 Trazodone (Desyrel) is…
Trazodone (Desyrel) is…
a drug that was produced for use as an antidepressant drug but which is almost always used in its low dose formulation as a sleep aid in chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM). In fact, low-dose trazodone is reportedly the second most commonly used sleep aid used in the U.S. for insomnia.
Arousal Combatter – Trazodone is mostly known as a serotonin antagonist and reuptake inhibitor (SSRI). By inhibiting the reuptake of serotonin and blocking the histamine and alpha-1-adrenergic receptors, trazodone reduces levels of neurotransmitters (serotonin, noradrenaline, dopamine, acetylcholine, and histamine) that are associated with arousal. That’s potentially an important asset for people with ME/CFS/FM whose sleep gets disrupted by the arousal of the HPA axis. Trazodone is classified as a “weak histamine antagonist” but its histamine blocking effects could conceivably be helpful in people with mast cell activation syndrome (MCAS).
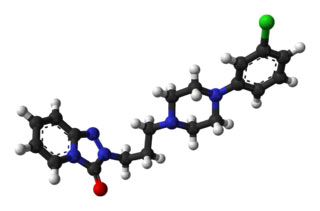
Neuroinflammation Reducer? Trazodone may have an unexpected trip up its sleeve. Trazodone is a triazolopyridine derivative that is structurally more closely related to other triazolopyridine-derived drugs than the drugs that make up major classes of antidepressants. Trazodone’s unusual structure prompted lead Italian researchers to check out what impact it was having on neurons in the central nervous system.
Adding trazodone to human astrocytes (brain neurons) prior to subjecting them to an inflammatory trigger stopped the effects of a powerful pro-inflammatory cytokine called TNF-a in its tracks and reduced the activity or expression of other pro-inflammatory cytokines. It also protected nerve cells from damage due to neurotoxicity apparently by activating 5-HT1A receptors and blocking 5-HT2A/C serotonin receptors.
This finding jives with findings indicating that inflammation triggers depression in some people and that some antidepressants may be reducing neuroinflammation. Trazodone may also be helpful with erectile dysfunction.
Trazodone and Sleep
Mathew Walker has inveighed against the use of sleep drugs because he reports that they don’t improve sleep architecture and are associated with detrimental long-term effects. A recent review of trazodone (and other antidepressants as well as anticonvulsants and antipsychotics) reported that it and the other drugs had “a beneficial effect on sleep architecture” but may suppress REM sleep.
A 2021 review reported that trazodone is less effective than hypnotics in treating sleep-onset insomnia (i.e., the inability to fall asleep) and when used for this purpose should be taken at least an hour before going to sleep. On the other hand, it is “very effective” in treating “sleep-maintenance” insomnia; i.e. insomnia that occurs later in the night or morning. It also reported that Trazodone increases the”duration of deep sleep, which is associated with better sleep quality as assessed by patients”.
Trazodone may also enhance the benefits of mindfulness practices such as cognitive-behavioral therapy (CBT) in some people. A small 2008 study found that while CBT improved sleep time and latency (the ability to fall asleep quickly) that CBT plus trazodone resulted in a further increase in the restorative period of deep, slow-wave sleep in people with depression.
Twelve years later, another small study reported that trazodone was more effective than CBT-I in people who exhibit “physiological hyperarousal (ie, activation of the stress system)” during sleep. Trazodone appears to be achieving this by reducing night-time cortisol levels. (Doxepin elixir – another sleep aid often used in ME/CFS and FM appears to do the same thing.).
Doxepin Elixir (Sinequan, Silenor) for ME/CFS and Fibromyalgia
Studies suggest that trazodone is able to effectively reduce cortisol levels during sleep, thus calming the central nervous system down and resulting in longer sleep times, increased deep sleep, and better sleep quality.
One review suggested trazodone might be helpful in combatting the side effects of SSRIs.
Trazodone Studies in Chronic Fatigue Syndrome and Fibromyalgia
A 2011 open-label FM study found that trazodone markedly improved sleep quality, sleep duration, and sleep efficiency, and also had moderate effects on other symptoms such as anxiety and depression scores and pain interference with daily activities. The authors called the improvement of sleep quality ‘striking’.
Another 2011 open-label FM study by the same group found that trazodone helped with “global fibromyalgia severity, sleep quality, and depression, as well as pain interference with daily activities”. When Lyrica (pregabalin) was added further improvement improvements in morning stiffness, pain (body pain and pain severity), and anxiety.
An interesting placebo-controlled 2018 study found that in Vit. D-deficient fibromyalgia patients’ trazodone (25 mg) given at bedtime + vitamin D 50 000 IU weekly significantly improved pain and sleep scores.
In 2016 Biovista, a drug repurposing company engaged to find a drug combination that might work for ME/CFS, proposed that trazodone plus low-dose naltrexone should get tested in ME/CFS.
Low Dose Naltrexone Drug Combination Proposed for Chronic Fatigue Syndrome (ME/CFS)
Chronic Fatigue Syndrome (ME/CFS) Doctor’s Report
The IACFS/ME Treatment Primer states trazodone ‘may be the least likely to lose effectiveness over time in ME/CFS. Dr. Lapp reports that he has ‘excellent luck’ with trazodone and Dr. Bell states that “Trazodone is one of my most favorite medications for sleep. “Trazodone doesn’t cause dry mouth or stimulate the appetite (no weight gain) and puts you into deep stage three or four sleep”. Since it works best in the early morning hours it is a good medication for those who wake early and can’t get back to sleep. It also helps with anxiety.
On their Unraveled Patreon podcast #18 in their series, Dr. Ruhoy and Dr. Kaufman both reported that trazodone was their go-to drug for sleep.
Dosage
Dr. Bell starts at 25 mg. (taken ½-2 hours before sleep) and works his way up (50-150mg.). Dr. Lapp recommends 50 mg. Dr. Bell states it should be taken approximately one-half hour to two hours prior to going to bed. A Spanish FM study suggested that low doses can effectively enhance sleep but that higher doses are needed to affect depression and FM symptoms.
Side Effects
Tachycardia was experienced by 32% of patients and was the most common reason for discontinuing trazodone in the Spanish FM study, leaving the authors to suggest that autonomic nervous system abnormalities in FM may leave some patients more susceptible to tachycardia.




