

A Central Nervous System Hypothesis of Chronic Fatigue Syndrome
“… neurophysiological and neuroimaging studies in combination with subjective or a newly developed objective evaluation method of chronic fatigue have begun to clarify the mechanisms underlying chronic cognitive fatigue …”
Deciding that ‘chronic fatigue’ had become not just an illness problem but a productivity concern for their economy, the Japanese initiated a program a couple of decades ago to understand and treat it. They note that a third of the Japanese population complains of “chronic fatigue” and that “chronic fatigue” contributes to cardiovascular conditions, epilepsy, and early death. Their program has encompassed all levels of fatigue from chronic fatigue to chronic fatigue syndrome. We’ve missed out on a lot of their work focused on fatigue because it doesn’t show up in searches for Chronic Fatigue Syndrome (ME/CFS).
Relative to most of the rest of the world, the Japanese program is a large one – probably larger than the NIH/CDC efforts in the U.S. Led by Drs. Watanabe and Tanaka, the Japanese found the first direct evidence of neuroinflammation in the brains of Chronic Fatigue Syndrome patients.
The Japanese doctors believe they understand enough of the origins of chronic physical and cognitive fatigue in ME/CFS to develop a hypothesis about how they develop and why they persist. Displaying an initiative rarely seen in western ME/CFS researchers, they’ve put their ideas on the line and actually published them.
- Masaaki Tanaka, Akira Ishii, Yasuyoshi Watanabe, Regulatory mechanism of performance in chronic cognitive fatigue. Medical Hypotheses 82 (2014) 567–571.
- Tanaka M, Ishii A, Watanabe Y (2013) Neural Mechanism of Facilitation System during Physical Fatigue. PLoS ONE 8(11): e80731. doi:10.1371/
Let’s see what they have to say.
The Origins of Physical Fatigue in Chronic Fatigue Syndrome (ME/CFS)
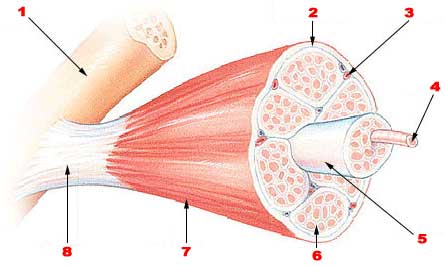
Muscle Fatigue
When we exercise, our muscle activity is impaired by declining ATP and glycogen levels, problems with calcium transport, and oxidative stress. (The author do not believe that lactate buildup is particularly important.) Muscle fatigue due to metabolic problems, however, is not the kind of fatigue they’re interested in. Nor do they appear to believe it plays much of a role in chronic fatigue syndrome (ME/CFS).
They’re focused on another place – the brain – and they’ve done enough original research to propose not just a new hypothesis of fatigue but to assert the presence of neural circuits specifically designed to reduce or accentuate fatigue.
Central Fatigue
When we engage in any physical task, the primary motor cortex in our brain activates the motor neurons in our spinal cord which then sends a signal to the neuromuscular junction of the muscle telling the muscle to move. As a muscle fiber becomes fatigued more muscle fibers are recruited. So long as new, fresh muscle fibers remain to be recruited, the exercise can continue. If no muscle fibers are left to be recruited or if the brain has a problem recruiting new muscle fibers, fatigue sets in.
When fatigue becomes apparent during exercise we can do one of two things: we can stop the exercise or we can increase our effort. In a process they call “facilitation”, increasing our effort causes the primary motor cortex in the brain to increase its output to the muscles.
We all did this without thinking thousands of times prior to the onset of ME/CFS; we started to get tired, we increased our effort, and the fatigue disappeared for a time. That bull-through-the-fatigue approach obviously doesn’t work well after Chronic Fatigue Syndrome has set in.
Facilitating Muscle Activity and Energy
In 2012 these researchers proposed the existence of a central nervous system circuit that allows humans to “increase their motor output”. It includes the limbic system, basal ganglia, thalamus, orbitofrontal cortex, prefrontal cortex, anterior cingulate cortex, premotor area, supplementary motor area, and primary motor cortex.
The first six of these regions (limbic system, basal ganglia, thalamus, orbitofrontal cortex, prefrontal cortex, anterior cingulate cortex) have consistently popped up in ME/CFS studies. The last three regions involving the motor section of the brain have shown up in ME/CFS literature, but not a lot, and it’s been years since they’ve been studied. Since the motor section of the brain basically drives physical activity, it’s puzzling it hasn’t been given more emphasis in the most fatiguing disorder of them all. The Lights noted that the most common cause of muscle failure is a decrease in the command signal from the motor cortex to the muscles.
A 2003 study suggested that reduced muscle recruitment due to reduced motor cortex output might be the cause of the fatigue in ME/CFS. That study suggested that “… changing motor deficits in CFS have a neurophysiological basis [which] … supports the notion of a deficit in motor preparatory areas of the brain“.
That study titled, “Deficit in motor performance correlates with changed corticospinal excitability in patients with chronic fatigue syndrome“, to my knowledge was never followed up on.
In a process they call “central fatigue”, Watanabe and Tanaka believe the brains of people with ME/CFS are simply not recruiting enough muscle fibers.
They also believe that reduced dopaminergic inputs into the system are thwarting motor cortex activity in ME/CFS. That’s an interesting conclusion given recent work by Andrew Miller of Emory University suggesting that reduced dopaminergic drive plays a key role in the basal ganglia dysfunction and fatigue seen in ME/CFS.
The Cause of Cognitive Fatigue in Chronic Fatigue Syndrome
Two years later, Watanabe and Tanaka identified a cognitive facilitation circuit that allows one to push through mental fatigue. It consists of a neural loop that interconnects the limbic system, basal ganglia, thalamus, orbitofrontal cortex, prefrontal cortex, and anterior cingulate cortex.
Motor imaging and cognitive task studies suggest this system is not working well in Chronic Fatigue Syndrome. This is probably, they believe, due to metabolic, functional and structural damage to the basal ganglia, orbitofrontal cortex, prefrontal cortex, and anterior cingulate.
That’s not enough, however, to account for the extreme fatigue found in ME/CFS.
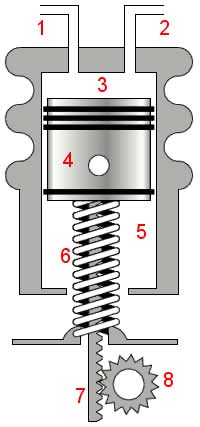
Enter the Fatigue Inhibition System
Studies indicated that giving a maximum effort plus electrical stimulation of the motor cortex was not enough to drive the spinal motor neurons to produce maximal muscle output. That suggested another neural circuit was involved.
They called this circuit the “fatigue inhibition system”, but it’s really a “fatigue enhancement system”. This is a system that, perhaps somewhat like the pain inhibition system that has gone awry in fibromyalgia, interacts with signals from the brain.
When we’re fatigued, the fatigue inhibition system stops signals from traveling from the motor cortex to increase muscle performance. This system essentially locks down further muscle recruitment and induces more fatigue. They believe this ‘fatigue inhibition circuit’ (better understood as a fatigue-inducing circuit) is turned on full-time in Chronic Fatigue Syndrome.
This circuit stretches from muscle nerves to the brain and includes everything in between. It consists of the spinal cord, thalamus, secondary somatosensory cortex, insular cortex, posterior cingulate cortex, premotor area, supplementary motor area, and primary motor cortex.
Energy System Burnout

Push the energy facilitation system too hard and the authors suggest it will burn out leaving the fatigue enhancement system in charge
The authors believe that overuse of the facilitation system via continual attempts to overcome fatigue is counterproductive and ultimately impairs the system’s ability to produce energy.
Animal models indicate that continually pushing the energy facilitation system via overwork or prolonged stress (or perhaps pushing the system during extreme fatigue after one has gotten ME/CFS?) causes this second ‘fatigue inhibition’ to lock everything down.
Their studies suggest this is the result of classical conditioning which means, if I understand it correctly, that after repeated attempts fail, the system simply shuts off that option.
Thus, there are two parts to centrally produced fatigue. There is the facilitation process that allows us to activate the motor cortex and recruit more muscles in the face of fatigue, and there is the inhibition system that stops the facilitation system in its tracks. The authors believe the second of these is in control in ME/CFS.
Prefrontal Cortex Again
“This brain region also has a crucial role in determining physical performance.”
A recent blog suggested that damage to the prefrontal cortex in ME/CFS was associated with autonomic nervous system problems, and a review of the literature indicated that damage to that area of the brain has been implicated in other fatiguing disorders.
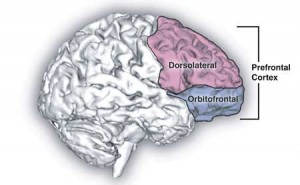
The authors suggest damage to the prefrontal cortex may play a critical role in the fatigue found in ME/CFS
The Japanese researchers zeroed in on the dorsolateral prefrontal cortex (DLPFC), a part of the brain that regulates a variety of functions often impaired in ME/CFS including sensory inputs (physical sensations, over-stimulation), emotions (high emotional lability), attention span (attention what?), working memory (“please repeat that”), planning (right!), self-control (highly needed) and decision-making (agonizing). It’s the seat of executive functioning – and studies suggest it’s not doing so well in ME/CFS.
Cognitive processes are what the prefrontal cortex is known for, but that’s not why these researchers are zeroing in on it; it also plays an important role in motor control; i.e., movement. The DLPFC connects to several parts of the brain that regulate movement including the premotor cortex, supplementary motor area, cerebellum, and basal ganglia.
Because the dorsal lateral prefrontal cortex appears to decide which process – energy enhancement or the induction of fatigue – is going to prevail, the authors hypothesize that metabolic, functional, or structural damage to this part of the brain is key to the development of fatigue in ME/CFS.
In a Nutshell
Here in a nutshell is how it appears to work. Once you begin feeling mentally fatigued you, without knowing it, activate something called the facilitation system to enhance your mental performance. This system consists of a neural loop connecting the limbic system, basal ganglia, thalamus, and frontal cortex. It’s thrown into action mainly through dopaminergic inputs into the striatal-thalamic-frontal loop, but studies suggest those are inhibited in ME/CFS.
Cranking up this facilitation system too often (something that will surely occur in ME/CFS) causes an inhibition system (consisting of the thalamus, somatosensory cortex, insular cortex, posterior cingulate cortex, and frontal cortex) to become activated to suppress performance — to induce rest and avoid more fatigue.
The more you try to punch through your fatigue, the more the inhibition system (via classical conditioning) induces fatigue. At this point, you’re in a state of ongoing chronic fatigue.
Damage to the prefrontal cortex likely pushes the brain to increase activity in the fatigue-inducing circuit.
The Japanese do not appear to include peripheral sources of fatigue in their model. However, evidence is accumulating both in ME/CFS and Fibromyalgia that problems below the head could play a role. The Lights at the Univ. of Utah have stated they want to do for fatigue what’s been done for pain; namely they, like the Japanese, would like to elucidate unique fatigue-producing pathways in the body. Their studies suggest hypersensitive muscle receptors in ME/CFS may be telling the brain that the muscles have been damaged and it’s time to shut them down.
It’s good to see ME/CFS research groups working on elucidating fatigue pathways to the brain.








Keep trying to tell people I had a full, 100% remission from training up Sensory Motor Rythmn (SMR, 12-15Hz) at C4 with EEG neurofeedback, but no one seems to care, lol. The effects lasted for days, were total and complete, and only disappeared when on the advice of the clinician I did more training at that site to keep the results going. That’s the usual model in neurofeedback for “normal” people: keep training to get lasting improvements. Apparently the CFS brain is more delicate, however – more unstable, if you will – and the results can happen much faster — even with a single sessions — as well as be more susceptible to being lost for the same reason.
CFS imo is all about the brain and neurology, and how the CNS is controlling metabolic and immunological systems through feedback mechanisms. Wild goose chases for “the microbe” or pathogen, etc. are bound to come up short, imho, because if you solve for those things (if they even exist, which is doubtful), the underlying dysregulations in neuroimmune/neuroendocrine and neurometabolic systems remain. So there will just be another “pathogen” to keep you sick. Change the neurology, however, and then it won’t really matter what’s there (subclinically, etc.) — we’ll deal with it just like everyone else does.
Very interesting Jrez.
Could you please tell us where/how you did this SMR training?
Where does one go to get that kind of treatment?
Congratulations on your improvement :). The Japanese are certainly highlighting feedback mechanisms….Any way to get improvement works for me. I hope to learn more about how you went about this.
Can you be more specific about your smr? What is it and where can I learn more about it?
Where can one get more information about smr?
Jrez, how often were you doing SMR when you were having good results and how long were your sessions? I did nuerofeedback for a while, and some sessions made me very relaxed and uplifted while others were just ok. I’ll have to look into SMR I guess. Can you do SMR again or did your brain completely stop responding to it?
Hello Gail, Bruce, LaCan,
Yes, my brain did stop responding to that particular training, at least in that way. So now it’s a matter of finding what might re-regulate things again, if possible, and hopefully cause another remission.
SMR stands for “Sensory Motor Rythmn,” and it’s a way of referring to a particular bandwidth within the EEG frequency spectrum. You might have heard of alpha waves, delta waves, gamma waves, etc. — well, SMR is just another range of waves within those other more or less arbitrary designations. The entire spectrum our brains operate on is roughly 0-40Hz, and more specifically, SMR is generally considered to be within the range of 12-15Hz.
I would also caution that it’s not a matter of thinking that training to increase SMR worked for me, so therefore it will work for everyone. That’s just what my brain seemed to need at that particular time. Perhaps someone else would need more or less alpha at certain locations, or beta, or some other frequency or approach (more or less coherence, etc). Raising SMR is just what happened to work for me at that moment — and in fact, I was also suppressing theta and high beta, so it could also have been related to that aspect.
Cort and I have discussed doing a blog entry on this, so give me a little time and I hope to write something up with more detail. Whether people can get remissions is a pretty big thing to hope for, but based on my experiences, I am really convinced almost for sure that NF could at least help many people symptomatically, especially with some of the central OI/POTS kinds of issues, sleep (I can literally almost turn my sleep on and off with NF), possibly brain fog and related cog problems. So maybe that will be useful in some cases, if people can only get access to treatment. With a wider database of CFS patients getting NF, perhaps we might even start seeing some common patterns, just like we see in ADHD, or depression, etc. That would be my hope, at least.
whoops, “rhythm.” 😉
Hey Jrez…who did your testing? and you can you explain in a little more detail? Thanks.
I found this article to be the closest thing to being a very good explanation of what happens in ME! It is exactly what I find happens to me-the fatigue, the over-exertion, the crash. the fact that I am shutting down faster and faster now from even one year ago. And the mental ability being affected. And possibly the IB now starting. It comes from the brain!! I have seen all kinds of symptoms listed and I have had many from one year to the next, and in the end many can be helped by medication, but they are all there, lurking for when the brain misfires and starts a bout of something, or your eyes don’t see right for a few days, or your acid reflux flares up. Even depression-SSRI’s-HA None of them have ever agreed with me, let alone get rid of depression! My brain does that when whatever is stressing me conquers it! This is a completely off the wall diagnosis I made of myself at least 10 years ago!! Now it looks like my simple conclusions might belong to a huge body of things to be researched! Hooray!! I probably sound silly, but I will be saving this article!!
Jrez,
Your statement “the underlying dysregulations in neuroimmune/neuroendocrine and neurometabolic systems remain”, is consistent with the position held by Jay A. Goldstein M.D. for some years.
Goldstein’s position caught my attention. Do you have other source materials consistent with this position?
Robert
U hit the nail on the head. I’ve had ME/CFS & Fibromyalgia for 45 years! There damage that’s not going to change! I’ve excepted that & work within those bounties, but would love it if this research continues, them others may not wind up with long term damage like me.
Thanx Kamneo
I know it has been 5 years since this comment but if you somehow see this comment please contact me asap i have big ideas and insights.
Share with us please
I’m all ears 😄
I’ve had ME/CFS and FM since 1984 (38 years) and I would love to hear your big ideas. Seriously.
Great to see that Japan takes this disease so seriously and that they have provided significant resources for research. So far, it sounds like they are making great strides.
Thanks for the info, Cort!
I particularly like their hypothesis of reduced muscle activation – makes sense to me 🙂
I wonder if neuromyotonia, antibodies to the nerve muscle junction, could be involved.
I’m very curious as to whether they have deemed latent infecting pathogens such as Lyme bacteria or various Herpesviridae viruses as precursors, eg causing the brain damage
I don’t know if they’ve ever gotten into pathogens. My feeling is that they haven’t. They do ascribe the neuroinflammation they found in their previous study to astrocyte or microglial activation – both of which could become activated in response to pathogens.
Interesting, but what next?
Hypothesis of explanations are goog, but what we sick and suffering people expect is an advice on what to do? Our life is fading away and so true help in sight!
I do not expect miracles but articles on more than possible causes: at least possible solutions. Kind regards
Thomas
My guess is that the problems in the brain may be driven by the problems in the body….and that’s where the treatments will come in.
On the other hand, this is the same group that found evidence of neuroinflammation in many of the parts of the brain they referenced in these papers (but not oddly enough the prefrontal cortex :). In that paper they suggested astrocyte and microglial was probably to blame. If that’s true then microglial inhibitors could be helpful. (We have a page on microglial inhibitors on the website).
Of course it’s pretty much speculation at this point….we need more studies and the Japanese are reportedly embarking on bigger study.
If I read them correctly, I believe they do suggest things to stop the fatigue inhibition (or enhancement) system from going off. I presume that would include things like meditation to stop the alert from being sounded.
A recent paper (last 2 years-ish; I think the main one came to mass media attention in 2013) brought together research on the glial cells’ function. From what I recall (not much right at this minute), very simply, the glial cells act in the brain as the lymphatic cells act in the body. This has led to the formation of the term “glymphatic system”. The article focused a lot on sleep – the glial cells cleanse the brain while we sleep. It did state that it didn’t seem to matter when the sleep occurred, as long as the brain rested, the glial cells cleaned out ‘junk’.
I am not sure is microglial cells are doing the same, but the idea still fits – just perhaps more along the lines of the detoxification pathways not working – which fits with the low levels of glutathione and high levels of oxidative stress seen in CFS, as well as lesions on the brain, often seem in Lyme disease (my confirmed diagnosis, although chronic fatigue – syndrome, or symptom? – persists, despite massive improvements in other areas with Lyme treatment).
I.e. if glial (and/ or microglial) cells are causing inflammation in the brain due to pathogens, they may just be working harder – and failing – to try to get rid of them. Inhibitors might not be helpful, something to aid in the process of detoxification and brain healing may actually be more effective. I realise this is further conjecture.
Very interesting article. Thanks.
Thomas,
Do not despair. Granted, the illness we have is difficult. This web site is a treasure trove of information to help you get started on figuring out what is going to work for you.
I have achieved a fair degree of re regulation from some what is discussed in the last couple of posts on this site. I am not cured (whatever that means), but I can work, and participate in professional, social, and family life.
Best regards,
Robert
Can you be more specific about your smr? What is it and where can I learn more about it?
Nice write up Cort.
The potential role of the prefrontal cortex in ME/CFS is very intriguing.
It’s interesting that irritable bowel syndrome (IBS) patients appear to have reduced activation of the dorsolateral prefrontal cortex (ref here: http://www.ncbi.nlm.nih.gov/pubmed/22841782 ).
It may be that IBS sets the scene of prefrontal cortex dysfunction, such that already having IBS may then predispose individuals to developing ME/CFS. This could explain why IBS is a very common comorbidity of ME/CFS.
Perhaps ME/CFS patients should be exploring medications that can improve prefrontal function, such as the stimulant drug Vyvanse (lisdexamfetamine) that you discussed in your blog here: http://www.cortjohnson.org/blog/2012/12/28/26/ .
Alpha-2 agonist drugs like Clonidine can also improve prefrontal function.
I tried Clonidine in doses of 75 mcg to 150 mcg, but found this drug made me acutely deeply fatigued and sleepy for about 3 hours after taking it (and then I fully recovered my energy very quickly). This increased fatigue effect of Clonidine in ME/CFS patients is exactly what Wyller found in his study (as your blog details here: http://www.cortjohnson.org/blog/2014/02/15/sustained-arousal-hypothesis-sustained-wyllers-clonidine-trial-chronic-fatigue-syndrome-fails/ ).
Good to hear they are doing research but more theories, not really tested – disappointing.
I think Hennessy said somewhere, regarding the poor funding from the NIH, that this illness is costing the economy massive losses each year, such that the Government is not just cruel, but also plain stupid! – Well it seems the Japanese aren’t stupid…The illness is costing a lot and they want to solve the problem…
About the above model, I wonder how it applies no only to chronic fatigue, but to the suddenness of a relapse or a full blown crash. Are they “in” on PEM, especially in its dramatic forms?
This goes hand in hand with what is seen in major depression… In fact I have seen several hypothesize that mdd and cfs are both on the same spectrum… (Excluding atypical mdd). The abnormalities seen in mdd are essentially caused by stress and an over active hpa axis. This is also common in cfs. Hpa dysfunction is related to neurotransmitter dysfunction, probably serotonin (in my experience) although other systems are involved. This receptor dysfunction can be caused by chronic stress, inflammation, or a combination. Over active hpa leads to excess adrenal hormones in circulation. This is what causes the destruction as noted above. The structural damage is usually repairable and limited to the hippocampus. The function impairments in the Pfc become regulated with treatment.
Therefore in my experience cfs and mdd are best treated the same way.
Ssri’s (yes they sound so scary) are a great approach. Ssris work by regeneration brain cells in the hippocampus (the damaged area) as well as flooding the Pfc synapses with serotonin causing glucocorticoid levels to drop and breaking the cycle. Usually a 6 month course is sufficient to put things in remission.
Another approach is anti glucocorticoid drugs. A couple studies back in the 90s showed that 75% treatment resistant depressed patients achieved remission after treatment with ketaconazole, a potent cortisol synthesis inhibitor, for 4 weeks. The response was maintained at 5 month follow up. (Probably due to down regulation of neural glucocorticoid receptors). Finally, if all else fails, ect therapy is extremely effective with remission rates upwards of 80%.
This is my two cents but I think treating a cfs like major depression while the underlying infection is simultaneously dealt with is essential.
Thousands of MECFS patients have been treated for depression with dozens of different antidepressants and the feedback is that it just doesn ‘t help. I did a decade of them myself and it didn’t make a damned bit of difference. I never had any symptoms of “depression” except for dibilitating fatigue that those docs couldn’t wrap their minds around so did the default diagnosis: depression.
Amen to THAT!
I’m glad an SSRI helped you, but it caused some serious damage in me. Increasing serotonin was not what I needed. My sister, who also has CFS, reacted very badly to SSRIs.
There are 3 places in this article that seem to indicate deficient dopamine usage (see below). I have self-medicated with Mucuna capsules, an herbal source of dopamine. This has helped me more than the tricyclic anti-depressants, or the SSRI I was on. (SAMe is another way to boost dopamine levels, but it takes months, and for us the boost was too small.)
Might a dopamine supplement make more sense than manipulating serotonin?
Kim & Kelly Derrick
Dopaminergic quotes
“They also believe that reduced dopaminergic inputs into the system are thwarting motor cortex activity in ME/CFS. That’s an interesting conclusion given recent work by Andrew Miller of Emory University suggesting that reduced dopaminergic drive plays a key role in the basal ganglia dysfunction and fatigue seen in ME/CFS.
This system consists of a neural loop connecting the limbic system, basal ganglia, thalamus, and frontal cortex. It’s thrown into action mainly through dopaminergic inputs into the striatal-thalamic-frontal loop, but studies suggest those are inhibited in ME/CFS.
Kim and Kelly,
Would you be willing to tell me which brand of mucana capsules (and what strength) has been helpful for you? Thank you!
Greg, have you read the studies done by Dr. Mark Demitrack?
He proved that CFS and MDD are opposites in terms of cortisol and the HPA axis. SSRIs can be damaging to people with CFS.
I have a question about this. When I had bad depression I was forced to have ECT treatments. I had electrodes put on the front of my brain and was sapped. I don’t know how many times because we were put out. We were given something to relax our muscles. Because once they gave that to me first before they put me out. I had a lot of trouble breathing until they gave me the med to put me out. These treatments caused us to have convulsions. How many I don’t know, we were never told. This went on to me for over a year.
My question could these treatments have caused me to have CFS? I have Fibro, and AS. The combination of these, could that be causing me to have CFS? I don’t know all of these hard words and terms that are being used in this article. I just know how I feel.
Thanks for any help,
Kathy
Hi Kathy. Ect is not fully understood. Few studies have attempted to find how it alleviates depression and it is currently believed to do so in a similar way to ssris, neurogenesis, up regulating or downregulating certain receptors etc.. It also has effects on brain waves (EEG readings) so it is quite possible the fibro could be related. Or the fibro could be related to a pathogen that also was causing the depression. There is no way to really know unfortunately.. Hopefully you are not still experiencing depression
Hi Kathy. Shock therapy is not fully understood. Few studies have attempted to find how it alleviates depression and it is currently believed to do so in a similar way to antidepressants, neurogenesis, up regulating or down regulation of certain receptors etc.. It also has effects on brain waves (EEG readings) so it is quite possible the fibromyalgia could be related. Or the fibromyalgia could be related to a pathogen that also was causing the depression. There is no way to really know unfortunately.. Hopefully you are not still experiencing depression.
Also, It is possible too much shock therapy could cause chronically low stress responses and CFS like symptoms. Perhaps you should have a 24 hour cortisol test if this is a concern
Here we go again. How does this explain “sudden on-set”? Some can tell you what day they became sick. Other’s, including me, were a part of a group that got sick, such as at Incline Village, and so on.
Just about all complain of Gastro issues in the American model. And, it may very well be contagious if one has all the other genetic, immune and stress components as shown in whole families becoming ill. Let’s not rush to judgment, till the jury is in! i.e. Lipkin for one
What about DR Lerners protocol??? Come on guys, buck up! RP
Good question.
I think what happens is that we get hit by a very virulent infection, when our immune system is down. Both factors are necessary.
Then, the infection creates some sort of permanent damage to parts of our brain.
Andrew Lloyd et al proposed this several years ago. It’s the “hit and run” theory, and I am very confident that it’s right.
Lloyd does not think CFS is perpetuated by a virus. I totally agree.
Researchers are wasting time and money – and our lives – by searching for viral causes.
I came down with CFS as sudden onset. My brother and I both got a very nasty virus. He recovered, I didn’t. I was highly stressed for several months prior, he was not. I think I got CFS because my immune system as down, his was strong enough to fight the virus in a manner which meant it didn’t damage his brain.
It would be very nice – and important – to know why and how CFS is triggered. But its more important, in my opinion, to know why CFS is perpetuated, and try and address, if not to reverse, the problem.
The issue lies in the brain, and I’m confident if research focuses there we will find the answers. But if we continue down the immune system distraction, I fear it could be a long time before we really make progress.
I think this model explains sudden onset very well, certainly in my own experience. I had some remissions and relapses in the early years of my illness, terminating in a five-year-long remission. By the end of five years, I was sure I was over this illness for good. Then it turned out that I had an old shingles lesion that was itching more and more, and when I had my doctor look at it, he told me that it had turned into a basal cell carcinoma, and it should be removed. That certainly sounded reasonable. A week later, I had it removed. Almost exactly 24 hours after that, at 3:10 p.m. on the afternoon of September 17th, 1998, my ME/CFS returned.
It was sudden onset.
One moment I was feeling absolutely fine. Then I felt a wave of weakness wash over me, and I immediately recognized this very unique feeling. “Oh no! It’s back!” I thought. Within two seconds, I had gone from feeling completely fine to feeling quite ill all over, including the muscle weakness, which was in fact my most prominent symptom.
What could cause all the muscles in my body to go weak all at the same time? Only one thing travels that fast in the body, and that’s nerve impulses. From this experience and a number of others, I always knew that ME/CFS was fundamentally a neurological illness originating in the brain.
As for what caused this neurological illness, having had shingles meant that I had varicella zoster virus hiding out in my nervous system. The removal of the lesion apparently reactivated the virus, and herpes zoster is known to cause encephalomyelitis. After one day, the reactivated virus (which would not have to spread the way a newly acquired virus would) did enough damage to my brain to cause functional problems. It’s a bit like a rat chewing through an electrical cable; the rat may chew for hours with no apparent effect, but when the rat actually chews through the cable, the power to a whole building may suddenly go out in a single moment.
For these reasons, the work of Dr. Jay Goldstein always appealed to me, as he also pinpointed the heart of the problem as being in the brain. More than that, he was fantastically successful in his treatments. By the time he retired in 2003, he was able to make 97% to 98% of his CFS and fibromyalgia patients asymptomatic, usually within a few days. And his theory matches up perfectly with that of the Japanese doctors, though he doesn’t go into the detail that they do. Specifically, on page 14 of “Betrayal by the Brain”, Goldstein says:
“Chronic Fatigue Syndrome is a disorder or the management of sensory input by the brain. Information from inside and outside the body is misperceived, resulting in inappropriate sensations. Touch can be painful, odors can cause illness, climbing a flight of stairs can be like climbing a mountain. If input is dysregulated, output will be also, because the brain will make regulatory decisions based on improper ‘data processing'”.
It is the last sentence that seems very prescient (as does much of Goldstein’s work); he is effectively implying what the Japanese doctors are saying, although without the detail. And this is in a book written 18 years ago. It is really a shame that in all that time, no one has followed up on Dr. Goldstein’s work.
However, he did leave behind the one piece that many people have commented is missing from the Japanese work – a practical treatment. Between “Betrayal by the Brain” and its successor, “Tuning the Brain”, Goldstein describes a system of what he calls neurosomatic medicine to successfully treat almost everyone with these problems. Goldstein’s work is highly technical – too technical for most doctors – but it contains a working approach that is continually being vindicated by new studies in the field.
I used to be a patient of Jay Goldstein and I don’t think he had anywhere near a 97%-98% remission rate. Where did you get that statistic? Also, Goldstein “retired” in 2003 because otherwise he would be forcibly retired by the Board of Medical Examiners. This was after a patient complained (correctly based on my experience) that she was never informed by Goldstein that he was experimenting on patients.
In the Preface to “Tuning the Brain”, Dr. Goldstein states: “During the past five years I have significantly expanded my therapeutic armamentarium to the point where I can help almost every patient.” Later in the book, he mentions that there were currently only 2% or 3% of his patients that he couldn’t help, and that he was able to make the rest asymptomatic. Usually this happened within a few days, but sometimes it could take weeks or longer.
It is important to note, as he does, that this statement applies to his success rate at the time the book was written, which was shortly before his retirement in 2003. His success rate had been gradually climbing since he first started treating CFS in the mid 1980s; it wasn’t until the late 1990s that his success rate started to approach what he described.
As for experimenting on patients, although it might appear to someone unfamiliar with his work (including many of his patients) that this was what he was doing, if you read his books carefully, you will see that he was following a very well-defined protocol based on solid theory and the best available understanding of each drug’s mode of action, which is a lot better than most doctors I’ve seen do. He always complied with FDA regulations, and although his use of many drugs was off label, this is perfectly legal, and in fact (as he points out) 40% of all drug prescriptions are for off label use.
As for his retirement, Dr. Goldstein practiced medicine in a very unorthodox style, and because of this, and because everyone expected to be cured due to his reputation, from time to time he would be sued for malpractice, and other patients would complain to the California Medical board (including patients whom he never treated, and patients who got better under his treatment.) He never lost or had to settle a lawsuit. One complaint to the California Medical Board from two patients he helped took nine years to resolve, but eventually all charges were dismissed. Please see “Tuning the Brain” for more details.
The ruling by the California Medical Board says nothing about experimenting on patients. The one relevant sentence that sums up its decision is as follows: “Respondent acknowledges that he suffers a neurological impairment that affects his ability to practice medicine safely.” In “Tuning the Brain”, Goldstein describes a recent serious neck injury, though he also describes his recovery. He may have relapsed. Or this may have been yet another spurious complaint to the board, and Goldstein, who was continually operating on the verge of bankruptcy despite a three-month waiting list, simply did not have the resources to fight it. I have been unable to find any publicly available information with further details.
I agree with you about Goldstein. He was WAY ahead of his time.
And it is a tragedy that work on the brain in CFS has been so long coming.
At least there is some promising progress from several researchers now.
What an amazing story Steven – very compelling. How to explain the acute onset is a fascinating problem. I’m surprised more researchers aren’t interested…
Time will tell and it may be not be the entire picture but I think Goldstein was right
“Chronic Fatigue Syndrome is a disorder or the management of sensory input by the brain. Information from inside and outside the body is misperceived, resulting in inappropriate sensations. Touch can be painful, odors can cause illness, climbing a flight of stairs can be like climbing a mountain. If input is dysregulated, output will be also, because the brain will make regulatory decisions based on improper ‘data processing’”.
Thanks for the quote.
I could never make it through Goldstein’s books – they’re so complicated – but I think I should try again.
I am not clear about whether the “overuse leading to shutdown” syndrome of this hypothesis, is intended to refer to actual physical over-use.
I believe it will be related to “flight or fight” stress response “overuse”, not actual physical over-use at all.
“Over-training” per se is not something that affects anyone other than a very few wannabe athletes. I don’t believe that everyone with CFS will have got that way by being a pathological over-trainer.
I have fibromyalgia myself, not CFS, but the differences and similarities are not 100% clear yet. I definitely have found that once you have the malady, your threshold for “over-training” is very low indeed. The only way I have been able to use physical exercise as a means of improvement of my condition, is by rationed doses of a wide variety of exercises targeting different muscle groups. Exercise machines in the gym are the way to go, plus a little swimming and a little walking. A little bit of everything, and not a lot of any one exercise.
But keeping the muscles restored with a routine of stretching, spas, massage, topical medications, etc, is also important. One discovery I believe I have made is that muscle stretches are far more effective if done in the hot water of a spa pool. Therapists I visit occasionally are very impressed with my improvement over the last 12 months, in limb mobility.
What else might have helped? Going on the Atkins diet, knocking carbs out of the diet. Balancing the supplements to compensate for the loss of nutrients has been important, especially the electrolytes to keep muscle cramps at bay.
What I am wondering is whether my condition was not helped, to say the least, in that my own methods of trying to cope with heavy stress loads in my life – and for years I had undiagnosed fibromyalgia that I was trying to fight through the pain of – involved massive doses of cycling as my preferred mode of exercise (I was quite competitive locally at one time). I now suspect that this made my condition get worse, with actual damage to muscles that never recovered between doses of exercise.
But my first piece of advice to the whole world is – don’t allow yourself to be maneuvered into situations of unfair chronic stress in your life; unrelenting periods of most of every day where you are wound up and on edge, as if you are fighting in a messy war against terrorist insurgents in a dense urban environment. There are jobs like that. The whole professional discipline of organisational management and occupational hazard management and the legal frameworks surrounding them, need to be more deeply involved in why people get fibromyalgia and CFS. One of my regrets now, is not suing my employer when I was diagnosed with fibromyalgia, after years of disagreement over the stressful nature of the whole way my job was designed; and a related regret: not being wise enough to quit and find something else as soon as it became obvious in the early stages that stress was going to be a problem. Once your suspicions that it is a problem have been confirmed by diagnosis of a stress-related ailment years later, it is far too late to undo the damage.
Thanks Phil,
My experience with ME/CFS ironically is that prior to it I was not in a stressful situation but afterwards being wound up and on edge is par for the course for me; it’s the water I swim in and I certainly don’t understand it. 🙂
Other research by these same authors indicates that the fight or fight system is activated in ME/CFS and one of the things they suggest is doing things to turn off the alarm system in the body.
Not an easy thing to do, for sure…
Spot on. I have the same regrets!
Me too.
Interesting.I had a recent Cat Scan which showed a non acute shrinkage of the prefrontal cortex area, wonder if this ties in with the Japanese research
I would think it would fit perfectly. If that area is damaged your brain may be activating the fatigue enhancing pathway again and again.
It’s my understanding that a shrinking prefrontral cortex or cerebral cortex? is par for the course with ME/CFS. Didn’t I read that here, somewhere?!!?
yes let us know more about SMR & WHERE TO GET IT….thanx to all!
Fantastic information. Thank you Cort, yet again.
My questions would be
How sure can we be that it is still not a viral, bacterial etc effect on the body which results in the brain ‘driving’ the body in that very specific conserved way?
A story that sticks with me is of a young boy who was afflicted with an extreme behavioural change after a dosing of antibiotics. Seemingly normal beforehand. Sever autistic tendencies thereafter. Naturally to have been given the antibiotic he must have been carrying some sort of infection. Did the infection or the medication cause the change? Who knows!
His mother some years later noted that subsequent doses of other antibiotics somewhat corrected his behavioural traits and he was more ‘normal’ whilst he was taking them. The antibiotics were not an ongoing treatment option, due to their strength. But obviously the ‘invader’ in his system responded to the meds by going into hiding until the meds were withdrawn. At which time they reemerged with a vengeance. But, during the use of antibiotics his brain obviously functioned more efficiently.
So, would treating the identified brain changes in CFS/ME sufferers result in a cure? Or potentially just a pause?
Any ideas?
They really don’t get into the causes here but they do – based on their neuroinflammation study – believe activated glial cells/astroctyes are present. Since those cells direct the immune response in the brain – surely an infection is a possibility.
Brilliant article ,Cort.
Thanks so much for making this information accessible to us.
The brain is not separate from the rest of the body, especially the immune system and the gut brain that responds to emotions and the enteric nervous system that works with the brain in the head.
Everyone knows an emotional event is felt in the gut and if there are gut problems the whole body can collapse.
Seven years ago I wrote in my book that one can not have CFS without gut and immune issues, whether known or not. Nothing has changed my mind since. RP
Can an MRI see this damage in the brain Cort or some other type of imaging so we can see that it is a reAl illness?
MRI’s and other types of brain scans are showing damage in these areas. Some find white matter drop out, some show grey matter drop out.
We are losing sight of the genetic, autoimmune aspect of the research and the disease. How does the Japanese research relate to Dr. Isabel Babao’s research at the Simmaron Institute? (link below)
My sister & I have had CFS since we were very small. I don’t know if there was a viral trigger, or what virus it might have been. I do remember my sister have two severe bouts with Roseola, 1. at about 9 months, and 2. at about 18 months. Roseola isn’t a virus I’ve ever seen associated with CFS. My sister & I don’t think it’s the specific virus that is important, but rather the autoimmune reaction it engenders.
Could the autoimmune reaction, or the associated inflammation, cause the malfunction in the fatigue circuit?
My sister & I know the autoimmune reaction is a major portion of what makes us sick. Our father had more than 1 autoimmune illness, and our mother has at least 4. Studies have shown that this means my sister & I have at least 4 times the likelihood of having an autoimmune disease. (When both parents have an autoimmune disease, their children’s chance doubles. Then the child’s chances increase again every time one of the parents are diagnosed with an additional autoimmune disease.)
I think this is supported by the high percentage of fatigued people in Japan – possibly 33% of the population. Japan has a much smaller gene pool than those in North America or Europe. They are concentrating the autoimmune genetics.
Kim & Kelly Derrick
Link to Simmaron Research
http://simmaronresearch.com/2014/06/simmarons-next-immune-study-wheres-weak-link/
Sorry, it’s Dr. Isabel Barao.
Kim Derrick
I definitely agree!! Thanks for the link to the article. I have no idea what the answers are but it seems very clear to me both from my own family and hearing many other stories that there is a genetic component and I have said all along through our journey that there has to be an autoimmune component. My kids both have CFS , and though not officially diagnosed there are clearly at least two others with it on the maternal side of my family and one with fibro. There is extensive autoimmune history on the maternal side of my family, I have at least two autoimmune diseases, and my spouse also has one. It’s always been amazing to me when chatting with others affected by these illnesses how common it is to hear of the autoimmune issues in their family history, both immediate family and further removed. I have always said that potentially a lot could be learned by studying family histories of patients with CFS, fibro, etc.
Clearly it’s complicated and I do believe there is also a brain component involved in all of this. There also seem to be different triggers of the full-blown condition. My daughter had what appeared to be sudden and certainly severe onset after back to back viral illnesses. It would be hard to deny that the viruses did not have something to do with the trigger and I do believe they did though they were also clearly not the underlying cause as in retrospect there were also much more minor signs for at the very least a couple of years prior to the debilitating symptoms. On the other hand our son’s severe onset was gradual and there was no obvious triggering event other than being around the age of puberty. Again in retrospect, he had many, many signs that went back to a very young age. So in the same family we had very different onsets but clearly the same condition and in retrospect other signs earlier on. Regardless of what else is involved, I am always ultimately led back to my belief of underlying autoimmune hereditary factors.
Here we go again. Speculation, speculation and yeah… speculation 🙂 It can all be true or false. What causes this central dysfunction? I don’t think it the system is damaged in the beginning. This disease is reversabel in my opinion. If it was damaged you couldn’t have good days. I think.
there are a lot of assumptions and presumptions here by certain people. Firstly CFS is not like Major Depression. Several biological differences between the two illnesess have been found by researchers. CFS or ME as it is called in other parts of the world is a serious biological illness, encompassing immune dysfunctions, neurological dysfunctions, brain lesions, infections, endocrine abnormalities, cardiac abnormalities and mitochondria abnormalities. There has been a lot of talk about the brain and what may be causing the brain abnormalities. There are too many uneducated and poorly informed people making guesses and assumptions about this. My question is this – who has actually analysed brain tissues from the brain parts from patients, and determined what exactly is causing the lesions, the inflammation, the structural brain damage ? You need to establish this before you discuss the brain in CFS and ME.
The scientific research findings show that infections of the nervous system, brain, the immune system and the red blood cells play a major role in ME and CFS, and that these can cause a wide variety of symptoms. Please read http://www.me-ireland.com/listing.htm
Tests must establish exact biological abnormalities, dysfunctions, and infections present in the patient before applying any medical treatments and dietary changes.
Dear Yasuyoshi and WatanabeMasaaki Tana,
I wish to reply to your paper
A new hypothesis of chronic fatigue syndrome: Co-conditioning theory Medical Hypotheses Volume 75, Issue 2, Pages 244–249, August 2010
Your paper neglects to mention what causes the brain lesions, the inflammation, the dymyelination, and structural brain damage in several areas of the brain. Has any researcher analysed brain tissues from the brains of patients, and determined what exactly is causing the lesions, the inflammation, the dymyelination, the structural brain damage ? The research so far, shows:
infections are occurring in the brains and nervous system of subgroups of CFS patients.
infections of the immune system is occurring. These include mycoplasma, lyme, viruses, bacteria.
the immune system is inflicting inflammatory damage in the brain and nervous system
infections of the red blood cells is occurring, and this is causing these cells to form abnormal shapes. This is affecting the delivery of oxygen and nutrients to the brain cells. This can cause the death of brain cells and neurons
Evidence: http://www.me-ireland.com/listing.htm and http://www.me-ireland.com/scientific.htm
These factors can cause the motor cortex, the frontal cortex, the basal ganglia, the dorsal root, limbic system, thalamus, anterior cingulate cortex to malfunction or function poorly. This has multiple domino effects on the body.
Could you please investigate the causes mentioned above. When we identify causes, we can develop specific tests, and establish the exact biological abnormalities, dysfunctions, and infections present in the patient. This will be used to apply medical treatments and dietary changes.
I look forward to corresponding with you.
Best Regards,
David Egan.
Sent: September 5th 2014
No. The issue is not being caused by chronic infections. A highly virulent infection in susceptible individuals damages the brain / cns. The virus leaves, the damage does not. It’s a hit and run.
I don’t think we need another 25 years pursuing the futile infection path.
May be another argument for my favorite name for this, Neuro-Immune Metabolic Failure.
Re: SSRI’s, see Dr Cheney’s cautionary article outlined here:
https://www.massmecfs.org/resource-library/9-treatment/117-x-dr-cheney-warns-against-long-term-use-of-ssrls-and-stilmulants
Upon reading this, I discontinued Prozac daily, and only use it when excessively emotionally labile. Works well so far on a PRN basis. (Had taken it daily from 1980 to 2018 and no MD thought to stop it).