
Some long-COVID researchers have met with resistance from large drug companies.
For patients, it all comes down to treatments, and that means clinical trials – and lots of them. Given that, it was hard to read Rowan Walrath’s article, “Long COVID studies stymied by pharma’s lack of cooperation“, in Chemical and Engineering News (C&EN), indicating that big pharma is not embracing long COVID. (Most of the first part of this blog is taken from Walrath’s article. Hats off to her and C&EN for charging to the forefront with three articles on long COVID over the last couple of months.)
For people with ME/CFS, the lack of interest from drug companies is nothing new. Despite the millions of patients with the disease, ME/CFS has seemed like kryptonite to the big drug companies. Except for Rituximab, which was largely patient-funded, and the Ampligen trial done decades ago, it’s hard to think of a single large drug trial for ME/CFS that has taken place. Ampligen is still the only drug that has made it even partway to FDA approval.
Could long-term COVID, even with its tens of millions of patients in the U.S. and the huge potential payday they represent, be suffering the same fate? While it’s clear that’s not going to happen, Walrath’s article indicates that the same biases and problems that have afflicted ME/CFS for decades are hampering the search for a treatment for long COVID.
Avindra Nath’s search for a drug trial is a good example. One might think that Nath—the clinical head of the NINDS intramural center—might have some sway. Nath successfully used a drug called Keytruda to treat progressive multifocal leukoencephalopathy (PML) and has stated he wants to try checkpoint inhibitors in long COVID and ME/CFS. However, his attempt to get MERCK to provide Keytruda, which is used to treat T-cell exhaustion, failed. A similar attempt to get Bristol Myers Squibb to provide a different combination of checkpoint inhibitors met the same fate.
Here’s the thing: Nath had everything but the drug taken care of. Using the NIH’s investigator-sponsored research funding mechanism, the NIH was willing to fund Nath’s and his staff’s salaries, lab needs, patient recruitment, etc. All Nath needed was the drug company to provide the drug gratis. Nath told Walrath, “All the rest we can do ourselves. We just need the drug.”
While these drugs are not cheap—they cost upwards of 10K a dose for patients – the companies stand to make billions and are already making billions from them. Keytruda earned MERCK and Company a cool $29.5 billion last year. Nath stated, “They make billions of dollars off this drug alone. In dollar amounts, for them, [drug donation] is a drop in the bucket.”
Nath, unfortunately, is not alone. Walrath reported that Northwestern University neurologist Igor Koralnik got the same answer when he approached Eli Lilly, Amgen, and other drugmakers for drugs to treat severe headaches in long COVID. Sounding surprised and rather bitter, Koralnik, who has published a remarkably extensive paper on the neurological manifestations of long COVID, told Walrath:
“It was a big expenditure of energy and time on my end for no results. It would be interesting if you could go to Eli Lilly and can talk to the people who are making the decision about headache and say, ‘Have you ever even heard of Dr. Koralnik?’ I would bet my saddle and my horse that they would say no.”
Nancy Klimas’s attempt to find a company to provide a drug that was: a) no longer being used; and b) just sitting on a company’s shelf, presents another cautionary tale. Klimas was ultimately successful, but it took work. Even after getting remarkable results in her long-COVID patients, Klimas was still turned down by three large drug companies (GSK, Lilly, Regeneron) before she found one willing to help. Klimas called it a “happy ending to this story instead of a terminally frustrating one”.
What’s Going On?
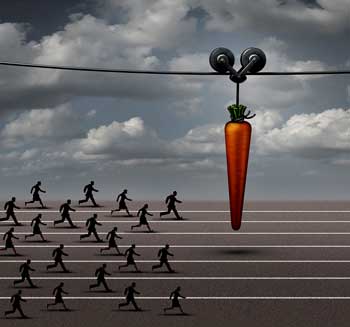
Tens of millions of long-COVID patients in the US alone have not been enough to entice many big pharma companies to provide support.
The big question is why big pharma is not chomping at the bit at the huge potential payday that will clearly result from producing the first FDA-approved drug for tens of millions of people in the U.S. alone.
Walrath’s article suggested that one reason may be quite mundane—and that’s bedeviled ME/CFS at the NIH and elsewhere for decades. It’s a matter of location. Where do you fit a disease that affects so many systems? If you’re a major pharmaceutical company, do you give long COVID to your cardiovascular, metabolic, or immune teams?
Indeed, a general lack of clarity about the disease itself, plus the sheer difficulty in assessing a drug’s effects, appear to be the primary culprits. A biological biomarker that could be used to track drug efficacy would solve all problems. It was that kind of biomarker that quickly turned around drug development for HIV/AIDS.
A biological biomarker is not always necessary, though. No biological biomarkers have been found for fibromyalgia (FM), but FM has 3 FDA-approved drugs and regularly receives clinical trials. FM has something, though, that both ME/CFS and long COVID lack—a clear FDA path to drug approval. Once the FDA stated it would accept validated pain assessments as proof that a drug works in FM, the drug companies quickly came on board.
Because we know much more about pain pathways in the body than we do about fatigue, FM’s path was easier. We know, for instance, that pain-producing pathways, involving nerve centers in the body, the spinal cord, and at least six regions in the brain, as well as at least six neurotransmitters, have been dysregulated in FM. Plus, assessing pain sensitivity levels using objective markers of heat, pressure, and cold is simple.
Nothing close to that has been achieved with regard to fatigue in ME. Numerous validated fatigue assessments do, however, exist. Seth Lederman of Tonix Pharmaceuticals asserts that the quickest way to get pharma involved in ME/CFS and long COVID is simply for the FDA to tell pharmaceutical companies that their drugs will get approved if they meet certain fatigue criteria.
Missed Opportunities – the Biomarker Issue
The clinical trials dilemma the ME/CFS-like subset of long COVID is in could have been predicted. A new, heterogeneous disease characterized by two mostly mysterious symptoms (fatigue and post-exertional malaise symptoms) was never not going to make it with big pharma on symptoms alone.
The NIH’s $1.15 (now $1.65) billion long-COVID RECOVER Initiative presented the best possibility for finding a biomarker. It had the funds to do a deep dive into the molecular underpinnings of long COVID but chose not to. One could understand RECOVER being wary about doing that, but in retrospect, what other choice did it have?
Anyone looking at ME/CFS realized that ordinary laboratory tests would have been largely unrevealing, yet RECOVER has spent much of its money attempting to characterize long COVID using these tests. The result is that 5 years later, RECOVER has not come close to accomplishing what arguably should have been its first task: to produce clear and accurate diagnostic criteria that paved the way for drug trials.
Not All is Lost

Many drug trials are underway, though, and some are large enough to provide instant validation.
All hope is not lost, though. The field may not be moving forward as quickly as we wish, but it is moving forward in surprising ways. Even with big pharma still acting largely allergic to long COVID, many intriguing small and large drug trials are underway. ME/CFS patients note that most of these drugs have probably never even been contemplated in ME/CFS.
Note that this list focuses on drugs, and because most of the data comes from the https://clinicaltrials.gov/ website, it is surely incomplete. It does not, for instance, include the next $500 million round of long-COVID clinical trials produced by the newly revamped treatment arm of the RECOVER Initiative.
Check out the wide variety of drugs being explored.
Immune Drugs
Antivirals
- Truvada trial (tenofovir disoproxil/emtricitabine, TDF/FTC (Group 1) or Selzentry (Maraviroc) (Group 2) – two repurposed HIV drugs. PolyBio study. Putrino, Iwasaki and Proal (n=90)
- Ensitrelvir – small antiviral trial at UCSF led by Michael Peluso that will explore efficacy and try to understand what’s going on in long COVID
- Remdesivir (Veklury) – antiviral; Remdesivir is being explored in COVID-19, but it’s a broad-spectrum antiviral that may be helpful with many RNA viruses (but not herpesviruses, which are DNA viruses). (Two trials are underway: n=48 and n=150)
- Plitidepsin inhibits coronavirus replication and other viruses, including MERS, Zika, herpes simplex, etc. Has not been tested against EBV or HHV-6, but its mechanism of action suggests it could be helpful (n=90).
Monoclonal Antibodies
- Monoclonal antibody AER002 – small monoclonal antibody trial at UCSF led by Michael Peluso, which will explore efficacy and try to understand what’s going on in long COVID; (n=30).
JAK 1 / 2 Inhibitor
- REVERSE LC – Baricitinib may help with inflammation, neuroinflammation, and blood vessel functioning; (n=500).
Blood Filtration (Apheresis)
- Seraph 100 – apheresis filtration trial attempting to remove pathogens (viruses, bacteria), toxins, and pro-inflammatory cytokines (e.g., IL-6, IP-10) from the blood using heparin; (n=100).
Other Immune
The REVITALIZE Trial – a major effort by a non-profit that will start with upadacitinib (Rinvoq) or pirfenidone and then add other drugs on as the trial progresses; one person with severe ME/CFS experienced an astounding recovery using Rinvoq n=348).
Learn more about the Schmidt Center and its long-COVID work.
- IVIG – RECOVER Initiative – finally a large IVIG trial! (This is part of RECOVER’s autonomic clinical trials, including Ivabradine; n=380). May help with many factors including autoimmunity, inflammation, immune modulation, viral clearance and neuroprotection.
- Selzentry® (maraviroc) plus Lipitor (atorvastatin)—Bruce Patterson is putting his money where his mouth is with a 32-week randomized, 252-patient, double-blind, placebo-controlled, multicenter study.
- Apabetalone is a bromodomain and extraterminal (BET) protein inhibitor that has dual antiviral and anti-inflammatory mechanisms, and may help with blood vessel functioning (n=200 people with long COVID and type II diabetes).
- Autologous stem cells – stem cells can modulate and even rebuild the immune system (n=20 and n=12).
- More UCSF trials! – More small trials have been promised by Michael Peluso to explore efficacy and try to understand what’s going on in long COVID
Metabolism and Mitochondria
- Rapamycin– an MTORC1 inhibitor is such an intriguing possibility. Rapamycin can improve mitochondrial functioning, regulate immune senescence, reduce inflammation, and rebalance the immune system. Anecdotal reports suggest it can be helpful in ME/CFS, and a recent journal article proposed that long COVID and ME/CFS are MTORC1 syndrome diseases. Two trials (Simmaron– n=150; Mt Sinai – Iwasaki and Putrino – size unknown).
- Bezisterim – a safe drug that may be able to reduce neuroinflammation, and help with metabolism (insulin sensitization), (n=208).
- Metformin – metformin has been shown to reduce the incidence of long COVID, may positively enhance metabolism, gut functioning, and have anti-inflammatory and antiviral effects. Two trials – one small (n=16) and one large (part of the REVIVE trial) (n=1,500).
- Dapagliflozin – could reduce inflammation and improve metabolism – currently used in type 2 diabetes (n=192).
Central Nervous System
- Amantadine, a dopaminergic, NMDA receptor antagonist, and mild antiviral, may help with fatigue and brain fog. Two trials (n=30 and n=60)
- Ivabradine – may be able to reduce heart rate and improve autonomic functioning trial (part of RECOVER autonomic clinical trials, including ivabradine; n=380). Plus another 250-person POTS/long-COVID trial
- Fluvoxamine Maleate 100 MG – an SSRI, fluvoxamine may help with ER stress, reduce inflammation and neuroinflammation, and protect the blood-brain barrier; part of REVIVE trial (n=1,500)
- Ketamine – may help with neuroinflammation and improve cellular energy production; n=20)
- DAOIB for the Treatment of Cognitive Impairment Induced by COVID-19 – an Open Trial (n=40); unknown drug
- RISE Project – Budesonide/Formoterol; Vitamin C combined with Coenzyme Q10 oral treatment; Montelukast tablets oral treatment; inhaled corticosteroid (budesonide) reduces airway and systemic inflammation. Montekulast may help with breathing, reduce neuroinflammation, and have antiviral effects (n=632).
Coagulation
- Lumbrokinase—an anticlotting and anti-platelet hyperactivation agent, lumbrokinase could reduce inflammation and improve blood flow. PolyBi- supported ME/CFS, long COVID, and Lyme study at Mt Sinai; size unknown.
Gut
- Larazotide (AT1001) – restores the barrier function of the intestinal lining and reduces abnormal permeability, often referred to as “leaky gut”; (n=48).
Conclusion
Yes, many big pharma companies are not embracing long COVID, but not all hope is lost. Investigators are clearly interested in long COVID, and clinical trials employing a surprisingly wide array of drugs are underway. Many of these are larger trials. Fourteen trials have over 100 participants, and ten have over 200 participants. Some trials could provide immediate validation of a drug and quickly lead to new treatments.






Thanks Cort! It’s actually quite a decent number of trials, far far more than we ever had with ME/CFS. Here’s hoping. It gives me at least a bit of hope.
You mention in the article that Nancy Klimas has had great results with long covid patients. ‘Great results’ sounds almost too good to be true. If so…. What is she using, and what are next steps?
Actually, ‘remarkable results’!