragraphs that are in parentheses- they were not covered in the talk.)
The Gist
- This is the second in a series of blogs on sleep and the 4th in a series of blogs on Dr. Ruhoy’s and Kaufman’s ongoing series of Patreon podcasts called “Unravelled” on understanding and treating ME/CFS/FM/long COVID and allied disorders. At about $9 a month and with over 50 podcasts under their belts this is the best deal in town. (Please note that the text enclosed in () was added by me and was not part of the podcast).
- Their 18th podcast from back in May of last year dealt on sleep – a crucial but complex topic in ME/CFS. Dr. Kaufman started it off by saying that “sleep is a complaint of every single patient” of his but that when his patients tell him about their sleep problems he said “he takes a deep breath (!) because sleep disorder is really challenging“.
- Dr. Ruhoy noted that poor sleep can keep the brain from detoxifying properly, inhibit learning, and affect the stress response and immune system. She also suggested the chronic activation of the motor cortex that we’ve seen crop up in ME/CFS, FM, and long COVID, might leave the muscles in an energy-draining state of chronic activation making it difficult for the body to settle down and get good sleep.
- (Some studies suggest that people with ME/CFS may have a hyperarousal sleep disorder caused by activation of the fight/flight response during sleep.)
- Dr. Ruhoy focuses more on sleep hygiene believing that long term that’s where the money is concerning sleep. (Sleep hygiene includes things like how to get ready for sleep, having a good sleep environment (cool, dark), having a good sleep schedule, avoiding screens like phones, and TV, at night, not eating at night, using your bed only for sleep if possible; taking a warm bath at night (cools the body down), meditating before bedtime, etc.)
- The circadian or 24-hour rhythms that our brain, in particular, runs on. matter. While it’s not often easy to attain, having a consistent bed and wake time that accords with our natural circadian rhythms (going to bed at a decent time at night and waking with the sun) is important. Early morning sunlight – often just 10 or 15 minutes of exposure – early in the morning wakes the brain up.
- (Dr. Ruhoy said that our bodies thrive on routine and rhythm and recent studies suggest that “sleep regularity” – having a consistent bed and wake time – plays a more important role in our health than how long we sleep. (!)
- If you experience lethargy, difficulty with concentration, and exertion early in the morning low cortisol levels – common in ME/CFS – are probably the reason. Dr. Kaufman suggested that low-dose hydrocortisone early in the morning could help.
- Citing trazodone as their go-to drug for sleep, Ruhoy and Kaufman fell in line with some other ME/CFS expert’s experiences. Kaufman finds that Lunesta can be very helpful and Dr. Ruhoy is a big melatonin fan, uses something called deep-sleep-inducing peptide (DSIP), and has found that minocycline – which affects neuroinflammation – can be helpful.
- Dr. Kaufman also finds an antihistamine called hydroxyzine helpful in some patients. Hydroxyzine has sedating properties and Kaufman recommends very tiny doses; i.e. take 1/4 of the lowest dose (25 mg.) Neither are experienced in or prescribe cannabis products but Dr. Kaufman said that of his patients who try it, about 50% find it brings good benefits.
- Dr. Kaufman finds that low doses of a muscle relaxant, cyclobenzaprine (Flexeril) (2.5 – 5mg) can be helpful. (That brings up Tonix’s fascinating new drug that will soon go to the FDA for approval in fibromyalgia. The drug called Tomnya, is a Flexeril derivative may help with both sleep and pain. An interview with Tonix’s president is coming up.)
- We also compared and contrasted other doctors’ recommendations on sleep found on Health Rising. (See blogs listed at the bottom of the page for more on that). Comparing and contrasting 4 doctors (Murphree/Teitelbaum/Attia/Huberman) with those above revealed some heterogeneity. Several sleep aids, magnesium, L-theanine, 5-HTP, GABA supplements, and blue-light blocking glasses commonly suggested were not mentioned in the podcast. Attia was really big on comfortable mattresses – which scored pretty high in Health Rising’s sleep survey.
- Dr. Teitelbaum is unusual in his approach of using low doses of up to 4 sleep aids to achieve better sleep. Teitelbaum’s first choice is Ambien followed by Trazodone, Neurontin and Flexeril. If that doesn’t work he goes to Klonopin, amitriptyline, doxepin, and others. He reports that antihistamines work well.
- Focusing on the hyperarousal/central sensitization found in these diseases Dr. Bateman suggested using nervous system calming agents before sleep (Neurontin, Lyrica, low dose naltrexone, Klonopin, low dose amitriptyline, doxepin elixir, and cyclobenzaprine) as well as deep breathing or relaxation exercises and/or yoga. She noted that long deep breaths with longer delayed exhalations release chemicals from the parasympathetic nervous system that turn down the SNS.
- Check out what Health Rising found in its mammoth sleep survey as well (See bottom of page).
- Coming up next – an interview with the head of the developer of Tomnya – a sleep and pain drug coming up for FDA approval soon.
Unraveled Session #18 May 16th, 2023 – Sleep
“I can’t imagine recovery without getting good sleep” Dr. Ruhoy
Dr. Kaufman started it off by saying that “sleep is a complaint of every single patient” of his and noted that unrefreshing sleep is one of the core criteria for ME/CFS. When his patients tell him about their sleep problems, though, he said “he takes a deep breath (!) because sleep disorder is really challenging”.
Effects of Poor Sleep
Dr. Ruhoy noted that poor sleep messes up the HPA axis (and morning cortisol – usually low in ME/CFS) (which sounds like it could produce something of a vicious circle) leading to increased sympathetic nervous system activity (fight/flight) in the brain during sleep – leading to poorer sleep – worse HPA activity, etc.)
(The sympathetic nervous system mention was interesting as the only ME/CFS studies that I’m aware of that have started to get something of a handle on the sleep issue in ME/CFS found that increased sympathetic nervous system activity (fight/flight) was the only factor they could associate with poor sleep. They proposed that decreased parasympathetic nervous system activity during sleep was preventing people with ME/CFS from benefitting fully from deep sleep.
(Some evidence suggests that people with ME/CFS/FM may have a “hyperarousal sleep disorder” and the authors of a recent FM/autonomic nervous system study went so far as to suggest that going to sleep with FM was equivalent to undergoing a stress test (!). Increased heart rates muscle sympathetic nervous activation, and other evidence of an activated sympathetic nervous system response made sleep anything but restful for FM patients. )
(Trazodone – the go-to sleep drug for these and other ME/CFS/FM experts (and for those with a hyperarousal sleep disorder) – can tamp down SNS activity (see below) and is a drug of choice for many ME/CFS experts.)
- Dig Deeper: Are ME/CFS and FM Hyperarousal Sleep Disorders?
Dr. Ruhoy noted how important it is to have 4 or 5 good sleep stages or sleep periods during the night. Its during sleep that the glymphatic system cleans our brains of toxins like metabolic waste productions, misfolded proteins, etc. – all of which can contribute to neurodegeneration- and, of course, produce brain fog.
Not only do we solidify memory during sleep but by doing so we clear the way for new learning to take place. Whatever was learned during the day doesn’t get consolidated – truly learned – until we sleep. During the consolidation process data is moved from the hippocampus to other parts of the brain – clearing the hippocampus – and leaving it ready to receive new data. Poor sleep, then, produces a double whammy cognitively- we have more trouble consolidating what we learned and are not as ready to learn the next day.
(Sleep also has a vast impact on our immune functioning. Sleep-deprived people, for instance, appear to produce much higher levels of damaging pro-inflammatory cytokines when confronted with a pathogen. Poor sleep also interferes with building the metabolic reserves and producing the cytokines our immune cells need to fight off pathogens.
- Check out “Is Poor Sleep Pummeling the Immune System in ME/CFS and Fibromyalgia? A Vicious Circle Examined” on the Simmaron Research Foundation
Ruhoy regularly orders sleep studies – which can show sleep apnea which causes a hypoxic (low oxygen) state during sleep, producing inflammation, more abnormally folded proteins, etc. At-home sleep studies are more common now but don’t have all the bells and whistles that lab-based sleep studies do.
Dr. Ruhoy then added a really interesting possibility given what we’ve seen recently in ME/CFS, FM, and long COVID studies – that chronic activation of the motor cortex can leave the muscles in an energy-draining state of chronic activation and which makes it difficult for the body to settle down and get good sleep.
Sleep is such a complex subject that it seemed almost inevitable that at some point these two ME/CFS experts would talk about how much they don’t know. Dr. Ruhoy – who clearly loves the hunt and whose mind always seems to be coming up with new possible links and answers- said “the why plagues me – I lose sleep over the why”.
Treatment
Sleep Hygiene
The initial goal is to avoid drugs so Kaufman will go over what appeared to be basic factors regarding sleep hygiene. He said that he often didn’t learn too much from that. Dr. Ruhoy, on the other hand, seemed to place more emphasis on sleep hygiene – at one point stating that in the long term, her money is on sleep hygiene.
Concerning eating late at night, Dr. Ruhoy pointed out that a lot of food sitting in your stomach takes away energy from the restorative activities that occur during sleep. She said she sleeps so much better when she stops eating after five.)
(Dr. Kaufman is clearly not the best role model (lol). He stated that he tends to eat late, and reads books on his IPAD before going to sleep – and admitted to getting poor sleep :). Ruhoy, on the other hand, doesn’t eat past 5 pm – and said she sleeps much better because of it – and also only reads printed books. She appears to sleep well).
(Good sleep hygiene includes things like how to get ready for sleep, having a good sleep environment (cool, dark), having a good sleep schedule, avoiding screens like phones, TV, at night, not eating at night, using your bed only for sleep if possible; taking warm bath at night (cools body down), meditating before bedtime, etc.)
The author of a review paper on the effects poor sleep has on the immune system reported that practices like cognitive behavioral therapy for insomnia, Tai Chi, and yoga which tamp down sympathetic nervous system hyper-arousal and improve immune functioning can help improve sleep.)
One thing that’s really helpful for sleep is the one thing that most people with ME/CFS cannot do – exercise. Dr. Kaufman noted that if he doesn’t get a workout in he often has poor sleep. I have found that short-term anaerobic exercise can be helpful and I wonder if short anaerobic, strength-enhancing exercise sessions can help.
Circadian Rhythms
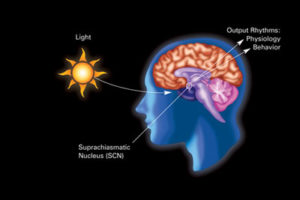
The brain is exhibit #1` of an organ driven by circadian rhythm – the 24-hour cycle of the day.
Dr. Ruhoy put a big emphasis on circadian rhythms – the 24-hour cycle that governs many of our body processes. She noted that we are circadian beings and in no part of our body is that more true than the brain. Dr. Kaufman said patient after patient will say I don’t go to sleep until early in the morning and then wake up during the afternoon – which he said: “feeds their illness”.
Dr. Ruhoy tries to correct the circadian rhythm issue with sleep hygiene which includes going to bed and waking up at the same time whether you want to or not. Getting sunlight early in the day and later in the day can help.
(Interestingly the light rays from the early sun and the late sun – tell the brain to wake the body up by increasing cortisol levels and to calm down. Dr. Huberman reported that on a clear day, only about 5 minutes of sun exposure in the early morning is needed. On cloudy days, ten minutes is usually enough, and on really overcast days, it may take 20-30 minutes. Even on cloudy days, the light intensity outside is much higher than anything you can produce at home. Because windows block some of these wavelengths it’s best not to look through one.)
(Huberman also reports that if you take caffeine in the morning you should wait 90 minutes to do so as caffeine can stop adenosine – a critical sleep factor – from washing properly out of your body.)
Dr. Ruhoy acknowledged that it’s not easy to change your sleep cycle but if it’s off getting it back on track can be very important. Physiologically, we thrive on routine and rhythm – and not just during sleep times but also during the day. Having a good routine helps.
(Sleep Regularity Takes Center Stage)
“In summary, our findings challenge the long-standing assumption that sleep duration is the most important index of sleep for human health”. The authors.
Using a measure of circadian disruption to assess sleep regularity, a recent study “Sleep regularity is a stronger predictor of mortality risk than sleep duration: A prospective cohort study” found that sleep regularity – that is going to sleep and waking up at roughly the same time – was more important for our long term health than how much we sleep (!). With that, we got an important new factor to add to our sleep hygiene practices.

Early morning light exposure tells the brain to wake the body up and can help reset the circadian rhythm.
The 8-year, 1859-person study relied on only one week of sleep data – and then followed the participants for years. Given that it was remarkable how robust its findings were. It found that higher degrees of sleep regularity were associated with a 20%–48% lower risk of death, a 16%–39% lower risk of death from cancer, and a 22%–57% lower risk of death from cardiovascular diseases.
How regular is regular? The people with the highest scores regularly went to sleep and awoke within approximately 1-hour windows. People with the lowest scores went to sleep and awoke within approximately 3-hour windows.
The noted that other studies have found that irregular sleep patterns have been associated with higher mortality risk, metabolic abnormalities, and cardiometabolic risk factors. Interestingly while light exposure at night has been associated with an increased risk of a variety of cancers (breast, thyroid, pancreatic cancer), short sleep has not been associated with cancer mortality. Sleep regularity; i.e. creating a regular sleep routine, then, appears to be a very good thing to strive for.)
Fighting the Early Morning Blues
During the latest Patreon open discussion session I asked about the trouble I concentrating, engaging in physical activity, and the unsettled feelings I experience early in the day. Dr. Kaufman said he could think of maybe 1 or 2 patients who didn’t have low morning saliva cortisol levels and that low dose hydrocortisone in the AM can make a big difference for some.
Treatments
(See earlier section for sleep hygiene)
Trazodone
Both Dr. Kaufman and Dr. Ruhoy said that trazodone was their go-to sleep med.
(They are not alone. Both Dr. Lapp and Dr. Bell also tagged trazodone as their favorite sleep drug. Trazodone is an interesting drug. By inhibiting the reuptake of serotonin and blocking the histamine and alpha-1-adrenergic receptors, trazodone reduces levels of neurotransmitters (serotonin, noradrenaline, dopamine, acetylcholine, and histamine) that are associated with arousal. Some evidence suggests that trazodone may also have neuroprotective properties and help with neuroinflammation.
A 2021 review reported that trazodone is less effective than hypnotics in treating sleep-onset insomnia (i.e., the inability to fall asleep) is “very effective” in treating “sleep-maintenance” insomnia; i.e. insomnia that occurs later in the night or morning. Trazodone may also increase the amount of time spent in deep sleep.
A small but interesting 2008 study found that while cognitive behavioral therapy improved sleep time and latency (the ability to fall asleep quickly) CBT plus trazodone resulted in a further increase in the restorative period of deep, slow-wave sleep in people with depression. A small 2020 study reported that trazodone was more effective than CBT-I in people who exhibit “physiological hyperarousal (ie, activation of the stress system)” during sleep. Trazodone appears to be achieving this by reducing night-time cortisol levels.
A couple of open-label fibromyalgia studies also found trazodone was helpful with sleep and a really interesting placebo-controlled 2018 study found that in Vit. D-deficient fibromyalgia patients’ trazodone (25 mg) given at bedtime + vitamin D 50 000 IU weekly significantly improved pain and sleep scores. Some doctors think we should all be supplementing Vit D.
My brother’s doctor has found that taking trazodone with melatonin helps.
Low Dose Naltrexone (and Trazodone?)
Citing the inflammatory situation in ME/CFS and the effect inflammation may be having on sleep, Dr. Kaufman noted that low-dose naltrexone – which ironically can interfere with sleep in the beginning – often allows people to sleep better. Taking it in the morning can help with the sleep problem but Kaufman noted that it probably works better when taken later in the day. Both agreed it can be helpful with sleep.
(That and the trazodone recommendation were interesting given Biovista’s finding. A drug repurposing company hired by the Solve ME/CFS Initiative to find drugs that might help, Biovista proposed that an LDN + trazodone combination should be tested in ME/CFS.
Delta sleep-inducing peptide (DSIP)
Dr. Ruhoy finds that delta sleep-inducing peptide (DSIP) – a peptide with an interesting history – can help. DSIP got a lot of research in the 80’s and 90’s and then kind of dropped off the map. A 2006 review “Delta sleep-inducing peptide (DSIP): a still unresolved riddle” demonstrated how conflicted the research community was with it. The inability to identify the gene that produces it or the receptor it binds to has apparently hampered research.
Animal studies suggest, though, that DSIP might help with pain, stress management, and other issues. Human studies – the ones that I saw were quite old and small – have had mixed results: some show it to be helpful while others do not. It seems quite likely that DSIP has never been effectively tested in a large, placebo-controlled trial.
On his “Get Fully Optimized” site Jay Campbell cites numerous anecdotal reports suggesting that DSIP was helpful, not in helping people get to sleep, but in getting deeper sleep. DSIP can be found in supplement form. Campbell recommended (that healthy people) start at 50 mcg with a 1x/week frequency and then gradually increase the dosage/frequency over time.
Others
Dr. Kaufman said that plain old Lunesta (zopiclone) helps a lot of people.( It was the most commonly mentioned drug in the comment section of Health Rising’s sleep survey – see below). Dr. Ruhoy is a big fan of melatonin. Dr. Kaufman said he’d never tried doxycycline/minocycline – but that they do similar things as LDN; i.e. they are potential neuroinflammation busters. Dr. Ruhoy reported that some of her patients on minocycline have reported improved sleep.
Cannabis and CBD – Neither Ruhoy nor Kaufman know a lot about cannabis and are hesitant to prescribe it. Dr. Kaufman said that about 50% of his patients who try it report it works great, though – and said they may call in someone who knows more about it to talk about it on the podcast. I hope they do. Cannabis products (both non-THC and including THC) have easily been the most effective sleep aid that I’ve tried.
Hydroxyzine – Dr. Kaufman also finds an antihistamine called hydroxyzine helpful in some patients. Hydroxyzine has sedating properties and Kaufman recommends very tiny doses; i.e. take 1/4 of the lowest dose (25 mg.)
No Doxepin – Interestingly, neither mentioned doxepin – a favorite of Dr. Cheney’s – which he felt was an important histamine blocker. (Cheney was way, way ahead of the curve on histamine…)
Cyclobenzaprine (Flexeril) and A New Sleep Drug for Fibromyalgia
Dr. Kaufman finds that low doses of a muscle relaxant, cyclobenzaprine (Flexeril) (2.5 – 5mg) can be helpful.
(That brings up Tonix’s fascinating new drug that will soon go to the FDA for approval in fibromyalgia. The drug, formerly called TNX-102 and now called Tomnya, is a Flexeril derivative that strips out a part of the drug that can produce toxicity. Tonix’s results suggest that Tomnya may help with both sleep and pain. An interview with Tonix’s president is coming up.)
More on Sleep
Four Doctors on Sleep
Comparing and contrasting 4 doctors (Murphree/Teitelbaum/Attia/Huberman) with those above revealed some heterogeneity. Several sleep aids, magnesium, L-theanine, 5-HTP, GABA supplements, and blue-light blocking glasses commonly suggested were not mentioned in the podcast. Attia was really big on comfortable mattresses – which scored pretty high in Health Rising’s sleep survey.
Dr. Teitelbaum is unusual in his approach of using low doses of up to 4 sleep aids to achieve better sleep. Teitelbaum’s first choice is Ambien followed by Trazodone, Neurontin and Flexeril. If that doesn’t work he goes to Klonopin, amitriptyline, doxepin, and others. He reports that antihistamines work well.
Dr. Bateman’s 2014 talk on Sleep
Bateman agreed that the best way to help with sleep in ME/CFS is to attack the core issues in it. Focusing on the hyperarousal/central sensitization found in these diseases she suggested using nervous system calming agents before sleep (Neurontin, Lyrica, low dose naltrexone, Klonopin, low dose amitriptyline, doxepin elixir, and cyclobenzaprine) as well as deep breathing or relaxation exercises and/or yoga . She noted that long deep breaths with longer delayed exhalations release chemicals from the parasympathetic nervous system that turn down the SNS.
If when you lie down you feel your heart pounding in your chest — beating hard, not necessarily fast – Dr. Bateman suggests you’re probably in the sympathetic nervous system overdrive category and might want to try the Klonopin before you go to sleep.
-
-
- If you can’t get to sleep – use low dose short-acting sleep drugs.
- If you have frequent awakenings – use longer-acting drugs in low doses.
- If you have early awakening – the meds you’re taking to help you sleep may be losing their effectiveness from overuse.
-
Check out Health Rising’s 2014 Sleep Survey Results
Klonopin and Ambien (53%) were top drugs in the effectiveness category with antihistamines (48%) and Flexeril, a muscle relaxant, coming in close behind (47%). (I forgot to include zopiclone (Lunesta) in the survey, however.) Check out all the interesting sleep drug and supplement combinations that have helped ME/CFS/FM patients below.
- Rising’s Mammoth ME/CFS and FM Sleep Survey
- Drugs that Helped with Sleep – Find out what patients said about drug combinations that helped them sleep.
- Drug/Supplement combinations ME/CFS and FM patients said improved their sleep-Find out what patients said about drug combinations that helped them sleep.
Health Rising’s Unraveled Podcast Series
- Unraveled #1: The “Septad” – a Treatment Roadmap for ME/CFS, POTS, Long COVID: From “Unraveled” a Patreon Broadcast from Dr. Kaufman and Ruhoy
- Unraveled #2: Idiopathic Intracranial Hypertension in ME/CFS and Complex Diseases
- Unraveled #3: Ruhoy and Kaufman on Idiopathic Intracranial Hypertension in ME/CFS and Complex Diseases
- Unraveled #4: Drs. Ruhoy and Kaufman on Sleep in ME/CFS, FM, long COVID and Allied Diseases






Thank you for another excellent article, Cort! I find it surprising that they didn’t discuss Xyrem/sodium Oxybate (generic). Dr. Lapp prescribed it for me when my sleep study showed no deep sleep and over 40 non-apnea arousals per hour. It is the only known medication that helps with deep sleep. We fight constantly with the insurance company because it is usually prescribed for Narcolepsy, but it is truly the only medication that has helped me. I only get 2-3 hours with a combination of ambien and klonopin, melatonin, CBD oil, magnesium. I regularly get 7 hours of sleep with Sodium Oxybate. It’s a shame that even the generic is still really expensive though.
I went back over my notes for Teitelbaum – he, too, said Xyrem was easily the best sleep drug for ME/CFS – but it was hard to get and too expensive for most. I didn’t know there was a generic out, though. I hope that has helped with price.
Wow – no deep sleep and lots of arousal….and then from 2-3 hours sleep to 7 hours – wow!
Thank you, this is sooo helpful. As a long-time patient of Stanford’s Chronic Fatigue Clinic, it’s always been a mystery to me why they don’t address sleep health! It seems like a no-brainer, as non-refreshing sleep is one of the core symptoms of ME/CFS.
So a few years ago I started getting serious about cleaning up my sleep hygiene on my own. I have ticked most of the recommended things off my list, and I track my stats using smart watches and sleep apps. It has helped quite a bit just to be focusing on it and noticing trends (like more disruptions for weeks after the time changes, grrr).
But one of the things I continue to struggle with is consistent bedtime and wake up time. I appreciate the reminders in this article, and I’m going to finally try to tackle that. This is especially challenging when you are severe/homebound and time is…well…different (as many people discovered during the pandemic).
One sleep aid I have found that has been remarkable not only for me but for several non-sick friends and family members I have given samples to: FABCBD PM gummies. They contain not
only CBD but L-theanine, 5-HTP, melatonin, Ashwaganda, and GABA. They help my sleep and I also wake up with less pain.
The Wyld indica gummies and a non THC CBD/CBN tincture really helps me. It’s not full proof but they are far more effective than doxepin, which I am also taking. I like all those additions in those gummies. There’s something to these endocannabinoid pathways – and I hope they get someone who knows on Patreon to speak to that.
I had a great example of sleep irregularity last nite. I usually go to sleep between 10 and 11 and was up until about 1 am. I took two big bites of the gummies and got to sleep. My sleep score on the Oura ring wasn’t bad but that late sleep time clearly really got to me.
I liked Huberman’s admonition to not take caffeine for 90 minutes after awakening to enable the adenosine to wash out and I’m trying to do earlier supper times. I also wonder about DSIP and hydrocortisone in the AM.
I got long COVID and now I have to use Chinese skullcap to get deep sleep and REM in the normal range on Fitbit. If I don’t use it I can still sleep but the deep sleep and REM are very low and I wake up in refreshed. Melatonin can help me sleep but did not help me get deep or REM sleep, so there must be something about Chinese skullcap that affects deep sleep. Unfortunately when I stop using it I go back to not getting deep sleep again.
I’ve been gradually working on the Stasis breathing program mentioned on this blog and it’s been dramatically helpful. It cut down the time it takes me to fall asleep from over 1 1/2 hours to about 20 minutes.
Thanks for mentioning that. I’m about to go on that program…It makes sense – proper breathing should reduce the arousal/fight or flight that can keep us from entering sleep and staying asleep.
Yes, and remember Wim Hof Method and his breath-holding for 10 seconds to increase the osmosis oxygen in amd carbon dioxide out.
You take in a breath, absorb the oxygen for 10, let it out and hold your no-breath for 10 to allow the Co2 out.
Hof credits this plus intentional cold exposure with eliminating his pain, anxiety.
One night I had a high-anger reaction to very unfair treatment and was awake 7 hours straight… UNTIL– I did the Wim Hof breath holding for 20 minutes. Nothing else could calm me enough to fall asleep
I had good sleep hygiene all my life before I got CFIDS/ME at age 40. Tried all the non-medicine suggestions first. Not helpful. Finally, a doctor prescribed Ambien, which has had few side effects except for one episode of sleepwalking in my room (partner told me). Would you believe I have been on it for over 20 years now! I always tell whatever doctors, and they are disbelieving, but each has said it’s more important with CFIDS/ME that I sleep. I have friends abroad who were refused any prescriptions for sleep and they have developed severe health issues on top of their CFIDS/ME. So maybe whatever helps you sleep is the best thing for you.
You mentioned that LDN works better if taken later in the day. Why is this?
I don’t know. That’s what Dr. Kaufman I believe said.
Thanks as always for the great info! Some personal notes.
1. If your getting-to-sleep time is late, or gets later and later (phase shift delay), or you have insomnia (trouble falling asleep), be careful about trying to adjust it with morning and afternoon light. For a person with insomnia or phase shift delay, this light adjusting (chronotherapy) can kick you into non-24 disorder, or worse. Non-24 is where the sleep cycle (wake + sleep) is consistently long or short, usually 22-26 hours. For people with non-24, a typical pattern might be, getting to sleep up to 2 hours later each night, and waking up to 2 hours later each day. The times get later and later until it’s worked completely around the day. It’s very disorienting, and impossible to keep normal work hours.
So if you have insomnia or phase shift delay, be careful about chronotherapy.
2. I have severe sleep swings (instead of around 24 hours, my wake-sleep cycle is anywhere 15-40 hours). Two different sleep neurologists have attributed this extreme sleep dysfunction to damage to the sleep center in my brain (the suprachiasmic nucleus, in the hypothalamus). I have extensive white-matter loss and atrophy, so this explanation is reasonable.
I’m offering these notes in hope that if anyone else has these unusual situations, the information might help.
I believe the lowest available size of hydroxyzine is 10mg, not 25mg.
Superb effort, Cort, on a crucial subject! Thank you!!
(If any readers can afford a donation like I just did, I would encourage it.
I wish I could afford more, I’m living off very minimum Social Security.)
Among other meds mentioned, a low dose Flexoril seemed like it might be worth a try. I’ve had severe PTSD and chronic muscle tension as a result of brutal child abuse and am imagining a muscle relaxant might help my sleep. Anyone with body tension find that it helped them? Also, I’ve never tried CBD, Cort you’ve had a nice effect on your sleep with CBD?
Agreed about the service Cort provides, Thomas. Thanks for doing some fundraising solicitation on his behalf. I like it better when the site visitors do this instead of Cort himself.
Thanks Thomas, yes CBD has helped with sleep and keep an eye out for Tomnya – I have high hopes for it! 🙂
Hello Thomas,
I have personally taken cyclobenzaprine (Flexeril) with great muscle results, albeit not for either CFS or FM.
I had debilitatiing anxiety since I have GAD and had not yet tried medication. The combination of a seated physically repetetive job and the fact that it would end in 2 months resulted in sharp pain on one side where the back of the neck meets the shoulder muscles. I had a chiropractor and a lifelong stretching/self-massage regimen, but NOTHING would alleviate this knot of pain.
Cyclobenzaprine did however!
I didn’t feel wobbly or anything, so I guess it was low-dose, and it didnt space out my mind or anything either.
In today’s blog the doctors recommend it for the Fibro patient whose muscle spasms, most likely, keep their brainstem alert, discouraging deep sleep.
I just want to be for you at this moment a first-hand witness that this relaxant was helpful and I would not say it was harmful.
What it did was take what we could call a “stored” stress and release it. After that it did not return. I think this may resonate a bit with the body memories concept found, for one, in ptsd.
I hope this is helpful
Thanks so much, Chris, for sharing your thoughts and experience with me. I’m very sorry you’ve had GAD and wish you all the best with that. I’m glad flexeril had helped you.I will consider giving that or another muscle relaxer a try hoping it may help the PTSD and body trauma memories.
“Antidepressants Could Trigger Some Cases of Chronic Fatigue Syndrome”
https://www.sciencealert.com/antidepressants-could-trigger-some-cases-of-chronic-fatigue-syndrome
Dear Folks,
I have a research-based insight to lack of restorative sleep in CFS, partly based on the above blog and partly on additional reading that I did based on it.
While melatonin triggers sleep, people find that typical supplementing does not *sustain sleep. I learned that what ” ” causes sleepiness or sleep need is build up of adenosine in the brain.
To put the conclusion first: if a CFS patient CAN NOT exert, physically, cognitively, nor emotionally (see SEID) then why? Because there is not sustained adequate ATP production by mitochondria.
Adenosine TriPhoshate.
Why would that matter? Because equally in the brain as in the body, if ATP is not put to work (sufficiently) then not enough adenosine will accumulate and need to be cleared during the inactivity of sleep.
To paraphrase sleepfoundation.org, ‘the longer we remain awake, which would normally include exertions, the more we will become sleepy. Adenosine build-up in the brain creates DEMAND for sleep.’
They also said that excessive napping, or the poor sleep hygiene of staying up late and not getting up on time will offput the normal melatonin release to send you to bed. If you rest extra long in bed the morning then both factors will prevent the punctual release of melatonin– but worse– less exertion can occur during the correct time window. ie. not enough adenosine buildup in brain to require enough deep sleep (restorative delta phase)
The pitfall in CFS is that, shown in previous blogs here, The body does use glucose, but insulin resistance relevant to (but not caused by ) diabetes is commonly found. Additionally, a premature switch to anaerobic metabolism for energy creation is seen in stress tests. To me that is a systemic failure of the glucose metabolism. We are questioning the cause. We would hope that fatty acid metabolism would fill in.
Rob Phair did a podcast explaining how the Itaconate shunt could take ATP out of circulation during aerobic glucose metabolism and fatty acid metabolism.
He made the hypothesis that fatty acid metab. would also have its ATP confiscated (sequestered) leaving only one last energy source: protein metabolism. But the only protein it could get would be glutamate from just outside the cell. Glutamate: the brain- and other-cell-exciter. He explained that in such an eventuality, because the glutamate/excite, GABA/calm balancing system is programmed to work this way: the GABA shunt would allow some ATP production, but also sequester some.
So I am suggesting that, as mentioned in today’s blog, a CFS patient “can’t” do what would be best for all of her/his systems: exercise adequately. It’s obvious why not, but unclear what keeps it that way.
I only clearly recall one of the recovery stories found on healthrising, that of the athlete who was prescribed off-label the diabetes drug Mestinon. It prevents clearance of Acetylcholine (ACh) at the muscle receptor and cognitive brain cell receptor (among a few others). Normally ACh will release 1,000 times and be cleared 1,000 times per second. The breakdown chemical for ACh is inhibited by Mestinon, leaving the muscle “charged” longer than one millisecond per release.
It was likely gruelling, but being already an athlete used to pushing herself yo the limit, she retrained her metabolism.
My point?
Perhaps a CFS patient might consider or has already considered changing the statement “I can’t exert” to
I will only be able to exert when “_____”
function is restored.
My last suggestion is only that, since I do not experience CFS. I am wondering, when CFS patient says that he/she has learned to pace themselves or know their limits….whether they work til just before they drop, or whether they distribute exertion over the day.
I wonder because sluggish *clearance of lactic acid and other metabolism byproducts leads to Post Exertional Malaise and “payback” sometimes over days.
What would happen differently if a person did 1/5 of their limit 5 times, spread out over the day and evening? My aplogies for my ignorance if this has been already widely discussed.
There is definitely a circadian cortisol pattern problem in CFS, with too little when you wake, too much when you go to bed. ie. you may be cold with not enough glucose triggered when you wake, and too hot if not unable to fall asleep when you retire. And my reading on adenosine also mentioned that “a build-up of adenosine makes it less likely that a person will feel awake when exposed to light.
And one will naturally reply “but you said there wasnt ENOUGH adenosine to sleep soundly”. True. But what happens involving new adenosine build-during that bed period of 10pm-6 am? We don’t know. Your cortisol is high on the wrong side of the am/pm split…
So one more suggestion is to perhaps experiment with exerting closer to bed, but not too close to bed. Because we do know that cortisol rises toward bed in CFS instead of falling. I don’t recall the exercise rule for good sleep, but I think it is not to exercise past 1 hour before bed.
And can we not also consider cognitive work and emotional work equal to physical? So you have 3 to choose from.
I hope this has been thought-provoking.
Chris
Thank you Cort. This series is so helpful and sleep has been our son’s biggest issue. Do any of the studies highlight or focus on a deficit in a sleep stage? From a major university we found REM stage issues but no OSA because they look for major events. Fast forward, we went to an ENT sleep specialist and he found Obstructive Sleep Apnea 99 awakenings during REM. Our son also has dysautonomia (POTS). It seems many with POTS have connective tissue issues, MCAS (gastrointestinal issues) and “chronic fatiguing type symptoms”. With our son, his airway collapses. Not enough to register as OSA but enough to keep him from restorative sleep. We are addressing this now. I’m sure there are many causes but I wanted to share our finding, if it can help someone.
Chris,
I believe the diabetes drug is Metformin. From my understanding can be both ant-inflammatory, help with type 2 diabetes as well as increase gut mucosal lining. Mestinon is pyridostigmine used for MG. But off label by Systrom to help PEM in ME/CFS.
On a recent Patreon podcast both Kaufman and Ruhoy were very big on Metformin and its anti-inflammatory effects. We’ve had a couple of blogs on it.
https://www.healthrising.org/blog/2023/01/02/metformin-long-covid-fibromyalgia-chronic-fatigue-buster/
So Vickie kindly set me straight on Mestinon not being a diabetes drug and that got me to reread the Mestinon-based recovery here on the site.
Only because of that reread did this line hit me:
“Mestinon did not improve pain or fatigue but did reduce anxiety and improved restorative sleep.”
Why would it? I gather it is because of adenosine, as mentioned earlier. Let me express it in these words: Adenosine knocks you out. Knocked out as in deep sleep, not restless sleep.
Since Mestinon inhibits acetylcholinesterase, that allows aceytlcholine to keep open longer the cell membrane channel responsible for the influx/outflux of the electrolytes that polarize our muscle cells in order for them to attract magnetically (chemically) together end-to-end or “flex”.
I had only mentioned mestinon as one example of an intervention in an energy system gone wrong. With such a helping hand, then the patient could do the rest … as far as resuming exerting exercise. I was not thinking of ATP.
Mestinon allows more exercise, but ATP is the great dependency. If ATP complies enough that means that as it does the work adenosine will be released.
Have you ever been on a long hike with someone, or else watched crazy kids running around all day and someone said “They’ll sleep well tonight!” Adenosine.
So this is now the question in my head: Are skeletal muscle mitochondria unable to make enough ATP? Or are they simply not receiving the command to do so ? Acetylcholine is the command.
And Thyroid hormone homeostasis is also involved to trigger energy production and shiverring but also to say “okay *cool it* “, meaning dont overdo it because the event is over and if the muscle continues anyway, it will overheat.
Muscle mitochondria are not exactly lke incandescent light bulbs… but are similar. The goal of a bulb is to produce light but I think incandescents were famous for only 10 % of the energy emitting as light and the other 90% squandered as heat.
The goal of the mitichondria is to produce ATP that will move stuff around in/out of the cell. But a percentage of the energy is INTENDED to to be release as heat. 97 degrees.
If you are not actually locomoting, you still need to shiver occasionally. But my friend who has both CFS and FM says she can never get warm enough– AND SHE DOESNT SHIVER.
That’s not good. That is a lack of command from the HPA Axis to maintain optimal temperature.
In that case even shiverring will no longer output adenosine to make one sleep deeply.
Can anyone answer this? When a person takes Mestinon… does proper shiverring resume?
Myasthenia gravis is the product of an autoimmunity. An autoantibody is generated againt the Nicotinic Acetylcholine receptor on the muscle cell membrane (motor neuron synapse).
But CFS isnt MG, is it.
It provokes one to think back one previous step to the thyroid, or back even further to the Hypothalamus core temperature set point, which is flexible (see: fever, hypothermia).
After 3 years of analysis, I think that the failure of a body to fully heal from an infection during the acute stage (fever etc) and to still have inflammation, forces the Hypothalamus to choose hypothermia as the new temperature set point. Would it do that for the body to continue to starve the virus? Im not sure. Would it choose therapeutic hypothermia to save its own brain? ABSOLUTELY.
This, then, is my thought-provoking question to you:
Is the brain inflammation involving microglia pushing the brain too close to its maximum safe temperature?
Does exertion threaten to raise the brain temperature too high? Including mental exertion.
If I were a hypothalamus, having chosen hypothermia as opposed to death,
I DEFINITELY would not instruct the thyroid to instruct the muscles to exert.
And for this reason, Acetylcholine transmission would be set WAY back.
Will healing the brain heal the body?
Great discussion on sleep! It’s cool that top ME/CFS specialists are talking about lifestyle interventions like sleep hygiene (and disappointing, but not surprising that Stanford hasn’t given this info to patients – per another person’s comment). Perfecting my sleep hygiene was a key part of the layers of my own healing.
What I did, night before:
1. Put phone on silent in another room
Morning:
1. Sunrise sunlight exposure
2. No screens for first 90 minutes of the day (I journaled, meditated, visualized, earthed in the grass outside)
3. Zero news. I had to go into my settings or install plugins to block news sites that activated my stress hormones, which kept me in fight-or-flight. And I deleted certain mobile apps, only keeping messaging apps to stay connected with friends and family.
4. Stopped screens at 6 pm. (Later on I’d do an episode with dinner). Zero scary or high-adrenaline TV shows.
5. Dinner at 6
6. Bedtime between 9 and 9:15 am.
I also had: Full blackout blinds, No lights/electronics in bedroom, Low glycemic, protein rich diet. I also had the most physical activity within my health zone in the morning and afternoon, rather than midday. I read a sleep book that said midday movement was the least helpful for our circadian rhythm, and the other times were better.
I found it worked best when I started getting up earlier, though the first few times were tougher, rather than trying to go to bed when I wasn’t tired.
Yes, it was kind of like living like a monk, but it was so great for me.
Nice! Great suggestions. I just started having dinner between 5 and 6 and lo and behold I had my best sleep in quite a while and even remembered my dreams – which were kind of nightmarish involving some sort of demon – but which didn’t phase me at all (lol).
*9 to 9:15 pm rather. (: Oh good to know!
I think I really want to go back to this. (What I shared was my schedule from 2019-2020.) We have often been having dinner at 8 pm after toddler in bed, but the times we had things together to all have dinner at 5/6 pm it was great.
Right now I’m on a 10:30 pm to 7-7:30 schedule, and I want to go back to the 9:15 to 6-6:30 schedule. But yesterday I blocked some sites that were my culprits, and I think that plus the earlier dinner are going to help nudge me back to the good times. My sleep right now is good, but when I was on the 9:15 pm bedtime and the sunrise rising, really felt the best during the day.
Lol re the demon dreams! At least you’re not phased by them!!
I’ve had delayed phase sleep/reversed sleep most of my 30+ year ME experience. I am a bit weary of experts, all of whose expertise is based on “normal”, assuming that it will all translate directly onto ME, instead of realizing that ME does not conform to “normal” by definition, and there are other things at play. And I think there is far too much tendency to consider the sleep issues to be causative rather than the downstream effect I think they are.
I tried some sleep aids early on, but they made me feel worse than without. I tried all the recommended sleep hygiene rules, but they did not help.
For years, I tried to force myself to strict wake and sleep times, but that only ever worked for at most 1 month at a time, at the end of which my schedule would spontaneously revert to its preferred state (awake at night, sleeping during the day). If I did not allow it to do so, the stress of sleep deprivation would cause my immune function to drop so that I would come down with the next thing I encountered – and what would be a very mild cold in someone else would be a very bad one for me, and that in turn would cause a drop in my baseline, which meant sleeping during the day, which meant I was back to the start.
As long as I was working even part-time, I had to stay on some sort of schedule, but it was a constant wrestling match that I liken to stretching a rubber band; it can only go so far before either a) you lose your grip or b) it breaks, and then either way it snaps back into its default state. I would stick to the schedule, I’d get sick. I would stick to the schedule, I’d get sick. Over and over. On the rare occasions I didn’t get sick, it would revert anyway. In other words, it could not be trained no matter how hard I tried. And I tried for decades.
When my ME worsened to the point that I had to give up work, I decided I was done fighting what my body clearly wanted to do, and was going to let it find the schedule it preferred. Since then, I have noticed the following things:
– The more I am pushing or exceeding my energy limits, the worse my sleep is. The more rested I am, the better and longer I sleep.
– My body does not get enough rest during sleep, so it must rest *before sleeping*. I need several hours of quiet downtime before bed in order to sleep well. This is key, as I notice that situations where the unexpected may occur** require all my brain/body systems to be always “online” and ready to respond. This readiness apparently takes a lot of energy – but it seemingly takes a *devastating* amount to come online quickly on demand; like requiring afterburners to go from 0 to 100 instantly – and that drains the tank completely, which is Bad. So while there is any likelihood of being needed, those systems will not shut off. And therefore I cannot rest. Long periods of external quiet including “narrow focus” activities (I like listening to music, watching YouTube and solving variant sudoku) before bed allow my body to shut down systems that deal with outside influence and make it easier to sleep. This is different than the sleep hygiene approach which says to turn everything off.
**The unexpected can be very mundane and non-threatening, such as a short conversation: I don’t know what the other person will say, therefore my brain must be ready to take in information, sort it, and muster a response to whatever is said at a moment’s notice. This apparently uses multiple areas of the brain and my body finds this tiring to do.
– External stimulation or demands will make my body push later and later. I conclude that the delayed phase/circadian rhythm disruptions are my body’s attempt to lessen outside stimuli and the possibility of the unexpected with its high cost. At night it is quiet, there are no interruptions, and very few unexpected events. When my body is stressed, it needs more of this, so it stays awake all night and makes me sleep during the periods of the day when Things Might Happen. That, of course, causes other life complications, but this isn’t being driven by the conscious processes, it’s instinctive defense.
– Sleep fragmentation is the first and last symptom of PEM for me. My pain and other symptom flares will hit 24-48 hours after the event and may last days to weeks, but my sleep will suffer immediately, and I will sleep only in 1-2 hour chunks, with long wakeful periods in between. This will last for a while after other symptoms have resolved. I now do not consider my crashes over until my sleep has gone back at least to 5-6 hours in my initial sleep, with hopefully another segment of 2-3 shortly after. This can often take 4-6 weeks or longer in a serious crash or continual rolling PEM.
– On the rare occasions when I manage to keep well under my energy limits for an extended period and my body considers “Critical Demand Mode” over, my circadian rhythm and sleep begins to normalize all by itself, shifting back toward normal timing and duration. This is lovely, but life has a way of presenting unavoidable exertions, and so then we go back into crisis mode.
– My sleep, whatever it is doing, seems to stem *out of* my underlying ME, not cause it. While lack of quality sleep piles on difficulty and symptoms in addition, even when I am getting good sleep my underlying ME does not improve.
While sleep aids may work well for some, they don’t work for everyone and I think it is not a solution, and certainly not in any way a fix or cure for ME. It is merely imperfect symptom management, and should be considered in those terms. Things that are “core symptoms” in diagnostic terms, in my opinion are just big secondary effects, and not the root problem in itself.
There is a tendency to think “Repair and healing systems go to work while sleeping, so getting more sleep = healing and repair”. This is true of normally functioning systems. But I think the healing and repair systems themselves are working inefficiently or unable to meet demand, which is *causing* sleep to not be restorative. The more that backlog builds up, the more the body increases its coping mechanisms. If we want to really make a difference, chasing down why the body can’t clean up/repair is going to be the bigger solution.
Hydroxyzine is widely available in a 10 mg tablet.
I was rather disappointed by what these doctors had to say. I didn’t find anything new in what they were saying.
I’ve tried sleep hygiene until its coming out of my ears. Been prescribed with numerous anti depressants to help and they definitely did not help. I’m on low dose Naltrexone and it does nothing for my chronic insomnia but helps with muscle pain.
My insomnia is being helped, by preventing me from waking up so often during the night, by a relatively new medication which suppresses wakefulness receptors in the brain: Doridorexant. This sadly does nothing to help me get to sleep which takes several hours each night.
There is a desperate need for new and original research into sleep problems amongst people with ME.
A new ME/CFS study is underway and hopefully we’ll have a better sleep and pain drug by next year.
Great info to add to my ongoing research on sleep. I am creating an online sleep course specifically for fibromyalgia in the coming months.
Cort – you might be interested to know that sleep expert Matthew Walker warns about the detrimental impacts of cannabis on natural sleep cycles. He acknowledges it helps some to fall asleep but that it has other negative impacts. If you google Matthew Walker marijuana you’ll see some podcast clips where he talks about it.