

Lactate has become a big deal in both chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM). A by-product of anaerobic energy metabolism, lactate ordinarily gets pumped out of our cells in large amounts during exertion. The lactate findings suggest that the energy needs of ME/CFS/FM patients are largely being addressed by glycolysis or anaerobic energy production. Anaerobic energy production plays an important role in energy production, but when aerobic energy production is not available and it becomes the major source of energy it produces metabolites that produce the burning muscles, fatigue and other symptoms we associate with over-exercise.

Lactate is ordinarily associated with over-exercise but high levels are present even in under-active ME/CFS and FM patients
That makes it all the more shocking and puzzling to find high lactate levels in two diseases in which exercise is often hardly tolerated. That suggests that something is profoundly off with ME/CFS and possibly FM patients’ energy productions systems. The fact that increased lactate levels have been found in several different compartments of the body in these diseases only sharpens the interest.
We mostly focus on lactate in the muscles and blood, but high lactate levels have also been found in the brains of people with chronic fatigue syndrome (ME/CFS). Over the past ten years Dr. Shungu and Dr. Natelson have documented large lactate increases in the ventricles in the brains of ME/CFS patients. They’ve also found large decreases in brain glutathione levels as well. In their latest study, they went a step further and examined lactate levels in the brains of FM patients as well.
Ventricular Lactate and the Cerebrospinal Fluid
When Shungu and Dr. Natelson refer to ventricular lactate, they’re also referring to the cerebral spinal fluid – a “tissue” that is becoming increasing important in ME/CFS and FM. The ventricles are four cavities sitting at the bottom of the brain where the cerebral spinal fluid (CSF) is produced. The CSF functions as a kind of cushion, a blood flow and neuro-endocrine-immune regulator and as an important waste removal outlet.
Analyzing the cerebral spinal fluid is the closest we can get to the brain short of a biopsy. CSF studies are able to uncover several different kinds of pathologies associated with the brain including bleeding, infection, inflammation and autoimmunity. Protein analyses of CSF have identified unique protein signatures for multiple sclerosis, lupus and other diseases.
Cerebral spinal fluid studies are also beginning to unlock what’s going on in ME/CFS/FM. CSF studies from the Simmaron Research Foundation and the Center for Infection and Immunity uncovered a pattern of immune upregulation / exhaustion and identified an atypical ME/CFS subset. Other CSF studies found a different protein signature in ME/CFS vs. Lyme disease and evidence of increased intracranial pressure in ME/CFS. Low levels of glutathione suggest the brain’s antioxidant defenses are down.
- Pressure Building? Study Suggests Cerebral Spinal Fluid Pressure May Be Causing Problems in Chronic Fatigue Syndrome
- Simmaron’s Spinal Fluid Study Finds Dramatic Differences in Chronic Fatigue Syndrome
- Peterson’s Atypical Subset Opens New View of ME/CFS in Columbia/Simmaron Publication
This study examined the makeup of CSF – aka the brain ventricles – in ME/CFS, FM, and healthy controls
The Study
Elevations of ventricular lactate levels occur in both chronic fatigue syndrome and fibromyalgia. Benjamin H.Natelsona, DianaVua, JeremyD.Coplanb, XianglingMaoc, MichelleBlatea, Guoxin Kangc, Eli Sotod*, Tolga Kapusuzd and Dikoma C. Shungu. FATIGUE: BIOMEDICINE, HEALTH & BEHAVIOR, 2017 http://dx.doi.org/10.1080/21641846.2017.1280114
Four studies have found increased lactate in fibromyalgia, and three studies have found it elevated in ME/CFS patients’ brains. This study used an H MRS I scan to examine lactate levels in 74 ME/CFS, ME/CFS + FM, FM and healthy controls’ brains.
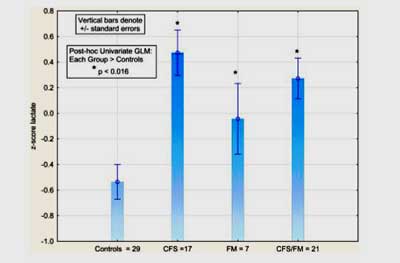
Lactate levels were greatly increased in the ventricles of ME/CFS, ME/CFS+FM and FM patients relative to healthy controls.
It found highly increased levels of lactate in the brains of chronic fatigue syndrome (ME/CFS), fibromyalgia, and ME/CFS+FM patients.
This means increased lactate levels may be one of the few abnormal findings present in both ME/CFS and FM. In fact, the authors – two longtime ME/CFS/FM researchers – believe lactate elevations are likely to be a core part of both syndromes. Further study is needed, but this could be the tie that binds the two disorders together.
I asked the senior author of the study, Dr. Shungu, how he got interested in lactate and ME/CFS/FM in the first place.
It turned out that he got drawn into ME/CFS research in the most backdoor way impossible. Fascinated by some brain scans he’d been asked to analyze that were suggestive of mitochondrial disease, he asked who they were from. It was only then that he found out they had chronic fatigue syndrome (ME/CFS) and had come from Paul Cheney MD. So began a decade-plus journey with ME/CFS – one which has yielded important insights.
“As with many, if not most, scientific endeavors, it was serendipity, and it also intertwines with how I got started in this area of research. My interest in ME/CFS research first emerged out of nowhere in 2002 after I had the opportunity to conduct diagnostic (as opposed to research) brain MRI/MRS evaluations and “metabolic workup” in patients with ME/CFS, who turned out to be patients of Dr. Paul Cheney (I did not know who he was at time and I had never heard of ME/CFS).
The results of that fairly routine clinical brain MRI/MRS scan piqued my interest because – and here are the answers to your ‘how?’ and ‘why?’ questions above – they revealed elevations of ventricular lactate similar to those that we had observed in patients with primary mitochondrial disorders, which I was investigating at the time as a Radiology faculty member at Columbia University Medical Center.”
Those increased lactate levels are basically synonymous with mitochondrial dysfunction…
We have found elevated ventricular lactate in nearly every disorder in which mitochondrial dysfunction has been implicated. These include primary mitochondrial disorders that I am still investigating with researchers at Columbia [Kaufmann et al 2004, Weiduschat et al 2014], Parkinson’s disease, lysosomal storage diseases, etc. We also recently reported increased ventricular lactate in FM, as well.
Shungu’s next steps revealed just how important small pilot studies funded by organizations like the Solve ME/CFS Initiative (SMCI), the Open Medicine Foundation and the Simmaron Research Foundation can be. Three seed grants from the SMCI kept his work going…
Greatly intrigued, I decided to find out more about ME/CFS, and I then teamed up, first with Dr. Susan Levine, and then with Dr. Benjamin Natelson, to apply (successfully) for three successive “seed” grants from the CFIDS Association of America (now Solve ME/CFS Initiative) to investigate, using brain MRI/MRS, whether mitochondrial dysfunction was responsible for the elevations of ventricular lactate that we’d observed in ME/CFS [Mathew et al 2009, Murrough et al 2010, Shungu et al 2012].
Shungu was then able to turn the pilot data gained into grants totaling almost $2 million. That’s a great return on investment for people who donated to the cause. That return on investment continues to build: Shungu has produced a comprehensive hypothesis on how ME/CFS begins and is maintained, and is submitting further grant proposals.
With these preliminary data and new evidence, which consisted of a robust 36% deficit of cortical glutathione (GSH) – the most abundant and primary antioxidant in living tissue – in ME/CFS compared to controls, we competed for NIH funding and were awarded two grants, descriptively titled, “Specificity and Validity of Oxidative Stress Model of Chronic Fatigue Syndrome” (R01 MH100005) and “[N-acetylcysteine] NAC for Treatment of Oxidative Stress in Chronic Fatigue Syndrome” (R21 NR013650).
Oxidative Stress
The Gist
- Lactate a by-product of anaerobic metabolism – which causes fatigue, pain and other symptoms, has been found in FM and ME/CFS
- Dr. Shungu and Natelson have found increased lactate levels in the brains of ME/CFS or FM patients in four studies
- Dr. Shungu became interest in ME/CFS when brain scans from Dr. Cheney’s patients suggested they had a mitochondrial disorder
- Dr. Shungu’s subsequent findings, which included finding low levels of the main antioxidant in the brain (glutathione) in ME/CFS patients, suggested that neuroinflammation and oxidative stress are the key culprits in ME/CFS and/or FM
- Shungu believes an antioxidant poor environment allows an infection to trigger a free radical explosion which shuts down the blood vessels causing a hypoxic – low oxygen environment – in the brain.
- That low oxygen environment results in an emphasis on anaerobic energy production (lactate), the conversion of pyruvate to lactate, and possibly mitochondrial problems.
- Shungu’s next step is an exercise/brain imaging study to assess energy production and a PET scan study to determine if neuroinflammation is present.
- A combination of treatments will likely be necessary to address the issues in ME/CFS/FM
Rather than directly implicating mitochondrial dysfunction, the three studies culminated with strong evidence supporting oxidative stress and associated pathophysiological consequences as the most likely neurobiological underpinnings of the observed elevations of ventricular lactate in ME/CFS [Shungu et al 2012].
Shungu’s last NIH funded (2013-2017) grant examined oxidative stress levels in the blood, urine and cerebral spinal fluid and determined if increased levels were synonymous with increased symptoms and reduced functionality. That study is finished and its results buttressed Shungu’s view that oxidative stress is a major component of ME/CFS/FM.
Both studies have now been completed and they have solidified our view that oxidative stress is a major player in ME/CFS etiopathogenesis. Shungu.
Shungu believes that free radicals are squeezing the blood vessels, causing low blood flows, lactate production and mitochondrial dysfunction
Why does Shungu believe mitochondria dysfunction is probably secondary in ME/CFS? Because he’s not seeing alterations in the levels of brain ATP and other phosphates, or reduced levels of NAA. The one proviso is that he’s been studying patients at rest. Next he plans to combine an exercise challenge with an MRS brain scan to determine if energy replenishment is occurring normally. Only then will he know for sure if the mitochondrial problems are primary or secondary.
For now, Shungu is focusing heavily on an oxidative stress model. High levels of free radicals that can chew up and blast cells – and even affect blood vessel functioning – have been found several times in ME/CFS and FM.
Oxidative stress itself is a normal part of cellular functioning. During the process of aerobic energy production, the mitochondria produce enormous amounts of free radicals, and immune cells use free radicals to kill pathogens as well. Too much oxidative stress, however, can damage the mitochondria and impair cellular functioning. Shungu’s finding of highly reduced levels of glutathione in the brains of ME/CFS patients suggested that the antioxidant systems that normally keep oxidative stress in the brain in check were not doing so any more.
High levels of isoprostanes in two (ME/CFS) studies, including one of Shungu’s (unpublished) provided an important early clue for Shungu. Isoprostanes are turning out to be major players in both cardiovascular and neurological diseases.
Shungu’s model – which builds on Martin Pall’s ME/CFS NO/ONOO model – goes something like this:
- An immunological trigger or pathogen triggers the production of pro-inflammatory cytokines and the potent free radical peroxynitrite.
- Inadequate antioxidant reserves result in peroxynitrite reacting with lipids to form isoprostanes.
- Isoprostanes – potent vasoconstrictors – compress the blood vessels, reducing blood flow, and producing an hypoxic or low oxygen environment.
- That low oxygen environment: (a) results in increased anaerobic energy production (glycolysis); and (b) promotes the transformation of pyruvate into lactate – hence, the high lactate levels found in the brain.
Shungu believes mitochondrial dysfunction is present in ME/CFS; he just doesn’t believe it’s the driver of the disease.
I believe that mitochondrial dysfunction is present in ME/CFS. It’s just that it is not a driver of the disease (i.e., not pathogenic), and it is fairly mild under resting conditions. The way mitochondrial dysfunction likely becomes more manifest in ME/CFS is when symptoms are provoked and de novo energy production is required…
It’s not that the mitochondria are not involved – they are – but the mitochondrial problems are secondary to the neuroinflammation and oxidative stress that’s present. The general outlines of Shungu’s model don’t appear to be that far from Naviaux’s, Davis’s and Fluge and Mella’s findings suggesting that something in the blood is turning off the mitochondria in the cells, and affecting the blood vessels and blood flows at the same time. That something for Shungu is oxidative stress and neuroninflammation.
“… mitochondria are incapacitated by the primary lesions (oxidative stress, neuroinflammation) in the disorder, leading to ineffective replenishment of cellular energy. Shungu
Once the process starts, it can be hard to tell what is causing what as the mitochondrial and oxidative stress problems feed into each other:
In our study of primary mitochondrial disorders (e.g., MELAS), we have found a cortical GSH deficit that seems to be even bigger than in ME/CFS, meaning that mitochondrial dysfunction and oxidative stress co-exist and likely potentiate and sustain each other in such disorders.
Fibromyalgia – A Neuroinflammation Disorder?
At least three possible mechanisms could explain the increased lactate levels seen in FM: problems with anaerobic energy production/mitochondrial dysfunction, neuroinflammation and oxidative stress. Again, note that none of them are exclusive of each other. Oxidative stress can whack the mitochondria and cause neuroninflammation. Neuroinflammation, on the other hand, is a really potent oxidative stress inducer. The question is where does it all begin?
Right now Shungu’s betting on the neuroinflammation option for fibromyalgia, but believes oxidative stress, neuroinflammation and mitochondrial dysfunction are all “co-conspirators” in producing ME/CFS, FM and other diseases.
I think that you are right in suggesting that pain and increased ventricular lactate in FM may have a different mechanistic underpinning (than in ME/CFS) and a strong candidate is neuroinflammation.
Personally, and this is the next phase of our research, I believe that oxidative stress and neuroinflammation, and possibly a secondary mitochondrial dysfunction, may all be ‘co-conspirators’ in the etiology of most of these unexplained and highly overlapping and related multisystem/multisymptom diseases like ME/CFS, FM, Gulf War, IBS, etc.
One of his earlier studies found that Savella (milnacipran) significantly reduced FM patients’ pain as well as their ventricular lactate levels. Despite those reductions, the FM patients’ lactate and pain levels were still higher than in the healthy controls. That suggested that further reductions in ventricular lactate levels might be able to reduce pain levels even more. I asked him about that.
It was clear that Savella can only go so far in FM. Might other drugs or classes of drugs or other substances do better in reducing brain lactate levels? He suggested that it wasn’t going to be as easy as that.
This suggests that a single drug that targets ventricular lactate may not be effective because it would be targeting a consequence rather than the cause of the disease. This also suggests that a ‘drug cocktail’ that targets the complex etiologic factors of these disorders may be more effective than a single drug. Thus, combining N-acetylcysteine (NAC) to elevate brain glutathione levels and alleviate oxidative stress, with, e.g., a nonsteroid anti-inflammatory drug (NSAID) to target inflammation might be more effective than either intervention alone.
(Dr. Shungu’s NAC trial had positive results. We are awaiting publication.)
As for a drug that might be more effective at reducing lactate, we did conduct a clinical trial of precisely such a drug – dichloroacetate or DCA – in patients with the syndrome of Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-like episodes (MELAS), a primary mitochondrial disorder with gallons of ventricular lactate. However, we had to abort the trial because we found DCA to induce toxic neuropathy in MELAS patients [Kaufmann et al 2006]. Perhaps DCA would be safer in patients with milder lactate elevations, which ME/CFS and FM have in comparison to MELAS.
While Shungu is pointing at a different or at least an additional cause of the high lactate levels he’s found, it’s important to note that the same endpoint has shown up again and again:
With regards to the single syndrome hypothesis: could the general finding of increased lactate in the ventricles of ME/CFS and FM point to a similar neuroinflammatory state in ME/CFS and FM which is expressed slightly differently – producing more fatigue in one disease and more pain in the other?
We have done so little research in neuroinflammation and the data on it in ME/CFS or FM is so discrepant that it is tough to speculate. So, I will have to ask you to stay tuned, because we now have a proposal pending to combine MRS with positron emission tomography (PET), the “gold standard” approach for measuring neuroinflammation, to extend our oxidative stress model of ME/CFS (also applicable to related multisymptom disorders) upstream to try to obtain empirical evidence supporting neuroinflammation as the “missing mechanistic link” between oxidative stress and ME/CFS etiopathogenic factors like systemic immune dysfunction.
- Check out Dr. Pall’s treatment recommendations for breaking the peroxynitrite cycle.
Conclusion
The most important takeaway from this study and from Shungu’s and Natelson work is that the same central finding – an overemphasis on anaerobic energy production- is showing up in both ME/CFS and FM, and it appears to be showing up across the body.
What’s causing the problem is almost secondary at this point. The biggest issue in ME/CFS research has been identifying the core problem present. If it’s true that problems with energy production are that core issue, then what’s left is the working out of why and how it showed up and how to fix it. That’s a much easier task than finding the core problem and one that the NIH and others should find much easier to fund.








Please forgive me for dissenting but are you seriously suggesting that “What’s causing the problem is secondary?” In my opinion, it’s everything. But that would fly in the face of how medicine works in this country. The goal for the medical establishment seems to be to find a drug that will mask symptoms, not get to the bottom of the problem, and goodness forbid, heal a person. You guys are running in all the wrong directions. Stop looking for drugs! Find the cause!!!!! Start with looking for toxins in our everyday lives.
:)… I knew this would get people but I am absolutely sincere that thebest thing that could happen in FM and ME/CFS is to identify the core problem: once that is identified everything changes: a clear pathway presents itself and ME/CFS, in particular, changes from being this kind of complicated mess of a disease that most researchers don’t want to touch to being something they can work on. Resources will really show up then.
I don’t think there is consensus that the core problem is energy production problems but resources are getting thrown at that problem including studies that are examining whether energy problems are afflicting immune cells.
Toxins, for instance, might I suppose become a possibility if the core problem is oxidative stress initiated energy problems but they get hardly a nod unless they can become linked to the core problem. (How much toxin research do you see in ME/CFS/FM right now?) Eliminating toxins in our environment is almost akin to masking the symptoms; the problem is still there. We need to find out why toxins are doing what they are doing. As someone with chemical sensitivities I would love to know that.
Yes, doctors may be trying to mask symptoms with drugs but researchers like Shungu, Ron Davis, Bog Naviaux, Zaher Nahle, Chris Armstrong, Patrick McGowan, Derya Unutmaz and others are trying to get at the core problems in these diseases.
‘Eliminating toxins is never going to do it.’ Why? The reason I ask is that I have been trying to decide whether or not to pay out all that money to see if a far-infrared sauna blanket would work for me. Your statement above makes me think it would be a waste of money while the article had me thinking it may be worthwhile.
(I hate making decisions!)
Sorry about that. Actually my personal experience is that eliminating toxins is a good idea but the best answer to the disease IMO is finding out why even small amounts of toxins are so harmful for some people. Then hopefully you can reverse the whole thing and not worry about toxins. Good luck with the infrared sauna blanket should you try it.
The research by Innovative Med Concepts suggests that the fibromyalgia and MECFS population may suffer from an abnormal “ongoing” stress response. This continuous “flight or fight” response over time could produce this exact increase in serum and CNS lactate levels. Knowing what creates the abnormal stress response and turning it OFF is what is needed to reverse the systemic changes seen in FM and MECFS.
Thanks very much Dr. Pridgen for that insight. Personally, I would be shocked if an ongoing stress response wasn’t present in these diseases.
You can find the latest update on Dr. Dr. Pridgen’s antiviral trial for fibromyalgia here – http://simmaronresearch.com/2017/03/valley-death-fibromyalgia-pridgen/
Diane, I tried to reply to you below your comment, but it came out below the next one.
I understand your feeling, but the line is actually “almost” secondary, with the following sentence clarifying the need to the discover cause and etiology (why and how). Nowhere does anyone mention the development of drugs as a priority. I agree that the medical world here in the US often offer treatments to mask symptoms, but there are patients who demand that: “I just want to feel better.” I think every step toward identifying the core problem is deeply significant.
Diane, even if eliminating toxins doesn’t get to the core cause, it is absolutely going to be beneficial for so many things. The total load that anyone’s body has to deal with impairs so many functions & also causes a lot of reactions, even for people who don’t have multiple chemical sensitivities or impaired methlyation & don’t even realize they are being affected. That said, I wouldn’t use a far-infared sauna blanket to try to get rid of toxins. The materials the blankets are made of are toxic themselves, and for many people, the use of electric-powered things on the body (like electric blankets & heating pads) also has an effect similar to other toxins.
There are some inexpensive & safe supplements that can help eliminate a lot of toxins. Bentonite clay & charcoal are a couple of these. The only thing to be aware of if you try using them is that they can also absorb nutrients, so you should take them a few hours apart from when you take any other supplements or meds (if you take any).
Dr. Katrina It doesn’t seem like you have actually done YOUR homework. Those of us who have tried just about everything, including our personal studies, and have seen every specialist and at least 2 in every specialty in each group, trying to find some kind of answer, including the CAUSE. Don’t you think we want to know the CAUSE? There comes a time that you just have to have some sort of band aide for this condition just so we can work and do the basics. I remember talking to my PCP over and over about CFS and also pain, her response was “even if you do have CFS there’s nothing you can do about it” wonderful!! Trying to work and take care of your family, yeah, right! I take issue that it is toxins that can do this to us because “I” out of all the people I worked with in the health dept. nurses and all, was the only one who prepared my food, my self, with all the fresh foods you can think of. I carried my lunch EVERY day in contrast to the rest of the staff that ate out, and also ate processed foods,(hot pockets) smoked and certainly did not have a toxic free life. I did not smoke or drink alcohol.One of my co-workers was very over weight and ate anything that didn’t eat her first, and she was just one of these people, but she had energy to burn, had big weekends (fun).On the other hand all I could think of was finding my way to the bed, could barely get thru with my obligations at at home, let alone any kind of fun like hiking, canoeing, my art, and just enjoy my family. I am 67 at this point and this has been cardinal in my life. I have missed so much in my life because of this, right down to funerals of my own family.We live out in the country and have fresh vegetables,
We use (which I happen to like) no sprays of any kind, and I also tried to work out on a regular bases, until I crash, this is mild exercise. I have looked at everything for over 15 yrs. and tried it all, to no avail.It drives me crazy when people speak with authority on subjects they really don’t know anything about. None-the-less a doctor, which most of us have seen many, many doctors, with just a shrug and comment”well I don’t really know.” I don’t even expect doctors to know or understand this stuff, there’s just not enough information and study about it, but please don’t dismiss the information we offer when you haven’t done your own study, it’s a slap in the face for us that have suffered so many yrs. along with guilt that we just can’t keep up. We have always (a least in the beginning)trusted our doctors to know what’s best, and their knowledge, then to have a doctor to say something like this, It really goes against doctors in general. It would be BETTER just to say “I just don’t know”. To any of you struggling with this, at this point (don’t know the cause) my band aide is Vyvanse, and pain mgnt. Which, is the best I can do, and God bless my new PCP that has prescribed this for me, who also has fibro her self.
I think you are right. I am sure that all sorts of fascinating malfunctions in neurological and metabolic channels could be found in the systems of victims incarcerated and tortured over long periods of time by evil regimes around the world, but discovering these and inventing drugs to suppress some element at some stage of these dysfunctions would kinda miss the point about the external intrusions into the system, that are responsible for the malfunctions.
I agree with Dr Shungu’s vicious circle of effects, and the mystery of “which one started it”? But what if vasoconstriction (and the constriction of other vessels and nervous system signal carriers) is where this particular vicious circle begins, but the cause of this in the first place is external to this particular vicious circle? Eg as you say, toxins and dehydration. Starlanyl and others focusing on the myofascia, hypothesize that the ground substance becomes sticky from toxins and/or dehydration and starts to form “stuck” clumps of tissue at the level of the sarcomeres themselves. All the vessels that pass through the affected spot, are restricted.
The dehydration itself could be the result of the body trying to rid itself of toxins, I know my FM developed over the course of a couple of years of frustrating tendency to excessive urination that the doctors were unable to solve. I tried ever-increasing doses of electrolytes (I was athletic and did lots of exercise and used electrolytes anyway) but these just increased the urination.
2 frustrating decades later, hair mineral analysis testing showed I had high levels of cadmium. This toxin is very nasty because it tends to not show up in tests at all until the renal system is already saturated with deposits.
But as Cort and others know from my regular comments here, I discovered over the last 3 years that my condition is helped significantly by a low carb diet and plenty of low intensity exercise, deliberately avoiding anaerobic exertion, and building the aerobic threshold so that more activity is possible without activating the anaerobic mechanism. My hypothetical reasons for doing this, was that burning sugar for exercise produces “dirty” by-products while burning fat is “clean” – hence the diet as well as the carefully targeted exercise program. And those “dirty” byproducts could be one of the toxins that linger in muscle tissue, worsening the vicious circle with the myofascial ground substance stickiness as its source.
Taking lots of dietary sulphur may have helped get the cadmium flushing out, the levels in the HTMA have been falling, but due to the renal system saturation, it may take me years to “get better”, if I ever do “recover fully”. But I have made spectacular progress over the last 3 years, it is just that “the better I get, the worse I realise I WAS”.
I have been trying to work with my physical therapist to create an exercise program that will avoid anerobic and increase CV efficiency. We are trying to use monitoring HR and keeping that at or below 100 bpm during activity My resting HR is already 80bpm and minimal activity ( emptying the dishwasher, folding laundry jumps me up to 100. Climbing a flight of stairs i jump up tp 120! It is impossible for me to train thus way. How do you approach avoiding anerobic training?? I’m so frustrated!
This story might help – https://www.healthrising.org/blog/2013/08/13/heart-rate-monitor-program-improves-heart-functioning-in-chronic-fatigue-syndrome-mecfs/
Lorena, it is really interesting that you are on this track. I understand completely. It might be a nuisance to wear a heart rate monitor all day, but if you experiment with one, you can get a feel for the level of exertion that you can handle.
When an unavoidable routine is too much, the only solution is to slow it down. I spent a couple of years climbing stairs painfully SLOWLY. Hold the hand-rail, take one step at a time, use as energy-conserving a posture and gait as possible. Stop for breathers.
The key is to do a LOT of exercise and movement at the intensity you can handle. The more you keep this up, the quicker your threshold will rise. When I first thought this was worth trying, I dedicated 2 to 3 hours per day to it, my income suffered, but it was worth it. (I am self-employed).
After a couple of years, my aerobic threshold was so high, I was freaking out other people in the gym on static exercise machines, because I was maintaining the same power level as them but with a heart rate 30 beats per minute lower. But that was the limit of what I could do; I still can’t do what normal people can – dig really deep, go anaerobic and generate a lot of energy to achieve a result, then recover overnight. People like you and I do not recover overnight.
But I have regained the ability to do something I used to love to do 25 years ago, and lost – I participate in group bicycle rides, the real lycra-wearing type. I can keep up with some pretty fit people most of the time. But I have to just let them go when they decide to put on a burst of speed, and when it comes to riding uphill.
Now isn’t that something Phil! What an accomplishment and what an interesting thing. That certainly brings hope.
I personally think it is a mito issue.
Yes, someone needs to get at the core cause of these diseases, which unfortunately are still just called “ conditions” because no one knows their real causes.As a long time sufferer of FM, I have thought there must be metabolic issues involved, even though many experts say the fatigue is only caused by dealing with constant pain. If they experienced what we experience they would know that the pain and the fatigue are two very different symptoms. I have dealt with extreme pain before and it doesn’t cause the body to react with the kind of all encompassing, mind numbing fatigue that comes with FM. Toxins may or may not play a part, but I think genetic make up has more to do with it. If it was only toxins, then everyone in our day and age would be experiencing these symptoms. I look forward to more studies and results of this nature.
I can’t believe it!!! Don’t they realize, the brain is just a reflection of what is going on in the gut and colon! I have had CFS/MCS for over 20yrs and now know it was caused by having the drug FLAGYL, because I had a Gardia infection, which wiped out my good bacteria and I am working with Prof. Tom Borody, at the Centre for Digestive Diseases in Sydney, Australia. This man knows more than anyone I have ever been to,(he even had CFS ,so he really understands and got himself well with their treatment – A Feacal Microbal Transplant) Don’t all these doctors and researches realize, we have just had our good bacteria wiped out(which used to line our colon, and be protective barrier that stops toxins leaking into our organs and joints ), which in turn causes the aches and pains of FIBROMYALGIA. That is the real cause!!!!!!!!!!! It’s easier than they make out what is really wrong with us, it’s just the fixing it that is the problem. It all begins and ends in the GUT and COLON. Haven’t any of them read the GAPS Diet by Dr Natasha Campbell McBride or THE BODY ECOLOGY DIET by Donna Gates, it’s heals some CFS patients, but if it doesn’t (which was me) it’s because we have had to much damage done to our gut/colon but drugs/chemicals etc. I get so frustrated with all this research, they all want to make a pill, when it’s all about our GOOD BACTERIA, well, lack of it
Yes you are completely right – something in the body could be sending the brain and central nervous system into a tizzy! In fact the next blog in the series is going to suggest just that 🙂
If they find the cause how do you propose they treat it without drugs? Eating brocolli?
There are countless examples of drugs masking and minimising symptoms and helping people return to everyday life who would otherwise be bedridden. Often the cause cannot be treated. Drugs are to manage the cause are all there is.
Give me effective drugs that manage the cause of the disease so im not in pain, fatigued, severely senstive to light living in darkness. Ill take them.
Dear Luke, thank you for your sensible comment. Quinine was used to successfully treat malaria long before the cause was understood. Any effective drug that can treat the symptoms is to be welcomed, and I’m sure scientists will continue to try and find a cause.
I Concur
Dr that’s how western world work, we are not going to change that, what make them more money, the core underplaying cause of Me/cfs is a veryyy polémic issue, it’s obvious cfs is a chronic disease and they down played and missed Leaded for decades trying to cover up what???
Even now that it’s accepted as one of the more chronic disease on earth affecting soo many why they still funding soo little????
That show clearly they are trying to limit resources why?? To cover up what???
Every time a retrovirus surface something later happen then we go back to zero and the conspirancy theories..
But let’s not make of this a political debate cause won’t take us anywhere.
It’s obvious beyond any reasonable doubt that people with FM & Me/CFS have genetic changes, have altered many of the body funtions many path ways are disrupted , our gene expresión have been altered, as Dr Rawls call it body disruption, with this impaired and broken paths ways everything else becomes a problem , expousure to toxins, pathogens , microbios, obviously the most oportunist and aggressive ones causing mayor damage, like the ones we see the most in Cfs, EBV, HHV6, CMV, HSV-1, MYCOPLASMAS ,HEAVY METALS, MOLD ETC…
This are just co infections that will predict severity do to our broken system.
What’s causing the broken system the body disruption DNA changes has to be a pathogen capable of cutting into your DNA and changing they way your body function as a one nearly perfect machine, most likely a pathogen with reverse transcriptase enzyme , this allow the pathogen to change your body’s function turning the body into a broken one struggling to keep up with it functions .
I lost hope that the undelaying cause of me/cfs the pathogen will be expuse accepted by science as the main core cause of the illnesses, but as Cort Johnson once said “ some times you have to let go certain things to allow new ones to come, to open the door for new ones or we will stay there in the Dark forever.. just like we were
I agree….find the cause, not a drug.
Thanks, interesting info.
I wonder if upping NO would be effective as that dilate the veins and improves oxygen flow? L- Arginine comes to mind.
Issie
Hyperbaric chamber helped some people. They do improve oxygen flow. Looks that there is something to it.
Cort and Elvira, When I had cancer, 15 yrs ago, I thought that God had taken away the CFS/FMS so I could deal with the cancer. I took radiation then HBO therapy. I am not sure if the HBO made me feel healed or not; but I felt better than I did in 20 years. I have been cancer free for 15 years. Thank God.
Fortunate for me the Lord healed the cancer. When I went to MD Anderson, to get the cancer out, Dr. told me it was gone. It was not a misdiagnoses because I had 6 biopsies and 3 bouts of cancer in 2 years.
The CFS/FMS/EM is a lot worse than the cancer was with 13 surgical procedures. CFS is much worse. Also, I got rid of the cancer, the EM has been with me 33 years. There is finally hope with all this research
I found a juice only diet for a few days at a time reduced my neuroinflammation associated with fibromyalgia.
I know an Australian Journalist, Catherine Cashmore, who says the same about a “Fruitarian” diet and its effect on her FM. I have not tried this myself because low-carb has worked for me and I love my red meat. I have no idea why such disparate diets are both effective, it certainly does not fit my surmise that burning sugar for energy is more toxic for the muscles than burning fat, hence my improvement by depriving the muscles of sugar for fuel and forcing them to burn fat (ketosis).
Ime on number 50 oxygen therapy may help fatigue but not pain as yet
https://draxe.com/l-arginine/
Opens blood vessels, helps blood flow.
I agree, we need to get to “core” problem. Tell me WHY, and then I will decide if I want to mask it (with meds) or fix it (if that’s possible). We may can only put a “bandaid” on. But some things we consider “symptoms” may in fact be very necessary compensations. Masking a correction could prove very detrimental.
If we could “fix” our autoimmune system and get rid of inflammation – we would probably be as good as we can be. Genetics and Epigenetic may play a big role. But, it still comes down to a faulty regulation of our bodies detection systems.
Issie
I like it!
Can a substance dilate a blood vessel that is trapped in tight surrounding muscle tissue? This seems to me like using a radiator flush on a radiator where the problem is crushed coolant micro-tubes.
Possibly some improvement happens because part of the flow system is helped, but if the biggest part of the problem is external strangling of the vessel, can a vessel-dilating substance actually push back against this?
Here again, there can be MANY causes of this, but the antibiotic is not what’s caused my pain, which mine is caused by hyper mobility causing micro tears in muscle and tissue. Viruses and lord knows what else could be the cause of this problem. Good luck every body.
Looks promising
One of my early symptoms was diagnosed as pseudo tumor cerebri, an excess of spinal fluid, mine to the extent I lost a little vision in one eye. Ten + years later I still must control it with medication. I’m wondering if any other PWMEs have had this experience. When it was diagnosed there were only guesses as to its cause: hormone imbalance and excess weight were prime guesses. Ironically, besides medication, I got the greatest relief for the headaches etc from a 90 minute nuts nonstop vigorous walk…
I have pseudotumor also, and later a diagnosis of FM. I’ve always felt they were somehow related, and oxidative stress related, as my body is always in fight or flight. I’m also allergic to everything!
I was finally diagnosed with pseudotumor cerebri (intracranial hypertension) when I was in my mid to late 20’s, but was very symptomatic with it when I was 13 or 14. I also had a bout of mono?CFS? not sure what it was, but I was exhausted for weeks, unable to work, would be exhausted just trying to shower, get dressed/drive into work. Was in bed for weeks, but after about 8 weeks or so I recovered. This also happened in my mid to late 20’s. Fast forward to age 49 when I got mono, and my life came to a screeching halt. Never recovered from mono, and was eventually given the dx of ME/CFS by way of exclusion from anything else it might be. Never had an MRI to look for abnormalities, not sure if its something I should ask for or not. Just wondering if there could be some correlation between IH and ME/CFS. Some sort of damage done to internal brain structures, wondering if increased intracranial pressure could be the cause of inflammation which is what triggered my bodies reaction and subsequent development of ME/CFS.
Hey Cort, the link for New York letter to doctors is going to run for hIs son article:-)
Whoops! Thanks for letting me know 🙂
What is the problem with the modern alopatic medicine? Not just in the US. Ask any doctor or nurse. The first thing they learn at the school is that the role of medicine is not to cure, but to improve the quality of life of their patients. Finding the cause is not important?
??? Sorry, but that may be a message that some take home from their education, but I certainly don’t recall being taught that the role of medicine is “not to cure.” In fact, my observation is less attention is given to patients’ quality of life in favor of attempts to cure. Look at end of life cancer treatment, for example. All the emphasis tends to be on last ditch attempts to cure, with little attention to making those last weeks or months the most fulfilling for the patient.
Elvira, as far as ME, CFS, MCS, FM are concerned, the viewpoint of physicians is indeed that the conditions are in the psychiatric purview which makes many feel that all symptoms of the patients are to be addressed as not “curable” only “manageable”. It does marginalize patients and cuts them off from medical care. In the movie “Unrest” Jen Brea’s husband is at the Emerg dept with Jen and says to the camera, “You can’t tell them too much or they don’t help you and you can’t not tell them too little because they won’t know what’s happening at all.
I strongly dessagree, they may pretend it’s to core but in fact they don’t .
Every time there is a real success scientist that finds what it may become a cure eradicate the disease , something happen, either way miateriously dies, or something happen, especially if it’s something natural or unexpensive, that won’t make them huge profits.
It’s imposible that after sooooooo many years of study and research were you have an phone and a Siri that can nearly tell you anything you ask them, with so much technology it’s IMPOSIBLE that most of chronic illnesses around the world , cancer, ms, cfs, autism, fibro, diabetic… I mean you name it.. none have a cure or validated reversible cause .. sorry science is manipulated by the pharmaceutical industry and the globalist elite at their conviniance
Which definition of the non-existent condition ‘ME/CFS’? This information is useless without knowing what patients were selected. Use the correct terminology!
But Guido you just called ME/CFS non-existent…How can you have a definition of a non-existent condition? Maybe you can take some comfort from the fact that whether they had “ME/CFS”, ME/CFS + FM or FM they all had increased lactate levels – that suggests increased lactate levels are found across a wide swath of people with severe fatigue and/or pain symptoms.
How many people have heavy metals in there bodies. So many people have chelated (the correct way) and there fibro symptoms have dissapeared. Its time the establishment stopped pretending mercury in amalgam is a safe procedure . You want to know were you’re oxidative stress is coming from ,its right there . You want to know what affects your enzymes that control candida ,its right there. You want to know what affects you’re gut bacteria your ability to produce glutathione what triggers inflammation your bodies ability to detox ,suloxidation etc etc .In other words all of these studies only confirm the symptoms of the processes that are happening . The cause has to be environment. Some of those environments can be pin pointed (lyme , fluoroquinilones,diet ,mold and others)Most of those when pinpointed can be effectively treated , but the ones that don’t respond eventually heal once the heavy metals have been removed (correctly) Lead mercury etc are very common. The body has an ability to deal with these but everyones breaking point is different probably due to the influences the environment has had over time and the bodies ability to deal with it.
It’s that breaking point and why it’s happening that I assert we ultimately have to figure out. Until then detox away. Glutathione, which Shungu found to be reduced by about a third in ME/CFS patients, is the major antioxidant in the body.
Pinning the blame on the environment is ignoring the fact that most people are able to handle the toxins in the environment without getting a disease like ME/CFS. The best answer would be to explain what is happening in their bodies that doesn’t allow them to do that.
I use immunocal for 17 years to up glutathione. Have almost no pain with it. But immunocal can ialso increase inflammation. So it is a balancing act
What about stainless pins in legs etc
Nigel; I had all my mercury dental fillings removed years ago in an effort to be cured of fibro. Unfortunately, it didn’t help at all. The symptoms I’ve experienced with fibro are very similar to a reaction I had when given the Salk live polio vaccine back when it was first administered. Three of us became deathly ill. Two had to be hospitalized. I later learned the vaccine may have been contaminated. We received 3 en masse inoculations in quick succession at school. I am not against vaccines, but can’t help but think there may be a connection.
Hi I’m new to this forum and haven’t been keeping up with research as I have an EMF sensitivity including around computers. It was suggested by one local Dr. who studied and treated people with ME and FM, such as myself, that we have more sensitive nervous systems – pre illness – and as such, have a lower threshold for stress, trauma and toxins, etc. It seems to bear out with many people I know.
Also, if we’re low in Glutathione might it be helpful to take NAC (N’acetyl L-Cysteine), a precursor to the above to up the body’s antioxidant capacity? I had used it as recommended by Dr. Teresa Clarke (the above Dr.) and was amazed at all the crap that came out – including a month of exhaling chlorine fumes after forty years of being a long distance swimmer.
Welcome! NAC is what Dr. Shungu tried in ME/CFS patients. He reported that the results were good at a conference but I don’t think we’ve gotten the paper yet.
How do you believe immunocal increases inflammation?
Ime on this what did you see come out
I read somewhere that peroxynitrite shuts off the Peruvate dehydrogenase enzyme. So you’re right, all of these fascinating studies recently do seem to support each other. Perhaps this is why injectable hydroxocobalanin helps me so much – it breaks that part of the cycle, reducing the oxidative stress and diminishing the neuroinflammation etc (at least temporarily!). I always thought Martin Pall was on to something there! These are exciting times in the research I feel. Much is being uncovered. Thanks for making all of this legible for us Cort! I’m very appreciative 🙂
Interesting! Hypoxia causes the enzyme that converts to pyruvate into lactate – instead of to the form o pyruvate used by the mitochondria – to get activated as well.
Toxins, mercury, lead, candida, moulds, fungi, DDT, agent orange, insecticides, fungicides, fragrances, paint, outgassing polyester clothing, cleaning agents, how long a list would you like, it is endless. Does anyone really think it is only those of us with ME/CFS or FM that are affected? How about the rise in road rage, domestic violence, single punch killers, motor neurone disease, MS ? ? ? Do they also suffer from drastic alterations in brain chemistry and stress?
Do we clean up our environment and allow our bodies superb adaptive mechanism to repair itself? or will we create ever more chemicals to confuse the issue and our bodies even further.
I have just had a visitor in my ‘safe’ home for 4 weeks, unknown to me a roll-on deodorant was the cause of increasing headaches, dizziness, dangerous rise in pulse & BP, jerking muscles, and ultimately after feeling as if a knife had been shoved up my nose into my brain, full body muscle spasms for about 1/2 hour. Another ME crash? No, my body doing what it is supposed to do when under a severe poison attack. We are still trying to clean up our home a week later.
Well maybe we all see what we want in this. Interests me because I improved quite a bit on N-acetyl-cysteine. It hasnt been a cure but anyone who hasnt tried it yet might be prompted by this to do so. Maybe I’ll try it with NSAI as I need something more to reduce inflammation.
Dr. Shungu reported good results at the IACFS/ME conference
Hi Thatt, what doses do you recommend?
Thanks for responce.
sincerely
Could oxygen not be the core problem of this disease? shape red blood cells etc…
I know everyone is different and can have varied results with different protocols. Over the 15 years I’ve had ME/CFS I’ve gone through successful treatment for Candida, Fungal Issues, Food Sensitivities, treated Hypothyroidism and Addison’s Disease, de-chemicalized my home and food and water and yard and even my dog and spent 10’s of 1000’s on specialized tests and vitamins, hormones and every new targeted supplement for ME/CFS. Am I improved? Nope. Do I continue to decline? Yep. But I still perservere. I didn’t see any difference when I tried NAC a few years ago although I take L-Glutothione every morning. If it’s the brain that is low in Glutothione I wonder if taking that or NAC gets through the blood-brain barrier?? My newest experiment is Kratom. I’m shocked that it’s actually helping with my body wide nerve pain. I see there was a thread back in 2016 discussing it. I won’t take opioids and it’s quite surprising that something, anything is helping.
Anaerobic energy production is not “dirty”. When oxygen isn’t available to complete the krebs cycle and the electron transport cycle, lactate is NEEDED to breakdown glucose. The extra lactate is reused in energy production.
https://www.khanacademy.org/science/biology/cellular-respiration-and-fermentation/variations-on-cellular-respiration/a/fermentation-and-anaerobic-respiration
“Muscle cells also carry out lactic acid fermentation, though only when they have too little oxygen for aerobic respiration to continue—for instance, when you’ve been exercising very hard. It was once thought that the accumulation of lactate in muscles was responsible for soreness caused by exercise, but recent research suggests this is probably not the case.”
“Lactic acid produced in muscle cells is transported through the bloodstream to the liver, where it’s converted back to pyruvate and processed normally in the remaining reactions of cellular respiration.”
https://www.scientificamerican.com/article/why-does-lactic-acid-buil/
“Contrary to popular opinion, lactate or, as it is often called, lactic acid buildup is not responsible for the muscle soreness felt in the days following strenuous exercise. Rather, the production of lactate and other metabolites during extreme exertion results in the burning sensation often felt in active muscles, though which exact metabolites are involved remains unclear. This often painful sensation also gets us to stop overworking the body, thus forcing a recovery period in which the body clears the lactate and other metabolites.”
“As our bodies perform strenuous exercise, we begin to breathe faster as we attempt to shuttle more oxygen to our working muscles. The body prefers to generate most of its energy using aerobic methods, meaning with oxygen. Some circumstances, however—such as evading the historical saber tooth tiger or lifting heavy weights—require energy production faster than our bodies can adequately deliver oxygen. In those cases, the working muscles generate energy anaerobically. This energy comes from glucose through a process called glycolysis, in which glucose is broken down or metabolized into a substance called pyruvate through a series of steps. When the body has plenty of oxygen, pyruvate is shuttled to an aerobic pathway to be further broken down for more energy. But when oxygen is limited, the body temporarily converts pyruvate into a substance called lactate, which allows glucose breakdown—and thus energy production—to continue. The working muscle cells can continue this type of anaerobic energy production at high rates for one to three minutes, during which time lactate can accumulate to high levels.”
The question is, why does the body give up so early on utilizing oxygen in energy production? And I think it has to do with faulty metabolism due to faulty connective tissues. Specifically our adipose tissues which uses ATP cells for 2 functions; temperature regulation and energy production. If we have faulty adipose tissues (which store ATP cells until we need them to produce energy).
http://histology.med.yale.edu/connective_tissue/connective_tissue_reading.php
“Brown fat cells [a type of connective tissue] are highly specialized for temperature regulation. These cells are abundant in newborns and hibernating mammals, but are rare in adults. They have numerous, smaller lipid droplets and a large number of mitochondria, whose cytochromes impart the brown color of the tissue. The electron transport chain of these mitochondria is disrupted by an uncoupling protein, which causes the dissipation of the mitochondrial hydrogen ion gradient without ATP production. This generates heat.”
I understand that the view on lactate has changed and that other metabolites are involved. I keep using lactate as a kind of “holder” because it’s familiar. Since lactate increases in conjunction with the metabolites that cause harm, even if it is not the metabolite causing the problem, it works as a good analogue for now.
I also agree that anaerobic energy production is not necessarily “dirty”, that it works very well and causes no distress when it is used as an adjunct to aerobic energy production. It also doesn’t only show up when aerobic energy production is not available. I was incorrect about that and changed the blog to reflect that and the metabolite issue.
When aerobic energy production is not available and when it becomes the primary source of energy production -which apparently is happening in ME/CFS – then its by-products or rather the metabolites associated with it, do, as you point out, produce the symptoms like fatigue and pain.
“Rather, the production of lactate and other metabolites during extreme exertion results in the burning sensation often felt in active muscles, though which exact metabolites are involved remains unclear. This often painful sensation also gets us to stop overworking the body, thus forcing a recovery period in which the body clears the lactate and other metabolites.”
At that point it becomes a kind of dirty energy production process. Thanks for pointing out though, that it’s not necessarily that. I will clarify that in the blog. It’s similar to oxidative stress; free radicals play an important role in our body’s; only when they are too abundant do they cause problems.
Sure, that is in healthy people. We are talking about the possibility that dysfunctions in energy metabolism are responsible for the problems of a subset of unwell people. But I need to make this clearer in my own commenting. I have proved to myself that avoiding anaerobic exertion resulted in reduction in muscle pain for the first time for 20 years. Normal people recover in hours or even minutes; my muscles just stayed sore forever, until I started avoiding anaerobic exertion, in which case they gradually eased over a period of months.
This research seems to coincide in some respects with recent research
concluding that acetate supplementation attenuates neuroinflammation in the brain–evidently through epigenetics and through an alteration in the glycolitic pathway (I think). Does anyone know whether there is such an association between the findings of these two research areas? (I can attach the research papers respecting acetate supplementation if anyone is interested)
Please do interested in acetate supplementation.
Hello Mr. Raba
Here are links to some interesting research studies showing that acetate supplementation attenuates neuro-inflammation.
The particular acetate (Triacetin) has been used safely in large doses given to babies with Canavan’s disease. It is also rated as a safe food supplement by the FDA.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3070819/ Acetate supplementation attenuates lipopolysaccharide-induced neuroinflammation
http://www.jneuroinflammation.com/content/9/1/249
Acetate supplementation reduces microglia activation and brain interleukin-1β levels in a rat model of Lyme neuroborreliosis
http://www.jneuroinflammation.com/content/11/1/99
Acetate supplementation modulates brain adenosine metabolizing enzymes and adenosine A2Areceptor levels in rats subjected to neuroinflammation
http://www.ncbi.nlm.nih.gov/pubmed/23709104
Acetate reduces PGE2 release and modulates phospholipase and cyclooxygenase levels in neuroglia stimulated with lipopolysaccharide.
http://blogs.und.edu/uletter/2017/01/und-scientists-pursue-treatment-for-the-lingering-effects-of-lyme-disease/
Jim
Need to be careful with increasing Acetate levels, it can feed growth in some tumours.
http://www.cell.com/cell/fulltext/S0092-8674(14)01579-7
It’s so very good to hear hopeful progress like this, Cort. A related concept: It seems glutathione treatment was groundbreaking treatment, in recent years, for my Parkinson’s friend/neighbor, here in Jupiter, FL, who had to have a local pharmacy prepare it (compound it?) specially for her use. A groundbreaking doctor on the west coast of FL who was booked a year in advance, with Parkinson’s patients from all over, used it for his Parkinson’s patients so rather than wait to get in with him she worked with the pharmacist here (eastern FL), somehow, to have him compound it, or what have you, for her. And Parkinson’s and CFS-ME seem to have things in common, somehow. Maybe connecting research or data on both illnesses, one day, could help with research progress. Just a thought.
But connecting the dots more clearly to enable a better or easier “fit” regarding grants for research, as you are explaining, as well as proving a pathphysiology behind our illness is very encouraging. My functional medicine doctor, Ahner, in Palm Beach Gardens, FL, just last year explained my CFIDS/CFS-ME to his shadowing Physician’s Ass’t. as, “It is real. These patients all have the same issues”, which kind of floored me to hear someone refer to my very heavily bedridden status seemingly still in question in any way, therefore in need of “convincing” a health care practitioner of the validity of my illness. It’s possible, in receiving home health care after having rhabdomyolysis last year (VERY serious stuff– amidst my typical post vacation month-long, turned two 2 months long, PEM phase), the Nurse Practitioner assessing me at home had second-guessed my CFS-ME status and it’s validity, reporting it to Dr. Ahner, as all she judged me on was a “snapshot” of my day, when “I looked fine to her”! So “Come on progress”!
See you again, Cort, next Ft. Lauderdale seminar, maybe.
Thanks Karen. Interesting about glutathione. I believe Shungu’s NAC is trying to boost that up and the report from the conference was good. I hope we meet again at the next conference. I must say Ft Lauderdale is a great place to have a conference.
Hmm. Are you saying, then, that this is a chance disease – a bit of bad diet plus a trauma? I’m trying to reconcile this with the fact that my mother, my sister, my niece and I all have ME/CFS.
Studies suggest that both ME/CFS and FM have a significant genetic component – possibly more significant than in autoimmune diseases – which have a pretty high genetic component. More studies need to be done, though.
Shungu has tried DCA but had to stop because of neuropathies.
As I understand it, DCA blocks PDK which inhibits PDH (enzyme that is needed for conversion of Pyruvate to Acetyl-CoA). If there is a shift towards glycolysis as the main way of ATP generation, lots of Pyruvate is produced. Fluge and Mella found that PDH function is impaired which would cause insufficient Acetyl-CoA supply for the following aerobic respiration. So DCA would cause less lactate production by lifting the “block” between glycolysis and the Krebs cycle.
Anyway, there’s a study that compares the effect of DCA and high doses of vitamin B1 (Thiamine) on cancer metabolism. Most cancers mainly use glycolysis (because it’s much faster) and shut down the Krebs cycle by inhibiting PDH. The conclusion of the study I mentioned is “Our findings suggest that high dose thiamine reduces cancer cell proliferation by a mechanism similar to that described for dichloroacetate (DCA).” It seems as though high dose Thiamine leads to a reduction in PDH phosphorylation.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3963161/
I’ve heard between 1,5g and 2g of Thiamine HCL work very well for some people with Fibromyalgia (probably also CFS). For me 1,8g worked amazingly for about 10 days but then stopped working for some reason. This isn’t to say this is a cure but I find it to be an interesting clue for further experiments and understanding of this problem.
Very interesting Cody – thanks for passing that along. I had no idea B1 might be an option 🙂
Conf Proc IEEE Eng Med Biol Soc. 2010;2010:835-8. doi: 10.1109/IEMBS.2010.5626786.
Review of studies on modulating enzyme activity by low intensity electromagnetic radiation.
Vojisavljevic V1, Pirogova E, Cosic I.
Author information
Abstract
This paper is a compilation of our findings on non-thermal effects of electromagnetic radiation (EMR) at the molecular level. The outcomes of our studies revealed that that enzymes’ activity can be modulated by external electromagnetic fields (EMFs) of selected frequencies. Here, we discuss the possibility of modulating protein activity using visible and infrared light based on the concepts of protein activation outlined in the resonant recognition model (RRM), and by low intensity microwaves. The theoretical basis behind the RRM model expounds a potential interaction mechanism between electromagnetic radiation and proteins as well as protein-protein interactions. Possibility of modulating protein activity by external EMR is experimentally validated by irradiation of the L-lactate Dehydrogenase enzyme.
PMID: 21096313 DOI: 10.1109/IEMBS.2010.5626786
https://www.ncbi.nlm.nih.gov/pubmed/21096313
J Vet Med Sci. 2005 Oct;67(10):969-74.
Effects of exposure to a 50 Hz electric field on plasma levels of lactate, glucose, free Fatty acids, triglycerides and creatine phosphokinase activity in hind-limb ischemic rats.
Harakawa S1, Inoue N, Hori T, Tochio K, Kariya T, Takahashi K, Doge F, Martin DE, Saito A, Suzuki H, Nagasawa H.
Author information
Abstract
We previously reported that extremely low frequency electric fields (ELF-EFs) affect energy metabolism in stressed conditions. To further confirm this, the effect of exposure to ELF-EFs on the experimental ischemic rat was examined. The test was based on a comparison of rats treated with EF alone, ischemic surgery alone, the combination of EF with ischemic surgery, or no treatment (double sham). The EF condition used in this study was an alternating current of 50 Hz EF at 17 500 V/m intensity for 15 min per day. The exposure to EF in ischemic rats significantly decreased plasma levels of free fatty acids and triglycerides, compared to those of the no treatment or EF alone group. The plasma lactate levels of two ischemic groups peaked on experimental day-4 and gradually decreased until the end of the study. The changes in the lactate levels induced by ischemia did not show any difference between rats treated with ischemia alone or a combination of ischemia with an EF. Any changes in plasma levels of glucose and creatine phosphokinase activity were not influenced by EF treatment. These results indicate that the EF effect on glycolysis parameters, plasma lactate or glucose levels, does not appear in a highly stressed condition and that EF effects varied dependent on the condition of organism but ELF-EF used in this study have impact on lipid metabolism parameter in a hind-limb ischemic rat. However, further studies are needed to elucidate the association of ELF-EF with the lipid metabolism system.
PMID: 16276051
[Indexed for MEDLINE] Free full text
https://www.ncbi.nlm.nih.gov/pubmed/16276051
Bioelectromagnetics. 2004 Jul;25(5):346-51.
Effect of a 50 Hz electric field on plasma ACTH, glucose, lactate, and pyruvate levels in stressed rats.
Harakawa S1, Takahashi I, Doge F, Martin DE.
Author information
Abstract
The effect of extremely low frequency electric field (EF) on stress induced changes of plasma ACTH, glucose, lactate, and pyruvate levels was examined in ovariectomized rats. The rats were exposed to 50 Hz EF (17500 V/m) for 60 min and were restrained for the latter half (30 min) of the EF exposure period. The restraint stress significantly increased the plasma ACTH and glucose levels (P <.05: Student's t test). Restraint induced increase of plasma ACTH and glucose levels tended to be suppressed by exposure to the EF. Meanwhile, the EF exposure also affected plasma lactate level. Thus, the EF exposure significantly decreases plasma lactate levels in the stressed rats (P <.05: Student's t test). Although the precise mechanisms in the restraint dependent alteration in plasma ACTH, glucose, lactate, and pyruvate levels are not fully understood, our results demonstrate that the 50 Hz EF alter both stress responses and energy metabolism in stressed rats.
Copyright 2004 Wiley-Liss, Inc.
PMID: 15197757 DOI: 10.1002/bem.10202
https://www.ncbi.nlm.nih.gov/pubmed/15197757
Radiat Res. 1990 Apr;122(1):24-8.
Use of calcium channel antagonists as magnetoprotective agents.
Papatheofanis FJ1.
Author information
Abstract
Human polymorphonuclear leukocytes (PMNs) exhibited a time-dependent (0 to 60 min) increase in the release of lysozyme and lactate dehydrogenase (degranulation) when exposed to a static (direct current) magnetic field of 0.1 Tesla. When 1 X 10(6) PMNs were treated with the calcium channel antagonists diltiazem, nifedipine, and verapamil before exposure to a magnetic field, no significant change in degranulation was detected compared to control and sham-exposed PMNs that were similarly treated. Likewise, magnetic field-induced inhibition of cell migration was prevented with the addition of these antagonists. Such changes in degranulation and cell migration occurred in a dose-dependent manner. These results indicated that these agents protected PMNs exposed to a magnetic field, and the damage to the cells that is mediated by magnetic field-stimulated Ca2+ influx might be preventable. In this regard, pharmaceutical agents might prove useful in protection against injurious electromagnetic field exposure.
PMID: 2320722
[Indexed for MEDLINE]
https://www.ncbi.nlm.nih.gov/pubmed/2320722
Dr. Mercola:
“How Cellphones Can Cause Brain Tumors and Trigger Chronic Disease”
https://www.youtube.com/watch?v=fOFkxoMWVIg
Story at-a-glance-
– Exposure to cellphone radiation may or may not increase your risk of brain tumor formation, but this is a minor risk compared to damage done by free radicals from peroxynitrites that radically impair mitochondrial function
– Science has linked exposure to peroxynitrites from low-frequency microwave radiation emitted from cellphones and Wi-Fi networks with chronic diseases such as heart disease, obesity and inflammatory bowel disease
…..Snip….
Peroxynitrite at the Heart of Cellphone Damage
Peroxynitrite is an unstable structural ion produced in your body after nitric oxide is exposed to superoxide. This complex chemical process begins with exposure to low-frequency microwave radiation from your cellphone, Wi-Fi and cellphone towers.
The process begins when low-frequency microwave radiation activates voltage-gated calcium channels (VGCC), producing calcium inside your cells and mitochondria.36 Nitic oxide is dependent on the presence of calcium to activate. With additional calcium present, nitric oxide is then activated in the cells.37
Nitric oxide is a substance present in all vertebrates, and helps to control blood flow, neural activity and clotting.38 While it has many health benefits, it can become destructive when superoxide molecules, an ionized oxygen molecule, is released during pathological change, such as a stroke or muscle injury.39
This reaction between nitric oxide and superoxide produces peroxynitrites, believed to be one root cause for many of today’s chronic diseases.40 Nitric oxide is the only molecule in your body produced at high enough concentrations to outcompete other molecules for superoxide and is a precursor for peroxynitrite.41
Peroxynitrite in Your Body
Once formed, peroxynitrite reacts relatively slowly with biological molecules, making it a selective oxidant. Inside your body, peroxynitrites modify tyrosine molecules in proteins to create a new substance, nitrotyrosine and nitration of a structural protein.42
These changes from nitration are visible in human biopsies of atherosclerosis, myocardial ischemia, inflammatory bowel disease, amyotrophic lateral sclerosis and septic lung disease.43 Significant oxidative stress from peroxynitrites may also result in single-strand breaks of DNA.44
This pathway of oxidative destruction triggered by low-frequency radiation emitted from mobile devices may partially explain the unprecedented growth rate of chronic disease since 1990.45 This, truly, is a FAR greater concern than brain tumors, when it comes to the hazards of cellphones.
Information from the scientific literature reveals a dramatic acceleration in a single generation in the prevalence of a long list of diseases. Once you understand that cellphones can contribute to these chronic diseases — not just brain tumors — you may be more apt to take a few precautions to limit your exposure.
Although the major health threats continue to be cardiovascular disease, cancer and infections, it should be noted that the following list of conditions often create significant challenges in the lives of those who suffer. Some of these diseases were not even public knowledge prior to 1980.46
Disease or disorder Increase since 1990
Chronic fatigue syndrome: 11027 percent
Bipolar disease in youth: 10833 percent
Fibromyalgia: 7727 percent
Autism: 2094 percent
Celiac disease: 1111 percent
ADHD: 819 percent
Lupus: 787 percent
Hypothyroidism: 702 percent
Osteoarthritis: 449 percent
Sleep Apnea: 430 percent
Diabetes: 305 percent
Alzheimer’s disease: 299 percent
Depression: 280 percent
….Snip….
Read more: http://articles.mercola.com/sites/articles/archive/2017/05/23/cellphones-cause-brain-tumors-trigger-chronic-disease.aspx?utm_source=dnl&utm_medium=email&utm_content=art1&utm_campaign=20170523Z3&et_cid=DM146932&et_rid=2015952822
‘Bad energy’ may have more to do with it than most folks realise. My recent integrative health perspective connects neurological/immunological stressors to the emergence of pain, inflammation, and sensitisation disorders in ME/CFS and associated conditions (FMS etc):
• Toxic mould fungi and other pathogens (certain viruses/bacteria)
• Non-ionising electromagnetic fields (EMF) and radiation (EMR)
• Persistent pollutants (e.g. heavy metals and pesticides)
https://doi.org/10.3389/fphys.2017.00088
I guess neuroinflammation is a red herring.
Neuroinflammation happens in Burnout Syndrome, Major depression even in Stress (elevated level of SOD 100 in combat fighter)
There was a case in Spiegel (famous magazine in Germany) of a student with major depression caused by a neuroinflammation. After treating a chronic sinusitis he was healthy again.
The experts called it “sickness behaviour” (i think i already heard this term :-))
And can be caused by for example an inflamed tooth root or problems with the gut or even a flu. (When you are sick you don’t wanna make party; you just wanna sleep and silence)
Here in Germany all the alternative medicines test cfs with isoprostan or nitrotyrosin; marker for oxidative stress ( you can even order some tests via Amazon.)
I forgot to mention that they also found low ATP production in Depression.
My idea is that something produces oxidative stress (the cause is in every case different) and the consequence is malfunction of the ATP production and inflammation in the brain.
The body goes into standby until the damage is fixed.
And this can be everything from leaky gut to chronic virus or too much stress.There’s no one size fits all solution.
That’s the reason why someone is healed with Gupta Training and a another one with Valcyte and the third one has just a splinter of wood in his toe.
Neuroinflammation is apparently found in many brain diseases – I think the question is where is it occurring and how much of it is there.
Or it depends of the genetic.
Maybe we have the genes for cfs and anther one for depression.
Maybe the cause is also a problem – an infection causes another pattern of Neuroinflammation as too much stress or overtraining
There seem to be a lot of studies on plants which suggest that heavy metals are affecting their glutathione production. Could this be happening in humans too? ?? The glutathione is used up too much or compromised in some way by the presence of metals??
Geez, I have so much to say, and no energy to do it properly.
The Downside of Upright Posture by Michael Flanagan, DC, neurological chiropractor , is an essential read to begin to understand more of the whole picture of brain fluid dynamics. Researchers MUST begin to appreciate that there is a whole system from the sacrum to the cranial bones that regulate fluid distribution and pressures. Hence, women are more at risk due to wider, more unstable sacrums. Dr. Flanagan also has a great website. Easily found.
So, I have been trying to understand for years why certain people with different physical structures ( like scoliosis/ vertebral anomalies) might be at greater risk for viral/ organism invasion of the Central nervous system. Well, an article in the April 2017 issue of Discover magazine begins to shed more light. “Hidden Invaders” by Pamela Weintraub.
Vascular biologist, Dritan Agalliu, has been researching how Th 17 immune cells damage the blood brain barrier and allow entrance of unwanted antibodies to enter. There is thought ( evidence?) that the TH17 cells are entering the CNS through the olfactory area.
Neuroscientist Jonathan Kipnis has been researching newly discovered (? ) brain fluid drainage systems that drains toxins into the cervical lymph nodes and jugular veins. Michael Flanagan has been discussing this for years.
So, might we have structural differences in the nasal/ cervical areas that inhibit fluid balance in the brain and affect the structure of the olfactory bulb where Agalliu thinks the blood brain barrier is being compromised? Who, besides me, has a deviated nasal septum? Lack of curve in neck? A tipped atlas ( from X-ray) ? Small posterior fossa? Short clivus, high-Arched palate?
More later. Exhausted.
How much NAC should we try taking to boost our glutathione? Anyone know? Is an L-Glutathione supplement of any use in preventing/relieving neuroinflammation? I really need to try this – it’s beyond any pain I’ve ever endured, including drug-free childbirth!
Clear Light energy has helped reduce my pain, eating gluten, sugar, diary free and practicing kundalini yoga and meditation. I remember years ago having IBS, but don’t have it now and years ago I drank this stuff ATP, no longer on the market, why is that, it used to give me energy, lift mood, etc….strange it is off the market. Why? I wish they could just stop the pain signals in the brain, that would be a 100% blessing, the pain causes the fatique and depression, ugh.
Hi Cort..I am 78 and a sufferer of these symptoms since childhood. It is speculated that Rocky Mountain spotted fever that left me in a coma might have been the onset..regardless I googled :the effects of long term use of sudafed and me/cfs and was directed to you again.
I asked this question as I was considering using it long term. Whenever I use it for sinuses I have more energy..can stay awake..can think n read and have better concentration..I even finished writing this.
I am a tai chi/qigong teacher and that has been beneficial but have had to temporarily postponed teaching..this year since January and am still out.
Have you read or heard anything about this. Afraid to use epinephrine/adrenaline long term until I find out..MD was not helpful.
Thank you thank you for all you do.
Hi,
Great article Cort.
Can anyone tell me whether you can get this MRI (i.e. measuring lactate and glutathione) in the UK and if so where (and cost if possible). Even a description of the MRI might help to identify medical centres which have this equipment (I may try the paper for this).
Is there any information re nonsteroid anti-inflammatory drug (NSAID) referred to above (e.g. have they tried one).
Based on 2 minutes on the web I found the following re glutathione:
“Elevation of glutathione as a therapeutic strategy in Alzheimer disease”
“Abstract
Oxidative stress has been associated with the onset and progression of mild cognitive impairment (MCI) and Alzheimer disease (AD). —In this review, we focus on the elevation on glutathione through N-acetyl-cysteine (NAC) and γ-glutamylcysteine ethyl ester (GCEE) as a potential therapeutic approach for Alzheimer disease.”
So there’s been some work on glutathione in Alzheimer’s did these researchers look at lactate and if so did they establish MRI tests for lactate.
We may benefit from other research such as this.
Thanks
I don’t know if you can get these tests done at the doctors office or not. Some of these are research only tests but we should be getting a paper pretty soon on the supplemental glutathione study….
I have no doubt that both mitochondria and lactate contribute to this awful disease process. Walking is like hitting the wall after 20 plus miles on a walk, except it happens at less than a quarter of a mile and if as anyone with the disease knows; you overdo it, you get the aches and pains of lactic acid for not hours, but days sometimes weeks. The mitochondria can’t get rid of it easy either, which is the dysfunctional part. Unfortunately at the moment we don’t have a clear understanding of which came first, the lactate or the mitochondria. Once we have that then we could move further forward I hope. But its a multifactorial disease process. You don’t just get the disease, it creeps up insidiously, and presents itself after certain stressors, Something big triggers it judging by the amount of type A people with it.
Thanks Doctor for your comment 🙂
From my own experience, a metabolic blockage in the urea cycle is causing the build up of lactate & ammonia. I am trialling Citrulline Malate at the moment with noticeable success. It mops up the ammonia /lactate, thereby reducing inflammation in the brain and body. It also seems to be reducing the bodys demand for the antioxidant glutathione.
No kidding! Citrulline malate – I’ll have to get some. How much improvement are you seeing?
Have there been any studies about similarities in a persons overall health other than being tired and sore? I ask this because I am highly susceptible to developing keloid where I’ve had surgery or an open wound from injury and I don’t get a satisfactory answer from my family physicians. I also feel like the bones or tissues around the bones in my feet feel swollen and tender but the more I walk on them the better they feel until I overdo it. For example when I wake up the feelings of swelling and tenderness are evident but after being up and walking th feet feel better until I’ve been on them all day. The xrays show nothing is evident to be causing this. I also have been told I have low nerve conduction in my lower legs, motility issues with swallowing food, and have small narrow veins among other issues that don’t bother me near as much as these ones do. I’m asking….do others with Fibromyalgia voice any of these as issues they too have. My family doctor says the symptoms I have might be part of the fibromyalgia or Chronic Fatigue I was diagnosed with over 30 years ago. I’m so tired of feeling sick and tired. I hope you can answer my questions.