

Geoff’s Narrations
The GIST
The Blog
As painful as it is, the pain in IBS isn’t caused by structural damage to the gut; instead, it appears to be caused by difficult- to-detect nerve activation.
Health Rising hasn’t published much on irritable bowel syndrome (IBS) and that’s a shame. Not only is it present in chronic fatigue syndrome (ME/CFS), fibromyalgia (FM), and long COVID, but IBS is part of a family of disorders that also includes chronic pelvic pain, interstitial cystitis, migraine, chronic low back pain, and many autoimmune diseases.
In each of these disorders, researchers have been unable to find a physical cause for the pain. For instance, despite all the bloating and pain found in the guts of people with IBS, the intestines look just fine. In fibromyalgia (FM), no one has been able to come up with enough evidence of damage to the muscles to explain the pain found in FM. Likewise, the intense pain in migraine isn’t associated with physical damage.
Diseases like these, for which clear physical causes haven’t been found and which also cause other symptoms (poor sleep, fatigue, cognitive issues, mood problems), have come to be called nociplastic disorders, and are primarily believed to be central nervous system disorders.
They also include a significant subset of people with disorders like rheumatoid arthritis/osteoarthritis and other autoimmune disorders where pain in the joints spreads beyond, producing widespread pain and other symptoms.
The GIST
- Not only is irritable bowel syndrome (IBS) present in chronic fatigue syndrome (ME/CFS), fibromyalgia (FM), and long COVID, but it’s also part of a family of disorders that also includes chronic pelvic pain, interstitial cystitis, migraine, chronic low back pain and many autoimmune diseases.
- These are all called nociplastic disorders. Nociplastic disorders occur when clear physical causes haven’t been found that could cause the symptoms (pain, poor sleep, fatigue, cognitive issues, mood problems) found in them. With their similar symptom presentation, ME/CFS, FM, and long COVID are all considered part of the nociplastic family of disorders.
- Researchers have been digging deeper into the gut tissues and are making progress. For over 15 years, IBS researchers have been taking biopsies of the colon, then spinning them in a centrifuge to separate the liquid, or supernatant. Then they expose gut neurons to the supernatant – and watch as, bang! – the neurons go off like rockets – spewing out electrical signals that produce pain and other symptoms.
- This study assessed the role mast cells play in IBS by exposing the supernatant from IBS patients, patients with a mast cell disorder called mastocytosis, and healthy controls to the nerves in the gut. It also determined if the entire gut is involved in ME/CFS.
- Despite the fact that all the IBS and mastocytosis patients experienced the same symptoms (bloating, diarrhea, abdominal pain), only the supernatant from the gut biopsies of the IBS patients sent the gut nerves through the roof. The authors also concluded that IBS was caused by a “general phenomenon (found) throughout the gut“.
- They did not find increased numbers of mast cell numbers in the biopsies of the IBS patients. Nor did they find any evidence of increased mast cell degranulation or histamine levels. They concluded that “mast cells are not involved in nerve activation”, and proposed that proteases (enzymes that break down proteins) are the main problem in IBS. While factors like histamine from mast cells and serotonin play a role in IBS, it’s the proteases that appear to set them off.
- It appears that in IBS, nerve activation in the gut activates vagal nerves situated outside the spinal cord in the dorsal root ganglia (DRG). The DRG is a central gathering place where sensory signals get sent to the central nervous system, and DRG activation is found in fibromyalgia.
- From there, the central nervous system activation spreads to cause symptoms like widespread pain, fatigue, sleep, cognitive and mood problems.
- it’s become clear that protease-driven protein breakdown in the gut is helping to set it off, and that provides an opportunity. One review called protease inhibition “one of the most promising novel therapeutic strategies to explore” in IBS but warned that more work is needed to identify the specific proteases involved.
- Because proteases appear to set IBS off, efforts are underway to find a way to inhibit them via gut flora modification, next-generation probiotics, fecal transplants, and drugs.
- With their wide range of symptoms, nociplastic diseases have been assumed to be primarily central nervous system disorders. This present study suggests IBS is also a nervous system disease – but begun by an abnormal activation of the gut neurons.
- In a recent interview, chronic pain researcher Daniel Clauw (coming up) suggested that a different kind of inflammation called “neurogenic” or nerve-associated inflammation is in play in these diseases. Something similar may have shown up recently when fibromyalgia researchers found that immune cells called neutrophils, taken from FM patients, attacked the sensory nerves in FM mice.
- The starting point in nociplastic diseases like ME/CFS and long COVID is less clear, as no specific tissues appear to be affected; i.e. they seem more like – at least from this vantage point – purely central nervous system disorders.
- Progress is being made in understanding what’s going on nociplastic disorders, though, and will be explored in future blogs. For now, it’s good to know that ME/CFS, FM, and long COVID belong to a larger category of nociplastic diseases. A breakthrough in one could benefit all.
- A recent interview with chronic pain researcher Daniel Clauw (coming up) suggested that these nociplastic diseases may often begin in a difficult-to-detect activation of the peripheral nerves that progresses to a central nervous system problem. He believes that a different kind of inflammation called “neurogenic”, or nerve-associated inflammation, is in play.
IBS is a complicated disease. Three types of it exist and it’s embedded in a complex physical environment regulated by millions of bacteria. In a presentation last year, Laura Pace, a neurogastroenterologist, threw cold water on diagnoses of IBS and small intestinal bowel overgrowth, stating that the diagnostics are so crude that they tell us little about what’s going on in the gut. She asserted that only detailed analyses of the gut tissues are going to tell us what’s going on in IBS.
Researchers have been digging deeper into the gut tissues and are making progress, and that leads us to a set of studies that have come out of Germany for over ten years.
How deep have IBS researchers gone? For over 15 years, they’ve been taking biopsies of the colon, and then spinning them in a centrifuge to separate the liquid, or supernatant. Then they expose gut neurons to the supernatant – and watch as, bang! – the neurons go off like rockets – spewing out electrical signals that produce pain and other symptoms.
Further analyses found that while serotonin and histamine stimulate the nerves, the major players are enzymes called proteases that break down proteins.
The Mast Cell Mystery
The role mast cells play in IBS has been unclear – some studies suggest they play a role and some that they don’t. During her presentation, Pace remarked on a study finding that eosinophils, in particular, and T-cells infiltrating the gut lining were causing the most problems in IBS.
It’s not that mast cells aren’t having an impact. Activated mast cells found near nerve fibers could be having a big impact on symptoms. Interestingly, Pace believed that histamine-containing foods have, at most, a “local” impact and don’t produce the systemic effects found in these diseases. (She employs mast cell stabilizers (H2 blocker 2-3x a day, and oral Cromolyn 4x a day (slowly titrated up) and/or quercetin with her patients).
Still, while mast cell inhibitors can help, they don’t always provide relief or don’t provide total relief. We either need better mast cell inhibitors or some other cells are involved.
The Study
The present study aimed to provide insights into the mast cell question by comparing mast cell density and histamine levels in people with IBS-D (D-diarrhea), people with a systemic mast cell disease called mastocytosis, and healthy controls. In gut-associated mastocytosis-D, high levels of mast cells build up in the gut. When they dump their loads, increased fluid levels and peristalsis (gut muscle activity and rapid motility) result in vomiting and diarrhea (apparently to get rid of the excess fluid).
The small study (n=32) also expanded past gut findings by determining if nerve activation in more parts of the guts (small and large intestine) is involved.
Results
Gut-wide Problem
IBS appears to result from the activation of nerves across the gut.
Even though all the IBS-D and mastocytosis patients experienced the same symptoms (bloating, diarrhea, abdominal pain), only the supernatant from the gut biopsies of the IBS patients sent the gut nerves through the roof.
(The supernatant from mastocytosis patients activated some gut neurons but to a much lesser degree, and the researchers concluded that they responded similarly to the healthy controls.)
Since the supernatant from both parts of the gut from the IBS-D patients activated the gut nerves, the authors concluded that IBS-D was caused by a “general phenomenon (found) throughout the gut“.
Mast Cells Take Second Billing
They did not find increased numbers of mast cells in the biopsies of the IBS-D patients. Nor did they find any evidence of increased mast cell degranulation or histamine levels.
They concluded that “mast cells are not involved in nerve activation, at least not in the patient groups enrolled in this study” and that, as their past studies have suggested, proteases produced by immune or epithelial cells are the main culprit in IBS. While factors like histamine from mast cells and serotonin play a role in IBS, it’s the proteases that appear to set them off.
How to explain, then, the fact that mast cell stabilizers can help in IBS? They couldn’t, except to note that mast cells may be nestled so closely next to nerves that even small (undetectable to them) amounts of mast cell activation could set them off.
Note that some studies have implicated mast cell activation in IBS as well. The situation is complicated, and factors other than mast cells must also play a role in IBS.
Prior studies have teased out the nerve connection in IBS. The nerve activation in the gut activates vagal nerves situated outside the spinal cord in the dorsal root ganglia (DRG). The DRG is a central gathering place where sensory signals get sent to the central nervous system, and DRG activation is found in fibromyalgia. From there, the central nervous system activation spreads to cause symptoms like widespread pain, fatigue, sleep, cognitive and mood problems.
The authors stated that protease finding helps explain one of the strangest findings in the field. Instead of becoming more tweaked, when the nerves in IBS biopsies were repeatedly exposed to a cocktail of IBS-activating factors (histamine, serotonin, tryptase, and TNF-α (IBS-cocktail), they became less activated; i.e. they had become desensitized. The authors of that paper proposed that a protective mechanism was trying to shut the nerves down. Proteases can do this.
IBS is a complicated disease, but it’s become clear that protease-driven protein breakdown in the gut is helping to set it off and that provides an opportunity. One review called protease inhibition “one of the most promising novel therapeutic strategies to explore” in IBS but warned that more work is needed to identify the specific proteases involved.
Because proteases are produced by the bacteria and other substances in our gut, altering our gut flora could conceivably reduce the proteolytic activity that is turning on the gut nerves. Another review suggested that next-generation probiotics will be able to turn down this activity and help return the gut to normal functioning. A fecal transplant study using stool from a donor with low proteolytic activity and containing the bacteria Alistipes putredinis is underway to see if the stool can dampen the high levels of proteolytic activity found in IBS and provide relief.
A serine protease inhibitor called nafamostad reduced the gut pain in a rat model of IBS. Another approach is to increase the levels of endogenous opioids in the gut to relieve pain.
Back to Nociplastic Disease
Because researchers have had trouble finding clear evidence of pathological problems in the tissues in pain (the gut, muscles, etc.), and because of the widespread symptoms (pain, fatigue, cognitive and mood problems), the prevailing thesis is that these diseases are primarily central nervous system directed. This present study suggests IBS is a nervous system disease as well – but one where the problem starts in an abnormal activation of the gut neurons – which took some deep digging to uncover. (No wonder it’s been such a mystery).
A recent interview with chronic pain researcher Daniel Clauw (coming up) suggested that these nociplastic diseases may often begin in a difficult-to-detect activation of the peripheral nerves that progresses to a central nervous system problem. He believes that a different kind of inflammation, called “neurogenic” or nerve-associated inflammation, is in play.
Something similar may have shown up recently when fibromyalgia researchers found that immune cells called neutrophils, taken from FM patients, attacked the sensory nerves in FM mice.
That suggests a different and hard-to-detect kind of inflammation affecting the sensory nerves, in particular, present in these mysterious diseases.
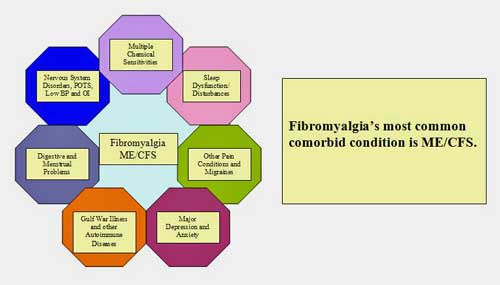
Fibromyalgia and ME/CFS are one of a series of conditions featuring nervous system-derived (nociplastic) pain and other symptoms.
The starting point in nociplastic diseases like ME/CFS and long COVID is less clear, as no specific tissues appear to be affected; i.e. they seem more like – at least from this vantage point – purely central nervous system disorders.
How nerve activation in the gut turns into a nociplastic disease featuring widespread pain, fatigue, sleep problems, etc., remains a mystery, but finding a starting point – nerve activation in the gut – should help.
Progress is being made in understanding what’s going on in nociplastic disorders, and that will be explored in future blogs. For now, it’s good to know that ME/CFS, FM, and long COVID belong to a larger category of nociplastic diseases. A breakthrough in one could benefit all.






Vagus nerve in play–yet again!
Within a month of getting Covid last year, my tolerance for animal protein plummeted. (and anxiety spiked) I have poor GAD genes, and one of my longest symptoms back to 2019 is sensitivity to emulsifiers like carrageenan and guar gum, etc. Seeing as glutamate is a key symptom in Cell Danger Response, I’ve assumed it was a glutamate issue. I’m considering Memantine. Trying to do Brain retraining etc…a TENS machine is helping vagus nerve, too..
Interesting. I don’t have LC. I have ME and I’ve found that animal protein is one of the few things I can tolerate. I don’t like eating animal protein so frequently but I have to eat something or I’ll wither away…I’m 5’4” and fight to keep my weight from dipping down under 100.
Thanks Cort. You might want to check out Dr. Nancy Rizzo and Health Curcuits.
To me, IBS represents the first time I have been looked at as being a fake by a long list of specialists. After years of diarrhea (10 + times/day) I sat there while this arrogant know-it-all faced old man explained to me that what I was explaining was not possible and that I was exaggerating. For most of my working years, I had to wake up more than 2 hours before work time in order to give time to my guts to calm down long enough for me to get there. Having CFS for more than a decade now, I had to face a long list of those old men telling me I am lying. Every time you relay researches like these, I can’t help but scream at all of them (in my head until I meet one of them) ‘I TOLD YOU IT IS REAL ‘. You are a precious human Cort. Thank you for being there for us.
The two-hour lead time is real!
The first doctor I pleaded with did nothing but tell war stories about himself from. The second WW.
he had a propeller of a plane mounted above his gloating desk.That was 40 years ago and I’m, believe it or not,still being shuffled between specialist….they want to bill the free medical system,paid for by our taxpayers.
I refuse to go anymore…simply put ,a fraudulent medical system in business to keep people sick and on as many meds as they can peddle.
Can we believe it ,somebody wants the Sackler name left on the building
I suppose you’ve had a colonoscopy. Your “before work” comment rang bells with me. My record was 17 times and this went on for many months!! I had a colonoscopy, polyps removed and no further trouble
This was around 16 yeaars ago before ME, and I’m “in the system” and checked 3 yearly. I’m UK. Just a thought
You are right, I had a few until I got tired of being insulted…. The last time I went, they diagnosed me with (drum roll) MIGRAINE !!!! LOL ! I looked at yet another old man, shook my head and never went back. I’m in Canada (Quebec) but I can see that we sadly all have the same story wherever we come from…
Don’t follow your reply. Colonoscopies have served me well and unrelated to ME.
On migraine, I started them 2 years into ME… silent/ with/without aura/ painful I had one daily for 8 years, A LOT of drugs and neuro testing. But my goodness they exacerbated all my symptoms…I’m severe.
Then 2 and a half yrs ago the UK GP put me on Propranolol and they have all but cleared up. Of course it’s possible I just grew out of them but I’m 66. When II still get the occasional one I take a Sumatriptan.
Hi Cort,
Is there a way that I can communicate directly with you? Do you have an email address that you would share with me?
My email is mardicrane2166@gmail.com
Kind regards,
Mardi
Exciting news today that Ozempic can reduce brain inflammation and is being tested for Parkinson’s. Perhaps something to research for MECFS? https://www.wired.com/story/the-benefits-of-ozempic-are-multiplying/
Whoa! A weight loss and diabetes drug can also reduce neuroinflammation and do other things. It’s apparently because the drug affects receptors found across the body. This shows that help could be just around the corner in an already available; i.e. repurposed drugs:)
From the article
That is really something!
I am a member of a number of insulin resistance facegroups and constantly come across people that have developed pancreatitis following treatment with Ozempic. This drug is dangerous but appears to be marketed for an increasing number of ailments.
Ozempic is another, very bad substance: https://bestnewshere.com/live-qa-with-dr-ardis-nicotine-ozempic-bird-flu-more-your-questions-answered-2024/
Yet another miracle cure. I would not use this drug. Certainly not if you have IBS. For people without diabetes, semaglutide can be harmful to health. For example, you may experience serious problems with your stomach and intestines.
Cort, before you go touting the possible benefits of a drug like Ozempic, go to the manufacturer’s web site and see what adverse effects they list.
Here is what they have on Ozempic:
Important Safety Information
Do not share your Ozempic® pen with other people, even if the needle has been changed. You may give other people a serious infection, or get a serious infection from them.
What is the most important information I should know about Ozempic®?
Ozempic® may cause serious side effects, including:
Possible thyroid tumors, including cancer. Tell your health care provider if you get a lump or swelling in your neck, hoarseness, trouble swallowing, or shortness of breath. These may be symptoms of thyroid cancer. In studies with rodents, Ozempic® and medicines that work like Ozempic® caused thyroid tumors, including thyroid cancer. It is not known if Ozempic® will cause thyroid tumors or a type of thyroid cancer called medullary thyroid carcinoma (MTC) in people.
Do not use Ozempic® if you or any of your family have ever had MTC, or if you have an endocrine system condition called Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
Do not use Ozempic® if:
you or any of your family have ever had MTC or if you have MEN 2.
you are allergic to semaglutide or any of the ingredients in Ozempic®. See symptoms of serious allergic reaction in “What are the possible side effects of Ozempic®?”.
Before using Ozempic®, tell your health care provider if you have any other medical conditions, including if you:
have or have had problems with your pancreas or kidneys.
have a history of diabetic retinopathy.
are pregnant or breastfeeding or plan to become pregnant or breastfeed. It is not known if Ozempic® will harm your unborn baby or passes into your breast milk. You should stop using Ozempic® 2 months before you plan to become pregnant.
Tell your health care provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, herbal supplements, and other medicines to treat diabetes, including insulin or sulfonylureas.
What are the possible side effects of Ozempic®?
Ozempic® may cause serious side effects, including:
inflammation of your pancreas (pancreatitis). Stop using Ozempic® and call your health care provider right away if you have severe pain in your stomach area (abdomen) that will not go away, with or without vomiting. You may feel the pain from your abdomen to your back.
changes in vision. Tell your health care provider if you have changes in vision during treatment with Ozempic®.
low blood sugar (hypoglycemia). Your risk for getting low blood sugar may be higher if you use Ozempic® with another medicine that can cause low blood sugar, such as a sulfonylurea or insulin. Signs and symptoms of low blood sugar may include: dizziness or lightheadedness, blurred vision, anxiety, irritability or mood changes, sweating, slurred speech, hunger, confusion or drowsiness, shakiness, weakness, headache, fast heartbeat, and feeling jittery.
kidney problems (kidney failure). In people who have kidney problems, diarrhea, nausea, and vomiting may cause a loss of fluids (dehydration), which may cause kidney problems to get worse. It is important for you to drink fluids to help reduce your chance of dehydration.
serious allergic reactions. Stop using Ozempic® and get medical help right away if you have any symptoms of a serious allergic reaction, including swelling of your face, lips, tongue, or throat; problems breathing or swallowing; severe rash or itching; fainting or feeling dizzy; or very rapid heartbeat.
gallbladder problems. Gallbladder problems have happened in some people who take Ozempic®. Tell your health care provider right away if you get symptoms which may include: pain in your upper stomach (abdomen), fever, yellowing of the skin or eyes (jaundice), or clay-colored stools.
The most common side effects of Ozempic® may include nausea, vomiting, diarrhea, stomach (abdominal) pain, and constipation.
What is Ozempic®?
Ozempic® (semaglutide) injection 0.5 mg, 1 mg, or 2 mg is an injectable prescription medicine used:
along with diet and exercise to improve blood sugar (glucose) in adults with type 2 diabetes.
to reduce the risk of major cardiovascular events such as heart attack, stroke, or death in adults with type 2 diabetes with known heart disease.
It is not known if Ozempic® can be used in people who have had pancreatitis.
Ozempic® is not for use in people with type 1 diabetes.
It is not known if Ozempic® is safe and effective for use in children under 18 years of age.
Please click here for Prescribing Information and Medication Guide for Ozempic®.
Ozempic® is a prescription medication.
Novo Nordisk provides patient assistance for those who qualify. Please call 1-866-310-7549 to learn more about Novo Nordisk assistance programs.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit http://www.fda.gov/medwatch or call 1-800-FDA-1088.
Terms of Use
Privacy Policy
Cookie Policy
Privacy Request
About Novo Nordisk
Site Map
Contact Us
NovoFine® and Ozempic® are registered trademarks of Novo Nordisk A/S.
Novo Nordisk is a registered trademark of Novo Nordisk A/S.
All other trademarks, registered or unregistered, are the property of their respective owners.
© 2024 Novo Nordisk All rights reserved. US23OZM00096 June 2024
Thanks, Cort. Dr. Tyna Moore has a different take on Ozempic as a type of peptide that it is quite effective if obtained, in low-dose form, from a compounding pharmacist. This avoids the problems associated with the brand name pharmaceuticals. Here’s a link to one of her talks.
https://www.drtyna.com/ozempicuncoveredyvideo4evergreen?dfp=D2JJ1JX5N2
Sulfur metabolism in the gut poisons gut cells that make GLP-1. Desulfovibrio overgrowth is linked to Parkinsons I think?
A video from Nick Norwitz mentions bismuth and inulin as potentially helpful for excess hydrogen sulfide producing bacteria – see https://www.youtube.com/watch?v=hiCxpHDAlbs&t=149s
Thanks for this Cort. Is there a potential pathway in this work to explain post-exertional malaise?
I have experienced symptoms of what I had assumed to be IBS for years–multiple bowel movements a day (sometimes 10 as Nathalie Langevin mentioned in a previous comment above) but was never formally diagnosed with a GI disease. I just chalked it up to another facet of ME/CFS that gets ignored by regular doctors.
The test those of use with abnormal bowel symptoms should be taking is called the
GI MAP test through Diagnostic Solutions Laboratory. I don’t think most allopathic (regular Western doctors) physicians are aware of this test. It is a complex analysis of every bacterial, viral, and parasitical pathogen in the stool. This test is not normally covered by insurance and costs is about $350–it can be ordered online.
I mention this because this test just diagnosed me with a Cdiff infection, the presence of occult blood and a high level of gut inflammation.
The multiple bowel movements a day as well as the darkness of the stool now make sense. I wanted to write in about this because I think ME/CFS patients tend to tolerate symptoms that healthy people would not. We get worn down by years of having doctors ignore or dismiss our symptoms.
Although traditional doctors would treat this with Vancomycin (an oral or IV antibiotic) I am choosing to use an alternative medicine approach.
Hoping this helps somebody else!
I heard Dr. Pace (referenced in the above article) speak recently and she indicated that stool tests do not capture the organisms from the part of the GI system that they need to.
IBS in ME/CFS
I was diagnosed with ME/CFS nine years ago. Almost from the beginning, I suffered with IBS and Interstitial Cystitis. I was constantly taking Immodium to control the diarrhea and the pain and urge to urinate constantly was very frustrating. Was told by two different urologists that I did not have Interstitial Cystitis, even through I had all the symptoms. Three years ago, I went on the KETO diet to lose weight. I noticed that the IBS and bladder pain completely went away. I suspected that it might be that I had given up gluten-containing foods. When I would eat food with gluten, the diarrhea and painful bladder came right back.
Also, about two years ago, I began noticing that I would have energy and ambition in the mornings, but as soon as I ate something, I immediately experienced the flu-like symptoms and had to go to bed. At first I thought that it might be carbohydrates but then discovered that it didn’t matter what I ate, I would still have that reaction. So, I began delaying eating as long as I could, sometimes late afternoon, but would ultimately become weak from no food. Then I discovered that if I took two Benedryl, the severe flu-like symptoms would improve significantly within 30 minutes. I would also take NyQuil at night with the same result.
Someone on this blog told me that it sounded like I had Mast-Cell Activation Syndrome. I recently saw Dr Bonilla for the first time at Stanford University ME/CFS Clinic. He told me that there was new thinking that the mast cells are not as significant as was thought and that the antihistamines helped because they helped control inflammation, probably in the vagus nerve. He prescribed Abilify to try.Right now, I have just begun the slow titration process, so I won’t be able to tell if it’s helping for a while.
I also just got over having Covid for the first time. The extreme fatigue is worse and I just can’t seem to kick it. I hope that this is not my new normal.
IBS is common in those with autism too.
https://www.healthline.com/health/autism/ibs-and-autism
Could you send us the Link to the original publication of your article. Thanks in advance💙🙏💙
Would this mean that taking protease enzymes for help with digesting food might be harmful?
I am wondering that as well. I take protease enzymes with my meals, too.
I am wondering about taking protease enzymes with meals as well. Does anyone have any ideas, thoughts, knowledge about this?
Now I understand why Big Pharma ignored us for years, whether it was diabetes skin problems, or even mental health, who knows what else.
My IBS and extreme fatigue literally disappeared with energy healing focused on the vagus nerve. The rest of symptoms are still present.
They should have measured Tryptase levels not Histamine… (to very likely find elevation in IBS and the mast cell connection)
Yes, Dr Prusty (Germany) is testing for tryptase in long Covid and ME/CFS.
According to him, If it exceeds 5-6 µg/L, there is probably a problem.. Allergies, histamines, SAMA?
Personally, my tryptase levels are at 6.72 µg/L. I was refused an appointment with a specialist in mast cell activation because in France, tryptase levels are considered normal if lower than 11.40 µg/L.
That’s a very good point. How could they miss that
Dear Cort, I thank you for keeping up with all of this. We get hopful and then we crash. You keep at it and bless you for that. Love, Javen
Die Hauptursache all dieser Erkrankungen ist eine Überlastung des Körpers mit Giftstoffen die er von selbst nicht mehr in ausreichendem Maße los wird.
Es sind so viele schädliche Substanzen in Lebensmitteln, in der Atemluft oder in Medikamenten, die die Körperfunktionen massiv beeinträchtigen. Um diese Substanzen wieder auszuscheiden werden große Mengen an Vitaminen und Mineralstoffen benötigt. Fehlen nur einige Bausteine, weil davon zu viel verbraucht wurde, gerät das ganze System außer Kontrolle und es entstehen vielfältige Beschwerden, die nach und nach immer schlimmer werden 😬
I’m late 50s & have IBS (& lower back pain).
What I’ve tried over the years below.
Helps:
1) Monthly colonics
2) Codeine
3) Merbeverine hydrochloride
4) Low stress environment
5) Cigarettes
6) Cherry Coke with sugar
7) Oxytech laxative
8) Loving wife
9) Loving cats
Doesn’t help:
1) Diets
2) Monosodium glutamate
3) Stress
4) Pre or probiotics
5) Digestive enzymes
6) High fibre
7) Antacids
8) Exercise
9) Ridged meal times
10) Peppermint tablets
Conclusion.
Helps:
1) Colonics beyond obviously removing faecal matter also resets the gut flora, which I suspect is the main benefit.
2) Opiates were a fabulous tool but sadly are so addictive.
3) Antispasmodics really help on the rare occasions of gut spasms, otherwise being of no help at all.
Conclusion
Doesn’t help:
1- 10) What I eat or drink really makes no difference.
Doctors can’t help.
I am quite thin.
IBS affects all aspects of my life including my ability to earn money.
5) Digestive enzymes with protease and HCL drunk before every meal had no effect.
I have been taking Norco four times a da for years and I don’t know where I would be, physically and emotionally, without them.
Kat please be careful with the opiates. I was great at first but 26 years of addiction later has taken it’s toll on me.
Thanks for your input, Rich. I began taking them after two major spinal-fusion surgeries, which happened after I was diagnosed with ME/CFS. Then I was referred by my pcp to a rheumatologist here to take over the care of my ME/CFS. He has now retired. He was a great guy and knew much more about the disease than any doctor I had seen, but still very little. I knew much, much more just by reading Health Rising. He was a pain doctor, so he put me on one Norco 10-325 and two Trammadol, four times a day, plus a muscle relaxer as needed. I was grateful. As you know, several years ago, after so many deaths from opioids, the restrictions became so-very stringent. My PCP has taken over that treatment because my rheumatologist retired. At that time, I took myself off of the Trammadol. As you probably are aware, doctors, now, can only prescribe the exact number of tablets for a 30-day supply. I cannot even take an extra two or three tablets during the month because I will run out before I can refill my prescription. I expressed concern to the rheumatologist about my being addicted to opioids. His response was, “You are not addicted, you are dependent “. I understand what you are talking about. It would be so easy to keep increasing the dosage, as sometimes it would really help with more severe pain. But since I don’t have extra tablets, I cannot do that.
https://www.facebook.com/share/GydktwUhyG1bEHz4/?mibextid=LQQJ4d
Kat, my wife Claire also has M.E. and runs the above Facebook page which you might find helpful. It’s called “It’s all about M.E.”
Also many people get caught up with “medicines” that are addictive and end up with two problems instead.
So I’m a member of Facebook group “Painkiller Addiction Support UK” for addicts like me and also those who just want to better manage their medications.
A lot comes up for me reading this article as my personal health journey with fibromyalgia (diagnosed 20 years ago) has strong ties to my gut health.
For over a decade I kept complaining about serious gut issues and every doctor said “it’s just part of fibromyalgia’ and did nothing. It turned out I had a severe H.Pylori infection (for 20 years) that had caused a whole raft of other gut issues. I only uncovered this from doing my own research and requesting the tests. Looking back I feel totally neglected as they never even did basic parasite tests or sent me for scopes.
Once I treated the H.Pylori with antibiotics 20 years of IBS mostly cleared up. I then had to try many elimination diets before I got clear on what I could digest and what created bloating, constipation… and widespread body PAIN!
Now I have a perfectly functioning gut, no stomach aches and my average daily pain score is 0.
However, I still have energy issues, nervous system regulation issues, a bit of POTS and OI (if I don’t keep on top of taking ORS and exercising) and I have to live a very healthy stress free lifestyle, and take a bunch of meds and supplements (inc LDN and valacyclovir) to stay pain free and functioning. I don’t get classic PEM (I do strenuous exercise everyday) but I’m not fully functioning so I’m not quite sure what diagnostic basket I fit into these days.
When I was still in a lot of pain I had started to accept that it was nociplastic, because that’s what some hypothesise….but it turned out for me it wasn’t. It was inflammation from gut and immune issues (as well as pesky herpes – thanks to Cort and Dr Prigden for the info on that!).
I don’t really trust that most researchers are looking at the gut in the right way. They do basic tests or scopes and find nothing. But having studies gut health through a functional and microbiome lens for a decade now, I can see that so many people are not looking after their gut and I have learnt that there are dozens of ways a gut can be disrupted that standard doctors have no idea about.
Dr. Datis Kharrazian has brilliant online courses that teach this. His Gut Health, Food Sensitivities and 3D Immune Tolerance courses explain the science. He ties together neurological, gut, immune and hormone functions in a way I have never seen and it’s helped me to understand my health issues better and slowly work to address each issues.
Is there a link to the study? I can’t seem to find one in this post.
I would like more information on IBS-C
The intestinal environment is very complex with a number of factors that play into each other. Popular research keys up onto the microbiome which turns out is a little more complex than what was understood previously. For instance, butyrate producers are now known to aid in a number of things but cannot proliferate in hostile conditions.
Barrier integrity is now known to be a key feature and shows up in a multitude of studies of recent. 70% of the immune system lies there as well and that immunity can not only address systemic infections but also localized. Systemic meaning system wide infections such as viral and localized as pathogenic organisms that lodge in the gut that don’t belong there.
IgA is an immunoglobulin that resides in the gut that plays a role in maintaining immunity. And many metabolic pathways that have interplay with the gut environment such as AMPK.