Geoff’s Narrations
The GIST
The Blog

Solve ME’s Ramsay program has a nice return on investment.
That was pretty quick! Health Rising reported on Heather Edgell’s Ramsay Award from the Solve M.E. Initiative in Aug 2022 and now she’s not only finished the study but has already published a paper, “Inspiratory muscle training improves autonomic function in myalgic encephalomyelitis/chronic fatigue syndrome and post-acute sequelae of SARS-CoV-2: A pilot study“, on it.
Moving quickly is one of the many advantages of supporting ME/CFS research foundations like Solve M.E., the Open Medicine Foundation, and ME Research UK. Applicants don’t have to suffer from extended grant application reviews from reviewers who don’t know the field – and may not even be sympathetic to it (like we sometimes see at the NIH). Look at what just happened at the NIH – somehow we lost an ME/CFS research center because the reviewers nixed it.
The GIST
- This blog is about a study and a critical part of ME/CFS and long COVID research – supporting our non-profits. Unlike organizations like the NIH non-profits like Solve ME, Open Medicine Foundation, ME Research UK, Polybio, and the Patient Lead Research Group review grant applications use only experts in the field, get their grants out quickly, tap into the latest research findings, take chances on high-risk, high-reward projects, and engage researchers new to the field.
- That kind of expertise and commitment results in a nice return on investment (ROI). Supporting the non-profits is a win-win for everyone.
- Two grants from Solve ME’s Ramsay program illustrate why. Heather Edgell inspiratory breathing grant brought in a new investigator and new treatment option to ME/CFS and long COVID.
- Three times a week, participants breathed through a device that restricted their breathing by a small amount in order to build up the muscles that move the lungs. (Those muscles can decay when we are bedbound). Heather Edgell said it was like breathing through a straw.
- The study found that the inspiratory training improved autonomic functioning in ME/CFS (vasomotor, secretomotor, weighted score), improved sleep, reduced resting heart rate (more rest and digest), maximal inspiratory pressure (stronger lung muscles), and even the distance the participants covered in the 6-minute walk test in both ME/CFS and long COVID. Interestingly, the ME/CFS patients started worse and improved more.
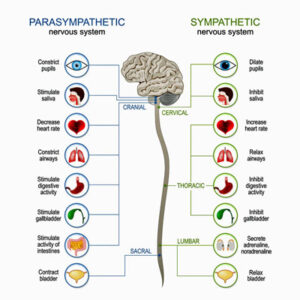
- The authors believed the improvements were due to improved parasympathetic activity (vagal tone). Encouragingly, the type of device Edgell used is readily available, not expensive, is safe, and can be used at home. (Check out the blog for ideas).
- Dr. Duricka’s Ramsay Award explored the effectiveness of another new treatment option. Stellate ganglion block consists of injecting an anesthetic into the stellate ganglion nerves near the voice box that regulate autonomic nervous system functioning.
- Duricka recently reported that the block was able to relieve pain, regulate sympathetic nervous system activity, improve sleep, increase cognition, and improve neurological function. Even the big hard-to-move symptom- post-exertional malaise – quickly improved. With one in three long-COVID patients still experiencing relief a month later, the shots had some legs.
- Since her Ramsay Award, Heather Edgell has won over half a million dollars in other grants to bolster her Ramsay Grant findings. She’s not alone. Solve M.E. reported that from 2016-2023, it funded $1.3 million in 37 infection-associated chronic illnesses studies through its Ramsay Research Grant Program. Over time, those grant recipients subsequently won over $27 million in funding. Many times all a researcher needs is a start, and that’s what the non-profits provide.
- Coming up – a look at a recent Open Medicine Foundation-funded ME/CFS study, and several talks with Benjamin Natelson on his new studies, the unique breathing problems he’s found in ME/CFS, and his new attempt to reset the autonomic nervous system using vagus nerve stimulation.
That kind of expertise and commitment results in a nice return on investment (ROI). Supporting the non-profits is a win-win for everyone.
Heather Edgell’s Ramsay Award

Heather Edgell is an example of what non-profits do best – bring in creative researchers who are new to the field.
Heather Edgell’s Ramsay award from Solve M.E. to do an inspiratory breathing study is a case in point. Edgell, from York University in Toronto, has never worked in the ME/CFS/long-COVID field and no inspiratory trials have ever been done. With ME/CFS studies demonstrating that breathing is altered during exercise and during standing, and with clinicians such as David Putrino using breathing techniques in long COVID and ME/CFS, it was clearly time for a breathing trial.
This trial, though, wasn’t just about improving symptoms. Like other non-profits (Open Medicine Foundation, PolyBio Foundation), Solve M.E. used this trial to dig into the patients’ physiology and learn more about the disease.
The Trial
The trial was small (long COVID – 9; ME/CFS – 12, healthy controls -12) – and it was supposed to be small. Organizations like Solve M.E. fund as many small pilot trials as they can to give as many researchers as possible the data to apply for larger studies from the NIH or private foundations.
The trial used mild to moderate patients; i.e. it avoided those who were house or bedbound.
Edgell found that a simple breathing device was able to help reset the autonomic nervous system.
The trial was hormetic in nature; i.e. in its attempt to retrain the autonomic nervous system and breathe more healthily, it used a small stressor to build up the muscles that move the lungs. (Lying in bed for long periods can weaken those muscles). Three times a week, participants breathed through a device that restricted their breathing a small amount.
Each session consisted of 6 sets of 6 repetitions (total of 108 breaths/week) with the goal of progressively reducing the rest time between sets from 60 s for the first 2 weeks to 10 s for the last week. (If I got it right they would take 6 breaths through the device, wait for a minute, then do six more breathes for a total of 36 breathes per session. Over time they would reduce the rest period to 10 secs.) Edgell said it feels as if you were breathing through a straw.
Various autonomic nervous system assessments were taken. Before the trial, the ME/CFS group exhibited worsened symptoms of orthostatic intolerance, vascular function, secretomotor function (fluid secretion), and gastrointestinal function than the healthy controls. They also exhibited more reduced vasomotor functioning (regulation of blood vessel diameter) than the long-COVID group. Both ME/CFS and the long-COVID groups displayed reduced HRV.
Edgell found the inspiratory training improved autonomic functioning in ME/CFS (vasomotor, secretomotor, weighted score), improved sleep symptoms in all the groups, and improved pain in ME/CFS. It also improved heart rate variability (a sign of parasympathetic nervous system (rest and digest) functioning), resting heart rate (more rest and digest), maximal inspiratory pressure (stronger lung muscles), and even the distance the participants covered in the 6-minute walk test.
The ME/CFS group was worse off at the beginning of the study, but gained more – showing greater improvements in vascular function, secretomotor function, the total weighted score of the COMPASS 31 autonomic questionnaire, and symptoms related to pain.
The improved sleep was a nice bonus but maybe not an unexpected one. These breathing exercises improved parasympathetic nervous system (rest and digest) functioning and studies have linked poor sleep in ME/CFS to reduced parasympathetic nervous system functioning.
This study was not about being cured – it was about finding something that could help relieve some symptoms. It’s amazing, though, that simple and easy breathing exercises done three days a week could have such an effect. The only thing the participants were working out, after all, was their lung muscles – and it wasn’t a hard workout. Edgell provided the easiest version of inspiratory training possible:
“We chose a type of training that did not increase effort with time, but rather decreased the time between breaths in consideration of the potential for post-exertional malaise (PEM). We were in communication with patients throughout the protocol to help with pacing and to make sure that patients were doing well. I highlight this as researchers need to act with care and understanding with any protocol that involves physical activity in these populations.”
The authors believed the improvements were due to improved parasympathetic activity (vagal tone).
Doing Inspiratory Muscle Training (IMT) at Home
Applying the Arseneau test, which assesses the factors below to help decide whether or not to try a treatment, suggests IMT is an easy win. The device is readily available, not particularly expensive, and the process is easy to learn.
- The credibility of the source – IMT has been time-tested in other conditions
- Quality of the evidence – while the study was small, the results were positive
- The benefit, the cost, and the risk–benefit – the benefits are probably moderate, the risk is low (you can discontinue at any time), and the cost is low.
What’s not to like?
The Respiratory Therapy Zone recommends the following trainers. Since some of them are quite different, it might be worth reading the reviews:
- The Breather Respiratory Muscle Trainer – $49.95
- POWERbreathe Plus Resistance Breathing Exerciser Trainer – $68
- AirPhysio Sports Edition Breathing Exerciser – $69.97
- POWERbreathe Plus Fitness Breathing Muscle Trainer – $49.99
- AirPhysio Natural Breathing Lung Expansion Exerciser
- Breather Fit Respiratory Muscle Exerciser Trainer – $59.95
- Expand-A-Lung Sports Breathing Exerciser – $49.90
- Voldyne 5000 Volumetric Incentive Spirometer Exerciser
- Quest Lung Performance Peak Flow Meter – $23.47
Note that it can take a month or so to begin to see results.
Quite the Return on Investment
The pilot study did what Solve M.E. hoped it would do – result in more funding. Since her Ramsay Award, Heather Edgell has won over half a million dollars in other grants to bolster her Ramsay Grant findings.
She’s not alone. Solve M.E. reported that from 2016-2023, it funded $1.3 million in 37 infection-associated chronic illnesses studies through its Ramsay Research Grant Program. Over time, those grant recipients subsequently won over $27 million in funding. Many times all a researcher needs is a start, and that’s what the Ramsay Awards provide.
The Duricka Award
Two treatments focus on either side of the autonomic system – and both provide help.
Deborah Duricka provides an intriguing counterpoint to Heather Edgell’s findings. Also a Ramsay Awardee, Dr. Duricka recently published a retrospective chart review on stellate ganglion block – another formerly untested treatment – targeted at the same system – the autonomic nervous system.
Duricka has found that injecting anesthetic into the stellate ganglion (the SGB) can relieve pain, regulate sympathetic nervous system activity, improve sleep, increase cognition, and improve neurological function. Even the big symptoms – post-exertional malaise – quickly improved. With one in three long-COVID patients still experiencing relief a month later, the shots had some legs.
Neither Edgell nor Duricka would have had a chance at the NIH. Both are examples of the uniquely creative approaches to ME/CFS the non-profits provide. Standing on the cutting edge, they open doors that would have never been opened without them.
- Coming up – a look at a recent Open Medicine Foundation-funded ME/CFS study, and several talks with Benjamin Natelson on his new studies, the unique breathing problems he’s found in ME/CFS, and his new attempt to reset the autonomic nervous system using vagus nerve stimulation.
Health Rising’s Donation Drive Update

Health Rising is on the hunt for cures and ways to improve all our lives.
Thanks to everyone who has donated over $45,000 during Health Rising’s End of the Year donation drive.
We don’t have a surefire cure for ME/CFS and related diseases yet but there are ways to get better and finding them and communicating about them is a core commitment of Health Rising.
If that’s important to you please support us!






I have ME/CFS (since 2000) and Long Covid since 2022. In May 2024, I was diagnosed with unknown myopathy and my respiratory muscles functioning at 17% of predicted (I’m 70). This explained my extreme shortness of breath but nobody has any answers. I bought The Breather and used it almost daily, twice a day, for over 3 months. I had absolutely NO improvement in my symptoms. I’m rather surprised at only doing it 3x/week. Maybe I was overdoing it because, yes, it exhausted me, but I was desperate for improvement. I might try again this way. Thanks.
I updated the blog. Here was the protocol.
Each session consisted of 6 sets of 6 repetitions (total of 108 breaths/week) with the goal of progressively reducing the rest time between sets from 60 s for the first 2 weeks to 10 s for the last week.
If I got it right they would take 6 breaths through the device, wait for a minute, then do six more breathes for a total of 36 breathes per session. Over time they would reduce the rest period to 10 secs.
Thank you so much for responding. I didn’t think you’d be able to give the exact protocol. You don’t know how much I appreciate this!!!
Glad to hear it!
Ooh such an interesting finding! I wonder if some forms of breathwork have the same or similar effects? Ie whether you need the device or certain breath patterns (eg ones with holds) would have a similar effect…..
Good question. The different thing about this may be that it adds resistance to the breathing. I would think that holding the breath would add some resistance somewhere 🙂
Nice! A quick and easy to try Pilot study that already resulted in further founding. Thank You Cort!
I Read the study and Noten an important step in the design:
The maximal inspiratory muscle pressure (MIP) of each participant was measured at York University (Respiratory Force Pressure Gauge, Vacumed, USA), a simple non-invasive procedure for determining inspiratory muscle strength.
Then:
The IMT devices were set at 80 % of each individual’s MIP for the duration of the study.
So as far as I understand, it would be best to receive a MIP Measurement to be able to pick the right trainer/ its strength.
I know this will not be be accesible for everybody but wanted to mention it as it seems quite important.
Hmmmm, I am looking at the Powerbreathe plus and I cannot find any online anywhere near price you listed Cort, do you have a link?? The ones I am finding are all about $200.
– Cheers
https://trainjelongen.nl/shop/leefstijl-medisch/plus/
The Powerbreathe Plus appears to be available on Amazon for around $75 (https://www.amazon.com/dp/B00AWRYQVU/) though there are different levels of resistance. Cort, do you know what level of resistance was used in the study or can you find out?
The level of resistance seems pretty important to me. There are indeed different levels of resistance depending on the device, in addition to being able to alter the resistance on individual devices. I used to recommend Inspiratory muscle trainers to patients, as a Respiratory Physiotherapist… but mostly avoiding the Power Breathe at the time as the resistance was too strong for patients with Respiratory conditions. I myself have bought a cheap but low resistance device and feel it is the right level for me – moderate/severe M.E/CFS… It’s surprising how tiring and difficult I find it even without Respiratory disease! I’ve been really rubbish and poorly compliant with mine – but my head tells me it’s good to do this sort of training when we are unable to get much aerobic exercise with M.E/CFS (and hence maintain respiratory muscle strength). Now that this study reports parasympathetic improvements too… I must start using it again, and frequently.
I think this is the one I have:
https://www.amazon.co.uk/Ultrabreathe-Adjustable-Resistance-Breathing-Exerciser/dp/B007CI0ZBC/ref=mp_s_a_1_19?crid=3T91TN62MUJGW&dib=eyJ2IjoiMSJ9.VYFyeEEjkWWQmnBsesNpHEtL0Ozas7o-ozFmVVSIuBUmbZjiwTDyy7AEfEHjlT-kMuhlrj4bdXZiI-lmaWJM0v35yRMDehMj3nluLYn0t7_8xPL5wQRa78LqS9LZRI55XbnmVWOM19F73ZSpvGP533tqBYwWSRBOk36BEekZ87DlPFRTrVpRSj9dxIWgyLBpI-EeG9s4zarQp9Z_t0ivcA.zzZ-IW-FarQYPgBJn8CJHr5TDF-pZ4X6W-jHA9IqxgA&dib_tag=se&keywords=respironics+inspiratory+muscle+trainer&nsdOptOutParam=true&qid=1735164375&sprefix=respironics+inspiratory+muscle+trainer%2Caps%2C101&sr=8-19
This is what we were supplying to RESPIRATORY patients around 15-20 years ago and I see no reason why they wouldnt still suit some patients: https://www.physioparts.co.uk/threshold-philips-respironics-imt
I have Long COVID since 2020 but diagnosed as having ME/CFS since I never had a COVID test when I first got sick (I didn’t qualify for testing). Recently I was given an additional diagnosis of Breathing Pattern Disorder after a CPET. Apparently it is common in long Covid patients.
I’ve been seeing a respiratory physiotherapist and an acupuncturist, the former for breathing exercises and the latter for fascial release of my chest and back muscles, to allow the muscles to work better. The combination has made a great difference, and I continue to do the exercises. I might invest in a Breather as well. I don’t feel like this is a cure but definitely an improvement. And I agree it is a process, it takes time for the benefits to start showing. Don’t overdo it, start slow and gradually increase as you are able.
The therapist told me she could hear no breathing sounds in my lower lung lobes, air wasn’t getting down there. Critically, that is where most of the alveoli are. I was sceptical, but over time I could walk further faster, without chest pain. When I am really tired I do the exercises, they take the edge off the fatigue. It feels like a minor miracle for me.
This is really encouraging! Thank you for sharing your experience. I often feel like there is a defector of oxygen getting into my lungs and body and I have to remind myself to breathe which sound really odd.
I was recommended by a SLP, and used an expiratory training device that was adjustable. I found it helpful early on and will revisit using it.
Thanks and good luck!
Finally this is an excellent therapy for ME/CFS patients with an overactive sympathetic nervous system. If you know what causes this unique breathing in ME/CFS patients, then you know the cause of this disease. I would also like to wish everyone here a good New Year and better health. Cort thanks for your blogs!
I too have to remind myself to breathe, although now it is more about reminding myself to breathe deeply, using my diaphragm not my upper chest.
Edit: I intended this as a Reply to Jessica Schmidt, but Oops! Brain Fog and/ or clumsy fingers
I have to remember to breath at times as well. I’m doing a bit better now but I’ve often thought I have not taken a nice relaxed deep breath in decades.
Fascia release of my chest and back muscles really helped. It made the breathing exercises so much easier, and the more I do them the easier it gets. Happy new year!
Nice – I hadn’t thought of fascia release of the chest and back muscles but it makes total sense. Peter Rowe uses something similar to release neuromuscular tension and I’ve found that stretching helps. Things get pretty tight after awhile….
This seems soo complicated, so I doubt I will get one.
However I practice 40 min. vagus nerve meditation every day.
I also practice coherent breathing every day which really calms me down and puts me into a “zone” I dont want to get out of.
My outbreath is always through an almost closed mouth to slow down the outbreath.
I think this comes quite close to these tools.
My next investment will be The “Visible” armband.
Maybe you could write about it one day, Cort.
Would be lovely.
Happy New year to all!
ps. I survived xmas quite well with visits on 3 days – it is because I did the 40 min. vagus nerve med. right after each visit and the coherent breathing before. I am very severe, bedridden fulltime
We wrote about the Visible but I think I’m behind. Is it out?
https://www.healthrising.org/blog/2022/11/19/visible-app-long-covid-chronic-fatigue-syndrome/
That’s brilliant I’m severe also. All these meditations on YouTube hun x
Thanks! Happy New Year to you too! (and to everyone – heres to a healthier year next year 🙂
My eye spots a problem regarding the HRV data versus conclusion:
The text above table 4 says:
In response to IMT, we observed that all groups decreased LF power (p=0.035), increased HF power (p=0.034), increased RMSSD (p=0.034) and increased pRR50 (p=0.035; Table 4).
Table 4’s data says:
Control (n=9) PASC (n=7) ME/CFS (n=9)
Empty Cell Baseline Post-IMT Baseline Post-IMT Baseline Post-IMT
RMSSD (ms) 54.2 ± 23.0+ 75.7 ± 37.8*+ 27.6 ± 14.3 36.5 ± 18.0* 33.7 ± 19.3 30.8 ± 11.1*
=> RMSSD decreases for ME/CFS after treatment contrary to the conclusions, while it increases for all other groups. It could be a typo in numbers, a wrong conclusion or my poor interpretation. So long this and its importance is not cleared out I would hold off from trying this at home for ME/CFS.
LF/VF also goes opposite in ME/CFS after treatment, although very much within the margins of error.
I’m concerned about this, would love another person with the research/stats skills to weigh in on these points.
Additionally the protocal seems to rely on measuring MIP first, and callibrating exercises to 80 percent of MIP. It’s easy to just buy the exercise device, but I’m finding it hard to know how to measure MIP.
There is definitely an inconsistency between the table and the text with regards to the RMSSD data. The value in the table goes down for the ME/CFS group, but the text says significantly increased. One of them is wrong.
Speaking as someone that’s analysed 1000s of clinical study reports, the way the statistics is reported in Table 4 is unusual and raises questions for me. Normally, you would compute a P value for each treatment group compared with the group’s baseline. However, here they are reporting a single P value for differences across all 3 treatment groups. Also, given the size of the differences from baseline and the reported standard deviations, I am surprized to see so many significant P values as I would expect to see more not statistically different outcomes.
I was thinking the same thing as Anon…. Is it to do with the baseline SDs being large? Is it taking outliers into consideration? Are there a large individual differences within the ME group? Can decreased LF account for the decrease in RMSSD from 33.7 to 30.8? How could it have significant result in ‘increased in RMSSD’? I am rather confused. Cort how doyou interprete the table 4 in the study?
This pilot study showed possibility of relatively cost effective and easy aid for those with ME but I agree with you Anon, I personally wait for further studies.
I didn’t notice that.
I asked ChatGPT – “If the LF portion of HRV goes down should RMSSD decrease or increase?
It was very interesting: the two are not exactly linear or measure exactly the same thing. Under different circumstances it may increase or decrease…
“RMSSD May Increase: If the reduction in LF corresponds with a shift toward parasympathetic dominance (e.g., during deep relaxation, recovery, or vagal activation), RMSSD might increase as parasympathetic activity typically boosts vagal-mediated HRV” – that apparently DIDN”T happen. Instead
“RMSSD May Decrease: If the decrease in LF reflects overall autonomic withdrawal (both sympathetic and parasympathetic activity reducing, e.g., during fatigue or illness), RMSSD may decrease as vagal tone diminishes. i.e.; it appears that the inspiratory breathing reduced autonomic overactivity, I guess.
I have heard something like this before – that it’s not just that the fight/flight system is overactivated but that the whole ANS is trying to find balance (and maybe is overactivated?
I remember Pocinki doing things with the ANS and getting weird results from his ME/CFS patients. It wasn’t as simple as we might have thought.
Thanks Cort for checking on RMSSD and insights on the overactivity of ANS.
I asked ChatGPT – “IF the LF portion of HRV goes down should RMSSD decrease or increase?
It was very interesting: the two are not exactly linear or measure exactly the same thing.
“RMSSD May Increase: If the reduction in LF corresponds with a shift toward parasympathetic dominance (e.g., during deep relaxation, recovery, or vagal activation), RMSSD might increase as parasympathetic activity typically boosts vagal-mediated HRV” – that apparently DIDN”T happen. Instead
“RMSSD May Decrease: If the decrease in LF reflects overall autonomic withdrawal (both sympathetic and parasympathetic activity reducing, e.g., during fatigue or illness), RMSSD may decrease as vagal tone diminishes. i.e.; it appears that the inspiratory breathing reduced autonomic overactivity, I guess.
I have heard something like this before – that it’s not just that the fight/flight system is overactivated but that the whole ANS is trying to find balance (and maybe is overactivated?
I remember Pocinki doing things with the ANS and getting weird results from his ME/CFS patients. It wasn’t as simple as we might have thought.
Can anyone explain the difference between the breathing devices listed in this blog vs a cheap incentive spirometer from the hospital? Because I already have an incentive spirometer from an old surgery.
I asked ChatGPT about this: it said an spirometer is used to increase lung expansion while an inspiratory breathing device – because it adds resistance increases lung muscle strength – so they are actually quite different!
It would be interesting in future studies on inspiratory muscle training if a measure of cerebral blood flow could be used to measure OI before and after, either Doppler ultrasound or the research version of of the Lumia Health cerebral blood flow monitor.
I don’t know if that’s in the cards as well but she hopes to expand the study greatly. I think that would be a great idea. Looking forward to the Lumia device when it (finally) is ready.
This is so interesting. A post here a few years ago was about the role yoga played in someone’s recovery/management of ME. I started doing it most days, and for me it has been the difference between being really quite sick, and being able to manage a full-time job. I always suspected it’s the deep breathing that is helping, and this study supports that. I might also give the IMT a go.
Nice! It’s all about oxygenation and calming down the ANS! Good to hear.
Cort, this study is so practical–even inspirational, thank you.
I’ve had breathing “from the mouth” problems since childhood. I remember snoring when I was barely 10 years old–and was teased as a child, called “slobber-mouth” from the neighborhood kids from my overactive saliva glands.
My parents thought it was a good idea at the time to have surgery to remove my adenoids (and tonsils too) which really helped me at the time. I was a good 4 sport athlete (with no lung problems whatsoever) through my teens and most of my early 20’s–and then CFS struck. I’ve been sick for 30+ years with this horrid disease!
I’ve been using a CPAP machine for 15 years to help me breath at night.
I purchased the $49 “The Breather” from Amazon and it arrived today. Maybe this device is not only about the lungs but about the breathing airway? Only time will tell, I’ll update here if it works.
BTW, I went through the Stellate Ganglion procedure 2 years ago. It did not help my CFS whatsoever.
I have used high salt and water and compressive garments for decades to counter Orthostatic Intolerance. A year ago I found that I could walk fast but not slowly. If I walked slowly I would become fatigued. Sometimes I could walk faster and exercise my way out of the fatigue, sometimes not. I tried Inspiratory Muscle Training, intitally through pursed lips, then with a cheap uncalibrated hands free device, then added a Phillips Respironics with an impedance maximum of 49cm water. I then tried chewing gum. Chewing gum had a greater effect on reducing fatigue than IMT and chewing was much less effort. I continue chew gum all my waking hours. I breathe through the Phillips device for 5 minutes every couple of days.
The effectiveness of the chewing gum in relieving fatigue indicated to me that not all of my fatigue was due to O.I. Some of the fatigue was due to low cerebral blood flow.
Recently I again began to have difficulty with walking slowly. I first tried exaggerated arm movements and clenching my fists, which was fairly effective. I then tried humming. Humming was more effective with less effort.
Thanks Ian – can you say what the chewing gum connection is?
The article stated that inspiratory training was beneficial but the nebu device on the link is for expiratory training. Was it an error to include that product?
The best way to test at home, would be to buy one of these devices for breathing and also to have a smart watch that can measure HRV, that we can have our own objective data.
But would the cheap and easy way, be to purse our lips and do the breathing cycles as described by Cort in another reply, and just see how our symptoms go after 6-8 weeks? EG, is it really necessary to use a device if our own mouths can restrict the flow of air.
Ik heb een Powerbreath gekocht. Ik begrijp dat je 6 sessies van 6 ademhalingen moet doen en daar 1 minuut pauze tussen houdt. De intensivering zit in het verkorten van de pauzetijd.
Mijn vraag is: op welke stand moet de weerstand staan?
How do you figure out which of these devices to use for your particular problem with breathing? My diaphragm just doesn’t open enough due to very tight ribs.