

She’s had chronic fatigue syndrome (ME/CFS) for twenty-eight years and has left no stone unturned in her attempts to get well. She’s traveled widely and seen some of the best ME/CFS doctors in the world. Despite being connected to the hilt in the ME/CFS, her results have been all too familiar; her health has improved a bit but she, a former fitness buff, has never been able to exercise.
She’d had a really tough year. Multiple surgeries including a gall bladder removal, multiple emergency room visits and a mysterious drug reaction had laid her as low as she had ever been.
Many people might have given up after that (and several decades of mostly fruitless searching) but last year there she was in a pulmonary specialist’s office with a catheter in her arm working away on an exercise test.
Her goal – to determine if the latest hot topic in ME/CFS – mitochondrial issues – were it for her. It turned out that they weren’t – her mitochondria were working fine. Nor, despite the sarcoidosis she had, was her lung capacity diminished – she still had the lungs of an athlete.
Her autonomic nervous system, however, was decidedly off. Her heart was beating way too fast and her blood was pooling in her legs instead of getting pushed back up to her heart, leaving her heart without much blood to pump. Her doctor, David Systrom at Brigham’s Women’s Hospital in Boston, turned to her and suggested Mestinon (pyridostigmine bromide). It’s helped, he said, with fatigue in patients like you have.
Mestinon turned out to be something of a miracle for her. She took too much at first – and had some rather drastic side-effects – but then ratcheted it down and then back up again.
Now she’s taking 180 mgs/day – which is on the lower end for people with myasthenia gravis. She hasn’t been able to exercise without paying for it for almost three decades, but within a couple of weeks she described suddenly feeling like “going for a run” – a feeling she hadn’t had in decades. She was tired afterwards but the dreaded PEM never materialized.
Then she went cross-country skiing—one of the most energy-intensive exercises. She’s now running 3+ miles a couple of days a week and working out in the gym. She has one side effect that’s apparently caused by the medication: sometimes, after exercise, she feels lightheaded.
Other symptoms improved. Her sleeping pills are working better and she was able to cut down her sleep by an hour or two a night. She’s able to work full days. Much of her alcohol intolerance has disappeared. Her very high resting heart rate has returned to normal. She’s not healthy but she’s improved enormously and she can exercise (!).
Imagine her shock when she learned that the drug that has done so much for her has been around for decades. It’s even prescribed for the orthostatic intolerance she has, but until Dr Systrom, no one had ever mentioned it.
Systrom is an interesting figure. He doesn’t appear to be interested in ME/CFS per se, but is very interested in exercise intolerance and is apparently bumping into ME/CFS patients from time to time. He’s at the same Boston hospital – Brigham and Woman’s Hospital – as Dr. Komaroff . (I believe but am not sure that a graduate student of his presented an abstract at the San Francisco IACFS/ME conference. )
I know of one other ME/CFS patient who has seen him. She, too, had preload failure and no mitochondrial issues but didn’t respond to Mestinon. Systrom is also connected with Dr. Oaklander who is doing small fiber neuropathy studies in FM.
Mestinon (Pyridostigmine bromide)
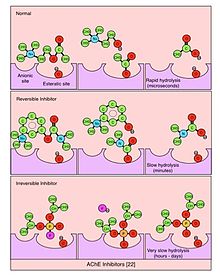
Mestinon is a cholinesterase inhibitor that stimulates the parasympathetic nervous system by inhibiting an enzyme called acteylcholinesterase that breaks down a crucial PNS neurotransmitter called acteylcholine. Taking Mestinon should result in more acetylcholine availability and more PNS activity – just what the doctor ordered for ME/CFS.
(Ironically Mestinon is produced by Valeant Pharmaceuticals – a poster child for rapacious price gouging in the pharmaceutical industry. Valeant’s former CEO is in jail and it’s under investigation from Congress, federal prosecutors and the Securities and Exchange Commission for its practice of buying up old drugs and raising their prices astronomically.)
Mestinon is primarily used in myasthenia gravis (MG), an autoimmune neuromuscular disease characterized by muscle weakness and fatigue. MG is usually caused by antibodies that attach to and block the acetylcholine receptors at the neuromuscular junction. Blocking the receptors makes it impossible for acetylcholine to tell the muscles to contract which leads to weakness and fatigue.
Myasthenia gravis is similar to ME/CFS in that it occurs more frequently in women, but is different in that it usually causes muscle weaknesses that show up in such symptoms as eyelid drooping and difficulty swallowing. Still the fatigue and weakness problems between the two were similar enough to lead some Japanese researchers to suspect neuromuscular problems might be present in ME/CFS as well.
Their case study of three ME/CFS patients in 2003 suggested Mestinon might be helpful in ME/CFS. Each of the Japanese patients had a similar profile to the patient in this blog.
All three cases involved women with excessive fatigue whose extensive lab workup’s had been for the most part normal; clinical findings, blood chemistry, spinal fluid, cancer screen, urinalysis, stool, ECG, EKG, and motor conduction studies were all normal.
All displayed some evidence of EBV reactivation, however, and had mild autonomic problems (altered postganglionic sympathetic function and the heart rate response to deep breathing) and substantially reduced muscle activity (compound-muscle action amplitude at baseline).
Treatment with 30 mg of pyridostigmine bromide caused one young woman’s three year case of ME/CFS to promptly disappear, and her muscle strength to return to normal. After a month on pyridostigmine bromide another woman’s ten year problem with fatigue improved significantly with her “muscle-action amplitude” more than doubling. The last woman with 15 years of chronic fatigue syndrome experienced significant relief on the drug. The authors noted the “dramatic effects” Mestinon had on their patients.
The authors proposed that calcium channel problems perhaps caused by antibodies were impairing acetylcholine release at the neuromuscular junction in their patients. They suggested that Epstein-Barr virus may induce B-cells to produce antibodies which then cross-reacted with the calcium channels in the nerves. The inhibited calcium channels reduced acteylcholine release which in turn caused muscle weakness, fatigue and autonomic nervous system dysfunction.
They proposed that trials be done, but that was the last mention of Mestinon and ME/CFS in the scientific literature that I can find.
Orthostatic Intolerance and Mestinon
Mestinon, is also used to treat orthostatic intolerance. A large study (n=172) of postural orthostatic tachycardia syndrome (POTS) in 2011 found that Mestinon improved the symptoms in the 52% of patients able to tolerate the drug and 42% of patients overall.
Interestingly, among the most improved symptoms was fatigue (55% reported improvement) with palpitations, dizziness and fainting showing high rates of improvement as well. The most common side effects were gastrointestinal symptoms.
An overview of five Mestinon and orthostatic intolerance studies found that Mestinon improved “hemodynamic measurements” such as heart rate and blood pressure but could not conclude that Mestinon was significantly superior to placebo in improving symptoms.
A large fibromyalgia Mestinon/exercise study in 2008 was successful but not in the way the authors intended. Instead of enhancing HPA axis functioning, Mestinon appeared to assist autonomic nervous system functioning. The authors argued that this made sense given the dysautonomia that even then was clearly present in FM.
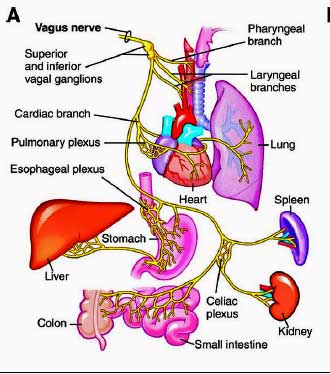
Mestinon did not improve pain or fatigue but did reduce anxiety and improved restorative sleep. The authors believed that increased vagal tone likely accounted for the improved sleep and they traced the reduced anxiety to improved heart rate variability – a measure of autonomic nervous system functioning. (Reduced heart variability – a function of poor vagus nerve functioning – has been associated with poor sleep in ME/CFS.)
(Exercise did improve fatigue, VO2 max, strength, etc. in the study but not pain levels. Noting that rigorous exercise increased pain levels a more moderate course of exercise was used. It included low-impact, nonrepetitive cardioaerobics training for 30 minutes, strength training for 10 minutes, flexibility training for 5 minutes, balance training for 5 minutes, and relaxation for 10 minutes 3 times a week. The intensity goal was 40–50% of the patient’s maximum heart rate or a perceived exertion of 10–12 of a total of 20).
Parasympathetic Nervous System / Vagus Nerve Stimulating Options
Vagus nerve stimulation is getting ever more interesting. We’ve covered surgically implanted vagus nerve stimulators and non-invasive forms of vagus nerve stimulation on Health Rising in past stories. Now there’s Mestinon, and other possibilities are present.
A bevy of drugs, many of which have not been tried ME/CFS or FM, can improve parasympathetic nervous system functioning. They do so either by blocking aceytlcholine from being degraded (e.g. Mestinon), or by increasing acetylcholine release, or by inhibiting sympathetic nervous system activity.
Reversible parasympathomimetic drugs include Donepezil, Edrophonium, Neostigmine, Physostigmine, Pyridostigmine, Rivastigmine, Tacrine, Caffeine (non-competitive) and Huperzine A.
Drugs that inhibit sympathetic nervous system functioning (clonidine, propranolol, atenolol, methyldopa prazosin and oxymetazoline) are far more commonly used in ME/CFS and FM.
Dr. Natelson is expected to begin a non-invasive vagus nerve stimulation study in Gulf War Syndrome patients in the U.S. soon, and it’s believed that the non-invasive vagus nerve stimulator will be approved for use in the U.S. later this year as well.
Conclusion
The short history of Mestinon use in ME/CFS, FM and orthostatic intolerance has had mixed results. Mestinon did very well for our patient and in the three case reports from the Japanese. It’s apparently one of the few drugs that can significantly impact fatigue and exercise in the right person. It can also help with sleep and autonomic functioning – as our case report of a patient indicated. It may also be able to impact mood.
It was helpful but had modest effects in FM and orthostatic intolerance.
The small Japanese study suggested the drug may be particularly helpful for people with EBV activation and autonomic nervous system issues. Our patient had both EBV (she’s currently on Famvir) and ANS issues, and clearly belongs to an ME/CFS subset that benefits from vagus nerve stimulation. In fact, vagus nerve stimulation is the only treatment that’s significantly moved the bar for her almost thirty years. Her doctor was not surprised that she showed benefit.
Mestinon clearly won’t help everyone but it doesn’t appear to have gotten as much attention as it could have in ME/CFS. Learn more about Mestinon.
- Plus – Learn more about Vagus Nerve Stimulation in our Resources section









Dr Grubb at University of Toldeo has been using Mestinon (and other drugs) for POTS for quite a long time. I thought the ME/CFS community knew about it’s use.
It didn’t work for me, but I’m now trying florinef & desmopressin. It’s too early to tell if it helps.
It’s fascinating the different ways there are to attack OI. If I remember correctly
Florinef increases blood volume
Mestinon increases acteylcholine activity
Midrodrine narrows the blood vessels forcing blood up from the legs
Desmopressin increases blood vessel tone by acting on adrenergic receptors
I think there are few others. It depends on where the problem is and there are plenty of possible problem places..
For OI I take licorice, which inhibits the uptake of cortisol; i.e. increases amount of cortisol. Takes a toll in boosting blood pressure but what do you do when caught between a rock and a hard place?
I think you may be confusing Desmoprssin and vasopressin? Desmopressin increases free water reuptake in the kidneys – a way of increasing circulating blood volume (similar to Florinef except that Florinef works by decreasing sodium excretion which results in water retention as well.)
I haven’t noticed Desmopressin helping my symptoms except for decreasing frequency of urination ( which can actually be a big help). I do have low vasopressin levels. Vasopressin does work as you describe on blood vessel tone, but desmopressin does not.
Thanks for very interesting article. I’m about to try mestinon. After 23 years I’d love a miracle, too!
Just reading this article now. A friend forwards your site in her news group. It is interesting to me. I have been on mestinon before. I mostly used it during the heat of the summer. I had acute side effects from it and did not get the relief this woman did. But nevertheless I may try it again when it warms up and see if it helps me feel better after seeing this. I have tried all those others you mention above. none worked on the POTS without side effects in me. the Florinef was awful. Made me feel severely depressed and I do not have that issue normally. I would never try it again. Weirdly the J&J vaccine put me in a relapse of CFS and caused some POTS symptoms. I have had CFS for 35 years so that similarity is what struck me about your article but POTS was not diagnosed till later. Wish I had known about this site earlier!
I would like to try this medication if possible and hopefully not too expensive. I’ve had severe M.E. 30yrs. under active thyroid b12 defiency IBS etc
I live in N.Ireland UK
Thanks
Is acetylcholine antibodies being tested for patients with ME/CFS?
Are you finding any help from Dr Grubb at University of Toldeo? Any one have ideas for a Dr iwithin driving distance of Cleveland Oh.
There is one physician at Cleveland Clinic that I’ve heard of for adults. Dr.Faroud? We had an awful experience with the pediatric doctor there.We ended up driving to Toledo to see Dr.Grubbs associate Dr.Karabin. It’s worth the drive
I see Beverly Karabin at Dr. Grubb’s in Toledo. I am on Mestinon as well and it’s significantly improved my ME/CFS and Dysautonomia/POTS. Also, she added Robinul for the profuse sweating/heat intolerance and 100 mg of Metropolol. Once I got on a Beta Blocker, my resting heart rate was 100 at times, went down to a normal 60-70 as my baseline which gave me a more wiggle room for my baseline which anything above 110 BPM sends me into a crash. I live in Michigan so, it’s a little bit of a drive but so worth it. Unfortunately, with our disease… until we get more physicians educated, travelling to get care has become a way of life.
May I ask if it worsened symptoms initially
I’m on day 28 of a small dose of Mestinon and my pain has intensified so much I can’t tolerate it M.E 35 year’s pots and since Covid it’s even worse which I did not think possible
Would clonidine help
Dr Frederick Jaeger is an electrophysiologist and Dr Robert Wilson ( NP is Kyle Shannon) in Neuro/ Muscular all specialize in this at Cleveland Clinic and are tremendous
Dr Robert Wilson at Cleveland Clinic, he is awesome
Dr Robert Wilson at The Cleveland Clinic
how did you get those drugs? did a doctor prescribed them? here in argentina it whould be impossible to convince a doctor to prescribe something they don´t know nothing about, as it is the case with every doctor here, they don´t knoww anything about POTS and CFS (bot of which I have)
Hi Laureano! Im having the same trouble. Im from Argentina too. If you want to talk, this is my email: noeliacsilvestri@gmail.com
Saludos!
Hi Laureano, I hope you have gotten answers and help, but if nothing, the person who shared this article with me was prescribed it by her neurologist. I’m not sure all would, even in the U.S. the advancements are not consistent, unfortunately.
I’m beginning it at the 30mg but the nausea is really bad – anyone able to push thru and find benefits on the other side ?
I tried mestinon several years ago as a trial therapy for my extreme exercise intolerance and lack of muscle endurance. My neurologist thought it was worth a shot but had no effect. I become lightheaded after the slightest exertion anyway so that was not a side effect of the drug. I do not have Orthostatic Intolerance. I had hopes that it would help but apparently I am not in that subset.
That would have been a nice subset to belong to…(I’m crossing my fingers). Thanks for passing that on, though.
My guess is that the vagus nerve does play a big role in ME/CFS but I imagine that it’s complex along with everything else and that there are different ways to attack it. I like the possible neuro-immune connection: EBV inspired antibodies whacking the receptors on the neuromuscular junction. If that was true a drug to attack those antibodies would be a possibility..
Great article. When I first became ill 4 years ago I was given the acetylcholine receptor antibodies blood test. It came back positive, 3 times I might add. I was sent to Myasthenia Gravis specialists in London who eventually concluded that because I did not present with outward physical characteristics of Myasthenia Gravis then I didn’t have it. I was never trialled on Mestinon. I have severe fatigue. I also have a slight droop to left eyelid and my left arm most of the time is so weak as to prohibit me lifting even the duvet covers at night. Interestingly I recently tested for EBV and results showed incredibly high numbers for activity. I have just returned from almost 3 weeks in hospital in Germany where I was given intravenous infusions of Acyclovir in very high doses 4 times a day for 17 days. Now I’m home I am on 800mg of Acyclovir 5 x per day for another 3 weeks. So far I have seen no improvement. This article has me thinking, perhaps I’m barking up the wrong tree and I need to go back to the Myasthenia Gravis specialists and ask for a trial of Mestinon. At the very least perhaps it can help with my poor sleep. I have a feeling from the described symptoms that I may be one of this subset of CFS/ME sufferers that could benefit. Thanks for bringing this to light Cort !
Really interesting Karin! You’re the first person I’ve heard of who’s been tested for those antibodies. Good luck with your search and please tell us how it goes.
Hi Karin,
So many years later… was myasthenia and Mestinon the right tree?
I hope you are doing well!
Hi Ana. No it wasn’t. BUT Dr. Pridgen and his 3 pronged medication approach did!
It took 7 months of being on the three medications before anything happened ( pretty much the time he’d told me it would take) and then I started to get better.
I am still to this day on the medication..but the trade of is I have.y life back. I do everything I did before I got ill.
I owe my life to that doctor.
Best wishes
Karin
Thank You so much for your answer!
Wow that sounds amazing. Is this the anti virals against herpes simplex?
I wish I would find sth that worked for me…
Enjoy your new old life the best you can and take care 🙂
The three medications are Valcyclovir / Celecoxib and Duloxetine at night for sleep. I tried everything. This was the ONLY thing that got me well.
Blessings to you. Don’t ever give up. X
Sorry just saw it thank you
What was your three drug approach ,
Valcyclovir / celecoxib and Duloxetine for sleep.
Thank you 😊
Is it possible if EBV antibodies are doing some whacking other antibodies might be as well? My EBV is not high but at last test my coxsackie ones were. Seems reasonable that any of the viral culprits could be doing the evil, right? I’m interested in a trial of this for myself!
There are a number of ways to increase vagal tone without medication, including certain forms of yoga, meditation and chanting, toning or singing. Even aparently bathing in cold water, at least splashing the face, will increase vagal tone. Sounds a little simplistic perhaps but after three years of practicing Kundalini Yoga and meditation I can say that it does work. I take Mestinon when I get weak and it does work, but since beginning this form of yoga I have been able to get back to work and have not needed a wheelchair or walker!
Thanks for passing that on Gabrielle. Very good to know 🙂
That is so true! The only downfall is that vagus nerve stimulation in this manner does not boost acetylcholine for the central nervous system (brain). If you suffer with brain fog, that may be worth considering.
Mestinon helped me immensely. It helped my POTS and muscle strength a bit. I tested negative for the antibodies. IF you test positive 3 times for antibodies – then you definitely have a form of Myasthenia Gravis…it is one of the dx I have been thru as I have a droopy eye when I am tired and was in a lot of discomfort behind my right eye. Since taking Mestinon, my eye is so much better. Turns out mitochondrial problems can also cause this droop- they are presently putting a lot of focus on ME patients who have immune dysfunction which leads to mitochondrial dysfunction.
Thanks Karen. Good luck with everything.
Fascinating article, Cort. I went to an orthostastic intolerance / blood pressure specialist for a while, but he never mentioned Mestinon. Will have to find out if it’s available in Australia.
Just checked, and it’s available in Australia for myasthenia gravis treatment. Finding a doctor to prescribe it for ME/CFS is another question!
My Rheumatologist gave me my script which I just started today. I told him it is helping some people with ME/CFS and he agreed to let me try it. He just told me to take 30 mg 2x a day. But a friend who just started it takes it in the am and at noon. Does anyone know the correct way to take it. Thanks and the best to all.
Fiona, were you able to find a specialist in Australia that was willing to prescribe Mestinon for CFS?
My GP in Melbourne was happy to prescribe Mestinon at my request. I found I had to start at 5 mg and work up, otherwise it made me very sleepy. It takes me about a week to adjust to each increase in dose. Currently on 30 mg twice a day and intend to keep increasing to find my optimal dose. The effects only last a few hours, so I currently take it morning and early afternoon, but will take it 3 times a day as I increase the dose. I had been totally housebound due to a flare-up of orthostatic intolerance for the past 9 months, and the Mestinon has definitely improved that since I started it 2 months ago. I ventured out for the first time a week ago (to the GP and chemist!), and did not become light-headed.
Mestinon is not available on the PBS except for myasthenia gravis, so I have to pay the private price.
Thank you for dosage info – I’m trying to start at 30mg and was so nauseated I am nervous to try again – maybe will start even lower
Not quite sure where to jump in. I am in NZ with fibro, Dissassociative connective tissue disorder and Chronic fatigue.I have some sort of weird muscle thing , where on load ie at the gym, walking up hills, or jumping my horse they seem to give out and don’t re energise. Along with fatigue.
I first read this article and discussion about 2 months ago. I started Mestinon, prescribed after showing my Rheumatologist this article, in September.
I started on 60 mg twice a day and have worked up to 60 mg three times a day. Only side effect is I can now go t the toilet almost once daily. A huge benefit me after years of extreme constipation.
It is definitely helping me. I have many more hours of useful time. I remain active and alert. My brain and ,even, my eyeballs feel more alive and somehow better.
YesterdayI decided to see if I can reduce my prednisone .i am on 7.5 mg daily. Now taking 5 mg.
In any case , it appears to be working really well.
Not a miracle but really really positive.
Have you been tested for small fiber neuropathy? The gold standard test is a skin punch biopsy to test nerve fiber density.
That’s great to hear Robyn. Thanks for sharing your experience and good luck on your health journey.
I was tested once for Myasthenia Gravis when I first became disabled, and it was negative. I didn’t know about the 3 times protocol. My right eye droops and I’m very weak. I’ll ask for a trial. // I was bowled over by Dr. Systrom’s presentation at the NIH; first time I’d heard of his research. Is there an obtainable published article by him that I can show my pulmonologist and cardiologist? I found an abstract on a rat study but couldn’t find anything like what he presented at the conference.// Finally, yes Cort thank you so much for this great article on the conference.
I have ME/CFS with autonomic dysfunction and had a neurologist prescribe Mestinon early on. Unfortunately,it had no impact on my symptoms. I don’t want to dissuade anyone from trying it, tho – it sounds like it’s beneficial for a subset of us.
(By the way, since it’s mentioned here and in case it’s helpful for anyone, want to add that I reacted very badly to atenelol – greatly exacerbated wooziness — and switched to propranolol for tachycardia and found it much easier to tolerate. For whatever that’s worth.)
Yes, atenelol was also bad for me – it made me even more tired, if that’s possible. Makes sense, because it slows your heart rate, and I think I already have low blood volume.
Hi! Thanks for posting this article.i may have to ask for Mestinon due to at least 2 relevant antibodies present at abnormal levels. Striated muscle Abs & voltage gated calcium channel antibodies. Interesting to read that calcium channels play a part in the post exercise fatigue. It’s one major issue that Florinef & Midodrine are not able to help with.
I also take propranalol for tachycardia. Actually started off taking it for essential tremor, a classic use.
The action of this drug concurs with Dr. Diana Driscoll’s theory about low levels of choline and low functioning vagus nerve functioning in persons with POTS, MCAS & EDS. I have noticed some benefit from taking phyosphatidyl choline but not enough to exercise on a regular basis.
Want to mention that I have read several articles by persons other than D. Driscoll mentioning the ideas of low choline and decreased function of the vagus nerve, with regard to mechanisms involved in POTS and MCAS, so feel it would be incorrect to ascribe this idea to D. Driscoll’s “theory” alone. (If you google “POTS and low choline” for example, you will see what I mean.) With the same ideas being described by different people around the same time, it is impossible to say this “theory” was first devised by any one of them.
Here is one example article: http://www.science.gov/topicpages/p/postural+deficiency+syndrome.html
You will notice careful citations to people doing a study on low choline in POTS and none of these happen to be Dr.Driscoll.
That’s good! That means more brains on this and that’s a good thing.
I think the aspects getting missed in others’ work in choline is that choline is not sufficient for the production of acetylcholine, nor does choline cross the blood-brain-barrier to help with acetylcholine needed by the brain (brain fog anyone?).
Instead, we focused on what our bodies needed to boost acetylcholine to be sufficient to stimulate the (postganglionic) portion of the vagus nerve PLUS to provide acetylcholine for both the brain and the muscles (central and peripheral nervous systems).
Choline, mestinon and similar compounds are not sufficient to do this, nor do they provide the “work arounds” needed for those of us with difficulties in the pathway of acetylcholine production. Vagus nerve stimulation is not effective if the preganglionic portion of the vagus nerve is affected. As patients, we need something that pulls everything together to work around these issues. It’s so much more than a choline issue. Does that make sense?
This unique approach, hitting all of these issues affecting us just recently resulted in the award of a patent. I think being a patient and mom of affected patients helped us to dig deep for answers. I hope it is hugely helpful for others, too.
🙂
I had this test done & see the same doctor. The test was very invasive, difficult & I don’t recommend anyone go through it! But it does show telling results. I have POTS and this test was able to confirm that I have cardiac preload failure(very little blood getting back to the heart during exercise). But for me, it also showed that I have significant mitochondrial dysfunction. This is determined by the measurement of blood gases during exercise. I don’t know why some ME/CFS & POTS patients have mito dysfunction & others don’t. Mestinon helped me a little bit for about 4 months. Then i started developing side effects from it & had to take a break from it. My POTS did seem to get a bit worse off of it, so i restarted it. Unfortunately when i restarted it, it didn’t seem to do a thing or help at all. Bummer. I’m guessing it is more effective for patients with POTS/OI who don’t have mito dysfunction.
How interesting Anne!
Is it the catheter stuck in your arm that makes it difficult (other than the fact that it’s a maximal exercise test, I guess.)
And you have mitochondrial dysfunction as well. Did they recommend anything for that?
Dr Grubb has also found mito dysfunction in POTS patients. He usually doesn’t test for it though, I believe because there aren’t many treatments. He recommended I try L-carnitine, CoQ10, and ALA. if they help, I probably have mito dysfunction.
I’m not sure why more people don’t know about Dr Grubb. I think he’s the most prolific POTS researcher & author.
They put 2 catheters in you. The one in the arm wasn’t that bad but the worst part was putting a catheter in your neck and threading a tube from your neck all the way into your heart. That’s how they measure your blood pressure within your heart during exercise. I found the insertion of the neck catheter to be really awful & very anxiety provoking. Then you had to exercise on a bike intensely(as hard as you can) for 5-10 minutes. Then you had to keep the catheters in for another hour or so as they kept taking blood to measure gases. The neck catheter was very uncomfortable to me & I was dying to have it removed asap. It would be much easier to just try mestinon rather than go through this test! I don’t think that my data was used in their study but the only thing that comforts me about going through this test is that they are using these test results to publish studies and prove that people w/ OI/POTS/”exercise intolerance” are not just de-conditioned(as some doctors tell us) & that significant cardiac preload failure is occurring. This is very technical but here’s the study they just published: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4860548/?report=classic
And this journal article which was written as a result of this study: http://www.journals.uchicago.edu/doi/pdf/10.1086/687757
I was referred to a mito specialist who recommended a few things: vitamin b complex, Alpha lipoic acid, Coq10, high protein/low fat/complex carbs diet, eating 6 small meals throughout the day rather than 3 big meals, meditating, optimizing sleep, gentle exercise(only as much as you can tolerate without crashing- i.e. go for a walk twice/week and do some upper & lower body muscle strengthening twice/week). Not much else you can do for mito issues besides supplements & lifestyle changes at this point. A new mito drug which has been in clinical trials is slated to come out soon but i don’t know if ME/CFS folks would be eligible to try it or if it’s just going to be for people w/ genetic mito disorders. I could get genetic mito testing done but it was going to cost $19,000 & it would probably end up being negative….no thanks! But the mito doc said, “i wish i had a million dollars to study you folks”. I hope she gets her million $ some day!
Wow..that one in the neck sounds really rough!
Stay tuned on the mitochondrial testing – something new is coming out in the next month or so I believe.
Was the mito doc referring to ME/CFS patients? I hope she gets her million too!
Thanks for the links…
What kind of Dr are people seeing to get tested for mitochondrial dysfunction?
This is a pulmonary specialist but Ron Davis and the Open Medicine Foundation are looking at the mitochondria from an entirely different angle – from the metabolites in the blood. I rather think they’re doing a much less invasive test 🙂
Hi Anne,
I’ve been scouring the interwebs to find stories of people who’ve done the invasive cardiopulmonary exercise test. If this message finds you, can I ask where u had this done? I’m scheduled for the test in two months and I’m having a TON of anxiety about it. I’m worried that it will be painful, and at the end, the information it provides will help the doctor far more than it helps me. I’m seeing Dr Systrom at Brigham & Womens in Boston. I’m generally in good health, but the breathlessness, vestibular disfunction and insomnia are now touching every facet of my life. Don’t know if I’d even take the drugs if they prescribed them. Also don’t know if the skin punch test is worth the scar. I already have a skin punch scar and would prefer not to have another. Have you done this test done for autonomic neuropathy too?
Dear Rachel, I did the test with Dr. Systrom, and am the patient that was helped by it so much. It is not an easy test but I am so happy that I did it. Mestinon is a pretty benign drug and you will know fast if it working for you or not. I call it my “insulin” because I need it to function at around a 80% level. Don’t worry about the skin punch test; it is minimal scarring. it is like knicking yourself from shaving. Dr. Oaklander’s testing is not as sensitive as Dr. Novak’s, Chief of autonomic neurology at Brigham and Women’s. I am happy to talk to you on the phone if you would like. Cort can connect us as he and I are friends.
Thanks Mona 🙂
Hi Mona. My daughter (college aged) was recently DX with likely ANS issues/dysautonomia by Dr Kyle Staller at Mass General who is a nuerogastroenterologist. We are on the waitlist for testing which is currently scheduled 12 months out. She was just put on Mestinon and thus far we are not seeing results. I would love the opportunity to understand your experience. I know you mentioned you would chat on the phone to another person (nearly 5 years ago) but I would love the same opportunity. If you are willing please let me know here. Thanks!
I just had the advanced cardio catheter stress test at Brigham and Women. It was uncomfortable, but not horrible. I could do it again if I had to. The doctor said that it was the only test that would have caught my dysautonomia. As I do not have any underlying conditions, I was hard to diagnose.
Wow…Thanks for sharing that Colleen. I hope the results will help!
I had both the CPET-3(Dr. Systrom) & 2-day CPET (Dr. Keller- Ithaca College) done in the past year. The 2 tests are informative and involve different levels of invasiveness.
These tests documented the dysautonomia. My target heart rate is 84 and staying below this has helped me to avoid the massive PEM I experienced since the onset of this illness in 2012 until September 2018. I was a passionate athlete throughout my life and today my only exercise consists of short walking coupled with daily recumbent bike without resistance 30” (range 5”-30” depending on HR)/day ranging 2.3 – 4.2 mph to stay under my target HR. My functioning while better than it was is 30% of pre-illness.
I tried Mestinon for 6 months & could not tolerate the severe GI complications I developed. I recently started Midodrine and seem to be tolerating it better. I am happy to discuss with anyone.
Thank you – the GI issues which I already have so to exacerbate them just one 30mg of mestinon made me so nauseated for two days
Btw, Dr Grubb is a cardiologist.
Dr. Grubb is extremely well known in the POTS community. He’s very hard to get an appointment with and not inexpensive either.
Greetings- I would like to follow up with Dr Susan Taylor Brown re her progress with Midodrine treatment.
I did contact you approximately 4 years ago re my almost instant recovery from CFS,severe to high level of functioning following my first Alpha Stim treatment. I maintained this level of functioning until I became severely ill with a respiratory virus.
Incidentally,I learned about the Alpha -Stim
device from an OT who had a similar experience . Is this a treatment your members are aware of …they should be.
Thank you,Joan Gibson,Retired Psychologist
I have FM with Dysautonomia (my docs are not good at differentiating what type, ‘I’ believe it is POTS, as to my potsie friends who know my symptoms), I have been using Mestinon for about a year now and it has made a huge difference for me. Most days I can be ‘upright’ longer, I never spend a whole day in my recliner / bed, I no longer have the shortness of breath that plagued me for ‘no apparent reason’ for over a decade (I kept being treated for anxiety due to that 😉 (my Xanax didn’t help my breathing). The best part to me though, is that my mind is clearer than it has been since 2000…it’s not excellent, I still can seldom drive my car, but, I can hold conversations with people without planning ahead for what to say, or for talking points. I’m now on 30mg three times a day and doing well. I had muscle cramps in my feet / legs at first (that’s gone now), the only side affect that remains is that my eyelids twitch, not all of the time, mostly for an hour after each dose. I’m very pleased with it.
Glad to hear that it’s made a difference for you Toni. The person in the blog is on 180 mgs/day – about twice what you’re on. That’s the upper dose for myasthenia gravis. Do you have any idea why they picked the dose they did?
Hi Cort,
I have OH/OI with CFS/FM and have recently been tested for ANS thru Dr. Oakley, neuropsyiologist at UW in Seattle. I had two major abdominal surgeries in 2010 and 2011 for blockages/adhesions in small and large intestines following hysterectomy for maignant endo. My symptoms developed after the last surgery, including gastroparesis, chronic constipation, fatigue and brain fog and cognitive issues as well. I am 49, and was once an avid runner and life long athlete and learner. Did I mention I also have chronic neck and back pain and tested positive for AS antigen which many family members have. I take Reglan, Lactulose, Adderall, Lexapro, have taken Midodrine and was recently prescribed the Mestinon at 30mg 2x day to start and increase to 60mg 2xday. I was so excited to finally try this drug and after 4 days I could not handle the severe stomach cramps, pain and overall horrible GI issues. At first it seemed to be helping my vagal tone and constipation and even the brain fog but then I was in the fetal position for about 5 days after I discontinued it. I had high hopes, my quality of life is very low as is.
My question is, should I try again with the Mestinon at a higher dose and ask for something additional for the GI issues or have there been further developments with new medications that may be available since this blog started?
I am on Team Inspire.com for gastroparesis patients with dysautonomia and Mestinon seems to really help many others. I am hoping there is something else for people in my subset I can talk to my doctor about?
Thank you!
Maren, I know of many people who start Mestinon at a lower dose and move up slowly in order to avoid severe GI distress. They start at 15 mg once a day, then 15 mg twice a day, then 15 mg three times a day, then 30 mg once a day and 15 mg twice a day, and so on. Some spend 5-7 days at each dosage, while others move up after 2 or 3 days. Some stay with 30 mg three times a day and some go up to 60 mg three times a day. Starting with 30 mg twice a day may have been too much for you to tolerate. But starting more slowly could work.
I’m not sure where the idea that 180mg/a day is the upper dose for myasthenia came from?
For myasthenia, I often take 240mg/a day in comparison (though no more than 120mg at a time).
I tried a non-invasive vagal nerve stimulator for a few months that my doctor had and gave me to trial. I found it didn’t prophylactically help any symptoms, but if I had myalgic pain as part of PEM, it did help with that. Interestingly, I didn’t find any reduction in migraine pain, which is what the device was marketed as.
Hi Belinda, I was wondering what brand the non-invasive vagus nerve stimulator was that you used? My understanding is that you really need to use it for six months to see if it is going to work. Did you have any side effects and what were they? It looks like Vanderbilt is going to do a trial with tVNS and I am wondering what exact tVNS is being used in these trials. There is one in Europe that has good peer reviewed studies showing efficacy but it is impossible to get in the States.
Hi Rita
What is tVNS?
I spoke to one company – can’t remember who – and they hope to have a non-invasive stimulator approved this year.
Belinda, tVNS means transcutaneous vagus nerve stimulator and it works by applying electrical stimulation in a part of the ear with something that looks like an ear bud: the vagus nerve runs into that area so one doesn’t need to have it implanted in the chest area. How did yours work?
tVNS is transdermal vagus nerve stimulation.
this is the tVNS device that has been tested the most, and it is approved in Europe for epilepsy:
NEMOS
http://www.cerbomed.com/Therapy-with-NEMOS-92.html
it is made in germany, and available in a number of european countries. (it is available via various NEMOS distributors who based in various european countries.) it is not available the US. tho i know some US folks have managed to get it either by going to europe to get it themselves, or having a friend who is visiting europe bring it back to the US for them.
it is about the size of an iphone and like an iphone it has an earbud. that earbud is what stimulates the vagus nerve.
it has some downsides:
– you are to use it for 4 hrs per day, with the hours spread out. that is a lot of time each day. (but you can do other things as you use it.)
– it cost about $3000, so not cheap.
– it has only one setting, the setting that it works for for epilepsy.
as cort and others wrote in earlier Health Rising threads/blogs/comments, some patients are not trying to get the NEMOS device but rather are simply buying a TENS unit ($20? $50?) and hacking it to be used as a tVNS. (a TENS unit is an over the counter electrical stimulation device. and from what i understand, that is really all the NEMOS device is, a fancy electrical stimulation device that has been tested and approved for use in epilepsy.)
from reading the comments about these hacked TENS units, it sounds like some are getting good results.
i have also heard of a few patients using the NEMOS device and getting some good results in terms of energy and less PEM.
i had my doctor email the vanderbilt team using tVNS for POTS. they are using their own tVNS, not one of the devices available on the market in the US or Europe.
Hi Rita
The device I used was the gammaCore, but I don’t think it’s been approved yet for use in the US (I’m in Australia). I had no side effects from it other than a tight throat while I was using it.
http://gammacore.com/en/healthcareproviders/
Belinda, can you please tell us which device you used?
Hi rrr
I used the gammaCore device.
http://gammacore.com/en/healthcareproviders/
Dr. Patrick Nemechek of the Nemechek Protocol for Autonomic Disorders uses trans-cutaneous vagus nerve stimulation. He has a website. After reading about all the studies that are just happening I am wondering about his use. It is legal, approved etc.
Any recommendations on good doctors for fibromyalgia in Melbourne Australia. I feel like I’m on a merry go round going no where but with huge holes in my pockets. I prefer a drug free approach if possible, or at least that not being the main focus.
Mestinon was one of the 23 main drugs that Dr. Jay Goldstein mentioned in his 1996 book Betrayal by the Brain. He had been using it on ME/CFS patients for a while by then. The theory and results associated with his use of this drug were basically the same as described in this article.
Thanks zzz – I forgot to mention that. If anyone want to see Dr. Goldstein’s top 23 drugs for ME/CFS they can find them in our Resources section here.
Cort, thanks for another insightful article. I have been housebound with severe ME/CFS for 37 years. In 1980, while still trying to get to a diagnosis, a neurologist wrongly thought I had Myasthenia Gravis. I was given Mestinon and my thymus was removed. Unfortunately I didn’t respond to the Mestinon.
But, on a side note, one interesting thing is that my thymus was significantly enlarged – the size of a man’s two fists, rather than pea-sized as it should have been at that age. The surgeon was astounded. It was something he had never seen before. I have always wondered if there could have been a link between this and immune activation early in the ME. If it wasn’t for the surgery, I would not have known about this.
Are you referred to Dr. Blair Grubb in Toledo OH?
The answer I found in the first comment: Yes.
This is fascinating! I have had limited success with other supplements I’ve been trying (will write you with more details in future), but what is still missing is everything that you describe this being good for!
I have found now that nearly every Rx on Earth has a rough herbal equivalent, so I did a search and immediately came up with Huperzine A as the apparent supplement version of Mestinon. People with MG who took Mestinon are saying it has the same level of efficacy for them, without the side effects. They mention using doses of 150-250mcg.
So, I found a well reviewed brand and will be rush ordering.
Be CAUTIOUS – there are side effects and interactions, some potentially serious, so do your research first. I will start on a low dose first and see if I can work up. For many, it sounds like at worst it just has no effect.
Many other people report vastly improved memory, sleep, etc. (many of these people did not have a serious disease, but took it only for memory help). But it sounds powerful, and has a long half life, so can build up – apparently it is best taken in cycles, with time off, maybe alternating months.
I’m going to give it a shot and report back if I have any good effects. I will probably start with about 50mcg first, or even 25 (depending on the style of the pills), just to make sure I don’t have any terrible reactions.
If this works, it would be all that I am missing, and I would feel cured. Even if I had that function back for a month or so before stopping for a break, I think it would help me a lot to regain my health. Any period of time when the body is working correctly is sure to be helpful to restoration of cells overall, I would think.
Sunshine, you have peeked my interest. Unfortunately it will be about the 7th miracle cure that I will be trialing in the past year. But I see Swanson’s has Huperzine A so I am going to buy some. From reading, I think 50 mcg would be at the top of the range that I would start with.
Lynn
Lynn, she has “piqued” your interest, not “peeked.” The words have entirely different meanings. I peeked through the window; you had your interest piqued.
“Lynn, she has “piqued” your interest”
Yep, Brain damage from the illness. thanks for catching it.
Good luck Sunshine! Please let us know how it goes.
Hi Cort,
Since people seem to still be reading comments to this article, I will give a brief update. I have been taking Huperzine A (Source Naturals – available on Amazon) for almost 2 full weeks now. I started with 25mcg, and have slowly worked up to today taking my 1st dose of 200mcg (not all at once – half at night, half in morning). It is definitely doing something major to my body. I caution you all to be extremely careful if you want to try it, because I think there is potential to get really sick. But going slowly, and going up only 25mcg at a time, has helped so I have felt weird but no extreme symptoms of vomiting or heart problems, etc. On me, it does not do any of the miracle things other “healthy” reviewers talk about. But it is most definitely affecting my sleep, how awake I feel, my POTS, how I think, my vision, how I feel emotionally… a lot of stuff. It is too early for me to make any claims yet or tell a success story, or in good conscience recommend it to people who are vulnerable. But, I will say that I have been experimenting with a lot of things together, and this seems to be the piece I was missing. So, for the moment, in combination with other supplements I am working with, I still appear to be headed back in the right direction towards remission. I promise still to give a full account for the website of what has worked for me, when I finally reach a stable place and know for sure what got me there.
For now, I would say for those who are desperate to fix POTS symptoms, to get refreshing sleep, or to be able to exercise without it killing you, Huperzine A (starting in very SMALL doses!) might be an important component in achieving those things. Be sure to support your body as much as possible, don’t just take a pill and start climbing a mountain because you think you should be able to. Listen to your body, rest when you feel tired, back off if it feels like it’s making you sick, and make sure you get a full range of vitamins and antioxidants, as well as sodium and water in you – especially if you have POTS. We never find the cure because we only work one side of the equation at a time, and exhaust part of our body that goes into overdrive while the other part gets no help whatsoever. I think to treat M.E. effectively we have to really come at it from a comprehensive perspective, and any little bit that supports the body in functioning more normally can help a great deal over time, as the body works to try to heal itself.
I am testing a lot of different things in different combinations, but some that appear so far to be significantly helpful include: Vit. B1, magnesium glycinate, potassium, 4-5,000mg sodium/day with about 96oz. of water, licorice root, hawthorn berry, sea buckthorn juice (not just the oil), huperzine A, yohimbe, ice wraps for head to reduce brain inflammation, thigh high compression stockings (other lengths cut off circulation), and an inversion table. (That’s just the short list, lol!) All of these things can have negative effects of certain people, or if used the wrong way, so I won’t go into further detail in this comment but please do some research before trying any of them yourself to see if they really fit your needs, and make sure they don’t interact with anything else.
I have tested hundreds of things, and have made serious progress. I have gone from being bedridden – vomiting and crippled with pain – and needing a wheelchair to get around (with doctors only making me sicker), to feeling close to cured. I promise to give more details when I know more. We are a vulnerable patient population and I don’t want to send people on expensive or detrimental wild goose chases if benefits are not going to be long-lasting and major.
Cort, in case you are reading this, I am the one who wrote you maybe 8 months ago to tell you about the remission I seemed to have created. I maintained that for some 3 months, relapsed for very specific reasons that I knew were coming, and am now thankfully in the process of recreating another remission – hopefully more fully and long-term this time around. I will update you when I know more and can be confident in the research I have done. I feel pretty confident that the things I have found will work for at least a large and desperately ill segment of the patient population, not just for myself.
Sunshine, based on your comment I bought Huperzine-A. It arrived yesterday and I cut the tablet into 4ths. I took 1/4 of a tablet before going to bed and slept through the night for the first time in a long time!
Took another 1/4 tablet this AM and am feeling more energetic. I am very hopeful this will help me!
Update – not only did I sleep through the night, I had a great bowel movement shortly after waking (earlier than usual) and then had ANOTHER (unheard of) shortly after that! This stuff WORKS (for me) and all of that benefit from One Quarter of a 200mg tablet!
Did it work? Mestinon works for me so really interested if natural works fornyou
Thank you for this post, Cort! The parasympathetic nervous system (and vagus nerve) has been greatly overlooked in the past. I’m glad to see more awareness!
What our research found, was that the majority of CFS/ME patients showed extreme deficiency of acetylcholine levels, which can affect the performance of the vagus nerve, but can also affect the central nervous system (brain).
Unfortunately, Mestinon does NOT cross the blood-brain-barrier to help with acetylcholine in the brain (needed to think and for short-term memory). And although it slows the breakdown of acetylcholine, it does not increase levels by providing the building blocks of acetylcholine needed by many of us with genetic defects in the acetylcholine pathway.
Instead, we came up with Parasym Plus to do what Mestinon cannot. It effectively stimultes the (postganglionic portion) of the vagus nerve, but also increases levels of acetylcholine needed in the brain, and for the patients with genetic difficulties with the production of acetylcholine. Awesome. I’m happy to say that Genetic Disease Investigators, LLC has just been awarded a patent for its discovery.
It is available without a prescription — one of our goals so we could help ourselves if our doctors are not up to speed on the parasympathetic nervous system.
My lecture to the Univ. of Houston is here:http://prettyill.com/videos/watch/pots_what_have_we_been_missing_part_2
Our white paper is here: http://https://chronicdiseasedigest.org/
It’s sold here: https://vagusnervesupport.com/
I hope it is hugely helpful for us all. As you know, it was a necessary component of my recovery and that of my kids.
Hang in, my friends,
Dr.Diana
Thanks Diana,
I had a feeling this situation was going to be more complicated than presented here.
We’re going to cover Diana’s hypothesis next week (hopefully) in a blog.
Diana, where is the proof that mestonin does not cross the blood brain barrier. i saw your white papers but was unable to locate proof. thank you
Dr. Diana: Could you please re-post the link to your white paper? That link is not working. Thanks so much for creating this supplement.
Sure! So sorry…
https://chronicdiseasedigest.org/
Dr. Diana
Thank you so much for this info and your video, fascinating. Your description of feeling as though you’d been poisoned is the one I have used most often in the last 4 years to describe how I feel to doctors. I’m almost hoping this is a lightbulb moment for me. I tested positive on the acetylcholine receptor antibodies blood tests. Does this mean I am acetylcholine deficiant ?
Thank you for your kind words, Karin. Yes, I felt so vindicated concerning the feeling of being poisoned. 😉
If you tested positive for acetylcholine receptor antibodies, you may have autoimmune autonomic gangliopathy. Immunosuppressives can be important for this condition. You may or may not be low in acetylcholine (did you see the list of symptoms of low acetylcholine in my lecture at U of H? That may help!) It’s here: http://prettyill.com/videos/watch/pots_what_have_we_been_missing_part_2
If your receptors are affected, boosting acetylcholine helps — you want to continue to stimulate what few receptors you have. If you are low in acetylcholine, boosting acetylcholine is also necessary — so it’s a win-win situation.
I hope it is hugely helpful for you!
Thanks, not heard of “autoimmune autonomic gangliopathy” so will look into that. Yes, I pretty much have most of the symptoms that were mentioned in your video. This page here https://vagusnervesupport.com/top-ten-symptoms-of-low-acetylcholine/ shows the ‘top ten symptoms of low acetylcholine’ and I have them all accept dry eyes. I also have myclonic jerking that at times is so bad it literally jerks me awake. I seem to remember this being a symptom also.
I have just ordered a bottle of Parasym Plus (they ship to the UK) but having looked closer at the ingredients I note it contains acetyl-L-carnitine, which I have had bad reactions to in the past. How soon could one expect to see improvement on Parasym Plus if it were to work?
Karin, Everyone is a bit different (genetically and in their level of deficiency), but I will tell you that the worse we are, the more dramatic (and immediate) the response. For those with extreme mental fatigue, you can usually tell a difference in alertness within the hour. Gastroparesis/constipation is usually relieved within 60-90 minutes (that’s how you know the vagus nerve is stimulated).
I do recommend taking it on an empty stomach first thing in the morning. If you can wait an hour before eating after you take it, it will go into your system faster and it is easier to see the response.
Fingers crossed for you!
Thank you. I’m certainly in the “worse” camp so fingers crossed.
Karin, you asked about my story… I put out videos about my journey for years on Prettyill.com. I summarized much of it in my book (“The Driscoll Theory”). Although I started with abrupt autonomic dysfunction, I went into chronic fatigue, and eventually, pain. Ugh. The first thing we figured out was a propensity for high intracranial pressure… then we went from there. I hope my journey can somehow shorten yours!
Thank you Dr. Diana. I’ll take a good look through your website and watch the videos so as to get your full story. I posted a comment earlier today on my first two days trial of ‘Parasym Plus’ and wondered if you’d seen it ?
You’re welcome, Karin!
I haven’t seen your comment yet, but I’ll look for it.
I heard from a patient recently who said, “Please tell everyone to take Parasym Plus first thing in the morning and wait about an hour to eat.” Her response was good if she waited 15 minutes to eat, but dramatic if she waited an hour.
That’s a good point, since we need the ingredients to come together quickly to stimulate the nerve.
I wish you the very best in your journey, Karin!
Is this also the case for fibromyalgia? I have pain that keeps me awake every night. I am up at least 9 to 10 times a night when I do sleep. This is along with all the other symptoms mentioned, the foggy brain, tiredness, weeing a million times during the night. I really do think I am going insane?
In my humble opinion Nerida I’d hazard a guess at ‘yes’ this includes Fibromyalgia. I was diagnosed with both CFS/ME and FM when first ill (and now in the last year tested positive for Lyme and other co infections) since then I’ve had specialists tell me they are one and the same and overlapping symptoms are many. You are not alone in feeling as though you are going “insane”, but research and progress into this illness IS making headway so hang on in there. In the meantime, why not try boosting acetylcholine as suggested in this discussion, from what I can gleam the side effects are few and mostly from people who have taken to high a dose. I agree, low and slow to start with. But surely it’s got to me worth a shot and it’s why I’ve ordered it.
Thanks Karen, I will.
I agree. I think “fibromyalgia” has become almost a dumping ground for these invisible illnesses. I would have (incorrectly) been diagnosed with fibro, RSD and likely chronic Lyme had I not started out as a POTS patient (and continued to fight for answers).
During this journey, I certainly felt like I was going insane. Please understand I was dramatically ill, only staying awake about 3 hours a day for a while, I couldn’t think, and my personality was… let’s just say ‘altered’ — lol, but there were medical answers for everything. I do think there is hope for us all.
Dr. Diana, can we read of illness history and journey to recovery somewhere? What you experienced exactly and how you found your way to wellness ?
Nerida, I often wonder how many fibromyalgia patients are suffering with inflammatory pain (as I did). I would have been labelled as such if I hadn’t put up a fuss. I explained that my pain was inflammatory and asked for an MRI, which proved it.
New research is revealing inflammation as a source of ongoing pain for CRPS, so it will be interesting to see.
If we have vagus nerve problems, we will have problems with inflammation (the vagus nerve helps prevent the release of inflammatory cytokines by some cells). This was one of the necessary steps I needed to control my inflammation and the pain that resulted. Someday soon, I hope we separate out inflammatory patients so they can be treated appropriately.
Dr Diana,
I have watched your videos, read your white papers & everything seems to ring true & make sense. My sister & I both ordered Parasym Plus today. I was alarmed at researching the medications I am on for POTS, sleep & neuropathic pain are ALL anticholinergic!!! Does one need to have these out of their system to safely take or benefit from Parasym Plus?
Thank you so much for your diligence in endeavoring to find us some help!
I’m so glad you are finding the information helpful!
You don’t need to stop medication with anticholinergic properties. These properties (for example, with antihistamines) are not the mechanism of action of the drug — they are side effects. I hope to have a post out soon about how important it is to support acetylcholine production when taking most anticholinergics. We’ll concentrate on antihistamines first and the new research about how the anticholinergic properties may be contributing to dementia.
Boosting acetylcholine is our friend!
🙂
Has anyone who’s following this thread had success with the Parasym Plus. Mine arrived last week and I was eager to try it. First day I took one tablet (on an empty stomach). Didn’t feel too good a short while after it but thought perhaps that’s just my normal up and down. The following day I took 2 tablets, again on an empty stomach. This time within 20 mins I was feeling dreadful 🙁 Now I’m scared to try again. Anyone got results or had similar?
Dr Diana, I downloaded your PDF re POTS. What should one do if they have symptoms of intracranial pressure but are already on florinef & IV saline?
IV saline has been a major contributor to my qol improvements & has kept me from spiraling into an abyss in the face of stressors. However I do often experience headaches after receiving them. I have many of the symptoms of intracranial pressure. How does one go from convincing their Dr they need volume to asking for a trial of Diamox?
If one has the intracranial pressure would that be one reason they might not get the desired result of the Parasym within the 90 mins? My sister who is sick but much higher functioning than I had the desired reaction within 15 mins. I tried 1 first thing in the morning on an empty stomach, nothing after 90 mins. I then tried 2 the next morning, nothing. Went up to 3 the following morning, nothing. Although I am sleeping sounder at night.
I am also in the process of tapering off Amytriptilene 25mgs which I was taking for sleep & neuropathic pain. As I mentioned I am on several meds w anticholinergic properties. Would this interfere w the desired poo effect of the Parasym?
I am very far from your clinic but everything I have read & watched about your hypothesis rings true to me & fits w the issues I have dealt w for years. My mother was told your babies WILL NOT be constipated if breastfed. She breastfed all of us, we were all constipated. That’s just one of the lifelong indications of under activity of the vagus nerve.
Thank you for your patient & thoughtful responses!
Hi Hezza,
First, I’m so sorry you are going through a similar journey as my kids and I did. I wouldn’t wish this on anyone, certainly, but please know there are ways to improve, even recover.
Having said that, I think you understand that we are not all alike (I wish!), and it can be tough to peel everything back. That’s why we see patients for a full week at POTS Care (and work with them for weeks after).
Your question concerning saline/Florinef with high ICP is a good one. They DO work against each other. Instead, it takes figuring out why blood is pooling so you can correct that without relying on saline/Florinef — and reduce intracranial pressure, usually with Diamox.
When we first release The Driscoll Theory, many people asked how to get help with Diamox. For me, I told my doctors that I had symptoms of high pressure, did not want a lumbar puncture, and Diamox was a fairly easy trial. This blogger had some pointers: https://slingsandarrowsofoutrageousfortune.wordpress.com/2012/12/20/diamox-pointers/
I hope it helps!
Hi Diana, I have tried to order the parasym plus but Amazon says they do not deliver to me. I’m assuming they mean Australia. Is this right and if so is there anyway around it as I really would like to try it. Thanks
Hi Nerida,
They DO deliver to Australia. If you email orders@TJNutrition.com, they’ll take care of you.
🙂
I was prescribed Mestinon by my cardio who is good friends with Dr. Grubb but the cost was prohibitive. Now I’m wondering if I can afford not to try it. This drug has been around for decades the same as my illness. I’m going to check it’s cost maybe due to the publicity of the drug company, it has come down. Can anyone tell me what you are paying?
That company is in deep doo-doo. It’s not just the Congressional investigations they are having trouble financially.
It looks like its pretty cheap now. Walmart has 90 tabs of 60 mgs. for about $30. That would last you a month if you were taking the dose she is – 180 mgs/day.
http://www.goodrx.com/mestinon
Nice article and interesting discussion. I am newly initiated and stayed away from PB due to its suspected link with Gulf War Syndrome. Studies have looked at it alone or in combination with stress and/or other chemicals. I did not see any mention in the article or comments and was wondering if people knew and if so how it featured in their decision?
It’s so difficult to distinguish the nervous system and the immune system. Where does the dysfunction begin?
If methylation is suboptimal, and if methylation leads to lower levels of phosphatidlycholine and thus lower levels of acetylcholine as the late Dr. Rich van Konynenburg suggested), then the parasympathetic nervous activity will be reduced – perhaps leading to inflammatory or autoimmune reactions (as vagus nerve stimulation seems to clamp down on inflammation in rheumatoid arthritis)
http://forums.prohealth.com/forums/index.php?threads/rich-van-k-choline-sensitivity-methylation.209439/
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3574800/
Then does resultant increased inflammation (or immune dysfunction), in turn, interfere with acetylcholine receptors creating a viscous cycle of neurological dysfunction and immune dysfunction?
Maybe this is yet another, or perhaps the most important, potential viscous cycle in these conditions.
Thanks for this article, Cort. Sounds promising. I will ask my doctor if I can try this. I have ME, POTS and reactivated EBV.
I’ve been feeling much better the last few days since I’ve had a fairly severe case of poison ivy. I found an old article by Dr. Bell about a neighbor of his who had a similar experience. Apparently, the immune system must have a one-track mind and can be temporarily distracted.
I’ve also noticed a lessening of symptoms of cfs/me just before I get a cold or virus, so when I feel better I take it as an ominous sign.
I think I’ll wait to see if Mestinon, or any other remedy, makes it to the recommeneded list before asking for it.
I have been disabled with Chronic Fatigue Syndrome for nearly two decades now, and in the past couple years I was prescribed Mestinon by my electrophysiologist to treat orthostatic hypotension. My experience has been positive, albeit not quite so good as that of the fitness buff in the article (possibly because I was more sick).
As you all know, there are good times and relapses in CFS/ME, and in my bad times I was almost completely bedridden. I always tried to get up to go to the bathroom, even creeping on my hands and knees when I was unable to stand, partly because I thought that if I stayed in bed too long, I would deteriorate because of physical weakness, and partly because I wanted to maintain at least that level of independence and dignity, but I wasn’t always well enough to get to the bathroom on my hands and knees. Even in my good times, if I went to a family get-together on Christmas and holidays, I would be ‘crashed’ for weeks. When I was lying in bed, I could watch a movie only by breaking it up into several sessions, because of the fatiguing effect, and because I wasn’t able to keep track of what was happening in the film in one session.
I am still disabled, but the Mestinon has made a big difference. I still have to be very careful about pacing myself, but I am able to prepare my own food so long as I am not too strict about eating at exactly the same time every day. When there is a potluck or community meeting in my building lasting an hour to an hour and a half (I now live in an apartment building for the disabled and elderly) I am able to attend, I can sit in a chair the whole time, and I can stay lucid during the meeting. Sometimes I feel ‘crashed’ after a meeting like this, or after a trip to the store, but I can now GO to a store sometimes (riding in a vehicle, when the trip isn’t too long) and the ‘crash’ from a fatiguing event of this magnitude lasts a day or two, rather than a week or two. I haven’t had any of my accidental ‘crashes’ due to everyday activities trigger a full-fledged relapse the same way as happened to me several times before the medication. Mestinon has been the most effective and most consistent prescription medication I have received since I came down with CFS/ME, and I have been on quite a few.
I am sure that there are different subsets in CFS/ME, but I would not by any means rule out trying Mestinon if you suspect mitochondrial dysfunction. By far the most effective supplement for me is D-Ribose, which seems to work by improving mitochondrial function, but I also benefit from Mestinon.
I notice that some of the comments recommend non-prescription supplements aiming at achieving the same effects as Mestinon, and I will say that while I cannot speak precisely about the likes of Parasym plus, because it contains huperzia serrata, and also because the precise proportions of nutrients might make a difference, my experience with Choline and Aceytl-L-Carnitine is nothing like my experience with Mestinon. Interestingly, I did find both supplements to be helpful, but nothing remotely like the Mestinon.
If you are taking Choline and Aceytl-L-Carnitine I will also note that adding Alpha Lipoic Acid to the mix seems to improve their effectiveness HOWEVER, be sure to familiarize yourself with the symptoms of Candida overgrowth first. This combination of supplements provoked a fairly severe Candida infection in me, and I only, or rather, my doctor only figured out the problem by the time I had pus coming out of my navel. The Alpha Lipoic Acid seems to be the worst offender of these supplements in provoking Candida, so be sure to stop taking this supplement at least if you start to develop symptoms of an infection. Candida is very, very difficult to get rid of, and it keeps coming back. Not only can Candida infection cause serious problems, but the medications that can get rid of it are in many cases quite toxic. I know that the temptation to keep taking a supplement that helps you with CFS/ME is enormous, but it isn’t worth developing systemic candida.
Finally, I must note that Mestinon can have side effects, the most common of which, is diarrhea. I have this side effect, and it is severe enough that I wouldn’t be able to take it without help. The ‘antidote’ to the diarrhea is Loperamide (the same thing as Imodium, but the generic is just as effective). The reason that Mestinon often provokes diarrhea is that it increases smooth muscle contractions, and food moves through your gut because your gut is surrounded by a layer of smooth muscle. The Loperamide/Imodium lessens smooth muscle contractions, but the Loperamide does not have very much effect outside of the gut, while the Mestinon is able to spread throughout the body and have its systemic effect.
If you are thinking at this point that it sounds very artificial to be taking Mestinon and also Loperamide for long periods of time, you are right, but people with Myasthenia Gravis have been taking the combination for decades successfully. Both of these drugs are fairly safe; safe to the point that they can be given to healthy people, and for me and many others, CFS/ME is a very serious condition.
I am still not “well” but the Mestinon has been the difference for me of needing nursing-home grade care, and being disabled, but capable of living independently. I wasn’t sure how to interpret this in terms of CFS/ME before, since I was prescribed the medicine for Orthostatic Hypotension (I do NOT have POTS incidentally), but it looks as if other people are benefiting as well.
wow what a story! You are making me think that I really do need to find a Dr who will prescribe this for me to try. Thanks for posting this.
I started taking Mestinon a few weeks ago. From beeing unable to go for walks I noe can go short walks about 20 min times more.
How long time did it take before you had (the best) effect and what dosage?
Good luck in the future:)
It takes 6-8 weeks to see full effects for most patients and you should try to get on 180 mg time released pill once a day after building up to it. You start at 30 mg per day for a week, then 30 mgX2 times per day for a week, then 30 mg X 3 times per day for a week, and then 60 mg X3 times a day for a week; if you can tolerate that for a week, get the 180 mg time released pill that you take just once a day.
Diet/regular tonic water and magnesium will help if you get any cramping while your body is getting used to the drug. According to the doctor, that is a good sign that the drug is getting to where it needs to be if you experience cramping.
Hi Rita, your reply here is now 8 years old. I began trialing Mestinon a month or so ago. Thank you for the details of how to work up to 180 mgs. Are you still taking it? How has it been for you long term?
Thats great news Sigrid !!
So interesting. I have OI (passed out after 3.5 minutes in tilt table test) and also regularly show ACTIVE titers for EBV, along with HHV-6, along with a whole mess o’ other issues!
I’ve been on Florinef (0.1mg) for quite some time, though I’m trying to ween off. It does keep me upright some of the time, but not aways. And it’s helping zero with my intense cognitive issues/brain fog that keep me from being able to work, and are just getting worse and worse. (Think dementia, for real.)
I’ve just started some Butcher’s Broom, and I think that might be helping the OI in the afternoon when it gets really hot. (I tried it in the past, and it make my underarms and breasts ache. Not this time.)
I’m super interested in talking to my doc about the Mestinon. Not sure if I can try it while on Florinef, or that might be great! Dunno.
Does anyone know any doctors who are willing to prescribe Mestinon or other parasympathetic stimulating drugs for CFS/m.e and dysautonomnia (both of which I have) in the UK? Please let me know
Tareq, can you request your GP test you for Myasthenia Gravis ? Symptoms of MG can overlap with CFS/ME and this is how when I first became ill (prior to being labelled with CFS/ME they tested for MG with the routine Acetycholine receptor antibodies blood test. I am in the UK and as the test was positive the doctors explored the possibility I had Myasthenia Gravis, turned out they eventually decided I did not have MG but none of the specialists I saw could explain my 3 positive tests of Acetycholine receptor antibodies. I do know that if you tested positive for this test you would be able to get a prescription of Mestinon. There is a good chance you will also get a positive result on this test if what I’m reading on this subject is correct and a lot of those with CFS have Acetycholine problems https://chronicdiseasedigest.org/2016/02/23/37/ Because I didn’t exhibit the outward features of Myasthenia Gravis I was not given the drug, but I know I could have requested it. I’d encourage you to show your GP these findings and request the test.
I have now heard from someone that the medication Mestinon has been implicated in people *getting* Gulf War Illness. Yikes. And I read that the supplement alternative, Huperzine, can cause severe negative reactions, such as intense hours long vomiting (I saw this on Amazon.com’s reviews of the supplment). so, folks, like with everything you try, BE CAREFUL.
This medication has been used for years to treat Myasthenia Gravis without causing Gulf War Illness. Other factors such as Cipro antibiotics (Fluoroquinolone) may be implicated in that illness.
http://www.publichealth.va.gov/exposures/gulfwar/sources/pyridostigmine-bromide.asp
http://www.collective-evolution.com/2014/01/06/gulf-war-illness-tied-to-cipro-antibiotics/
Absolutely be careful. But the reviews on Amazon of Huperzine-A that were negative were mostly by people who took too much, or who ramped up way too quickly. A very large percentage of people noticed improvement, at the very least in their cognitive ability. And I just took my 1st dose today – 25mcg, which was a quarter of a tablet – and I must say that so far, no negative reaction yet, and already I feel noticeably better than I did before, with slightly clearer vision, less pain, and slightly more energy. I will give it time to build up, and will resist the urge to increase dosage right away. But given that I was feeling pretty bad this morning due to many days in a row of poor sleep, I must say that right now I am feeling really optimistic.
For those considering Huperzine A supplements, the brand I tried is Source Naturals, which has strong reviews that seem to indicate it at the very least is not a placebo, there is some quality stuff in there. I’ve been through this game before, so I’m not holding my breath, but I was not expecting much of anything, and so far there is no denying I feel better than I did in multiple areas of function. It wasn’t expensive, so I think is worth a try for many. Do your research to be sure it is ok for you. Note that many describe diarrhea as a side effect if the dosage gets too high. I will probably take only this 25mcg for a few days (in the morning – can apparently keep you up if you take at night), and consider going up later if I do not notice any bad effects. But considering it builds up in your system over time because its half life is longer than 24 hrs, be careful and err on the side of too little. Slow and steady wins the race, right? Good luck to everybody, and I will definitely report back to Health Rising if this is very helpful to me in the long run!
I read the same and had posted above. Some suggested it was the additional stress and other chemicals that lead to Gulf War Illness. I have mild orthostatic intolerance so not sure if this is for me, but I am planning to try out Huperzine a.
Hi there.
I’m posting again (sorry!), as I’m just realizing after all these years that I may have POTS and not “just” random OI! Any help with this would be greatly appreciated. (And I may have hit “submit” twice, so if this comes up twice, I’m super sorry!!
POTS never occurred to me, as I tend to be quite bradychardic, though I understand that can be.
I had a tilt table test a while ago, and the doc said in all the years he’d done them, he’d never seen one so dramatic.
Here is a summary of what the doc said in his report:
“. . . Her pulse was stable between 56 and 65 BPM. . . . Immediately upon being placed in the 70-degree upright tilt position, her BP was stable at 109/50, but her heart rate increase to 119 BPM. Over the next three minutes, her heart rate ranged from 112 to 120 while her BP gradually feel fell. . . . . Patient felt shaky, nauseated, which was followed by a cold sweat, and the patient became profoundly near syncopal.”
Summary: “Profound orthostatic hypotension with an immediate doubling of her heart rate upon going from supine to upright tilt, and concomitant fall in her BP from 109/50 to 40/30 with just 4 minutes of upright tilt. . . . The fall in her heart rate occurred after the fall in BP and was more likely an effect of profound cerebral hypo perfusion rather than frank neurocardioigenic syncope.”
He told me he my heart wasn’t an issue, and that it was either an adrenal or ANS issue. I now know it to be an ANS issue, but, as I said, had never thought I had POTS. I’ve been on Florinef for years. (I’m now wondering about MCAS, as I have many symptoms that fit that, as well.)
For this post, I just need to know if this sounds like POTS.
Yes! By definition, that is POTS.
I have a free brochure of the First 4 things I would do if my kids or I were just diagnosed with POTS (on the website). Perhaps that could help you?
I started with POTS, then went on to CFS/ME. It can be a beast of a condition, but recovery IS possible.
Hang in, my friend.
Thank you much, Diana. I know it seems silly not to have thought of it as POTS as it applies to me, but there it is!
What is the URL for your website? I’d like to see the four suggestions.
While I don’t have EDS (the tips of my fingers do curl up, but the second knuckle is fine), I downloaded your book, thinking there might be some helpful info in there as I do have some symptoms that indicate possible MCAS.
(And I just received ParaSym Plus in the mail. Got here fast! I tried two this afternoon, for the heck of it, and felt nothing. Though, I totally understand it needs to be first thing in the morning on an empty stomach. I will do that tomorrow morning.)
Thanks again.
Found the brochure!
Awesome!Hope it helps
Since you are kind of a newbie with POTS, you may like the “What is POTS” section here: http://www.potscare.com/about-us/
🙂
Thanks much.
I can’t believe all these years I never realized I had POTS because I thought I was only bradychardic. I was just feeling a bit blood pressure-y, as I call it when I’m getting orthostatically challenged, and took my pulse and it was 114. (It’s typically in the 50s and 60s.) I tried again a few hours later when I was feel that way, and my pulse was nearly the same. Who knew?? My pulse must be so weak that I can’t feel it in my chest at all. Ever.
I’m very seriously considering coming to your clinic in Colleyville, though I have all kinds of things that make me a bit of an outlier, in terms of symptoms. (I also don’t have EDS.) Maybe I’ll call and see if it’s worth making an appt.
You know, syd, I think our increasing heart rate kind of sneaks up many of us. And who would think to check it in different positions, right? That’s likely why it can take an average of 9 years for most people to be properly diagnosed. Yeesh.
We’re happy to chat with you and ask you a few questions to see if you may qualify. Whatever happens, I wish you the very best in your journey.
My doctor diagnosed likely partial Orthostatic Intolerance with me and prescribed Dixarit (clonidine) for vagus nervus stimulation. The result:
* My head improved significantly (beiing sharper, less brain fog).
* My legs went worse rapidly (a matter of weeks). I could less than a third compared to the litlle I used beforen (could walk less than 100 metres a day including from bed to sofa after the meds).
* Both endured long after I quit the medication.
Please know that Clonidine does not stimulate the vagus nerve. It is an alpha-agonist, meaning it is prescribed to decrease some affects of the sympathetic nervous system.
In my case (and it looks like the majority of us), our autonomic imbalance is not so much an over-active sympathetic nervous system, as it is an under-active parasympathetic nervous system.
Huge difference in treatment!
🙂
Great discussion. Thank you, Cort.
I have had success with Mestinon for MG appearing symptoms but remain MG antibody negative. I come by way of ME/CFS after multiple infections at different points in life (chicken pox, Lyme, Influenza). Each subsequent infection making matters worse. I do have EDS, POTS, MCAD and a mitochondrial myopathy (Carnitine) also diagnosed.
After recent rapid cognitive decline, I am beginning a trial of Exelon tomorrow. It is Mestinon with ability to cross blood brain barrier. It is an Alzheimer’s medication, however my doctor does not believe the current cognitive deficits are patterned to dementia/Alzheimer’s. Simply the success with Mestinon is driving the idea to try this for the cognition.
I have a low threshold for meds used to treat MCAD. The anticholinergic side effects add up to symptoms, that require stopping, with a relatively normal MCAD dosing schedule. So I think we are on the right track questioning acetylcholine involvement.
Also, I have a related question. If the Mestinon has been treating an underperforming parasympathetic nervous system – could this figure into an explanation for unexpected responses to stress management techniques (ie biofeedback, meditation)? I have had experience where if I get to relaxed, on some days, I can have a hyper-adrenergic response (physician observed). I thought Dr Rowe had mentioned an overshoot of the sympathetic if the parasympathetic got too low functioning. My memory is that he had observed this in ME/CFS kids he has treated. Is my memory serving me correctly or does this thought make sense?
Congrats on your success with Mestinon and good luck with Exelon. Please tell us how it goes. I don’t remember about Rowe saying that (which doesn’t mean anything) but given the yin/yang of the PNS and SNS maybe something like that can happen. For me when I find something that increases my energy I feel better for awhile and then get fluey and fatigued…
Hello,
How long time did it take for you who have effect of Mestinon? And what dosage? I am interested in trying.
I started seeing subtle changes in my breathing the first week but didn’t trust that it would stick, by the time a month had passed I realized my head seemed less foggy and I was staying up on my feet about the house more. That was about two years ago, I recently increased to 60mg three times a day and am thrilled with it. It’s short acting and I can tell when I need to take more. Go up slowly on the dosage, for me rapid changes made more muscle spasms, eyelid twitching.
Thank you!
Did it improve other symptoms also? Fex pain, heartbeat, temperature?
Mestinon has been a miracle drug for me. I take it for large fiber neuropathy. I also have lupus and inappropriate sinus tachycardia. I have gradually increased to 7 pills a day.because it works so well,doctor has cautiously let me increase
Hi Michelle, I am on day 2 and this seems like a miracle drug. Sonu build resistance to the effect if the drug? What dosage are you on and is it still working
Warm regards
Justin
ELON MUSK THE BORING COMPANY https://teespring.com/elon-musk-the-boring-company-t#pid=2&cid=573&sid=front
I have been prescribed Pyridostigmine, 60mg tablet cut in half 3 x a day. I immediately got my energy back and my pain decreased. As soon as I started I was able to be social all weekends. And I even went canoeing. before that I was laid up all weekend recovering from the week. My doctor is sending my blood work to a place in Germany to test for a certain antibody because he said it is the only place in the world to provide this test. I have EDS, Pots that is under control, and VWD, and other random things. My legs burn like hell to the point I have to use a wheelchair. My hands have been shaking for the past couple of years. This has helped stop the hands from shaking. If I forget a pill my hands will start to shake. Anyone know what the shaky hands are about? Or the burning legs?
Gloria, Sounds like you have small fiber polyneuropathy and that can be treated by IVIG, which is what I have just started treatment with. Not easy or cheap but it can heal the nerves, which takes about one year of infusions, three days in a row, every month. I was lucky that my insurance company is paying for it on the first ask!
I think you probably should be on a higher dosage of Mestinon. I am on 180mg time released, so I only take one pill a day. 180mg is the standard dosage and so easy to take on pill a day, rather than three.
Hi Mona,
This seems to be a miracle for me with dramatic increase in energy and loss of dizziness in 2 days. Does the drug keep working or does the body build resistance
Warm regards
Justin
Hi Mona.
Glad you are feeling better!
Would love to speak with you re/mestinon which I just finished. Could you contact me? thanks
Mona, how did you end up a candidate for the IVIG? Is the mestinon continuing to help you?
I watched the video you did with Dr. Systrom and am now a patient of his. I did my iCPET and skin punch biopsy in February and have confirmed preload failure and small fiber axonopathy. I’m nervous that the mestinon won’t help me – I’m not feeling any better after a month on it.
Kmac, I think the Mestinon is worth a try, and they will start you with small dose (15mg 3x/day) and increase by weekly increments if tolerated. I had my nerve biopsy at the Brigham with Dr. Novak 1/2021 and completed CPET testing with Dr. Systrom last week. Sadie Marciano, PA for Dr Systrom is incredible! She’s excellent at being both compassionate and blunt about symptoms/prognosis (I hate when DRs sugar-coat things so you don’t get the real story). Sadie said that it may take 6-8 weeks on an optimal dose of Mestinon before real benefit is seen. After 1 wk on Mestinon I’m not feeling much different, perhaps slightly better sleep, though I’m still recovering from the invasive CPET. I experienced mild GI symptoms on days 1-2 of Mestinon that have resolved. I had increase in right eye twitching which also resolved. Doing a trial of Mestinon may be helpful, if even to rule out that this medication is beneficial. It’s a process but could be an important next step toward better treatment. Good luck!
Gloria, you’re probably extremely deficient in B12 and/or possible thiamine. Drugs aren’t the answer, they only mask the symptoms TEMPORARILY. IVIG may work, but addressing the intestinal permeability is key to restoring immune function in patients with ME/CFS. There are several studies to back this up.
Likely small fibre neuropathy, which is linked to POTS and EDS. My legs also burn, but for me the doctors are stumped. They think it might be long term Suboxone use.
28 years w moderate CFS- and was getting worse over time. 4 days on Mestinon and so far so good.. afraid to say too much but this has been nothing short of amazing for my fatigue and PEM…. fingers crossed !
Glad to hear it Beth!
Good luck to you…. Please let us know how it goes 🙂
Hello fellow “weak, dizzy, brain fog people”. I am a Myasthenia Gravis patient that took years to diagnose because mine was very subtle and generalized, pain was a puzzling problem. They claim it does not cause pain. But one PA told me it is secondary to the disease, which makes sense since I was trying to do “normal” things people do with only 20-30% of the function of my muscles vs what others do with 100% of the use of their muscles. Who wouldn’t hurt! So the fall back is do less and less and even the muscles you do have get weaker if untreated . My MG only caused mild very occasional eyelid droop (like feeling sleepy), mild occasional slurred speech, slow chewing and swallowing but very weak walking and a wobbly gait and a mild idiopathic head tremor.
Mestinon 60 mg did help . 1/2 tab ( 30mg) three to 4 times a day. But the odd thing with me that stumped them is myasthenia gets worse when you exercise and “recovers” after rest. I felt the WORST trying to sleep and pain was my constant companion. I was exhausted even trying to sit up and brain fog was normal.
One thing I have not heard mentioned yet is SLEEP APNEA. The weak muscles occur in the throat and tongue – which are weak in MG. I was chocking to death and running in my sleep, clenching and snoring and felt like jumping up sometimes to breath. This additional discovery after getting a CPAP made my life much better, it completely stopped my restless legs syndrome, only briefly stop breathing 1 or 2 times per hour verses 30! morning headaches are gone and brain fog is gone.
New CPAP masks like the nasal pillows make CPAP a breeze. Full sleep studies can detect those issues, restless legs and deep rem deprivation plus almost suffocating in your sleep. ( I thought I slept like a rock just exhausted the next day!)
But there is also new take home tests for sleep apnea – where you sleep in your OWN BED and simply wear an O2 monitor and cardiac wrist watch and tabs to detect snoring and arrested breathing , these are often available from dentists ( like TX) and some ENT’s in some states and all neurologists are permitted to prescribe the tests to be read by a Sleep specialist for referral for CPAP or if mild to moderate a dental guard that puts your lower jaw in a sort of CPR position to open your airway.
had a prior DX as Fibro/Chronic Fatigue/ and just plain fat and lazy. WRONG. I am mild to moderate MG, spent a few years on Imuran ( immune suppressant pills) which put me in remission for several years but now – 5 years after stopping Imuran- all this has returned but now know the path to be able to finally turn over in bed on my own, sleep without chocking and running in my sleep, I can climb at least one flight of stairs without a rest vs very slow one step at a time and and not feel like I ran a marathon daily.
My point is get screened for sleep apnea. It is a dangerous condition- often not diagnosed- It may be your missing piece of your puzzle, esp for morning pain and brain fog.
Thanks for the suggestion Theresa. Most sleep apnea is not diagnosed…
Are you still better
How is myasthenia gravis being ruled out in CFS/ME patients who benefit significantly from Mestinon?
A couple of comments on this drug.
First, seems it is very, maybe extremely, difficult for ME/CFS patients to deal with initially, and has to be introduced very slowly in tiny doses. My CFS doc said only by liquid (syrup) very very slowly; and that then, it should probably be ok.
Second, there might be drugstore price idiosyncrasies. My drugstore (Walgreen’s) intially told me the price for the syrup would be over $1,000 for a month’s amount; 5 days later, the price was $379. Who knows; maybe tomorrow it will be $2,000. This drug pricing is crazy and something has to be done about it.
By the way, the tablets are much cheaper. But the side effects issue seems to be almost guaranteed.
Maybe it’s possible to move from the expensive syrup to the much more nearly reasonable tablet, once one has become accustomed to the drug.
But, I for one don’t feel it’s acceptable for the syrup to be so unreasonably priced. There seems to be some chicanery going on here, to be nice about it.
Sorry – I didn’t make it clear that the drug I was referring to is Mestinon, that is pyrodistigmine (sp?)
cdax, Definitely try goodrx for much less expensive prices for the syrup. Just print out the coupon and take it to your pharmacist. In my area, generic mestinon costs about $30 for 30 ml.
I use Good Rx. They are a tremendous help. I wouldn’t try to get a prescription without checking them first.
Are you having good luck with the Mestinon.
Interesting! Have you tried a drug discount card? I found great savings with Valtrex with GoodRx https://www.goodrx.com/discount-card?utm_source=google&utm_medium=cpc&utm_term=rx%20discount%20card&utm_campaign=Prescriptions&utm_content=Ad-Group_Discount%20Cards&gclid=CjwKCAjw27jnBRBuEiwAdjQXDGWhRyHFDgCkCepnacYRPGq2KuWlNpnl1gkUaDipgzeF92-KbwQHxRoCMQ8QAvD_BwE
Maybe something has changed in the last two years but my mestinon script cost me $8 USD.
Did this woman participate in Dr. Systrom’s “exercise test?”
Yes, she did.
How can you work out how much Mestinon to take?
I use Mestinon along with propanol and fludrocortidone and it has changed my life. I was effectively disabled and am now fully functioning again!
I had inflammation of the spine. I purchased a PEMF bed. What a difference. It doesnt heal but supports a non inflammatory environment. Eventually, the autonomic nervous system can hear itself through constant switching off of inflammation flight/fright response. Once it hears itself, it can talk to the brain. Once that connection improves, brain chemistry can regulate correctly. 5 years later, I take only vitamin support and occasional use of the bed. By the way, if you have bone weakness or bone marrow issues, PEMF in research has been seen to speed up bone healing in fractures. I had HSV, EBV, battled on with acyclovir 800 5 times per day until I stopped it due to liver pain issues, I placed all my focus on PEMF and vitamin support and yin yoga. That was the turn around. I’m well enough to work and earn a living, to enjoy gentle walks. I use PEMF to maintain a healthy body. For more info ochreoak@hotmail.com. Happy to connect and help others achieve wellness via sharing my path.
Any follow up on this story? Additional research? I’m definitely asking my GP and she really works with me on things like this I stumble across. 9 years chronic fatigue, fibro and a list of symptoms to go with, since chemo and viracella zoster virus flare up in my OPTIC nerve sheath (only symptom head pain and eye swelling) with 2 occasions of trigeminal neuralgia in the following 6 months! I’ve tried everything, from Neuro docs (including neuro-muscular) and infectious disease (dx mito dysfunction). Since I was on antivirals after VZV my PCP agreed to add Celebrex Based on blogs here I showed her, but got no relief, nor from mito mix of supplements. I keep coming back to cranial nerves + virus flare + damaged mito from chemo poisons. I’m still searching (for my former life)
Sorry to hear you’re still having so much trouble. The Open Medicine Foundation is funding a Mestinon trial with Dr. Systrom and the Solve ME/CFS Initiative is funding a research study with him as well. Hopefully we will get some more news soon. Good luck!
im commenting on the sleep apnea. I am sure i have sleep apnea but i honestly think its an end result of being so sick for so long. My doc says i got this (cfs) from infection. i ordered the book ” The perrin technique” as i have/had lumps all over my upper trunk (probably infection sent to the lymph). while my lumps have gotten considerably smaller, i was told by a ear, nose and throat specialist that i may have sleep apnea. Here in Canada things are quite a bit different with the way things are carried out in the health system. I am awaiting a ct scan of my head as my sinuses are completely closed off and breathing in air is almost impossible. My point is , i think sleep apnea is an end result…i had a complete blow up of my immune system…in fact ive yet to see another person as sick as me anywhere on here or other site….i had it all…i wanted to end my life as the pain was unbearable and went on for yrs. and yrs. I got sick when i was 33 and im now 60. This is a hellish nightmare with no help. Ive tried everything and can say that this book above, has helped me the most so far. I believe we are all different …while some like me have infection, there are many others with different issues. Somebody needs to sort us all out into sub groups, otherwise we will just continue to go in circles. Its a dam good thing my hunting guns were in my basement and a dam good thing i was too sick to get out of bed to go get them or i would have done it! Extreme fatigue can be your friend! im no longer like that as ive improved on my own without any help from the medical “profession”…I KNEW I WASNT CRAZY….I KNEW I WAS VERY VERY SICK AND KNEW I HAD TO HANG ON…AND HANG ON , I DID. THIS IS A MEDICAL TRAVISTY AND I WAS DISMISSED BY ALL OF THEM IN MY OWN CITY AND PROVINCE!!!
I’ve been on mestinon for three years now after 12 years of M.E and it got me from bedbound to 80 per cent normal. It’s been amazing. However, the past few weeks I have been getting new symptoms of shakiness, juddering, weird symptoms. Could the mestinon have stopped working for me I wonder? Have I built a resistance to it? Could I have developed a new problem. It’s so worrying…
I’m sorry to hear that Jane….Are the symptoms similar to what you experienced before or different? I hope someone has an idea and I hope whoever prescribed it has an answer. Good luck!
After seeing several of Dr. Systrom’s videos (including one with Mona :)) I was able to get a virtual appointment with him. I’ve had 11 years of dyspnea and orthostatic symptoms. I’m so excited to see him!
That is great! Please let us know how it goes.
KMac, I’m so interested to hear how you’ve done with Dr. Systrom! Have your dyspnea and orthostatic symptoms improved? Your post spoke to me as I’ve had years of dyspnea and orthostatic symptoms as well. The dyspnea is especially hard to endure for me. Hoping you’ve had positive results with and that I might glean from your experience. Thank you in advance!
Can anyone tell me how long it took to start working for them? Took my first dose (1/2 tablet, 30 mg) and felt nothing. Guess I was expecting a miracle. 🙁
Also, have any of you ever have the sensation of a thumping pulse? I swear my eyes, head, neck, and chest/heart thump so hard. I can ‘see’ my pulse in my field of vision and can ‘hear’ my pulse all day, but especially in bed at night. Hoping this might help.
Started taking Mestinon (pyridostigmine) last week and it seems to be helping my resting heart rate, but not my POTS. My resting HR is hovering around 65-70 after being around 85 for nearly a year. However, instead of my HR going from 90 to 125ish upon standing, it’s going from 60-100. Has this happened to anyone else? Does it get better after more time or higher dosage? Thanks!
Very Educational , I just Learned alot and i wish many people wish read from your blog
Hi, and thanks a lot! There is a study now ongoing about ME/CFS and Mestinon and antiviral medicine. Please look up swedish scientist Jonas Bergqvist and you will find it.
I am very sensitive to drug side effects, but figured it worth trying Mestinon, when all the Systrom research first came out (before Covid 19) came on the scene. I titred up very slowly but had to stop after a 6 week trial. I felt worse overall. I started it in late June, so the hot weather didn’t help.
But I’m happy for anyone it does help; and I wonder whether its success in helping some people points to any other pharmaceuticals that might help.
PS Thanks for the whole blog, of course, but also specifically thanks for including the 3 minute NPR clip. I heard that on NPR one morning last week, then again this morning, and am delighted to have it to send to others in this blog.
I found it interesting that the speaker specifically referred to PEM as also being experienced by CFS patients. I hope that helps our cred a bit(!)
This medication has helped me beyond measure. Its only been 2 weeks but im able to walk, converse with people, listen to music, go out with friends and family..just generally participate in life. Ive been housebound for 2 years. I hope i keep improving.
I have had ME/CFS for over 30 years. For the first eight years, I was completely disabled. I then made a partial recovery and now range between 50 and 60% of normal health. I have been taking Mestinon sporadically for several years. I discovered that it helps with the stomach issues caused by ME/CFS. I recently realized that Mestinon also helps with exercise intolerance and strength. I’m just starting a regimen of taking 30mg two or three times a day to see if I can get even more out of my bare bones workouts.
Congratulations, Ben. Thanks for sharing and good luck with the exercise 🙂
How much famvir against ebv? Thank you
Hi Cort,
The statement that “the upper limit prescribed for people with myasthenia gravis (180 mgs/day)” is incorrect and should be edited. This is on the lower end of daily Mestinon dosages for MG.
The Mestinon Consumer Medicine Information distributed by the Australian government states “In adults, the usual dose is one to three Mestinon 60 mg tablets, two to four times daily”. This means that 720mg of Mestinon is considered withing the “usual” dose. I recommend you read this informatin sheet.
For comparison, I am on 420mg/day (taken spread out over the course of the day) with no noticeable side effects. I can take 180mg (two 60mg tablets) in one go with no ill effects either, but I usually spread dosages out. My Neuro tells me that plenty of people take 540mg/day.
Some people experience side effects from Mestinon such as GI issues, so likely the 180mg/day is the maximum dose that the person in the article can handle.
Cheers,
Amy
Thanks for the update. It’s fixed!
Just wanted to share my recent experience with Mestinon for POTS and Orthostatic Intolerance. I started with the 10 mg pills and increased to 6x10mg three times a day. It has been a real game changer for me. My brain was razor sharp again and the “jelly in my knees”, SOB and nausea got a lot better. I filled a new script for the 60mg pills, all my usual symptoms were back within a few hours and I was even more nauseous than before. First I thought I caught a stomach bug but after 3 days I started wondering what I do differently. The 60mg look a lot different, are bigger and have a different coating. I googled Mestinon fillers 10mg vs the 60mg and it turns out that the 60mg have wax, lactose and sugar as fillers which could slow/prevent absorption and especially the wax can cause nausea. So I went back to the 6x10mg three times a day and feel so much better. The lesson here is the fillers can make or break the success of a medication. Try the a different strength with a different filler, try a different brand or even get it compounded to your needs.
Thanks for sharing that Carina!
Did she test for MG antibodies