Geoff’s Narrations
The GIST
The Blog
The GIST is on the middle right-hand side
“It is startling that here we are in 2024, recognizing how critical our immune system is for protecting us against infections and major diseases…yet we have no informative clinical test to get at it. We desperately need a means for assessing our immune system.” Eric Topol July 2024
“The paper provides a first proof-of-concept, a stepping stone, towards a full immunome.” Eric Topol February 2025
Topol first wrote about the need for an immunome—a way to assess all immune system components together—last July. He noted other studies that were beginning to grasp the “immunogen”, but all involved techniques that were too expensive to be used in the clinic. Not so with this latest technique, which offers the potential of an inexpensive way to chart the immunome—hence Topol’s title, “The First Diagnostic Immunome”.
Topol called the study, “Disease diagnostics using machine learning of B cell and T cell receptor sequences,” which appeared in the Science journal, “extraordinary,” and said it was co-authored by a who’s who list of immunologists and rheumatologists.
The Mal-ID process
The study assessed the receptors or antennae found on T and B cells. Because these receptors track and need to keep up with every pathogen, vaccination, autoimmune response, and toxic exposure our cells are exposed to, they provide a living encyclopedia of our immune history.
To respond to the many factors that our immune systems are exposed to, though, these receptors must be extremely nimble. That means they quickly rearrange their genes, or mutate, in order keep up with the bombardment of insults to which our immune systems are exposed. That complexity has made sequencing them difficult – if not impossible – to assess until now. Not surprisingly, it’s artificial intelligence that’s making the impossible possible.
Topol noted that Sarah Teichmann, at the University of Cambridge, stated, “This is a one-shot sequencing approach that captures everything that your immune system has been exposed to.”
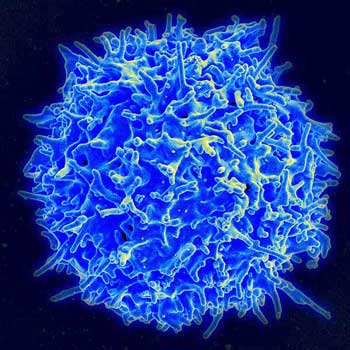
A T-cell.
The researchers, led by Maxim Zaslavsky, used a process called Mal-ID (Machine Learning for Immunological Diagnosis). The study, which included nearly 600 individuals with a variety of conditions (hospitalized with acute COVID, autoimmune Type 1 diabetes, HIV, 37 – a recent flu shot) and healthy controls, sequenced the two parts of B and T-cells (the heavy chain of the B cell receptor and the beta chain of the T cell receptor) that play a critical role in recognizing immune insults (antigens) and binding to them (so that the immune system can respond) in tens of millions of T and B-cells.
The authors used three different analytic models to assess the data. They found that T cell receptor analysis was best at predicting lupus and Type 1 diabetes while B cell receptor sequences were best at identifying HIV, SARS-CoV-2 infection or recent influenza vaccination.
THE GIST
- Because the immune system is at the heart of so many diseases, Eric Topol wrote last year about the importance of developing an “immunome”- a way to easily track all immune activity.
- This year, in what Topol called an “extraordinary” study co-authored by a “who’s who list of immunologists and rheumatologists,” a major step forward had been made in producing one – a step that could impact diseases like ME/CFS, FM and long COVID.
- The study deciphered the regions on T and B cells that rearrange themselves when the immune system is faced with pathogens, toxins, and autoimmune processes. These rearrangements are so complex that no one has been able to decipher them until now.
- Using artificial intelligence and other data analysis techniques, this team largely predicted correctly which participants had autoimmune diseases, diabetes, had had a flu vaccination, etc. When applied to a single disease, the authors stated these techniques can pluck out subsets and track treatment effectiveness.
- That’s where diseases like ME/CFS and long COVID come in. Topol said that this technique was perfect for deciphering mysterious, heterogeneous, immune-based diseases like ME/CFS, long COVID and post-treatment Lyme syndrome.
- Topol’s recent talk with the authors indicated that their techniques have progressed rapidly, and they feel these analyses can be made cheaply and affordably. That will presumably take some time.
- This study shows that it’s impossible to predict the impact of AI-driven advances on complex diseases like ME/CFS and long-term COVID. Who knows where we will be in two, three or five years?
The test’s ability to accurately assess disease specificity and sensitivity was lower (93% were accurately assessed as healthy or not, and 87.5% were accurately determined to have the correct disease). While some healthy people were assessed to have an autoimmune disease, Topol noted that these people could be vulnerable to an autoimmune condition.
Topol’s talk with the lead authors found that they’ve done sequencing in many more people with autoimmune conditions and that the tests have provided illuminating insights into therapies. Plus, when they become available, the tests should be inexpensively done at scale in batches with quick turnarounds.
The ability of this technique to subcategorize disease states at the molecular level could be particularly helpful in heterogeneous diseases like ME/CFS, FM, and long COVID. One of the co-authors – Boyd – noted that even autoimmune diseases have subsets that are significantly different at a biological or molecular level. Boyd told Science Daily:
“Mal-ID could help us identify subcategories of particular conditions that could give us clues to what sort of treatment would be most helpful for someone’s disease state.”
We’ve already seen that although Gulf War Illness and ME/CFS look the same in some ways, they are very different creatures indeed. A similar revolution in botanical classification took place with the advent of genetic analyses. Some plants put into families based on their appearance turned out not to be related at all, and plant classification was fundamentally changed.
Topol also noted that the use of a large language AI model called ESM-2 played a critical role in the study. While the study was a bit “contrived” because the authors used a limited number of conditions to test the model on, the authors stated that much progress had been achieved since the paper had been written.

The AI-trained system’s ability to identify molecular subsets within diseases could be a big boon in diseases like ME/CFS/FM and long-term COVID.
Topol envisioned integrating the T and B cell findings with other immune system findings (autoantibodies, virus and pathogen exposure, flow cytometry, T cell functional assays, interferon, HLA typing, etc) to create a full picture of the immunome. This seems eminently possible given the dramatic uptick in our ability to assess large amounts of data. The limiting factor doesn’t appear to be on the analytic side but on our ability to gather all the data; i.e., to get the funding to gather as much data as possible from as many people as possible.
Applications to ME/CFS, Long COVID and other Post-Infectious Illnesses
Topol stated that this new technique was perfect for understanding mysterious, complicated diseases like long COVID (and thanks to Mark Camenzind’s question) to ME/CFS and post-infectious diseases like post-treatment Lyme Disease (PTLD). Topol stated that not only that “diagnosing and following individuals with Long Covid is an exemplar for how this could be applied” but that it could be used to test the effectiveness of treatments.

When asked, Topol said the approach was “perfect for ME/CFS”.
When ME/CFS advocate Mark Camenzind asked if this approach could be applied to ME/CFS, Topol called it “definitely, a perfect application for ME/CFS”, and responded similarly to a question regarding Post-Lyme Disease Treatment Syndrome (PLDTS). The approach could also be used to uncover what’s gone wrong in post-vaccination syndrome and who is at risk for it. Mark Camenzind noted that the study originated at Stanford and that Paul Utz – who is studying ME/CFS and is the co-leader of the RECOVER long COVID program at Stanford – was a co-author.
This technology will take some time to become available, but it shows that we live in exciting times. With artificial intelligence enabling medical research in so many ways, who knows what’s around the corner?
The study was heavily funded by the NIH (20 grants (!))) as well as other grants and philanthropic support. Topol – who has been quite critical of the NIH – nevertheless decried the recent changes occurring at it, the CDC, the FDA and the Dept. of Health and Human Services. Calling it “dark times for biomedicine”, Topol – citing the “marked acceleration of progress” that is occurring, due in part to AI – said he had not lost optimism.






For those who believe their ME/CFS could have been triggered by a toxic exposure, the news I received this morning should be a “light in the dark” for you.
The National Institute of Environmental Health Services (NIEHS), an organization I worked with for 20 years, sent out a Public Health Impact story which reports on detoxification through safe edible clays and a cream to prevent toxic exposures.
Led by Timothy Phillips, Ph.D., a team at the Texas A&M University (TAMU) Superfund Research Program (SRP) Center developed sorbent materials made of nutrient-enriched clays that are safe for consumption. Research shows that after being ingested, the sorbents tightly bind complex mixtures of hazardous chemicals in the intestines, thereby decreasing chemical exposures and reducing the likelihood of harm to health.
The sorbents can be purchased commercially for human ingestion and are pending FDA clearance. This technology has also been modified to create a cream that forms a barrier between the skin and harmful chemicals. Usage of both types may follow floods, chemical spills, and other emergencies
Hi Betty – by any chance are they bentonite based? I used to hear a lot about bentonite 15 years ago….
Hi Kira, I am going to contact the researcher to find out what kind of clay they are using. I also heard about bentonite clay a while ago, but I am guessing this is somewhat different since they have developed a protective skin cream. I’ll let you know what I find out.
I take bentonite clay and charcoal on a semi regular basis. I’ve been exposed to many chemical throughout my lifetime…but…so has the next guy and he escapes unscathed. That’s the part that we need to figure out
thanks!
Thanks for the blog. I didn’t know this study was happening. Hope to see more of this type of research! Sounds like it could be quite promising.
I started using bentonite clay to detox internally 9 years ago. Dropped my arsenic levels per lab testing. Aristotle (384–322 BC) made the first reference to the deliberate eating of clay for therapeutic purposes. Good to see “modern” medicine approves.
The analogy of how plant classification changed with the advent of genetic analysis was so apt. This is a perfect example of the quality of journalism at Health Rising, where important scientific and medical concepts, as they relate to ME, are made accessible to the average reader. With developments like these we will hopefully see clear subsets of ME, Long Covid, etc arise and Drs will no longer be able to treat ME as a sort of disposal mechanism for complex patients, who then stop being individually investigated toward appropriate treatment.
Amen!
Thanks! My Masters was in Env Science with a focus on plant ecology. I love to get plant stuff in there 🙂
Is it possible to pinpoint an approximate date when someone came down with a particular infection?
Yes…I know the exact date of my
” infection”….or maybe you mean can the medical Establishment find the exact date
Roonie,
I’m referring to the researchers – if they have the ability to approximate when someone had an infection. For people like you and me, who can pinpoint a date, we’d be able to know what kind of a virus caused our disease.
I’m beggining to think my infection was caused by a molar tooth that had been pulled but not sewn up after extraction.my other 2 extractions were sewn up but one did not get sewn up.
That tooth socket took forever to heal over.all my troubles seem to be in my head….aching Jaws,very irritated gums,bleeding gums that I assumed were from not brushing,flossing enough as a teenager but then I finally remembered that tooth socket.
Then after my immune system went into overdrive,lumps appeared all over my body.i hade tiny bumps inside my nose that were white in color.
I continue to take ivermectin. I continue to slowely improve.i have 3 fused vertabrea that I’m learning can be from infection.i got gaslit since 1981.
Interestingly enough I just received an email from orthomolecular science on this very subject of infection from tooth extraction
Interesting paper from James Baraniuk:
https://www.nature.com/articles/s41598-025-91324-1
I wonder if EMF was included in the info given to the AI.
Let’s hope that Trump/Musk doesn’t cut funding for this research as well.
Can someone explain what finding was 99% accurate? It wasn’t disease specificity or separating healthy controls so what was it? I didn’t understand that bit.
Using AI to help diagnose and treat complex disorders like ME/CFS, Long Covid, FM, and GWS has the potential to save time and money. These conditions are multi-faceted and impact multiple systems in the body that are interdependent. AI has promise to better serve patients with treatments that are more customized to individual needs based on the data presented. I think AI could play a big role in the future of medicine.
It’s so depressing. It’s always “Could/Would/Should/Maybe/Will? Never anything certain. Sorry, I’m having a rough day.
Is there a chance in hell we could start a poll specifically to find out if most of our spouses also come down with me/cfs
Re: contagious
Excuse me if a poll has already been done
Thanks
Brianne Dressen, one of the authors of this study, shares her vaccine injury (from Fall 2020 after participation in one of the first clinical trials) in new book ‘Worth a Shot?’ by Caroline Pover.
I consider this research to be a significant breakthrough, and, since it was made with emerging (AI) technology, this is likely only the beginning (providing there is funding and initiative for further research). If I understood correctly, there is even a practical clinical application for a specific, affordable and conclusive diagnosis in the works.
I suspect that once the (epi)genetic (or other) changes (to T, B and/or other cells) that underlie our chronic symptoms are understood, there is a very good chance that effective treatment (or possibly even a cure) may follow. In general, it is unlikely that any problem can be resolved until after its cause is understood. It seems to me that this research may (finally) be getting down to the root cause(s). I only hope that practical applications for diagnosis (and effective treatment) become available in the foreseeable future, so current older patients can benefit.
Great reporting (Thank-you) Cort!
Wishful thinking IMO that this will lead to any real breakthroughs. Yes, we will see hints of patterns, but will they be actionable. Topol as usual love to jump to unwarranted conclusions and hype. Not that this work should not continue, but we should be circumspect in assessing its ultimate value
thank you for sharing Cort!