

Geoff’s Narrations
The GIST
The Blog
BOLD MRIs sound like the ticket for diseases like chronic fatigue syndrome (ME/CFS) and long COVID. BOLD MRIs measure blood oxygen levels (energy production) across the brain and what could be more telling than that?
THE GIST
- BOLD MRIs measure blood oxygen levels (energy production) across the brain and what could be more telling than that? Our brains are never always turned on – that would take too much energy. Instead, when a part of the brain is needed – say, during cognitive activity – the mitochondria in that part of the brain take up more oxygen in the blood.
- In a process called “neurovascular coupling” our brains quickly and efficiently transport blood to the active region. How well they can do this not only determines how well tasks are carried out but also plays an important role in the “energy economics” of the brain. Sluggish blood flows result in the brain working overhard to carry out tasks resulting in fatigue.
- This study gave ME/CFS patients and healthy controls two cognitive tests and assessed which parts of the brain reacted; i.e. which became more active. They wanted to see, if, as past studies have found, people with ME/CFS need to use more of their brains to complete the task – and to see if their brains adapted to the task.
- It turns out that when healthy people do the same task twice their brains use less energy the second time around – they’ve adapted to the task.
- The study found partial evidence that people with ME/CFS used more of their brains than healthy controls to complete the task. The major finding, though, was that their brains did not adapt – in what seemed to signal that postexertional malaise was present – their brains used more energy not less to complete the second task. Somehow doing the task the first time around had made things worse.
- The authors proposed an inadequate activation of a calcium signaling pathway that increases blood flows to distinct parts of the brain was present and noted that several Australian studies have found problems with calcium mobilization in TRPM3 ion channels in natural killer cells in ME/CFS.
- They didn’t mention it but the finding also appears to fit well with Wirth and Scheibenbogen’s hypothesis regarding calcium mobilization problems in the mitochondria and blood vessels. They believe that the inability of the Na+/K+-ATPase enzyme to remove sodium from ME/CFS cells causes the sodium-calcium exchanger (NCX) to import, rather than remove, calcium from the cells. The calcium buildup that results then impacts mitochondrial functioning and the blood vessels.
- Wirth and Lohn recently proposed that dysfunctional TRPM3 ion channels are wreaking havoc not just in immune cells but in cells across the body. They believe further investigations of this ion channel are “crucial” to understanding ME/CFS. (A blog is coming up.)
- The authors of the present study did not mention energy production. One wonders, though, if the exertion of the first cognitive test might have dampened energy production in the same way that physical exertion does.
- If the authors are correct then cognitive stress at least temporarily impairs the ability of the brain to speed resources (in the form of oxygen in the blood) to parts of the brain that need it – producing fatigue. (That sounds like postexertional malaise of the brain to me.) This group has been engaged in a large study (n=288 (!)) examining neurovascular coupling in ME/CFS from different angles.We should learn much more about that soon.
BOLD MRIs use blood oxygen levels to determine which parts of the brain are active. By having people with ME/CFS and healthy controls engage in a task, and comparing which parts of the brain get activated, researchers can determine if the different parts of the brain are getting activated (or not activated) in chronic fatigue syndrome (ME/CFS).

In what’s called “neurovascular coupling”, blood is sped to the active regions of the brain. Poor neurovascular coupling means fatigue and difficulty carrying out tasks.
Past brain imaging studies indicate that people with ME/CFS have to recruit more regions of the brain than normal to complete cognitive tasks. This suggests their brains are less efficient and require more energy to get cognitive tasks done.
The slowed processing speed cognitive tests have found in ME/CFS appears to make sense in this context; inefficient ME/CFS brains would naturally slow information processing speed down, making it more difficult to follow discussions, retain information while reading, etc. Interestingly, IQ levels don’t appear to be changed – it’s the ability to process information.
The Study
The Australian, Swiss, and US study, “Absence of BOLD adaptation in chronic fatigue syndrome revealed by task functional MRI“, examined which regions of the brain light up during an initial cognitive test. Then it went further by doing a post-exertional malaise-like assessment which brought to mind the 2-day exercise test.
They did a second cognitive test to determine whether the brains of people with ME/CFS had adapted properly to the first cognitive workout. It turns out that healthy people’s brains learn from a first cognitive test and become more efficient during the second: i.e. their brains use less energy (oxygen) the second time around.
Citing deficiencies in patient selection in past studies, the researchers buttoned up their study nicely by using ME/CFS patients who met the Canadian Consensus Criteria (CCC), and even using sedentary healthy controls matched for size, age, and sex (nice!). They even used actigraphy to ensure that the HCs were sedentary.
Several fatigue assessments (FSQ, parts of the DePaul Symptom Questionnaire) and depression/anxiety assessments were used to determine if the brain imaging results were correlated with fatigue and/or mood.
Thirty-four ME/CFS and 34 healthy controls were included. A “Symbol Digit Modalities Test” (SDMT) was used as a cognitive stressor. The SDMT assesses things like processing speed, attention, visual scanning, motor speed, and working memory. It’s often used to detect cognitive impairments and neurological dysfunctions in diseases like multiple sclerosis and traumatic brain injury.
Results
The idea that ME/CFS patients need to recruit broader regions of the brain during cognitive tasks was only partially confirmed. The within-group analysis found broader recruitment in the right dorsolateral prefrontal cortex and the left somatosensory cortex. The between-group analysis (the ME/CFS patients and the healthy controls) did not find significant differences in the number of brain regions recruited. The authors noted the high variability in the results – which is not unusual in ME/CFS – which would require larger studies to make sense of. They also questioned whether the cognitive test was difficult enough.
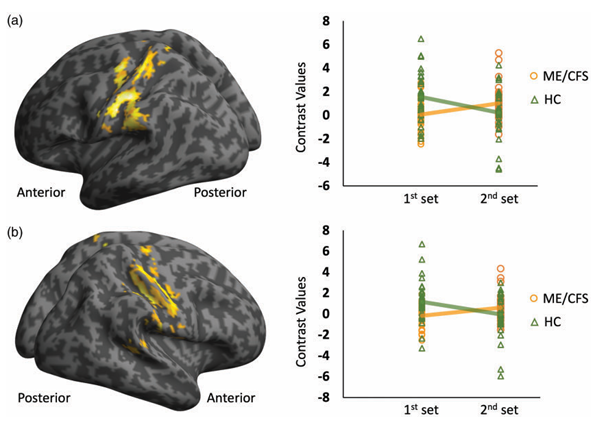
Increased activation in the ME/CFS patients (yellow line) vs the healthy controls (green line).
Adaptation was another and potentially more important story. Increased activation of the motor, sensory, and cognitive cortices in ME/CFS made sense given the movement, sensory, and cognitive problems found in the disease. The increased activity during the second test indicated that the ME/CFS brains did not adapt to the first cognitive test. Instead of becoming more efficient and using less energy during the second test, their brains used more energy during the second test. This is the same pattern found in multiple sclerosis and traumatic brain injury.
The authors highlighted problems with energy – not a lack of energy – but the strained energy resources and fatigue caused by the inefficient allocation of blood to the active brain regions.
“the lack of BOLD adaptation resulted in inefficient energy economics, which in turn led to the fatigue symptoms experienced by ME/CFS patients.”
Why was this happening?
The researcher believed that the “post-exertional malaise”, or fatigue, they found during the second test (they did not mention PEM) was caused by inadequate glutamate activation of a calcium signaling pathway that increases blood flows to distinct parts of the brain. They also mentioned “secondary metabolism-driven feedback”.
The glutamate pathway opens ion channels that allow calcium ions to flow into the neurons. The increased ion levels trigger the production of nitric oxide, which dilates the blood vessels, allowing more blood flow to the area. They believe the inability to get enough calcium into the neurons impeded their ability to deliver enough blood flows during the second test.
A calcium ion channel. The authors pegged problems with calcium mobilization as the most likely reason for the lack of adaptation shown.
The authors noted that this fits in well with studies from the Griffith group in Australia which found that damaged TRPM3 ion channels are inhibiting the calcium mobilization in natural killer cells in ME/CFS.
The finding also appears to fit well with Wirth and Scheibenbogen’s hypothesis regarding calcium mobilization problems in the mitochondria and blood vessels. They believe that the inability of the Na+/K+-ATPase enzyme to remove sodium from ME/CFS cells causes the sodium-calcium exchanger (NCX) to import, rather than remove, calcium from the cells. The calcium buildup that results then impacts mitochondrial functioning and the blood vessels.
Wirth and Lohn recently proposed that dysfunctional TRPM3 ion channels are wreaking havoc not just in immune cells but in cells across the body. They believe that further investigations of this ion channel are “crucial” to the understanding of ME/CFS. (A blog is coming up.)
The idea that problems with neurovascular coupling – the inability to quickly move blood to the areas of the brain that need it – are causing problems in ME/CFS is not new to the field. Altered cerebral blood flows were a main feature of Renz-Polster’s hypothesis that microglial/glial cell activation may be producing problems with neurovascular coupling (as well as reduced blood flows to the brain, raised intracranial pressure, and more).
The authors of the present study did not mention energy production. One wonders, though, if the exertion of the first cognitive test might have dampened energy production in the same way that physical exertion does.
More Coming
If the authors are correct then cognitive stress at least temporarily impairs the ability of the brain to speed resources (in the form of oxygen in the blood) to parts of the brain that need it – producing fatigue. (That sounds like postexertional malaise of the brain to me.) This group has been engaged in a large study (n=288 (!)) examining neurovascular coupling in ME/CFS from different angles. We should learn much more about that soon.






Very interesting, thank you. As you know, I have felt for a very long time that the core problems with ME/CFS lie in the brain.
Look forward to the findings of their other study
That is the really promising thing about this study for me – the 288 person study examining neurovascular coupling from three other angles including the glutamate idea they have. It makes me wonder how this big study happened.
What I don’t understand is that you’re lying down during an MRI. Normally you do not see reduced blood flow in ME/CFS patients. Well, if you sit or stand, orthostatic intolerance. Apparently if you carry out assignments while lying down during an MRI recording, they can see reduced blood flow to certain areas. But then you not only have reduced oxygen intake, but also of other substances.
If I take a high dose of calcium I will feel strange. I think more ME/CFS patients have this. How does this relate to the calcium ion problem?
How do you feel strange when you take a high dose of calcium? Can you elaborate?
Something good and bad but i can’t put it in words…..
I would love to know this as I need to take high levels of calcium for osteoporosis and I have M.E. and it makes me feel so ill I have had to stop taking it.
I guess if it was all about orthostatic intolerance, people with ME/CFS would feel okay after lying down for a certain period, but we know that isn’t the case. Although many feel less awful lying down, they still feel unwell. And PEM from mental effort can be induced by having a conversation or listening to an audiobook lying down.
This study, although about POTS, found that subjects’ cerebral blood flow dropped to the same extent when they a) stood up for five minutes and b) did a cognitive stress test while seated.
(The scientists couldn’t effectively measure blood flow when the subjects were lying flat due to the limitations of their equipment, so they had to do the cognitive test seated, even though it was not their preference.)
“Cerebral Blood Flow and Cognitive Performance in Postural Tachycardia Syndrome: Insights from Sustained Cognitive Stress Test”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7955388/
So maybe cognitive activity is a stressor on blood flow in the same way that orthostasis is.
I agree completely.I have had ME for almost 11 years,since 2013.I found 30 minutes trying to concentrate on a written text as physically exhausting as running for 30 minutes.I used to run and swim for pleasure for 30 minutes a couple of times a week prior to when I became too ill to work in 2013.Thank you to all researchers & all involved in Health Rising.
As everyone’s needs are different this may not be relevant to you but as the body only needs very small amounts of some nutrients,
I do not take extra calcium supplements (I take other supplements ,Q10,B-Complex,Fish oil,and Magnesium).One yoghurt a day seems to be slowly…I’m talking over almost 11 years with M.E….helping.It’s very much trial and error but I can relate so well to what you said you experience.Best of luck and thanks for posting.
On my screen The Gist stops before it gets to the results. Hope you can expand it; I can’t read the whole article. Thanks!
On my screen too. The bullet points under the box are the remaining gist.
Thanks – when the GIST formating goes out – it really goes out! Fixed.
same here
🙂 Fixed!
Much obliged for the fix (and for all your hard work!).
Sorry about that – the GIST went whacky! FIxed. 🙂
Incredibly exciting!!!! Thank you Cort!
I left a somewhat detailed response with a couple of questions and could not get it to go through. Rather an error message something about “reddit connection problem”? Whatever, I’m afraid I’m too tired at this point to go through the whole thing again.,
The question was about metamine (Nemanja).
So, Adderall (when I have it) lights up my brain & body. 10 mg & I’m a walking, talking, thinking machine!
Without it, I drag through life, bedbound, couchbound or at the very least sluggish.
But, after exerting energy while taking adderall my crashes are more profound.
Hoping for a cure that helps us rather than harms us.
Thanks Cort (for all you do). Brain Fatigue…yep, we know exactly what it feels like. Get some rest.
To Barbara: The Nemanda (I mispelled it as Nemanja) is for migraine prevention (off label use). It it also increases my energy, that would be nice, but I would still budget my activity and use of energy. Have learned by now tha tfor me, nothing overrides that.
Good luck.
Hi Cort,
I am an aerospace engineer working in a R&D environment at the very cutting edge of technology.
Your paragraph below totally reflects my reality. When tired (more then normally because I am always very tired), I can’t understand a text that I am reading without reading some sections 3 – 4 times, follow an intense discussion without asking to repeat or asking questions to evident things to make sure I understood well. I think very slowly, I search my words to speak, I forget name of colleagues and sometimes, I have the throat very dry and I loose my voice completely like if I had swallowed a full lion and not a cat. In other words, I have a very hard time to process any information all the time. Fortunately, I have a very ggod boss and good colleagues and I am still able to work because I have a very flexible schedule with reduced hours (between 3 to 4 days a week depending how I feel).
”The slowed processing speed cognitive tests have found in ME/CFS appears to make sense in this context; inefficient ME/CFS brains would naturally slow information processing speed down, making it more difficult to follow discussions, retain information while reading, etc. Interestingly, IQ levels don’t appear to be changed – it’s the ability to process” information.
@Canada – i have a similar background, similar position, similar symptoms. Are you me? 😀
Glad to see this work. Definitely feels lately like a lot of interesting info that ‘s waiting to be knitted together coherently.
No I am not you ! 😀 However, I find very interesting to know that I am not the only brave warrior surviving in this kind of extremely demanding environment. Never give up is my way of thinking but I absolutely needed to be able to adapt my schedule upon my needs, otherwise I would be dead by now. Hopefully, all hells will break loose in the research community and a little miracle will occur ASAP because I am so fed up to survive instead of to live (35 years now of this total crap and planning to retire in 5 years if able to last).
Exactly how I feel. I really struggle to follow recipes and enable myself to Cook. I cannot remember anything more than two seconds. Sometimes cannot get Brian organised to do any jobs at home. Following plots on tv almost impossible also remembering faces too hard so don’t know who speaker is talking about. I was always active physically and mentally, storing up jobs in brain and getting on to them. Now I’m useless except for 1-2 days/week. Everything is a huge effort.
I do all the same things as Helen. I walk around the house not knowing what it is I am looking for. Can’t remember names of people I know well. Lose track of words, sentences, I lose all my lists and to -do notes. Forgot my address, multiple phone numbers, everything in general. I get very irritable, like I am trying to live on the wrong planet. Put this together with chronic generalized pain, and I feel like checking out earlier rather than later. I confiscated my Poodle’s doggie tag and wear it myself, since I might not be able to find my way home when I get lost.
I am retired, thankfully, so I am facing similar processing difficulties but without the fear of messing up at work. The inefficiency of my CFSME brain is maddening. I am used to making swift sense of challenges & pre-CFSME I would never give up, but now I hit a brick wall trying to follow directions, remember names and nouns or understand simple sequences. I listen to intelligent young people in challenging jobs and recognize I no longer have a crisp, efficient, analytical brain.
Thank goodness the research focus is on processing glitches. And it repeatedly comes back to problems in the mitochondria. If I had a fortune I would throw it all into this area of research.
Thanks for all you do Cort. You bring us proof there is hope.
Effectively, the fear of messing up at work is always floating around. At least my boss is very understanding and bares with be (I have all the flexibility I need). Still able to work and sometimes to make a little breakthrough in my field but I ”no longer have a crisp, efficient, analytical brain” either. This is gone forever I guess. What I miss the most is sport. In my youth, I used to train hard on road bike and be an alpine ski instructor. When I am lucky, I can still bike and ski a bit alone at my own pace but I pay the heavy price on PEM for at least one full weak (when I do so, I absolutely need to plan a very small coming week or a week off to recuperate).
This is almost exactly what I experience. I am a science teacher and there are times when I cannot even focus on one child talking to me. I forget na.es all over the place.
I also have a fibromyalgia diagnosis.
Well that’s certainly what it feels like! Wonderful that they’re studying it. I do wish we got more studies of treatments though. Like, great, our brains aren’t working well, but what can we DO about it?
I think they will have some treatment suggestions – I don’t know how effective they but there are some things that can help with neurovascular coupling I believe. I think we should have a pretty good idea pretty soon how big a deal it is in ME/CFS.
This seems really relevant to me & my brain. Also from my lived experience, I can see that people may have more difficulties completing cognitive tests on the second day and not find the task easier.
I’m exasperated when I see ‘studies’ getting people with ME or Long Covid to participate in cognitive exercises. From my viewpoint that is just not going to work. I cannot build up mental stamina. My brain works best when I’m not exhausted & I’ve eaten the ‘right’ things & not the ‘wrong’ things.
Very interesting area of study for me.
Your comment intrigued me because I just enrolled in one such study out of Dartmouth called HOBSCOTCH. It involves 9 weeks of cognitive coaching for Long COVID patients with cognition issues. It’s a program they’ve had a lot of success with in epilepsy patients. They are now adapting it (separately) for LC patients and Parkinson’s patients. I had my intro session yesterday but the real work begins next week. I am wondering if it will improve my issues or further exhaust me, as you suggest it might. I guess we’ll find out!
Oh, interesting Amy. At least you’re aware of the issues. If I do too much my brain literally grinds to a halt. Like a boat running aground in shallow water. My issues seem to revolve around immune activation in my brain – microglia? Jarred Younger PhD territory & Michael VanElzakker PhD (poss vagus nerve/gut/brain) too. And simply running out of energy. And possibly low/slow blood flow.
Good luck!
Thank you! If I remember, I’ll come back with an update in a few weeks. Recently started following Younger on YouTube and relate to most everything he studies and posts.
Yes, Jarred Younger’s video series is great. I need to catch up with them.
Amy, That’s exciting. Please keep us posted on your progress.
Cort, So, I’ll try asking again. What about Nemanja (metamine)? My CFS doc has Rx’d is for patients as an alternative to Ritalin to increase energy. My neurologist has Rx’d it for preventing migraines. Both are off-label rx’s. It’s a medication for Alzheimer’s, not to reduce placque (sp?) but to prevent migraines (he found that as an unexpected side benefit).
Any comment from anyone??
Clarification: the medication is to reduce the symptoms of memory decline and cognitive fatigue from Alzheimers. Simply symptoms, no attempt to prevent plaque prformation. But off label uses for preventing migraines and increasing energy without having the cardiac bad effects of Ritulin by my neurologist and my CFS doc.
I would love feedback on this.
I think you mean Namenda/Memantine?
My neurologist also prescribed it for me after my stroke.
I’d like to hear if it’s good for CFS/ME, which I also suffer from.
Could be it — I just knew it as memantine, and then my cfs doc said the other name, which I’m sure is the one you mention.
I am always reluctant to take any medication without knowing others’ experience, especially on this site. So I haven’t taken it yet. My neurologist recommended 10 mg twice a day, starting with 10 mg at night. My CFS doc had very different advice: morning dose only, and only 5 mg.
Thanks so much for replying. I’m so sorry about your stroke and hope you are recovering well.
PS My CFS doc recommended it for increased energy and cognitive endurance. She said she had young and middle aged patients on it, as well as older patients. She said it was a good alternative to Ritalin, which has adverse cardiac effects. Apparently memantine does not. Online listed side effects include headaches but my neurologist (not my CfS doc) said he had in fact found that his patients on it reported that their migraines stopped.
I would love to know if other people on this site have any experience with it,
Your doctor is up on his/her literature 🙂 I think this is memantine (Axura, Akatinol, Namenda). A very small fibromyalgia trial found it improved cognition, depression, and global function and produced a non-significant trend toward reduced pain.
We have a page on it 🙂
https://www.healthrising.org/treating-chronic-fatigue-syndrome/drugs/memantine-axura-akatinol-in-fibromyalgia-and-chronic-fatigue-syndrome/
Thank you!!
I’ve been recommended it but havent started yet- for migraine. Just the regular hesitance.
Thanks for your response. You’re the first person who’s mentioned to me that they were rx’d it for migraine. My pharmacy and CFS doc hadn’t heard of that off label use. It is encouraging to know that someone besides my neurologist has found it useful for preventing migraine.
I have recently discovered that most of my CFS/ME symptoms were caused by low oxygen levels delivered to my tissues plus CO2 buildup in my blood while I slept. It tuns out that most people’s blood pressure dips by about 10-15% while sleeping. This is normal and gives the heart a rest. But there are outliers that dip by > 20% and are called extreme dippers by the medical world. Most people know that if your blood pressure drops too low, they will pass out. Very low blood pressure will not show as low oxygen saturation so will not show up on a sleep study. But the slow O2 delivery rate causes a low O2 perfusion into tissue and buildup in CO2 that is not being exhaled causing mild respiratory acidosis. The mitochondria make a large amount of ATP at night while sleeping so this can cause inadequate ATP to be created.
Since the FDA has elected to not clear any sleeping automatic blood pressure monitors, its very difficult to know if you are an extreme dipper. You cannot easily get one. I’ve seen probably seen 50 or more doctors where I mentioned sleep and not one thought about sleep blood pressure even though its should be obvious to anyone who studied physiology.
It turns out the body does this intentionally by lowering the baro-receptor threshold in the hypothalamus and then raising it again once awake. This is a very basic physiology problem which could be causing some CFS/ME problems for some people due to inadequate ATP and other side effects. Its somewhat like being on Mount Everest while sleeping and going back to low elevation upon awakening. After years of this, the body can adjust making it hard to come back. I just wanted to throw that out there since its hard to test for and even sleep doctors don’t think of it.
Maybe this explains why it takes my brain an hour every morning to come “online.”
Could be. People range from > 20% dip to a +rise and everything in between. 10-15% is the norm but how good your vascular system and capillaries are at absorbing O2 and releasing CO2, you could be on the margins. People who are marathon or Olympic class athletes do much better but regular people vary a lot. So how low your BP can go before you begin starving your body and brain is anybodies guess.
You could try the crude test I used. Since salt is sodium once dissolved and water follows sodium, taking a 500-1000mg salt tablet at bedtime and again if you awake mid morning like 2-3AM is a crude way of boosting your blood pressure just enough to tell any difference. If you notice no improvement, I doubt that’s the problem.
The other way is to try and buy an Omron Nightview blood pressure monitor on Ebay. It does 3 blood pressure measurements while you sleep. That should tell you roughly how much of a dipper you are after wearing it enough nights to get good data. If you see your blood pressure (not taking salt) drop down around 90ish/60ish, that’s not good and you should see a good cardiologist. It may be your problem.
Sounds like a lot of effort. My BP is normally 90/60.
That’s very interesting. How did you discover that?
I had thought for years that something was going on during my sleep that was causing all the other myriad of problems. But I was fooled by a combination of sleep studies and various doctors that if my O2 saturation was ok and no apnea, it wasn’t a sleep issue. That made me doubt given the sleep could be caused by something else. Eventually my heart rate began dropping when I fell asleep which I discovered with a recording pulse oximeter that also records heart rate.
It was obvious that when I fell asleep, my heart rate would drop from the 60’s and down about 1 BPM per second as I fell asleep. That caused such bad problems I ended up with a pacemaker. That clued me my suspicion about sleep was related to the autonomic system and possible blood pressure dropping ( also called dipping) because the autonomic system was also dropping innervation to the cardiac muscle and not just the SA node. The autonomic system is responsible for monitoring the baro-receptors ( blood pressure) and chemo-receptors ( CO2 and O2 to a lesser extent) and sending adrenaline to the heart muscle to pump harder. That in turn is a closed negative feedback system to regulate blood pressure during sleep.
So I wondered if given my innervation to my heart SA node for rate was going low, maybe the same was always true of the cardiac muscle contraction innervation. If you have very low blood pressure while awake, you will pass out from inadequate O2. If it happens while you sleep, a working autonomic system would direct blood to the brain and try and boost the pressure using the heart, kidneys and arteries constriction.
This seemed like an obvious sleep issue that would go undetected and had fooled me and doctors have no imagination. So I took some salt pills before bed to boost my blood pressure as the kidneys will see the increased sodium and water will be drawn to the blood increasing volume and therefore pressure. That’s why salt is not good for blood pressure. It worked. I awoke with no dramatic symptoms. Then I got the drug Fludrocortisone which does something similar and it worked also. I then got a night blood pressure monitor and can see how low it goes even on the Fludrocortisone. I dip about 25-30% which simply starves my body and brain of O2 and allows some CO2 to build up.
When you starve your entire body and brain of O2 every night, lots of bad things happen in your CNS, PNS, immune system, organs etc….
Thanks for the detailed answer. Extremely interesting!
The most interesting thing is blood pressure dipping is a well known and normal thing taught in medical school. But its a bell curve over the population. Some actually have a rise and not a dip, that’s bad. Others on the low end of the bell curve dip >20% and are classified as am extreme dipper phenotype. But as one ages and the cardiovascular health slowly deteriorates, extreme dippers are at risk for sleep hypo-tension. That’s bad. Studies have shown its not a small number of people. It looks like I’m and extreme extreme dipper but anyone in this category could be having night after night lack of O2. And its never even mentioned or investigated.
You cannot even get an overnight BP recorder in the US due to the FDA. Europe has them. I’m guessing but I bet some small proportion of ME/CFS people have this problem undetected yet so simple. Every doctor knows very low blood pressure will cause one to pass out but none think about sleep. Not even sleep specialists. You are on your own.
@Pgrovetom interesting. My BP is 96/40 my new doctor was very concerned about my low BP.
However, I had been to a Cardiologist & he said I have the heart of a 20 year old! Awww, (I’m 61).
It wasn’t until after I got home from my doctor appt that I realized how low my bp is.
I’m a “nose breather” at night, either nostril gets completely stuffed up (sinus disease) I sleep hard & wake exhausted.
I’ll have to look at results from sleep study a couple years ago & see if it mentions anything about BP. Thanks for your insight.
You might need a new cardiologist. That blood pressure is too low. Most people’s blood pressure dips by 10-15% while sleeping with some more. The dipping is caused by the sympathetic nervous system. So can low blood pressure as you have as can a congested nose. I had problems with nasal congestion also. As far as I know, most sleep studies including my 3 ( 2 at Stanford) did not monitor BP. If they had my problem would have been found. You should look into it.
Yes, Thank You,
I will definitely have some questions for my doctor at my next visit in September.
Thank you for posting this! There are so many factors that could be playing a role and since most Drs are clueless to start with (as you know-50 DRs, geez) it takes a lot or self research and luck to come across the right solution. I don’t remember seeing this info before so I hope it will help someone, myself included. You didn’t mention whether you found anything that helped but I pray you did!
Yes it worked 100%. All the morning and awakening horrible symptoms plus my IBS-C just plain stopped. Some nights even on the Fludrocortisone my BP drops to 99/67 and I feel not so great. But when the numbers recorded on my Omron BP recorder are in the >110/70 range, its a big difference. I had constipation and IBS symptoms for years and it just stopped. My bowels were not getting enough oxygen. Now I still feel fatigued and have some nervous system damage from years of low O2 but the sleep/night problems are nearly resolved. So its very real.
Don’t you need CO2 to push off. The oixtfeb from the red blood cell
No… The O2 leaves the red blood cells at the near end ( Arterial side ) of the capillaries due to partial pressure gradients and the CO2 enters on the venous side. Is a marvelous process.
From what I understand of the bohr effect, producing more CO2 improves oxygenation to tissues
Yes, once I realized it might be very low pressure while sleeping, I decided to take some salt tablets before falling asleep. Salt dissolves into sodium and chloride. The sodium goes into the blood and causes the kidneys to draw water into the blood increasing volume and therefore pressure. My symptoms stopped. Then I got my cardiologist to give me Flurdocortisone which works through the Aldosterone pathway doing essentially the same thing as the salt. It too worked. Even my constipation and nasal congestion stopped along with the more serious neurological problems. The only problem is after more than 10 years of starving my brain and body every night, my nervous system has some permanent damage. But at least I can sleep without awakening like I’m dying.
The part that blows my mind is I was looking down some pretty weird avenues for what was wrong. Finding out it was sleep hypotension and how that is very basic physiology made me even more angry at the myriad of doctors who are such idiots. Not one of 50 doctors including those from Stanford, UCSF, Mayo Clinic, John Hopkins and neurologists, cardiologists, sleep specialists etc… ever even thought of it. Trusting most doctors to even try to solve a weird problem that’s not in the cookbook is a fool’s errand.
Your info has started me down a new path, thank you! Most of us here know how clueless mainstream media is about a whole host of “issues”. Chronic Lyme (doesn’t exist even though their are pics of spirochetes in the brain), mast cell activation (top allergist in the State told me “we don’t believe that exists”!), ME/CFS, Spinal fluid leaks, intracranial hypo & hypertension, etc, etc. DRs look at you like you have two heads and they assume both of them have mental health issues! I’ve learned more on this this website, treatlyme.net and specific “issue” Facebook pages than any DR I have ever seen. My health is 75% better than 8 years ago, when a Dr refused to treat a tick bite that started this whole nasty cascade. Takes a whole bucket of supplements and restrictions and the 25% left may not be fixable but every little bit helps and I will definitely be checking my BP while sleeping since my heart rate can drop below 50bpm at night. Thanks again for posting!
I’ve been to Stanford, Mayo Clinic, UCSF and John Hopkins plus numerous local doctors. They are all stuck in a very narrow mindset and only willing to consider things on their “approved disorder” lists. They are not allowed to think or use any imagination. I’m a perfect example of where I didn’t try and convince them of chronic lyme ( even though I was treated) or something controversial. Every doctor and primary care obsesses over blood pressure and there are a dozen medications for high blood pressure. Every doctor knows low blood pressure causes problems and you will faint if it goes too low. Its rather obvious why.
You can buy 1 of a hundred blood pressure monitors on Amazon but not one that records during the night. But why? The FDA has seen fit to not allow it. That’s why I had to buy the Omron Nightview from Europe.
I suspected low blood pressure while asleep way back in 2016. I asked my primary care for a drug called Midadrine but was afraid to take it because I was nervous. But I did notice coffee before bedtime helped some. The problem is it wore off by early morning.
I don’t know if my autonomic nervous system sympathetic side is not working right or if I’m just a naturally super extreme dipper aging. Or it could be something like my adrenals when innervated by the SNS doesn’t release enough hormonal noradrenaline ( free in blood released by adrenal medulla) which lowers my baseline in my blood. When you add a lower hormonal noradrenaline to that released from the innervation of the heart, an extreme dipper might become a super extreme dipper.
I’ve read that the mechanism of dipping is the down adjustment of the baroreceptor ( blood pressure sensor in aorta) threshold during sleep. That’s why people have a blood pressure surge in the morning upon awakening as its reset to normal.
None of these unimaginative doctors even think about these things. They kept telling me to get a sleep study. That in turn showed nothing. I even asked the Stanford sleep doctor to be sure she monitored CO2 in 2022 but she forgot. Not only are they unimaginative but are sloppy.
I had to study physiology so I understood how the body and SNS regulate blood pressure and homeostasis in general just so I could figure out how my BP meds effect things and be sure it wasn’t my RAAS system. Once I realized salt was the most straightforward way to raise blood pressure while sleeping, I nailed it.
I even told this story to the president of Stanford Medicine, David Entwistle and all but blew me off. Probably afraid of a lawsuit for incompetence. Its sad!
I really appreciate all your info and the time it took to write all of this! I googled Omron Nightview and the reviews on TrustPilot are poor. It also looks like there may be knockoff issues or ?? with a couple similar websites. BestBuy is selling a different model with different name but same description from a quick look. I haven’t had a chance to delve deeper. I noticed the Nightview was being sold for hypertention. I wonder how the accuracy is for hypotention? Need to look that up too.
Since it was the only cuff based product available, I just ordered it via Ebay Europe. FDA has yet to clear on for the US. Once I got it, I checked it against my regular upper arm cuff unit I’ve used for years. For normal 120/80 or high 170/105, the Omron and my old one were pretty close. I checked it a dozen times and they were close enough it was better than nothing. I also ordered the AKTiiA, also from Europe but it uses a technique based on the delays of the ECG heart conduction and pressure pulse through the arteries and can measure on the wrist. Since I have a Pacemaker, I discovered the hard way that the electronic method doesn’t work because my pacemaker creates its own different ECG waveform.
In any case, the Omron measurements are also consistent with symptoms which I feel is the bottom line versus absolute accuracy. If my old cuff monitor was good enough for years, the Oron looks fine.
Thanks! The AKTiiA is launching in the US in 2025. I think I’ll wait for that model although I found the official website for the Omron. People are questioning where Best Buy is getting the version it sells. They may be getting scammed too. Glad you found something that helped!
In my searching, AKTiiA was my first choice. But not only do you need someone in Europe to order it for you, you need a VPN and fake European email to download its phone app or Google Store blocks it. I suspect AKTiiA is very sensitive as they are trying to get FDA clearance so are making it very difficult to cheat.
It uses the electronic ECG and pressure wave pulse delay technique which makes it unusable for anyone with a pacemaker. If you were to get one from say a friend in Europe, then use a fake email, download its app, it needs to be calibrated once as part of setup against a regular cuff BP monitor.
I suspect this is because everyone’s delay is a bit different and it needs to calibrate for your delay at least once. Then it can infer your BP from the calibrated delay.
Its very crazy one can buy a Chinese cuff monitor that is off by a mile and yet the FDA hasn’t seen fit to approve an Omron like device. I wish the Omron device was more programmable. It does a measurement at 2AM, 4AM and 4 hours after you push the night start button. I wish it had an hourly mode and certain hours could be excluded.
The Omron app does allow you to do daytime measurements plus the night and then graphs them on a nice plot. So for example, I can see when I’m asleep at 2AM and see say 105/65 and then I awake and its 135/85 at 2:30AM . Plus I can do a 9PM manual measurement and use it versus the lowest sleep BP to estimate my dipping percentage. I’ve seen numbers that range from about 25% to 35% even while taking the Fludrocortisone.
So long as you don’t have a pacemaker, the AKTiiA with its watch like wrist mount will probably be a big hit if its accuracy is ok. It sorta crazy because primary care doctors tend to obsess over BP measured in their office when you are nervous and give meds based on that. If they had full 24 hr data from either the AKTiiA or the Omron, it would mean so much more plus be able to characterize you as to your dipping phenotype. That number is very important because heart and artery disease is more a function of average BP rather than peak. Too high a peak can cause a stroke or white matter ischemic problems but for BP meds, a daily average would be very good to know.
My opinion is everyone with a mystery disease like CFS/ME should make sure their sleep BP is reasonable before pursuing the more wild strategies. It could be that 5% of CFS/ME people have an undetected hypo-tension while sleeping and have no way of knowing. They should also buy a <$100 overnight recording pulse-oximeter just to be sure their BP, O2 sat and heart rate all look reasonable. Its almost a no brainer.
I have an Apple watch that measures heart rate and O2 Sat. Both drop low at night as I have bradycardia and mild sleep apnea. I basically try to go into hibernation at night. 😉 I hope AKTiia does roll out in the US next year. In the meantime I’ll save my money and keep my salt levels up.
Its true but the biochemical process is a bit complicated. The CO2 causes the blood in the capillaries to become more acidic. That in turn reduces the hemoglobin affinity of oxygen making it disassociate more easily thereby releasing more O2 via perfusion.
A very straightforward explanation of the high level process of how O2 and Glucose are perfused into tissue via positive partial pressure differences and CO2 and waste is released due a reversed negative pressure gradient on the venous end but without the Bohr or more subtle biochemical adaption processes at the capillaries is here:
https://www.youtube.com/watch?v=GnriknE4YRY&t=11s
The more detailed adaptive process including the Bohr effect are described in great detail here:
https://www.ncbi.nlm.nih.gov/books/NBK526028/
The reason carbon monoxide is so deadly is it actually does the reverse of CO2 and increases the hemoglobin affinity thereby preventing O2 from leaving the hemoglobin starving one of O2.
This is interesting because I’ve read that many people with POTS (what I had first before suspected ME/CFS) are found to be non-dippers while they sleep, which is the opposite. My sleep has been unrefreshing for many years.
Regarding sleep monitors, I am hoping one day that the Lumia (formerly Stat) device will be able to measure blood pressure during sleep to help shine some light on this question. The company said that they have received a grant for tracking sleep parameters and for measuring absolute blood pressure, so it might be possible!A
Ooh, good point. I believe the first iteration of the device offers a blood pressure trend, not exact numbers. A trend of overnight data would be useful.
I can’t wait for it to get to Australia.
If anyone reading in the US is interested, the company is offering a financial assistance program. Applications open till 24 August 2024. (Future rounds of applications planned too.)
Because in 2021, it was found my heart rate was grossly dropping only when sleeping I got a pacemaker. It turns out most non cuff based BP monitors use a time delay of the pressure pulse using the electrical heart signal as a reference. Turns out my pacemaker causes this technique to fail because its on all night overwhelming my hearts normal ECG signal.
But the Omron Nightview does 3 measurements which is just about good enough. Even on the Fludrocortisone I’ve seen dips of >30% wake -> sleep and numbers as low as 105/58. That’s pretty low given I’m on a drug that is supposed to raise my BP.
For years, it’s been my BRAIN that crashes after physical or mental exertion, not so much my body. Often my brain tanks dramatically. Vision dims, can’t coordinate body movements, can’t think.
Doctors have never been able to seem to fathom it.
That certainly fits with the “slower not dumber” experience. It also might explain a bit of the paradox where in depth conversations from the long term memory (e.g. about your job, if you can still keep one down) don’t seem as demanding as free ranging small talk in a busy room.
Quite an interesting presentation fromnRon Davis at Invest in ME:
https://m.youtube.com/watch?v=ijkCw7VeOLo
Very impressed by these Precision Life people! Had never heard of them. Have some renewed hope after watching a few of these Invest in ME presentations!
https://m.youtube.com/watch?v=CS1Jr5kEOKY&pp=QAFIAg%3D%3D
I earned a PhD (Clinical Counselor/Psychotherapist) at age 58; loved my studies; could concentrate for hours. I was diagnosed with ME/CFS around age 62. However, I was experiencing increased fatigue over the years. About age 68, I started feeling fatigued more often, and concentration abilities were decreasing. Now, as of today, I can concentrate for about 20 minutes on complicated things and about 2 hours on easy things – like just watching tv. At present, my husband and I are planning a move to another state next month. With all the details, I can only concentrate about 1/2 hour before I feel drained and need to rest. New things that require new ideas and new answers are a pressure for me. I personally feel that mental concentrate causes my fatigue besides physical activities. I want to add that over the years I need to sleep longer each night and take naps during the day.
Dear Patricia (or Dr Schafer if you prefer); My slowly progressive mental struggles mirror yours (and those of numerous others in this thread). I have had CFS/Fibro for 39 years. About 30 years ago, I went for psychological testing – as it was clear to me that my cognitive processing speed had slowed down. After the testing I was (dismissively) told that my cognitive function and speed were just fine. I responded that my concern wasn’t that these capacities were deficient compared to average, but that they had noticeably declined (and were continuing to decline). However, their tests did not measure that. So, I went back 5 years later and requested the same testing – which demonstrated a clear and significant decline. I had hoped that the next step would be to investigate the cause to nip it in the bud ASAP. Of course, that did not happen. Now the problem has progressed to the degree that I struggle to follow a TV show plot, or to remember details for even a minute or two. I can relate to many of the debilitating mental problems conveyed by others commenting above.
I consider it very feasible that (as this research suggests) blood flows to the brain (and perhaps elsewhere?) could be deranged, and causing or contributing to many of our symptoms. Sometimes, when I stand up, I can hear the blood gushing thru the veins or arteries near my ear drums (whoosh … whoosh … whoosh – with every heartbeat – for a minute or two). This seems to indicate that “something” is affecting the blood flows in my head (and brain?) – but only sometimes. The “whooshing” periods also correlate to more sensitive eyes, hearing and migraine like headaches.
If I recall correctly, blood flow problems (and impaired oxygen delivery/utilization) to the body and muscles have been suspected and even demonstrated in CFS/Fibro patients by other researchers. This includes microvascular deficiencies which may cause small nerve fibre neuropathy (that may in turn cause numbness, sensitivity or pain). If these same (blood flow) problems are occurring in the brain – and affecting neurons (rather than nerves in the body), it could explain a lot. Thus, I hope this research is followed up to either conclusively confirm or dismiss such (promising) blood flow problems.
TY again Cort … for your usual priceless medical journalism.
OK, WE REALLY NEED A LIKE BUTTON on this platform.
I can empathize with you. I was extremely lucky, when I needed to sell a family home filled with 50 years of furniture and papers/photos, etc., to have a kind neighbor who volunteered to “help me pack”. She did far more than just help me pack. She took a systems analysis approach (remember that, back in the 1970s?) and sketched out a calendar from the house sale date (contract already signed) to the closing date.
She scheduled in rest days, due to my CFS, and asked questions like “What kind of help would you need to get that done? How can you identify whom to do it?” which she had an extra column for in her grid.
It was incredibly helpful. I will never forget it and always thank her. I’d like someone like Nancy now, but we’re far apart now geographically and out of touch since her divorce.
It is perfectly legit for a person with CFS who formerly would have been able to do all of this herself and easily to seek to find help from an “organizer” to help them do it now..
I wish you the best of luck.
Guess what drug can restore TRPM3 function? LDN
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6834647/
Good find! I had it on my list to look up. And when you wrote this I thought it sounded familiar, guess my brain isn’t totally dead. 😉 Here’s some info from Cort in 2021 on LDN that includes TRPM3. https://www.healthrising.org/blog/2021/09/07/ldn-low-dose-naltrexone-chronic-fatigue-syndrome-natural-killer-cell/
https://academic.oup.com/braincomms/article/6/2/fcae080/7623634
Re treatments: a quick Google search on Neurovascular coupling/dysfunction came up with this article. It looks too complex for me to read right now but there is a nice diagram with suggested treatments…
Very interesting topic. I thought I should let you know that the gist narration is missing the second half. Thank you so much for narrating, it helps my cognition a lot!
I still think TRPA1 is affected in the ME disease mechanism: “Brain endothelial cell TRPA1 channels initiate neurovascular coupling” https://pubmed.ncbi.nlm.nih.gov/33635784/
A role for TRPs in ME/CFS/POTS/MCS/pain/endothelial dysfunction…?
https://followmeindenmark.blogspot.com/2014/02/a-role-for-trps-in-mecfspotsmcspainendo.html
Are ME and MCS disease mechanisms linked through TRP ion channel dysfunction and ER stress?
https://followmeindenmark.blogspot.com/2023/08/are-me-and-mcs-disease-mechanisms.html
Is there any way I could be a part of future studies? I’ve been suffering with this illness for 38 years. Please consider me for future testing.
Search clinicaltrials.gov for me/cfs every so often, and some study might come up which is recruiting in your area.
Regarding the following in the above article: “They believe that the inability of the Na+/K+-ATPase enzyme to remove sodium from ME/CFS cells causes the sodium-calcium exchanger (NCX) to import, rather than remove, calcium from the cells.”…. I avoid pharmaceuticals at all costs because they all have side effects and because I’m hypersensitive to chemicals and many foods. With my body as my “experimental lab,” I discovered many years ago that sodium in my diet causes brain fog, shortness of breath, extreme fatigue, vertigo, lightheadedness on standing, etc. I experimented with an extremely low sodium diet which eradicated the worst symptoms. I know of no one who has tried my extreme diet but I have always wondered how many of you out there might have the same inability to process and utilize sodium. When I tell people about this, they say things like they never add salt to their food, which shows an extreme lack of understanding about the sodium content of all animal products and all processed foods. Sodium occurs naturally in many vegetables (e.g. spinach) to which I am symptomatic, so I had to do a sodium count to be sure to eat the right grains, seeds, nuts, fruits and vegetables. My sodium intake is less than 800 mg per day, often less in winter when I don’t perspire out the salts. It has made the difference between being able to get out of bed to function normally or being bed-bound, so I am wondering if any of you have ever considered this. The downside for me, especially in summer, is how to maintain bodily fluids when sodium and chloride levels are low. It can be dangerous to drop too low, so blood tests are important. On a recent blood test my thyroid numbers had increased so I asked my doctor to test for iodine levels due to my low-sodium diet, which showed a deficiency. She told me to add a couple of teaspoons of salt to my diet which would have put me back in bed so instead I went to the health food store and bought an oral iodine supplement of 150 mcg. I’ve yet to be retested, and am still dealing with the tricky-ness of maintaining a healthy, safe summer electrolyte balance. At least during summer I can eat a small amount of tilapia that has 50 mg sodium per serving. Winter, however, is a totally different issue. The diet is boring and restrictive but for me the alternative is being totally incapacitated. Anyone else noticing sodium sensitivity?
For 20 years, I took fludrocortisone, four buffered salt tablets, and a ton of water to boost my blood volume. I felt quite a bit better, physically and mentally. But that didn’t last. Things flipped, and now I’m sensitive to salt in bread and any prepared foods etc…. If I have a salty dinner, the next morning, my head pounds with pressure. And every now and then, the salt I eat gets into my tear ducts. And when my eyes tear up, they feel as if they are being burned by the salt and I have to flush my eyes with cold water.
I’m not as affected as you, and marvel at your discipline. I wish you the best of luck.
Wow, Neal…same symptoms here. Pounding head from salt, plus eyes burning and runny if I eat even the slightest added sodium. I also get vertigo and balance problems as if fluid has build up in my head, which it likely has because that’s what causes vertigo. I can’t help but think there’s a connection to CFS/ME. Does this sensitivity to salt run in your family?
Have you ever heard of FD/Familial Dysautonomia? It primarily affects people of Askenazi Jewish or Eastern Europe ancestry.
I found that 3000 mg ALCAR on empty stumac improves brainenergy. Benefitting greatly. Also reduses my PEM. Results may vary but wanted to share.
I am contemplating the descriptions of low blood oxygen while sleeping and issues with brain processing reported by these last few commenters. For myself I had a sleep study where my HR went down to 36 bpm where as normally while awake it is 85-105 bpm. Apparently I have a highly labile blood pressure and heart rate and appear hypertensive at the doctors and low normal when not under stress. It appears to bounce wildly throughout the day.
I also notice I have a brain with similar traits. Some days I can think clearly, swiftly and have no trouble with understanding complex articles. Yet other days, in fact sometimes it is a matter of hours, I can barely follow a sentence. This follows a loose pattern.
And then there are word finding issues. I am trying to express myself and know the concept but the correct word seems to be at the bottom of a well and if I wait long enough, it floats to the top of my mind. Unfortunately while in conversation, this can take too long and is especially disconcerting when conversing with doctors as I suspect I appear dumb (which I am not!). Again this problem seems to come and go.
In a broader scope, while navigating the days, on a rare day, I have super energy, and then I go back to struggling to get through my tasks. These ‘super days’ seem to happen about once a month. My normal struggle with fatigue is also influenced with my circadian rhythms (peak in the am, low mid day, small bump late evening). And then there is PEM if I have over done it the preceding day(s).
I’m sure all of you reading this are not so interested in my bodily cycles, but why I am relating this is because there seem to be cycles within cycles which have enough regularity as to be potentially useful in understanding ME/CFS. Not sure how to accomplish this, but some kind of study tracking these markers over time in a large group of sufferers could possibly be useful. There is something interesting with their repetitive nature and I do wonder if they could be compared with other ‘unrelated’ bodily cycles to find unsuspected correlations.
Hi Nancy,
I haven’t heard anyone describe the word-finding issues like that before, but it’s exactly how mine are too. If I push to find the word, I either can’t, or it uses noticeably more energy. But if I give my brain time and rest/move on to something else (non-demanding) then the word will often rise to the surface. This can happen with memories as well, but it’s less reliable that they’ll come back.
I wonder if this is how most people experience it? Maybe it’s just not something that is described in more detail than ‘word-finding problems’ in general.
I also have the word-finding difficulties, and they have gotten worse over time. I too will find myself at a loss for a word in conversation- and if I wait a few seconds sometimes it appears, sometimes not til a few minutes or more later. As a work around I will describe what I am speaking about or substitute a word or phrase to not only communicate to someone else but also to give me a clue for the word. The medical term used technically is ‘aphasia’ and we typically hear that used with stroke victims. It covers word finding (almost diagnostic for covid vacc cognitive injury), but also word understanding, reading or writing words. Some of us have these, I do not, and generally not common.
Thanks James, for some reason it hadn’t occurred to me there might be a term to describe this!
There is something wrong with your autonomic system if your sleep BP is 36 and daytime hits 100 for no reason. First you need a pacemaker to keep your sleep BP at 60. 36BPM will starve your body and brain of O2 unless you are a marathon runner. When mine hit about 45BPM as I was falling asleep, my whole body hurt and I began feeling very ill. If I got up just before falling fully asleep, my BP would return to above 60 immediately and all the symptoms would stop within a minute. I got a pacemaker and its not all that bad. It makes MRI’s a pain but my heart never goes below 60. And if I had AFIB, it might save me. Mu opinion, see a cardiologist and fix that first. Then see if that corrects the other issues.
@Pgrovetom,
First, thank you for your concern. I only mention that I had a low of 36bpm–not continuous. And with Ehlers-Danlos, I have seen cardiologists a plenty! Yes, I know I have dysautonomia and have had this frequent (but not completely) continuous high waking heart rate my entire life. Things like beta blockers would not work for me because of the wide range of variability. They could cause my lows to be too low. No cardiologist has even given a whisper about a pacemaker and besides, with the fragile tissues of EDS, such a procedure would be very risky. I’m a bleeder and don’t heal very well either. No A-fib, so as far as I’m concerned, I’m good to go. I’ve made it this far–just turned 72!
I just want to convey how much I appreciate all the comments and reports of readers after Cort’s summaries of research. Very often – I find myself thinking “Me too!” when I read, and sometimes the experiences of others helps me to understand and express my own symptoms better. I think that we stand to learn a lot of valuable information – from each other! TY to all who share. 🙂
I agree! Thanks to everyone who posts!
I really love your articles. They are extremely informative. I only wish instead of all the studies that are being conducted that they find treatment for PEM. I definitely need some kind of drug to treat PEM and brain fog from Covid.
Once again, not exactly on topic, and pardon me if this has been mentioned before, but here is a study which claims a test with over 90% accuracy for diagnosing ME/CFS.
https://onlinelibrary.wiley.com/doi/10.1002/advs.202302146
Not exactly ready for prime time, but apparently it’s out there.
Have you seen “Submaximal Exercise Provokes Increased Activation of the Anterior Default Mode Network During the Resting State as a Biomarker of Postexertional Malaise in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome” which found increased BOLD markers after physical exertion?
It would be interesting to tessellate this reasearch with this research:
“Cerebral Blood Flow and Cognitive Performance in Postural Tachycardia Syndrome: Insights from Sustained Cognitive Stress Test”
https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/33280488/
For example, how do the oxygen issues in the study described in Cort’s article relate to the blood flow issues found in this POTS study. Could we do the same study on fibromyalgia, ME/CFS and orthostatic intolerance patient groups and learn what unites or divides them in this aspect?
And do people with brain fog (but not necessarily any other condition) also have this problem?
Anyway, great stuff!
Thank you for the write-up, Cort.
Why wouldn’t it be the brain….it’s where viruses enter the nose and upward toward the brain.
The inside of my nose is a mess
The harder we think, the less we can. Dr. Naviaux’s research makes sense here.
Things that really help me
RAISE THE TOP OF YOU RBED 6-8 inches
HUGE Difference in quality of sleep and I lie down during the dsy to do cog tasks but feel refreshed having hesar raised
I suffer very severe migraines…me/CFS has been linked very strongly to ‘migraine brains..latest research shows malfunction in sodium potassium channel in brain and /ot calcium ion channel and migraines..so this latest research is NO surprise..
I do much better on a low potassium diet and high sodium/water diet..and calcium supplements and I believe LDN that I am on also affects calcium channel in a positive way
CFS/ME has been called one long extended Complex migraine FWIW thx for posting
Ha! We did a blog on that about ten years ago. One study found that a 30% tilt is the most optimal for humans.
https://www.healthrising.org/blog/2013/06/16/heads-up-are-you-missing-an-easy-way-to-improve-sleep-and-health/
Thanks for the refresher 🙂
Hey Cort
Thx for your response and all you do!
Ya I’m a long timer
Got ME/CFScat 19 in my prime
Struggled 29 years with it
Cost me 325000
In treatments
But still hanging in
Take care!
Tons of trial and error lol
Thanks! We are both long timers! Hang in there buddy!
Interesting as my blood rate is below 60, usually around 44. Also I have calcium deposits around my knees and extra bone deformities in my ankles.
I also have calcium intolerance and my son is allergic to dairy. I do not know if he has ME but I do.
If I do physical exercise then the next few days I am exhausted. My feet go numb and swell.
Hey Cort, I tried to listen to the audio of The Gist but it cuts off after only a minute. Is something missing?
Thank you so much for all the work you have done over all these years and thank you to Geoff for his wonderful narration!
Sorry about that Rachel – I don’t know what happened 🙁
Omgggg….. it describes exactly what happened to me and what I’m going through. My brain is so messed up. I can’t remember anything. I can’t follow instructions that are more than one thing at a time. I used to hold down two jobs and take care of a daughter and, three dogs at one time. My physical body is not fatigued. My brain is totally off the rails. I see my handicap so clearly it’s so frustrating. I’m not surviving in this world with these issues. I used to run my business now I can’t keep track of anything and can’t make decisions , and can’t understand the consequences of decisions. My life is falling apart, and I have no help. I am willing to participate in a study… If I can remember where I have to be, and when.. i’m struggling. I have no family.
I am thinking ..not all ME/CFS patient has the illness for the same reason..How can the outcome of a test then be the same.
The difference in how severe and different the illness acts..should also tell that it dos not effect the brain the same way for all..Should it not ?
Thanks for sharing the research. My own experience would echo it. I am left wondering however what if anything does this mean for treatment? Is there anything I can so, or eat for example which might help with this?
Re:Calcium …I have some background knowledge in food science and after 10+ years of being too weak and faint to cook,I am for now at least, grateful to be able to cook once or twice a week.The point I want to highlight though is the fact that the one food I always make sure to put on my grocery list ,without fail,is youghurt.I wonder is it related to my body responding to the need for it.I can no longer drink milk which I loved..but if I could only have one food in the fridge, it would be yoghurt.I know everyone’s needs are different ..just saying.Thank you to all hard grafting researchers chipping away at the Medical Mount Everest of M.E.Research.You are our Champions.I am so grateful to you all and all at Health Rising. Hope is everything.
Thank you Cort! Finding information on this debilitating illness gives me hope. You are an awesome human.
🙂
Cort,
Did the study say if on the repeat test, the ME patients demonstrated impaired performance? Longer times, decreased scoring? This could be crucial for all these folks that are slogging their way thru the SSDI application process now.
Hi Carol,
Unfortunately they did not report cognitive scores 🙁
Thanks for responding Cort. I didn’t think so, just checking that I didn’t miss it. If you are aware of any work that has touched in that direction I would love to know. The only one I am aware of is Bateman Horne’s paper when they did a cognitive test pre and post the NASA Lean test : https://www.frontiersin.org/articles/10.3389/fmed.2022.917019/full
https://batemanhornecenter.org/why-the-10-minute-nasa-lean-test/
Very interesting
Question
Thing that helped me most mess 3 iron IV’s
My ferritin was 90 low forca man 100! Is marker not woman there’s is lower
I had incredible improvement instantly from sble to drive 15 minutes to drive -2 hrs to snother province to visit brother and completely confident benift lasted 8 months til I needed AGSIN and get it once a year my ferritin falls cuz of an unrelated condition a artificial heart value
Anyway I always felt it helped more than it should even though we know iron is vital it took away my CFS completely
I’m a math guy not biology iron is an OXYGEN transporter could this study point to reason why it helped so much maybe some one with more biology could answer? I’m a lifer 38+!uears ehole adult life spent 380,000 to stay mot house bound but only basics Srnding blesdings Dan