

Check out Geoff’s narrations
The GIST
The Blog
(The GIST is about halfway down the page on the right)
Health Rising’s series of “What’s Up Doc?” Zoom videos asks chronic fatigue syndrome (ME/CFS), fibromyalgia (FM), long COVID and related diseases experts “What’s up? What’s exciting you now?” The first talk features Lauren Stiles, the leader of Dysautonomia International.
The Zoom Interview is below and below that is an overview of the interview that includes some added content.
I am new to this and for some reason the video starts about halfway through. Please use the scroll bar at the bottom to return it to the beginning.
Lauren’s Story
We will get to the “What’s Up” part but first, I had to ask her about Lauren about the illness that led her to found Dysautonomia International. A healthy, energetic 31-year-old environmental law attorney, Lauren suddenly developed postural orthostatic tachycardia syndrome (POTS) following a ski accident that produced a concussion and intracranial hypertension. Bringing up thoughts of craniocervical instability and a compressed brainstem in my mind, anyway, she described a spine that had been compressed together not by lax tendons but by an accident.
The injury damaged her autonomic nervous system, which then tweaked her immune system, which then apparently destroyed many of the small nerve fibers in her body. She described a harrowing trip through the medical profession that took her several years, but she finally self-diagnosed POTS from her hospital bed and got a neurologist – who had apparently never heard of POTS – to agree that’s what she had.
After another convoluted journey, she ultimately came to find that Sjogren’s Syndrome – a disease she believes is greatly underdiagnosed in these diseases – had triggered her POTS. IVIG treatment – which came with its own set of serious issues – helped greatly. At no time, over the first couple of years, did Lauren have an easy ride through our medical system.
- Check out Lauren’s full story here.
In 2012, Lauren, who had been engaged in non-profit work before, founded Dysautonomia International (DI) – a non-profit organization that quickly became the leader in the dysautonomia field. Dysautonomia International produces yearly international conferences, educates patients, provides information on doctors, and has dysautonomia, POTS and long-COVID research funds).
A Big Family…With Lots of Cousins
Lauren believes that ME/CFS, FM, POTS, long COVID and others are more alike than different.
Because dysautonomia is the one factor that shows up in ME/CFS, FM, POTS, Long COVID, etc., Lauren may be the most centrally located person I will talk to.
As a dysautonomia expert, Lauren has her eyes on everything from more obscure autonomic conditions like baroreflex failure and Autoimmune Autonomic Ganglionopathy to conditions like chronic fatigue syndrome (ME/CFS), fibromyalgia, and long COVID. Noting that POTS was the most common, and ME/CFS the second most common, comorbid diagnosis in a long-COVID study, she called them “cousins”.
She believes these diseases are more alike than different. Things like small fiber neuropathy, antibodies that disrupt the autonomic and sensory nerves, inflammation, and metabolic abnormalities appear to pervade all these diseases. Her assertion that if we find something in one disease, it will likely show up in the other diseases, brought to mind Avindra Nath’s belief that if we solve one, we will solve them all.
Lauren was a case in point. Through her healthcare journey, she met the criteria for chronic fatigue syndrome (ME/CFS), fibromyalgia (FM), POTS, and mast cell activation syndrome (MCAS) before she was finally diagnosed with Sjogren’s Syndrome.
That made me think of fibromyalgia (FM). Few people associate FM with orthostatic intolerance or POTS, yet multiple studies suggest OI may be common in FM. That makes sense given the evidence that autonomic nervous system problems could be contributing to the pain, sleep, digestive, exercise, and standing problems. At least 8 studies suggest that orthostatic intolerance is present in FM, yet the OI issue is virtually ignored. A 2018 Health Rising poll (n=457) found that 83% of FM patients said their doctors had never recommended a tilt table test.
Even if the FM patients had taken a tilt table test, it’s likely that many of them would have still been misdiagnosed, which is why I thought DI’s decision to provide transcranial doppler equipment to several doctors/research groups was simply brilliant. As Lauren explained, ME/CFS and POTS have near identical symptoms, but if you don’t show a high heart rate on tilt table testing, you’ll likely be told that everything is fine.
Visser, Van Campen and Rowe have shown, though, that virtually everyone with ME/CFS – whether they have increased heart rates while standing or not – has reduced blood flows to the brain. That is the core problem with these diseases – not increased heart rates. With this equipment, doctors can show that everything is not fine after all, and that brought up one thing Lauren is really excited about: the STAT earpiece.
The Exciting STAT…err Lumia Earpiece
Lauren said she’s “genuinely excited” about the potential of the STAT earpiece (recently rebranded to Lumia) which can measure blood flows to the brain. (She’s not the only one. I recently talked to ME/CFS expert Theresa Dowell, who is really excited about the device’s potential to assess treatment effectiveness, pacing, etc. We thought the earpiece would be available by now but I was told November is now the expected release date.)
THE GIST
- The first of Health Rising’s “What’s Up Doc?” Zoom interviews with ME/CFS, FM, long COVID, etc,. experts features Lauren Stiles, the founder of Dysautonomia International. The “What’s Up Doc?” interviews focus on what’s exciting these experts right now, but I first had to ask Lauren about the illness story which led her to create Dysautonomia International. (See the video at the top of the blog.)
- Lauren was a healthy, athletic, environmental lawyer when a ski accident caused a compression of her spine and intracranial hypertension (high pressure in her brain). It took Lauren two years before she diagnosed herself with postural orthostatic tachycardia (POTS) from her hospital bed.
- Her ski accident damaged her autonomic nervous system, which tweaked her immune system, which then destroyed most of the small nerve fibers in her body. After another convoluted journey, she ultimately came to find that Sjogren’s Syndrome – a disease she believes is greatly underdiagnosed – had triggered her POTS. IVIG treatment – which came with its own set of serious issues – helped greatly. Check out Lauren’s full story here.
- In 2012, Lauren founded Dysautonomia International the leading non-profit researching, educating and advocating about autonomic nervous system conditions. Because dysautonomia is the one factor that shows up in ME/CFS, FM, POTS, long COVID, etc., Lauren has her eyes on things happening in all these diseases.
- She believes these diseases are more alike than different. Things like small fiber neuropathy, antibodies that disrupt the autonomic and sensory nerves, inflammation, and metabolic abnormalities appear to pervade all these diseases. Her assertion that if we find something in one disease, it will likely show up in the other diseases, brought to mind Avindra Nath’s belief that if we solve one, we will solve them all.
- Tying all these strange and mostly neglected diseases (ME/CFS, FM, POTS, long COVID) together, Lauren asserted that “chronic autonomic dysfunction is going to lead to chronic immune dysfunction“. That made sense, as the autonomic nervous system is a major regulator of the immune system. The tie that binds all these diseases together is some sort of autonomic impairment.
- That made me think of fibromyalgia. Studies indicate that dysautonomia could be contributing to everything from pain to sleep to problems standing (orthostatic intolerance), yet few FM patients are ever tested for orthostatic intolerance, and FM is rarely studied in conjunction with its close relatives.
- Lauren noted that very early in the course of their illness, people with rheumatoid arthritis and Crohn’s disease already exhibit autonomic dysfunction. She explained that during an infection, the autonomic nervous system explodes into action – sometimes to the point of no return – which brings us to a possible ANS tamer – vagus nerve stimulation (VNS).
- Dysautonomia International has funded three successful VNS trials in autonomic nervous system diseases and Lauren is excited about the potential VNS holds for POTS, long COVID, ME/CFS, FM, etc. Parasym, a European VNS company, is attempting to obtain approval for its device in the US this year.
- Turning to the $1.6 billion NIH Recover initiative for long COVID, Lauren, who has sat on several RECOVER committees, described a mostly out-of-touch effort that never took patient engagement, or experts from the ME/CFS or other post-infectious illnesses, seriously. She said, “When you give nearly 2 billion dollars to people with no experience in post-viral syndromes, don’t be surprised when what you get is something that’s disconnected with what the patients actually need”, and does not believe that RECOVER is improving.
- Remarkably, POTS did not have an ICD code that enabled doctors to electronically document its existence until Oct. 2022. Having one now makes it possible to understand how prevalent POTS is, the cost of treating it, helps with disability, and has prompted pharmaceutical companies to start digging into POTS for the first time.
- Lauren was excited about Stanford research showing that insulin resistance may be contributing to POTS and vice versa, and the new STAT (now called Lumia) earpiece that measures blood flows to the brain. That device should help validate these diseases in the eyes of doctors and give patients and doctors a way to evaluate treatments and improve pacing. It should be available in November.
- Another subject of great potential for these illnesses is something called ganglionitis which refers to immune-triggered damage to the nerve bundles that relay autonomic and sensory signals to the brain. Ganglionitis could explain many of the strange sensory, as well as the autonomic nervous system, problems in these diseases.
- Lauren is much better now, but after being bedridden for years, she knows how tough this illness can be and how hard it can be to keep going. She said, though, that “so much research” is going on she that felt “strongly confident” we will see better treatments soon.
- Health Rising’s Quickie Summer Donation Drive is underway. You can support us by using the donation widget at the bottom of this blog, or with a check, Amazon Gift card or bitcoin gift.
Sjogren’s Syndrome – a Majorly Underdiagnosed Illness in the ME/CFS, POTS, FM, Long-COVID Sphere?
Lauren suggested whatever condition we get diagnosed with first will tend to swallow up all our subsequent symptoms. With our search effectively over, we get stuck with the treatments available for that condition while possibly missing the treatments available for other conditions – which brings up Lauren’s Sjogren’s Syndrome story.
Lauren believes that, absent her Sjogren’s Syndrome diagnosis and the door it opened to IVIG, she could have been bedridden for life. Her POTS, mast cell problems, migraines, and post-exertional malaise all got much better on IVIG.
Check out Health Rising’s IVIG Series
- An IVIG Chronic Fatigue Syndrome (ME/CFS) / POTS Treatment Success Story: IVIG#1
- Are Chronic Fatigue Syndrome, POTS and Fibromyalgia Autoimmune Dysautonomias? IVIG #2
- The Case for IVIG Treatment in Chronic Fatigue Syndrome (ME/CFS), Fibromyalgia, Small Fiber Neuropathy, and POTS : IVIG#3
She believes that Sjogren’s Syndrome is widely underdiagnosed in the ME/CFS, POTS, fibromyalgia and long-COVID communities. The Sjogren’s diagnostic criteria is something of a mess. For one, the diagnostic criteria used by doctors is research-based, not clinically based; i.e. it’s highly restrictive, so much so that Lauren herself, because she does not have the antibodies to Sjogren’s (about 40 percent of SS patients do not) would not meet it.
Lauren pointed out a study which showed Sjogren’s patients with a more neuropathic presentation (like those with ME/CFS for fibromyalgia) are more likely not to have SS antibodies. While no drugs have been FDA-approved, off-label drugs are available and clinical trials are underway. As noted above, Lauren’s ability to get IVIG was critical to her improvement. (Note that she highly recommends getting intramuscular IVIG shots over the infusions).
- She recommended following the Sjogren’s Advocate blog
- Check out Trish’s ME/CFS/FM/myasthenia gravis story for another story about how a different diagnosis opened up new treatment options
From a Spinal Injury to POTS, ME/CFS/FM and Sjogren’s Syndrome

Concussions trigger short-term and sometimes long-term autonomic nervous system dysregulation and immune dysfunction. (Image by Max Andrews, CC BY-SA 3.0 Wikimedia Commons)
How Lauren’s spinal injury led the development of SS is unclear, but Lauren noted that a study showed that concussions send the autonomic nervous system into a tizzy. Immediately after a concussion, both symptomatically and at the biological level, everyone after a concussion looks like they have POTS (!) Most people, of course, recover, but a subset get diagnosed with a chronic illness.
She believes that the reason that people who have experienced a concussion have a lifetime increased risk of all-cause mortality is inflammation.
Tying all these strange and mostly neglected diseases (ME/CFS, FM, POTS, long COVID) together, she asserted that “chronic autonomic dysfunction is going to lead to chronic immune dysfunction“. That made sense, as the autonomic nervous system is a major regulator of the immune system. The tie that binds all these diseases together is some sort of autonomic impairment.
Could autonomic nervous system dysregulation set the stage for trigger these and more diseases? She noted that very early in the course of their illness, people with rheumatoid arthritis and Crohn’s disease already exhibit autonomic dysfunction. Lauren explained that during an infection, the autonomic nervous system explodes into action – sometimes to the point of no return – which brings us to a possible ANS tamer – vagus nerve stimulation.
Vagus Nerve Stimulation
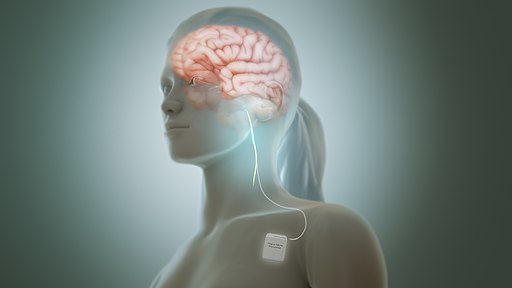
Dysautonomia International’s trials suggest VNS could be one tool in the complex chronic illness toolkit. (Manu5, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons)
Dysautonomia International recognized the autonomic implications of COVID-19 very early in the COVID pandemic and attempted to get a vagus nerve stimulation (VNS) study going that would crank up the parasympathetic tone and down-regulate inflammation during acute COVID.
(Interestingly, Lauren noted that benzodiazepines (Ativan, Xanax, Klonopin, Valium) can do the same thing! It’s their ability to stabilize mast cells and tone down sympathetic nervous system activity (and not their ability to reduce anxiety) that makes them so helpful at times in these diseases.)
A presentation at the upcoming Dysautonomia Conference will show that vagus nerve stimulation helped pediatric POTS patients with Ehlers-Danlos Syndrome (EDS). Another study found that NEMOS – a European vagus nerve stimulator – reduced symptom severity and functionality. In all, three different Dysautonomia International-funded trials have shown efficacy in 3 different groups with POTS – a nice track record. If Parasym, a European VNS company, gets approval for its device in the US, people in the US will have more options. Parasym will be presenting at the DI’s international Conference this year (June 28-30, 2024).
When I suggested that wouldn’t it have been great if the RECOVER Initiative for Long COVID had funded a vagus nerve stimulation (VNS) trial, Lauren, (her voice rising a bit (:)) said RECOVER turned down a VNS application because it hadn’t done its homework. It rejected the application because the VNS would not lower the heart rate in POTS.
Vagus nerve stimulation (VNS), however, is not used in POTS to lower the heart rate. (You’d have to stimulate all day long for it to do that). Instead, it’s used – for a few minutes a day – to lower the inflammation. That episode highlighted a big hole in the RECOVER program: somehow, despite the very early evidence that POTS was a problem in long COVID, it lacked experts in POTS.
Lauren believes that VNS is a benign, safe possibility for people with all these diseases. Because the field is dominated by small companies, it’s taking a while for the devices to take hold. Check out some recent VNS trials.
- The Stavrikis VNS POTS Trial
- Vagus nerve stimulation in rheumatoid arthritis and lupus
- Vagus nerve stimulation POTS and epilepsy
The RECOVER Initiative Flops Again
“When you give nearly 2 billion dollars to people with no experience in post-viral syndromes, don’t be surprised when what you get is something that’s disconnected with what the patients actually need”. Lauren
RECOVER misses again. Will we ever get good news from the RECOVER Initiative?
Lauren was on multiple planning committees for RECOVER and described a mostly out-of-touch effort. Lauren felt that for the most part, RECOVER never took the patient input aspect of RECOVER – which RECOVER has lauded again and again – seriously. While some individual investigators did involve patients, she felt it was given lip service at the highest levels of the RECOVER leadership.
Dysautonomia International’s request that researchers with decades of experience studying these diseases be included at the leadership level was ignored. She said:
“When you give nearly 2 billion dollars to people with no experience in post-viral syndromes, don’t be surprised when what you get is something that’s disconnected with what the patients actually need”.
Ouch! When asked if RECOVER was adjusting to the many critiques and bad press it’s received, the answer was “absolutely not”. (Double ouch!) Instead of acknowledging that changes need to be made, instead she’s seen more “defensiveness” and an effort to close the ranks on RECOVER’s part. In short, RECOVER feels they’re doing just fine.
Researchers from prestigious institutions like Harvard, Yale, and Stanford all urged RECOVER to do functional autonomic testing in a subset of its patients, yet 3 years later, it is still not doing that. The consequences – no data on functional autonomic dysfunction associated with long COVID from the biggest long-COVID effort on the planet – leaving doctors clueless. Meanwhile, research outside of RECOVER has shown that 70-80% of long-COVID patients have dysautonomia.
(Note that RECOVER is doing tilt table testing in its Tier III patients but isn’t employing the functional autonomic nervous system tests recommended. It is also funding two autonomic nervous system clinical trials – one using IVIG and one using Ivabradine.)
Lisa McCorkell, the founder of the Patient-Led Research Collaborative, feels much the same way about the RECOVER Initiative.
POTS Gets an ICD Code – and Interest from Drug Companies
Getting an ICD code for POTS was huge.
Early RECOVER Initiative studies relied on electronic health records which, because there no ICD code for POTS existed concluded there was no POTS in long COVID. (The researchers apparently missed the fact that because no code for POTS existed it couldn’t have shown up in their studies.) Outside RECOVER, of course, studies found not only that was POTS common in long COVID but that it was associated with significantly more disability.
Getting the ICD code (G90.A) for POTS in Oct. 2022 was a signature achievement of Dysautonomia International. Despite the fact that POTS is not a disease of the heart or an arrhythmia (it’s a tachycardia), it used to land under ICD code I49.8 “Other specified cardiac arrhythmias”. That code included numerous other medical conditions like Brugada syndrome, re-entrant atrioventricular tachycardia, ectopic rhythm disorder, and other arrhythmias – none of which have anything to do with POTS (POTS is not an arrythmia condition).
Dysautonomia International presented evidence for a change to the US Center for Disease Control committee, which approved the new ICD code (G90.A) Instead of being shunted in under heart conditions, POTS is now found in the autonomic diseases section.
Getting an ICD code may seem like a small thing, but it has big consequences. It makes it possible to understand how prevalent POTS is, the cost of treating it, helps with disability, and of course – electronic health data studies will now pick it up. Interestingly, Lauren said the implementation of the ICD code has also prompted pharmaceutical companies to start digging into POTS for the first time.
The goal now is to make doctors aware of the code change so that they can put it in POTS patients’ medical records. Check out Dysautonomia International’s letter that patients can give to doctors that helps explain what the ICD code and POTS are all about. (ME/CFS’s ICD code, by the way, is G93.32)
The Insulin Resistance Dysautonomia Connection
Could insulin resistance be causing dysautonomia and vice versa? (Image from public domain: Wikimedia Commons)
When asked what else excites her now, she noted that Cyndya A. Shibao at Stanford recently published a paper, “Worsening Postural Tachycardia Syndrome is Associated with Increased Glucose Dependent Insulinotropic Polypeptide Secretion“. After Dr. Shibao noticed that may POTS patients feel worse after a high carbohydrate meal, she showed that POTS patients eating these meals release a peptide called GIP which tells the pancreas to release insulin, potentially increasing the risk of insulin resistance; i.e. pre-pre diabetes. My first thought was, “Finally someone is exploring this very common reaction”.
Plus, sympathetic nervous system activation – a common finding in POTS – stimulates GIP. (She noted that normal blood norepinephrine levels may not reflect high intraneural norepinephrine levels). Insulin sensitivity, in turn, can cause sensory and autonomic nerve damage: a new pathway to POTS shows up! Plus, the finding lends itself to possible treatments. (Note that insulin resistance may predispose one to fibromyalgia as well.)
The other silver lining is the huge funding that diabetes and associated conditions gets, which Dr. Shibao has been able to tap into. (Dr. Shibao recommends that POTS patients try a low carb diet.)
An NIH Center for Post-Infectious Diseases
Lauren said she was 100% behind the effort to build a Center for these diseases at the NIH, helped to draft the legislation, and explained why. She talked about a failed attempt by a well-known and well-funded researcher at a major university to get a multidisciplinary genetics/immune/dysautonomia-funded long-COVID study at the NIH. The researcher was told by the various institutes that they couldn’t fund it because other institutes were responsible for different parts of the study. The application was rejected without even being reviewed.
Right now, ME/CFS researchers are not talking to or collaborating with FM researchers, POTS researchers are not talking to ME/CFS researchers, etc. An NIH Center that prioritized subjects of interest, that had these diseases be studied together, that was intent on showing commonalities between them, etc., would allow all these diseases to move together so much more quickly.
Could the Ganglia Have it?
Take post-exertional malaise (PEM), the signature symptom of ME/CFS. Is it found in POTS and, if so, in what percentage of people with POTS? Right now, we have no idea. After I brought up the recent Gulf War Illness (GWI) study showing no PEM in GWI, Lauren pointed out that a GWI study found damage to the autonomic and sensory nerves (ganglionitis). Might autonomic and sensory nerve damage be the tie that binds all these diseases together? (In an upcoming interview, FM researcher Daniel Clauw will highlight how important he believes damage to sensory processing plays in FM.)
A dorsal root ganglia. (Image DP Wikimedia- Commons – https://commons.wikimedia.org/wiki/File:DRG_Chicken_e7.jpg)
Unfortunately, there are no tests right now for ganglionitis but Lauren (again showing how much she is up on all these diseases) noted that autopsy studies have shown damage to the ganglia in ME/CFS. Ganglia problems have also shown up in post-treatment Lyme disease, and animal data indicates that COVID-19 can damage the autonomic ganglia.
Dr. Martinez-Lavin has proposed that the buck may stop at the dorsal root ganglia in fibromyalgia. Plus, the fibromyalgia study that transferred serum from FM patients to mice found that the mice suffered from damage to the autonomic ganglia. (A POTS serum study is underway…).
Small fiber neuropathy testing can pick up damage to the sensory nerves, but most labs do not assess the autonomic nerves that are just under them. Note that many things (ischemia, metabolic problems, insulin resistance, infection) can cause damage to these nerves and small fiber neuropathy can be found in many diseases. The good news is that these small nerve fibers can grow back. Lauren lost 85% of small nerve fibers. After IVIG, her small nerves weren’t completely back to par, but they all grew back.
Thanks to Dysautonomia International’s input, RECOVER’s autopsy study is going to assess the autonomic ganglia in long COVID. One wonders what role damaged autonomic and sensory nerves will, in the end, play in these diseases. They could explain a lot.
Lauren ended the interview by emphasizing the need to explore the overlaps between all these different, yet similar, fields. Creating an Office at the NIH would be a major step forward.
- Check out Dysautonomia International’s International Conference that is underway right now. DI makes it very easy to get a recording of the conference – just $25
- See Ten Facts Doctors Should Know About POTS
- Take the Dysautonomia International Decade + long POTS Survey

Lauren says: “hang on!”. She believes better treatments are coming.
Better Treatments Coming
Lauren is much better now, but after being bedridden for years, she knows how tough this illness can be and how hard it can be to keep going. She said, though, that “so much research” is going on she that felt “strongly confident” we will see better treatments soon.
Health Rising’s Quickie Donation Drive Blasts Off!

Health Rising’s summer donation drive blasted off! Thanks for your help:)
Thanks to the over 100 people who have contributed over $5500 to Health Rising’s Quickie Summer fundraising drive.
Access is important and as this blog shows – and as other blogs in the What’s Up Doc? series will show – Health Rising has access to the top experts in the ME/CFS, FM and long COVID fields and we are talking to them. If that’s the kind of access you want to see please support us!
;





If the medical system is our collective immune system (though that may be a highly imperfect metaphor) it struck me reading this article that ICD codes (International Classification of Disease codes) are almost like antibodies. Once we have the ICD code with which to recognize the dysfunction and not mistake not for something else, this sets in motion a cascade of systemic responses that can draw on various resources (like Diabetes funding!). This really shows how valuable is the clarifying work that Dysautonomia is doing. Understanding that confusion in assessment and diagnosis will inevitably lead to a confused medical response really helps explain the last several years of my life!
I never really understood how important ICD-10-CM codes until she explained it. Thank goodness for our patient orgs. It also shows how different and misunderstood POTS has been – it was shoved, I guess, in the arrhythmia category because they didn’t know where else to put it.
Speaking of ICD codes, I don’t know if you meant to link the old “chronic fatigue unspecified”, but the new ME/CFS Code is G93.32 https://www.icd10data.com/ICD10CM/Codes/G00-G99/G89-G99/G93-/G93.32
Another excellent piece, Cort, thank you. I pre-ordered the STAT/Lumia earpiece and am looking forward to trying it. IVIG has also helped reduce my POTS, but I am still severe/moderate ME, but also have diagnosed (but untreated) atlantoaxial instability and had tethered cord release surgery 2 yrs ago. So many pathways to this disease.
Thanks – funny that Google search gave me the old one! I knew patient orgs had done “something” with ICD codes. Good for them! 🙂
I wonder if it’s all immune related with the immune system attacking different things in groups of us? Did the surgery help?
After 35 yrs. I still keep getting a different label everytime I go to a new specialist.
Remember folks, your medical “chart” stays with you the entire life.at least up here in can can land it does.
so ,if they tell you you’re crazy who knows how and when they could use that against you.
If we look at these labels, it’s merely some high up bunch of people making all these names up based mostly on symptoms.
The entire medical system and their teaching to students is set up and funded through universities by big pharma
Make up a bunch of labels to stick on people then sell the desperate people some very expensive drugs so that not only the treating doctor profits but the profits get made all the way down the line.
Here in Canada the patient starts out seeing a general practitioner that really has been taught very little…the GP sends you off to different specialties. I found once i got to these different specialties, they start doing blood tests,etc. Then tell you firstly that there’s nothing wrong….that’s how the first journey for me started decades ago. The one GP I had decades ago did nothing but tell me war stories. It just continued to get worse from there.lots of narcs in the canadian system.yep, the canadian system is free but comes with a huge WARNING label.
I began looking at my long fraudulent journey from a money point of view and how much money I had lost and how much money they gained.yet they still have not one stitch of medical science, other than low red cells, to give to me after decades of frustration….frustration to put it mildly. By the time I got to the shrink, which i was forced to go, I was starting to sound very upset verbally…who wouldn’t have given the fact that i had over 100 symptoms….then I got another label….a mood dissorder….I got up and left. Soooo done with going to them.im not sure, if the and when the truth and cure comes out, oif I will trust them
My neighbour got a woodworking sliver under his thumbnail….they called him and told him his thumb had cancer.he no longer has a thumb…..
$$$$$$$$$$$$$$$$$$$$$$
I think the fact that so many of us fit so many different labels underscores Lauren’s point – that these diseases are more alike than different and that the best thing we could do is study them together.
Yes, yes, yes! Compression contributed to my spinal CSF leak and blood flow issues can lead to every single symptom in so many of these conditions. I love to see this.
Current diagnostics are flawed and patients are getting a diagnosis like POTS and told to just drink water without any further investigation. I have a compressed internal jugular and transverse sinus stenosis on one side, a partial IJV compression on the other, and bone spurs impeding CSF drainage in my spine but most doctors will dismiss all of those factors entirely. I cannot wait for the science to catch up on this.
I just saw an NPR article noting the connection to CSF and Alzheimer’s and Parkinson’s as well.
I thought that was so interesting and I’m kind of sad now that I didn’t pick up on that at the time. It was a compression injury that ended up tweaking her autonomic nervous system which apparently contributed to her immune system going haywire – leading to Sjogren’s and the loss of small nerve fibers across her body…no wonder she was so impaired!
There are so many ways to get at this illness….
Honestly, it took a long time to make all the connections myself. We have to go so deep to find the actual cause and there’s little help out there.
My theory is that when it starts with illness it’s because the illness raises pressure (or the medicine used to treat it does) and that can either lead to immediate blood flow or volume issues, or it can compress veins from too much pressure on them, or trigger leaks, or mast cells (which I’m now reading can actually be triggered by physical pressure) and cause connective tissue damage, and the longer it goes on the more systems can be collapsed or affected by the cascade (both quantity and severity). So a hundred ways in but all leading to blood flow/volume and structural changes. And every case is going to be slightly different depending on anatomy and affected areas. I would love to see some MRV imaging studies on these conditions.
Afaik Sjögrens is dormant in the body until a trigger sets it off. So maybe also a ‚regular‘ accident or a virus could have set it off? So that the route could have been: accident — Sjögrens—SFN&dysautonomia? Or at least for other patients it could happen that way?
Thanks Cort (and Lauren) this is really interesting! I resonate with so much of this and can see others have already commented about CCI-type issues as well.
I have severe ME, POTS, MCAS gastro issues etc and recently a specialist EDS physio told me they believe I have undiagnosed hEDS and CCI and that I need to try a cervical collar asap… Yikes. I’m pretty scared and I’m desperately hoping I don’t end up needing surgery, but it really helps seeing articles like this and your other blogs talking about it, as well as people commenting too. I think it’s probably a lot more common than is recognised and the sooner people are diagnosed and treated then hopefully worsening like mine and so many others might possibly be avoided.
Good luck with the cervical collar. You’re in an interesting place – the cervical collar could reduce symptoms – yah! – but then it might lead to surgery!
I would just be as well informed as you can be – Kaufman’s and Ruhoy’s Unraveled Series has good stuff on that surgery. Good luck!
Hi Cort! I know right – double-edged sword! I think on balance if it turns out to be the root of the problem then the awfulness would be worth it, my fear is ending up needing an op and then it not helping much or making things worse… but then you’ve got to try something or nothing will change!
I guess everyone with these diseases is part of a massive test phase in history – in decades to come people will have more guidance on what works and doesn’t but for now we can only go on the info we all have now (much of it thanks to you!)
Thanks for reminding me about the Unraveled series – it was so helpful!
Lauren is one of the many people who helped me on the path to get diagnosed with OCHOS by generously answering a question I emailed her. Thank you, Lauren!
On a different tack, it’s important to note that the Stat/Lumia earpiece is not registered as a medical device and therefore cannot be used specifically for diagnosis. The company has plans to make a medical version, which costs a lot more due to all the regulatory requirements. This will take some time, I imagine.
In the meantime, a Doppler ultrasound is the way to go for proving low blood flow to the brain.
And the Stat device is the way to go for monitoring your blood flow for personal use. I can’t wait to get one!
Interesting that some researchers are looking at insulin resistance or a abnormal body response to being glucose challenged as a stressor to POTS. While i don’t have POTS (nOH) i go thru the same tachycardia and lower blood pressures after eating a carby meal and the effects can last 4 ish hours or so.
I did read a study that tested the GIP levels in POTS patients when glucose challenged and the finding was that the release of the GIP hormone stayed abnormally high for up to 3-4 hours which can cause elevated heart rates and also works as a vasodilator which was hypothesised to cause the post meal drop in blood pressures. normal release of the GIP peptide is normally short lived in non dysautonomic folks.
Also, I just got a date for my Doppler ultrasound testing!
I’m having it done in Melbourne, Australia, theough the public system. Once my testing is done, anyone will be able to access the same testing providing their specialist is able to order and interpret it.
(The testing unit doesn’t have a tilt table, so it will be done during a NASA lean test.)
Nice! Love to hear your results if you feel comfortable doing that.
Will do!
Cort, I ended up cancelling the test. I did a three-week medication washout, but it turned out not to be enough. My symptoms didn’t come roaring back as I expected, but rather trickled back slowly, and I wanted to be tested when fully symptomatic.
I was kicking myself that I hadn’t done the washout for longer, but brain fog and a total lack of guidance from my “specialist” were factors.
I asked him to push the date back – he refused. I asked him if he would order a second round of testing when felt that I was fully symptomatic – he refused.
So I cancelled.
I didn’t want to have the test done if it was likely to be inconclusive, as that would then be on my records.
I haven’t given up on having the testing, but I have dumped the specialist 🙂
I suspect I have ganglionitis. My head and eyes are always burning and all the nerves in my body feel inflamed. I do have SFN that is exacerbated greatly by activity. What is causing such inflammation and damage to the dorsal root ganglia?
I can only image its the immune system. Check out this fascinating paper showing neutrophils attacking the sensory ganglia.
https://www.healthrising.org/blog/2023/05/10/immune-disease-neutrophils-fibromyalgia/
Wow…… Lauren is incredibly impressive .!!! I love her “ common sense” ideas. While researchers are involved with looking into microscopic dysfunctions they miss the bigger picture ….ie the macroscopic view that Lauren describes.How do we all end up in the same place in spite of such an array of initial triggers ?!! Her insistence on patient input is so important but sadly a missing and crucial piece of the puzzle.
Having Ehlers-Danlos, I’ve long been aware of Dysautonomia International and how interwoven autonomic dysfunction is intertwined with all these conditions. For a time I would take my HR and BP readings laying and sitting up at various times a day and at times I would definitely make the 30 beat difference required for POTS. Unfortunately during a Tilt Table Test, I was deemed ‘normal.’ One thing people should know is that POTS can be a dynamic condition and one test often does not detect it. Tell that to the doctors!
Not sure what the ‘functional autonomic nervous system test’ mentioned in Cort’s article is. The NASA lean test? For myself my HR is always very high when I am upright.
Ehlers-Danlos folks were quite upset to read research articles declaring that we all suffered from ‘anxiety’ (high heart rate). Sorry, no! What it often is, is a dis-regulated autonomic nervous system.
As alluded to in the article, after a bunch of ‘normal tests’ or even one or two real diagnosis, many doctors stop looking–and can miss something (like the Sjogrens mentioned) and really not see the total picture. I can’t tell you how many doctors have come up to the boundary of their practice area and say, sorry, I don’t do (neurology, cardiology, rheumatology or what ever else) and so the treatment ends there. All this stuff is so intertwined!
What I also want to know is how people convince their doctors to prescribe IVIG. It is so very expensive and insurance companies will frequently deny. I’d also want to find some step by step (for Dummies) directions of how to convert my TENS machine for vagus nerve stimulation. What are the settings? Where to place the leads. All the videos I’ve looked at recommend experimentation… I don’t want to fry my ear! Or give my heart the wrong instructions! I think I also might be suffering from PTSD as I electrocuted myself as a child.
The time of the day the test is taken can make a big difference and how long it lasts. Then there’s the more important finding – reduced of blood flows to the brain which you need the transcranial doppler for.
I’m not sure of all the autonomic function tests. There is the sweat test, gastric emptying test, pupillomotor testing, Valsalva test, and probably more.
Hi Nancy – if you are on Facebook, search for the group called AVA A Vagus Adventure. You will find links at the top of the page to tell you how to use a TENS, and lots of other great advice. Good luck!
That initial doctor clearly didn’t know how to practice medicine. Faking it all the way. This is happening way too much. How on earth did these folks pass their exams?
Hello
Im just wondering where Perrin treatment comes in all this! massage and cranial needed to encourage the lymphatic system to work the right way…not the wrong way (which can start due to a virus or some other type of trauma) where the toxins start to travel up outside the blood vessels (causing what are named ‘varicose blood vessels’) up to the brain & cant drain away as they should do, thus causing CFS/FM symptoms
I want to look more into lip biopsy for sjögren’s. So she is saying if you ever smoked your test might be false negative? Would not the nicotine have cleared from the tissues after awhile?
It’s covered briefly in this review article:
https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2021.792593/full
I haven’t read the associated references, but hope they would explain it further.
Why intramuscular IgG? It’s common to do IVIG or subQ IgG but this is a first for me. What kind of dose is used? The autoimmune dose is so much higher than for immune deficiency and it is difficult to get it with subQ, much less IM. I’m curious about this protocol. How did it get insurance approval without the Sjogren’s antibodies?
Cort! Thank you! This brought tears to my eyes.
After being severely sick for 2yrs I was dx with SFN in 2018. Didn‘t provide explanation for my diasabling symptoms, neuropathic pain was the least of my concerns. In 2022 I was dx with ME, in 2023 POTS (I suggested both and had to look for docs who diagnosed me).
I am now in the process of getting evaluated for Sjögrens. I have a weak positive ANA, speckled as in lupus/sjögrens, ss ab were neg but I am waiting for retest and more tests. I hope I will be able to receive scIgg treatment next year (had severe reaction to IVIG once administered falsely). Two SFN patients suggested to seek out a dx, both only dx via lip biopsy without SS ab present.
It means the world to me that Lauren says she would likely be bedbound without treatment and THAT HER SF LARGELY GREW BACK.
Great, but how did she get better? I mean….?????????????????