

Two studies suggest as many as 75% of people with chronic fatigue syndrome experience migraines and that most migraines in ME/CFS are undiagnosed. Agreeing that migraines are common in ME/CFS, WebMD, which has very little to say otherwise about chronic fatigue syndrome, states ME/CFS is one of five disorders with high migraine rates.
Consider, as you read the similarities between ME/CFS/FM and migraine below, that Rayhan and Baraniuk propose ME/CFS/FM patients may be in a kind of chronic migraine-like state.
Given the long list of migraine symptoms and the considerable overlap with ME/CFS symptoms (visual disturbances, sensitivity to light/sound, weakness, pins and needles, speech problems, nausea, vomiting, increased urination, etc) .the low diagnostic rates may not be surprising.
Besides symptoms and high rates of comorbidity, the relapsing remitting nature of both disorders, the problems with barometric pressure changes, some similar triggers (including exercise for some), similar central nervous system abnormalities, etc. make a possible connection between migraine and ME/CFS/FM an intriguing one.

As in chronic fatigue syndrome and fibromyalgia, more women than men have migraines. The disorders share several other commonalities.
Consider that about three times as many women as men get migraines. Consider that both migraines and ME/CFS symptoms are often substantially reduced during pregnancy. Consider that central nervous system hyperactivity plays a role in both conditions, that both feature blood vessel problems and inflammation is a key factor in both.
Consider that stress often plays a key role in triggering both migraines and symptoms in ME/CFS. Consider that during migraines and relapses in ME/CFS exertion and exposure to stimulit often must be curtailed dramatically. Whether in the midst of a ME/CFS crash or migraine attack hypersensitivity to lights, sounds and odors is common.
Asserting that similar central nervous system problems contribute to chronic fatigue syndrome, Gulf War Illness, fibromyalgia and migraine, Rayhan and Baraniuk propose triptans and other migraine treatments may be effective in people with these disorders who have and who do not have migraines.
Migraine Treatments
Diary
Interestingly, one of the first recommendations is to, just as in chronic fatigue syndrome (ME/CFS), compile a diary or chart, that helps you identify migraine (or in the case of ME/CFS, crashes) triggers.
Drugs
Most of the migraine drugs listed affect blood flows to the brain. With several studies documenting low brain blood flows in ME/CFS, and other studies documenting the possible consequences of low blood flows (increased lactate levels), drugs that affect brain blood flows may be a no-brainer in ME/CFS. In fact, several migraine drugs are used commonly in ME/CFS – not to treat migraines, but to reduce other symptoms. The big news in migraine treatment, though, is a new class of drug coming on the market in 2019.
The CGRP Antagonists
“For now, they (the new drugs) look fantastic. They shake the ground under our feet. They will change the way we treat migraine.” Dr. Stewart J. Tepper, a professor of neurology at Dartmouth College
Clinical trials suggest that CGRP antagonists will be much more effective than past migraine drugs. Drug companies are charging the migraine market en masse with three CGRP antagonists (erenaumab: (Aimovig) ; galcanezumab: Emgality; fremanezumab (Ajovy)) approved in 2018 and two more (Allergen – ubrogepant; Biohaven – rimegepant) expected to be submitted for FDA approval over the next couple of years.
The Migraine Drug Explosion Begins: Could Fibromyalgia and ME/CFS Benefit?
Triptans
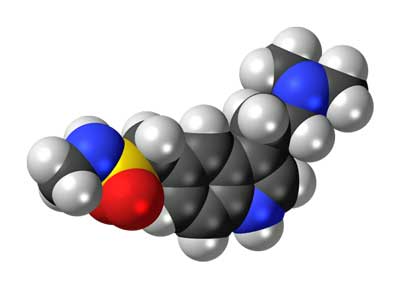
Triptans include sumatriptan (Imitrex, Imigran, Cinie, Illument, Migriptan), rizatriptan (Maxalt), naratriptan (Amerge, Naramig), zolmitriptan (Zomig), eletriptan (Relpax), almotriptan (Axert, Almogran), frovatriptan (Frova, Migard, Frovamig), and avitriptan (BMS-180,048). Triptans are definitely not on the list commonly used ME/CFS drugs but Baraniuk et. al. specifically referred to them in their study.
Sumatriptan or Imitrex is commonly used to stop migraine attacks…Could it help with ME/CFS crashes as well?
Sumatriptan reduces inflammation in the arteries and veins in the brain by enhancing 5-HT (serotonin) production which causes the over-dilated veins to constrict. Sumatriptan also deceases the activity of nerves called the trigeminal nerves that are associated with cluster headaches. Interestingly, some research suggests triptans may be affecting the periphery (the body) more than the brain. Triptans’ difficulty passing the blood-brain barrier has stimulated research into its effects elsewhere. Studies suggest triptans ability to reduce pain-producing peptides such as substance P in the periphery may block pain signals to the brain.
Beta Blockers
Used to prevent migraines, beta blockers dilate blood vessels, allowing more blood flow to the brain. Migraines appear to be accompanied by a process called ‘cortical spreading depression’ in which low blood flows to the brain cause an over dilation of the blood vessels or vice versa. Beta blockers may help prevent situations in which low blood flows to the brain occur. Propanolol – has shown to be effective in reducing orthostatic intolerance and fatigue in some ME/CFS patients
Calcium Channel Blockers
By blocking serotonin in the blood vessels, calcium blockers stop the blood vessels from constricting. Since serotonin also reduces pain tolerance, calcium blockers can reduce pain as well. Verapamil, Diltiazem and Nimodipine are three calcium blockers used sometimes in migraine. Low dose Nimodopine plays a key role in Dr. Katherine Downing-Orr’s treatment protocol for ME/CFS.
Topomax
Topamax – an anticonvulsant sometimes used in ME/CFS – can be successful if the side effects which can be substantial – can be avoided.
Dr. Bateman states: “Topamax (topiramate)…. must be dosed very carefully to avoid common debilitating side effects (e.g., fatigue, nausea, diarrhea, trouble concentrating). Start low (12.5 mg) and build very gradually (12.5 mg every one to two weeks), with the largest dose at night and little or none in the morning. Topamax may control the migraines, get your patient sleeping, and work as a mild pain modulator to minimize the FM during the day.”
Ergotamines
Ergotamines are drugs derived from the fungus ergot, which combined with caffeine, narrow the blood vessels. Migranal, cafergot and DH-405 are three ergotamine drugs used to treatment migraines.
Alternative Remedies
Nutrients and Herbs
Many herbs and nutrients have been used to treat migraines. Some (Vit. D, magnesium, fish oil, coenzyme Q10, gingko biloba, valerian) are used in chronic fatigue syndrome but others (peppermint oil, petadolex, feverfew, butterburr, migrelief) and others many not. Check out this page for information on nutrients and herbs used to treat migraines.
Dr. Teitelbaum emphasized petadolex, Vit B-2, magnesium IV’s, COQ10, excedrin for migraine (as effective as Imitrex) and others in his video.
Dr. Teitelbaum on Treating Migraine Naturally
Mind/Body
Yoga, meditation, tai chi, hynoptherapy, cognitive behavioral therapy, biofeedback and others are used to reduce stress and avoid migraines.





