



Did you know that you probably have a smaller heart than normal? Four studies suggest that if you have chronic fatigue syndrome (ME/CFS) you probably do. The word on the small hearts for years has been that they’re probably caused by inactivity or deconditioning. This study suggested that they probably are indeed caused by inactivity – but not by deconditioning at all.
Newton’s earlier small study had found reduced heart mass and significantly reduced blood pumping by the heart, and Miwa in Japan has produced three studies showing that smaller hearts are present in people with chronic fatigue syndrome (ME/CFS).
Mirroring Dr. Cheney’s unpublished findings, both Newton and Miwa have also found reduced diastolic volume (30%). The diastolic phase of the heart cycle is the filling phase. During diastole, the ventricles relax and then, in an energy intensive process, expand so that they can fill with oxygen enriched blood. Reduced diastolic volume or preload indicates that the heart is not being filled as much as normal.
Both Newton’s and Miwa’s study published last year found significantly reduced diastolic volume and mass, stroke volume index and cardiac output. (Miwa targeted and consistently found reduced left ventricular volume and density. He did not measure right ventricular functioning. He or she also appears to be the first Japanese researcher to drop the term CFS and use myalgic encephalomyelitis exclusively throughout the latest paper. )
The Study
Now Newton is back doing more tests with a much larger and better defined cohort (n=41 ME/CFS patients / 10 healthy controls).
Newton measured how much blood entered the heart during the diastolic phase (end-diastolic volume) and systolic phases (end-systolic volume) then how much it spate out (stroke volume). She also assessed the size or mass of the heart.
This time, suspecting that reduced blood volume played a role in the poor cardiac performances, she analyzed blood volume three ways: total blood volume (TV), red blood cell volume (RCV) and plasma volume (PV).
As before, Newton found reduced blood volume during both the diastolic and systolic phases of the heart cycle and not just minor reductions either; ME/CFS patients had a whopping 25% less blood entering their hearts than the healthy controls. They also had about 25% less stroke volume and index and almost 30% smaller heart mass. These appear to be very large reductions in both heart mass and heart functioning in ME/CFS patients.
Blood pressure was affected as well; ME/CFS patients had significantly lower systolic (125-109) and diastolic (76-70) blood pressures than the healthy controls. The reduced blood pressure and stroke volumes could result from the poor heart functioning or they could produce the poor heart functioning by not pushing the heart to work harder.
Dr. Cheney appears to believe that reduced heart energetics are interfering with the hearts ability to contract enough to accommodate the blood entering it. Another possibility is that reductions in blood pressure have resulted in smaller hearts.
Another possibility is that there’s something wrong with the vascular system leading to the heart which is reducing blood flows to the heart. Reduced blood flows would result in a smaller heart. That’s the option Dr. Newton appears to be most interested in.
Non Compliant Veins?
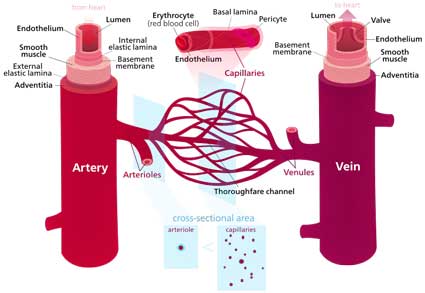
Dr. Newton questioned whether a problem with “venous compliance” was present. Since 2/3rd’s of our blood is locked up in our veins the reduced diastolic volume or preload found in ME/CFS could reflect large amounts of blood that has somehow gotten stuck in our veins.
That could lead to reduced preload (reduced diastolic volume).
Venous compliance can be affected by a number of factors including vasodilators and vasoconstrictors, the muscle tone of the smooth muscle tissue, and the renin–angiotensin system. One wonders if connective tissue problems (eg Ehlers Danlos Syndrome) could come into play as well.
Blood Volume
The blood volume results were assessed according to the norms expected. Blood volume was lower in the ME/CFS patients, but perhaps not to the extent that might have been expected. About half the ME/CFS patients had normal red blood cell volume and about half fell below the 95th percentile expected. About a third of ME/CFS patients had plasma volumes below the 95th percentile.
On the other hand, statistical analyses suggested that the reduced red blood volumes were strongly associated with reduced ventricular mass in ME/CFS. That suggests the ventricles may be smaller they’re not getting as much blood as usual.
There’s quite a bit of increased interest in blood volume right now. Medow’s study on the effects of saline solution on ME/CFS should be published soon. He is currently examining whether the World Health Organization’s oral rehydration formula could be helpful in ME/CFS. His ability to use phenylephrine to increase blood flows to the brain and completely knock out POTS during a tilt test was astonishing.
Dr. Newton proposes to increase the blood volumes of ME/CFS patients and see if the size of their heart’s increase to normal size.
Is Arnold Peckerman Smiling Somewhere?
Arnold Peckerman apparently passed away a couple of years ago but one wonders what he would be thinking of all this. Peckerman, LeManca and others working at Dr. Ben Natelson’s NIAID funded ME/CFS research center were hot on the trail of cardiovascular issues when NIAID pulled the plug on its ME/CFS research.
The group had produced some interesting results. The first heart study in 1999 showed increased heart rates and reduced blood flows during a tilt test and presaged the attention on orthostatic intolerance and POTS. The declines in heart rates and blood pressure during a stressful cognitive test they found may have been the first indication that the autonomic nervous system was prone to poop out under stress.
In 2003 their finding that people with ME/CFS were trying as hard as healthy controls knocked the legs out from under a prominent psychological interpretation. Next, Peckerman showed that people with severe ME/CFS (but not moderate ME/CFS) had a significantly lower stroke volume than healthy controls. Then he showed that the blood pressure responses of ME/CFS patients were off during exercise.
These results were positive but it was the last study, whose results were never published, which was a potential game-changer.
An MD, Peckerman, had seen post exertional malaise in some of his heart patients after the blood flows through their hearts had been stunted. Peckerman, therefore, decided to measured heart functioning before and after exercise in ME/CFS.
It was a small study – just 16 ME/CFS patients and four healthy controls but the results were astounding, and if they had been published and held up could have produced a simple and effective exercise test. Peckerman didn’t measure VO2 max – he measured blood flows – and it didn’t take him two exhausting exercise tests to get his result; he simply measured heart blood flows at rest, had his subjects exercise, and then measured blood flows at rest again.
In 2003 at the American Physiological Association conference Peckerman reported that 13/16 ME/CFS patients had significantly reduced blood flows at rest after exercise. WebMD ran a story titled “Tricky Heart May Cause Chronic Fatigue Syndrome” in which Peckerman, obviously no shrinking violet, stated that the reduction of blood flows he had seen was the very definition of heart failure.
An Emory cardiologist in the story agreed. The finding of reduced heart blood flows was, in fact, what he saw in people with serious heart disease:
“Typically we see this in people with three-vessel heart disease. A drop in [blood pumped by the heart] during exercise is not a typical response. It is actually a marker of significant coronary artery obstruction.”
Dr. Natelson described being quite excited at the results but we now know that “heart failure” is not present in ME/CFS. Heart failure is a progressive condition that ultimately ends in death for just about everyone who has it, and, the fact that ME/CFS patients were not dropping dead from heart failure puzzled both Peckerman and Miller. They both recommended that further study be done.
The study was never published, however, and we don’t know why. After one more study on ME/CFS – which did not find differences in cognition before or after exercise – Peckerman was done. He’d participated in 13 studies on ME/CFS and GWS and never published again.
The cardiovascular connection to ME/CFS has never died, however. As noted above both Newton and Miwa have found significantly reduced blood flows and filling in their studies. It now appears that those issues probably reflect significant problems with the cardiovascular system not the heart.
The outstanding question remaining from Peckerman’s unpublished study, though, is what happened during exercise to so dramatically affect the blood flows to the hearts of his ME/CFS cohort the next day? The vascular system in ME/CFS and FM is a subject that continues to fascinate.








Excellent and welcome news. A few years ago, the American Heart Association’s website said that POTS was most often due to a smaller heart, but that was later removed. I have been disappointed (to put it weakly!) that the AHA has not actively connected the prevalence concomitant ME/CFS with POTS. They should be sending everyone with a POTS diagnosis to ME/CFS specialists… if there were some. The fact that there aren’t enough should be bringing them into the ME/CFS fold. Well, maybe these studies finally will.
One thing I’m wondering about, though, Cort, is where you write “…but we now know that ‘heart failure’ is not present in ME/CFS.” Can you clarify that a bit more? Do you mean congestive heart failure only? Because I don’t think the prevalence of heart failure among us has been resolved in any studies. Dr. Jason’s statistical analysis of causes of death among people with CFS showed “heart failure” to be the leading cause. People’s hearts can fail for lack of enough blood moving through them to cause arrhythmias, etc., not just because of clogged arteries. All of us with ME/CFS at or above that median age for death from heart failure Jason found are quite interested in this topic being more fully explored.
A good friend with ME/CFS had a very atypical heart attack a few years ago, and amazingly survived but with much heart damage. A cousin who I was not close to died last year at age 63, when “his heart just stopped.” His sister said they didn’t know what all he had, he’d been a poor health, kind of sickly for a long time. That sounds suspiciously similar to what so many of us go through until we’ve had a proper ME/CFS diagnosis. I look forward to the time when informed cardiologists will be part of the front line of diagnosis and compassion. Right along with members of the American Psychological Association.
That study got a lot of publicity – which was probably its purpose – but to be honest I’ve never had much faith in its results. As I remember Jason’s study relied on people who reported the deaths of people they said had ME/CFS to a website….The analysis was statistical but it was analysing hearsay.
Another Jason study that actually followed some people with ME/CFS over time did find increased rates of mortality over time but no heart failure…
None of the few studies that have assessed mortality have found increased rates of heart failure in ME/CFS. I have a lot more confidence in them. http://www.ncbi.nlm.nih.gov/pubmed/16893495
My understanding of heart failure is that it is almost always fatal and I imagine that it follows a fairly standard course which ends with people having to be propped up in order not to drown in the their fluids. I’ve never heard of that in ME/CFS.
Heart pathology – some sort of injury to the heart in some people I assume is possible in as big and heterogeneous group as ME/CFS.
I may have used the term “heart failure” incorrectly. “Heart failure” can be synonymous with “Congestive Heart Failure”—the kind I think you’re writing about Cort, and indeed my friend with ME/CFS and the very atypical heart attack was in that situation of nearly drowning in fluids. “Sudden cardiac death” is probably the correct term for when the heart stops because of cardiovascular disorders other than congestive heart failure.
Until we have better diagnostic criteria, etc., all deaths that occur to people with ME/CFS will be attributed to something else. They will only be hearsay.
Both studies–Jason’s and the one you cite–are from 2006. Our community deserves follow up studies. I do believe that Jason is trying to gather data for an update. Here is a 2009 review of literature that can support Jason’s earlier study, citing 248 references, many deserving a good look:
Why ME/CFS May Kill You:disorders in the inflammatory and oxidative and nitrosative stress (IO&NS) pathways may explain cardiovascular disorders in ME/CFS
http://www.ncbi.nlm.nih.gov/pubmed/?term=Why+MECFS+May+Kill+You
On page 7 there’s a good diagram of how ME/CFS risks are not the “conventional risk factors” of clogged, etc., though of course ME/CFS patients may have those too. These authors begin with Jason’s study and then review a lot of medical literature to elucidate how and why this is true for our patient population:
“Recently, Jason et al (2006) reported that the mean age of patients with myalgic encephalomyelitis/chronic fatigue syndrome dying from heart failure, i.e. 58.7 years, is significantly lower than the age of those dying from heart failure in the general US popula- tion, i.e. 83.1 years. These findings implicate that ME/CFS is a risk factor to cardio-vascular disorder.
This review demonstrates that disorders in various IO&NS pathways provide explanations for the earlier mortality due to cardiovascular disorders in ME/CFS. “
And there’s the original Jason study Causes of Death Among Patients with Chronic Fatigue Syndrome
http://www.ncbi.nlm.nih.gov/pubmed/16844674
Should patients seek out treatment by a cardiologist? How does this info translate to treatment?
I think the general message is that the reason hearts are smaller is that they’re probably not get loaded with blood as much as they should. Newton’s next step is to increase blood volume and see if that increases heart size – so doing everything you can to do that might be helpful.
Yes and no. Cardiologists are not trained in ME/CFS. Even the one who performed the tilt table test in which I fainted says he doesn’t “believe in ME/CFS.” I went to another one who suggested that antidepressants might help. I don’t think we’ll get the help we need from cardiologists until the diagnostic criteria changes, the CDC tool kit changes. Meanwhile, I have a supportive Nurse Practitioner to whom I bring all of the studies and discuss, and it is through him–and because of the tilt-table fainting resulting in diagnosis of POTS and NMH–that I can receive the weekly IV-saline.
I have had fibr and cfs for more than 30 years. I’m wondering about the heart also. I just read a book, not about cfs, but about the heart and cayenne. If you get a chance read this book. It is called – Left for Dead, by Dick Quinn.
Great article. My daughter has had the typical drop of heart rate and drop of body temperature after exercise! The doctors just scratch their heads!
Does anyone have any comment on the use of a whole body vibration machine to tone muscles and increase blood flow without the attendant exertion?
I’m curious about the whole body vibration machine. Judith, who occasionally comments on this site mentioned that she bought one.
Me too….I hope we hear more.
Did I hear someone say my name? 😀 Yes, as Stephen said, I DID recently purchase a really nice whole body vibration (WBV) machine. The model I bought I have not found anywhere else on the internet except the site I bought it from. Living on Social Security, I had to get an “affordable” machine that met my needs as well. At the time I bought it, Becky Chambers’ site http://www.bcvibranthealth.com/ was offering the model I have (the gentle version) for a big reduction, so I got a great price. Be careful about buying any of the “oscillating” type machines on Amazon or elsewhere – they go see-saw, side-to-side. Becky’s book (more info. below) and web site explain why. Her machines go vertically (linear), up-and-down. HOWEVER, I almost bought one of the other kind, and if that’s what you can afford and you use it slowly and carefully, it should still provide good health benefits. And there are LOTS of health benefits! I got it especially for improving bone density (I’m 71) and helping my body function better overall. After a few weeks, I’m still at 30 to 60 seconds at the lowest setting. It takes time for those with chronic illness to slowly build up to the higher settings; you detoxify too fast, among other things.
Firstly, and this is what I did, do your research. I read articles and looked at machines all over the internet. I eventually got Becky Chambers’ “Whole Body Vibration: The Future of Good Health” on my Kindle. But her site also has an immense amount of information. She was severely ill throughout a significant part of her life, and she describes her recovery path. She is also a homeopathic doctor, but if homeopathy isn’t your thing, just overlook that part.
I look forward to my short session each day, and intend to keep up with it and build my endurance further so I can eventually tolerate the higher settings. I’ll update my progress, maybe in the forum, as time goes on.
Thank you so much for your very thorough and considered reply. I wish you well in the use of the machine! How long have you been ill and can you comment on any time frame on getting even small results from the WBV?
Good luck and please keep us informed on the Forums!
I’m trying to figure out how to reply to Linda’s comment in this discussion thread. Hopefully, this will show up somewhere in this area about WBV.
Linda, I was diagnosed with CFS in 1997. I’d been diagnosed with FMS around 1988 after a car accident. I’m 71 now. I guess I’m around 50% or more recovered. On some days, I can garden in the heat, or go shopping, run errands, lift heavy items, and have a good day. But those days are few. I have challenging symptoms, and I do cycle through bad phases. My meds coupled with carefully chosen supplements help.
Based on Becky Chambers’ book, I believe I can expect to see improvement in my symptoms over time. It IS a slow process. Because WBV helps the body better assimilate supplements, meds, treatments due to the action at the cellular level, I would imagine that within a few months’ time, I may start to feel a difference, or sooner. It’s easy to read the information on Chambers’ site to understand how the vibrations work by moving lymph more efficiently, as well as helping circulation. The tiny, quick vibratory movements cause muscle flexing in small muscle fibers and their attachments to bone that conditions muscles without the stamina required for standard exercise. If it would be for your daughter, all she would have to do would be to simply stand on the platform while it vibrates.
I really urge you to read the information on Ms. Chambers’ site to better understand the process. She also lists the diseases and disorders that are *contraindicated* for use of WBV machines. I’d suggest looking at that list first and see if she has any of those issues, and if she does, then, at least for the time being until that changes, she (or you, if that’s the case) wouldn’t be a good candidate of WBV.
All the best to you and your daughter, Linda.
I take it this is not the Bemer. I tried it and didn’t get any results, although I was using it for longer periods and stopped after 1-2 months
oh gosh Cort.
I have never commented before and not sure how to put this information together but I think it might be of interest.
Over the years there has been a collection of minor internal abnormalities observed within me. Starting with inersusseption at approximately 6 months old which indicated a weakness in the bowel.
Then later as a teenager a retroverted uterus was discovered and then later again through an ultrasound a deformity of the kidney called horseshoe kidney.
Another minor difference of interest was unusual narrowing of the ear canal, pointed out by a doctor when examining for an ear infection who noted that due to this narrowing I would be prone to these types of infection.
I couldn’t help putting this new information about the abnormal narrowing of the arteries and the smaller heart size into this collection of minor internal flaws.
Could it be possible that these internal abnormalities add up to a pre-disposition to acquiring an illness like ME/CFS later in life?
I have no idea but that’s quite a pattern Debra.
Debra , I believe your comment is very important. I also began to note various physical issues in myself, my maternal line, and the individuals in the large support group I led for 13 years here in L.A.
The early bowel problem you describe was probably a result of a malrotations/malattachments of the intestines. This phenomenon occurs early in fetal development – like 4 to 6 weeks. I have a long, redundant, tortuous colon , which is considered a malrotation issue by some specialists. Also for me: bladder/uterus in left side of abdomen. Urethra fused off to left side of bladder. Deviated septum, one side of face slightly smaller. Rotated little and index fingers, hammer toes, rotated big toe, mild scoliosis, hemangiomas in liver and thoracic vertebrae, small skull base ( posterior fossa) and more.
Yes, other people in group commented about unusual kidney shapes, poly cystic kidneys, heart issues ( reversal of the great vessels), and more. Have searched and searched for a genetic syndrome that ‘fits.’ Closest one I came up with was chromosome 22 / 11.2 deletion syndrome – Di George syndrome. Check these out.
Hi Merida,
Thanks so much for taking the time to comment on this.
While reading it I realised that I also have scoliosis which I didn’t think of before, as well I have just been diagnosed with fatty liver disease, which apparently is most commonly attributed to a fatty diet and over consumption of alcohol.! I happen to be a vegan for health issues and definitely don’t consume a lot of alcohol. When researching this I found there are other reasons for having this condition, like toxin exposure and other things.
So, thank you so much for drawing my attention to this. As well, I just realised that my mother was epileptic and I have had a few fits over my lifetime.
I was listening to a Hay House radio interview last night with Anthony Williams who wrote Medical Medium and he was talking about the connection with a sensitive nervous system and chronic illness symptoms.
I will also look into the things you suggested.
It seems that “we are not all created equal” when it comes to physical issues and some of us are born with strengths and weaknesses that will reflect the state of our health as we age and get various illnesses.
One of the things he said that I really appreciated last night was that “it’s not your fault”. After years of having CFS and feeling like I had somehow “failed” in my life this was very affirming.
Wishing you all the best,
Debra
Well this certainly is a timely article for me. Just turned up with blood pressure all over the place – as high as 180/ 122 . But also what appears to be bradycardia in the evening when pressure normalizes. I found out that my blood pressure was jumping high when I stood up. This all started with a lot of dental work several months ago. With disturbance of the carotid artery?? So finally I am in process of major heart and kidney work up. I will report what I learn. Pretty crazy.
Hi, Cort,
I am an ex-medical person and would like to correct a misconception which appears in several places in your otherwise fantastic article.
In the first paragraph or two you state that the left ventricle receives blood from the body’s veins and pumps it back up to the body. Unfortunately that’s not correct. The left ventricle receives blood from the lungs, oxygenated blood, and then pumps that out to the body.
The right ventricle receives blood from the body’s veins, D oxygenated blood, and pumps it through the lungs where it is oxygenated and sent to the left side of the heart.
Therefore, I would be curious to know how the right heart fits into this whole situation because it is the right heart directly which provides the preload to the left heart.
Clear as mud? Thanks for everything you do! I rarely miss an article.
Sue
Sorry, that should be “Deoxygenated”
This is confusing. You are completely right about how the heart cycles blood.
I don’t see any sign of the right ventricle being affected. Miwa found that the left ventricle mass was reduced but now I notice that he didn’t measure right ventricular volume at all (http://www.ncbi.nlm.nih.gov/pubmed/22120591). I assumed the left ventricle was receiving blood from the veins because it was what he reported was reduced. The same is true for his other study (http://www.ncbi.nlm.nih.gov/pubmed/24736946); he only appears to measure the left ventricle! I wonder why.
Here it appears to state that the left ventricle is the first to receive the blood. Does that mean it would be the logical place for reduced mass to occur if the heart wasn’t receiving enough blood?.
It is true that diastolic phase or preload that is most affected in ME/CFS and that is connected with venous return. (Thank god I got that right (lol))
I think the gist of the blog is correct but the anatomy was definitely off….
I have a small heart (noted on xray-suspected due to decreased blood volume) and small left ventricle (noted in echocardiogram). I also had compression of my left renal vein (Nutcracker Syndrome) which kept half my blood volume refluxing in my lower body. I have since had nephrectomy so the blood is all flowing correctly now and am living my best life with no more POTS symptoms, no more pain and pressure in my legs, no more shortness of breath, no more IBS-the symptoms associated with the refluxing blood and the relief with nephrectomy is truly amazing. There is a higher incidence of vascular compressions in those with EDS. In my opinion the first thing to discern with any small heart issue is whether the person has any vascular compressions: May Thurner Syndrome, Nutcracker Syndrome, Celiac Artery/Median Arcuate Ligament Syndrome (MALS), Jugular Vein (Eagle syndrome) etc. And then to test/assess for Eller’s Danlos Syndrome (EDS). The medical community ignores vascular compressions as “too rare” but based on my experience I would harken to say they are way more common than thought. A lot is missed due to the “rarity” factor when possibility of vascular compressions should be assessed first.
Hi Sue,
I’m a cardiac RN, very new to this world of ME/CFS. I’ve been a medical mystery since 3 months after my pregnancy 6 years ago.
I watched a recorded webinar on YouTube of Dr. Nancy Klimas to IM physicians in New Zealand (2011). In the video she discussed Starling’s law and how low intravascular volumes returning to right heart cause ineffective pump through ineffective stretch. I found it fascinating as a heart nurse. Ineffective pump=faster HR=symptomatic. Her recommendation in that video was low-dose beta blocker (slow HR to allow R ventricle to fill) then increase blood volume with Gaterade twice daily and water plus salt tablet replacement-if no contraindications exist.
I haven’t even been diagnosed yet, but found a cardiologist willing to tilt test and try this therapy plus IV replacement weekly to see if it helps.
Thanks for telling us about Dr. Klimas video. Good luck with everything and please tell us how it goes.
You might want to read the article I believe it was on Forums about an oral saline solution being as effective as IV saline. Lots less trouble
It’s the latest resource in our Orthostatic Intolerance, POTS and Dysautonomia section
https://www.healthrising.org/forums/resources/categories/orthostatic-intolerance-pots-and-dysautonomia.119/
It is an interesting article Cort Thank you. I also agree with Sue re the right and left side of the heart functions.
I developed heart failure and was diagnosed with cardiomyopathy at 50 years of age of after thirteen years of almost unrelieved tachycardia because of my ME which had been triggered by a Coxsackie B virus.I had no blood vessel damage but the left ventricle was very dilated after exertion. Unfortunately this undiagnosed POTS was not recognised at the time or treated until this episode. I am happy to say that I am still alive and with appropriate treatment the cardiomyopathy seems to have reversed.
I will be very interested to read further information on the effect of ME/CFS on the heart as I know it has always affected mine
This bloodflow problem must be aguired. We didn’t born with it. The low blood volume is an adaptation to the veins. These are narrower by an autoimmune autonomic nervous system problem in the veins. Increasing the blood volume with fluid infusion is meaningless, you will pee it out 🙂
My instinct is that you’re probably right. More of an autonomic issue.
I remember Cort’s article about Dr Bell treating his patient by greatly increasing her blood volume. It worked for a few days until it didn’t.
If you buy a heart rate variability biofeedback monitor like the em wave, you can learn how to manipulate your breathing to balance the sympathetic and parasympathetic activity.
Until we get more answers, controlled breathing may be a powerful therapy.
IV saline is no cure, but I have it every week. Using a MIO Alpha HR monitor for two years, and now a FitBit, I can see that my POTS is improved in the days following, as is my heat tolerance. Improved but not gone. It often helps my sleep for a few days too.
Hi Carollynn,
I wear a Fitbit HR too! It definitely evidences POTS. Every time I go from sitting to standing it documents a 20-30 beat/min increase in HR. I used this evidence to persuade a cardiologist to tilt table test me. If that is positive, I will try a low-dose beta blocker with IV hydration to improve filling and stretch/pump action. I’ll let you know how it goes.
You might be right. I would argue that people can benefit from increasing their blood volume – I think that’s been shown – but it obviously doesn’t fix ME/CFS so there’s a lot more to it.
Is that what the Norwegian Researchers Fluge et al are looking at, amongst other things? They might be on to a winner.
I would like to make awareness of an association between CFS & a simple vitamin deficiency which is being misdiagnosed worldwide.30yrs ago postnatally I was diagnosed with ME . 3yrs ago I crashed low cortisol,profound fatigue,liver & gut inflammation.It Took me 15 Drshere in Australia including 7 specialists ,,2 brain & thyroid scans before a diligent holistic Dr gave me a diagnosis in 2 visits.of vitamin B12 deficiency with a genetic mutation MTHFR .Since then I have diagnosed at least 10 persons including my husband who has had DVTS ,atrial fibb,depression,PE ,memory loss,peripheral neuropathy in both feet.Last Nov his MRI showed SACD which is permanent nerve damage in spine.This all could have been prevented by early treatment .
Hi Marilyn,
I have had ME/CFS for sixteen years, and would like to ask you if you could give me the name of the Doctor you went to as I live in Australia too. I am presently in New South Wales but will be moving to Queensland as soon as my house sells.
I just had my vitamin and mineral levels checked a couple of weeks ago and all was fine. So I’m wondering if this will help me.
I would really appreciate some more information if you have the time.
Kind regards,
Debra
Debra,
I am in Brisbane. My daughter has had CFS (moderate) since she was vaccinated and caught a virus and vaccinated again via the BCC! All at the age of 13! She is now 20. I would like to keep in touch with ‘locals’ to compare treatments, doctors etc. if you are interested let me know. Not sure how we translate this communication to a more personal level?
Thanks again so very much, Cort. I am seeing an interested cardiologist about a-fib, have told him of Dr. Peckerman’s study and am now unfortunately taking a Beta blocker(makes one wearier). Will tell him of your latest article. It all helps!
Dr. Cheney has a different explanation for “small heart syndrome”. His 3-D echocardiograms show a change in shape of the heart at different elevations on a tilt-table. Most observations of a small heart take place with the patient upright, as happened with an X-ray of mine years ago. The original report thought I might have an enlarged left ventricle, as happens in known heart disease. On reanalysis the problem disappeared. It was years later before I made the connection with observations made while upright or supine. In supine posture my heart looks normal. Upright it looks like the left atrium folds in. This at least suggests low intake pressure at a place where this is particularly difficult to measure.
Hi Anciendaze I am in Australia and my supine echocardiogram showed normal left ventricular size when I was in aytipical heart failure. A stress echo showed immediate almost total dilation of the left ventricle as seen in myocardial infarction. However all vessels were clear on an angiogram and there was know understood explanation for the cardiomyopathy I had at the time. The cardiologists had no idea of ME/CFS.
Hi Maggie,
From your description I’d guess that most doctors would not call this heart failure, even though your cardiac output while upright would be in a similar low range. The absence of structural defects and coronary artery disease is typical for ME/CFS. In general we are talking about episodic changes in vascular compliance rather than the structural defects cardiologists are trained to look for. The episodes can take place every time you stand up, yet still be missed by doctors looking for something else.
My latest wild idea is a defect in a process called functional sympatholysis though most work on this is found in sports medicine. I would be surprised if this happens without the presence of autoantibodies which form complexes with target molecules degraded in the cell. A byproduct of this process is a change in purinergic signalling.
Unfortunately, the standards for testing such things as anticardiolipin antibodies were adjusted to match diagnosis by clinical signs like the rash in lupus. Since ME/CFS does not produce convenient clinical signs this means all such patients will be unlikely to rate a diagnosis of an autoimmune disorder. Antibodies seen in other life-threatening condition like those to GAD65 or N-type calcium channels are newer, and the medical profession hasn’t figured out what to do with patients who test positive, but do not have, e.g. diabetes or cancer. This looks like “the tip of an iceberg” to one expert.
I just went back and read an earlier post of yours concerning infection by Coxsackie B virus. This makes me wonder if you have antibodies to GAD65. One hypothesis for the cause of these is molecular mimicry by that virus. All the people I’ve heard from who have antibodies to N-type calcium channels appear to have POTS with prominent tachycardia. Other symptoms are less consistent. These are just two possible autoantibodies which show up on tests in other cases where people have unusual problems that sound like yours.
That is interesting Anciendaze as at the time my CFS specialist who I had just found queried involvement of the Coxsackie B virus. He also mentioned an article by Peter Behan in Glasgow regarding malfunction of ion channels in ME/CFS. This was in 1999. The other finding was T-wave flattening which could have been consistant with hypokinesis or ischaemia which was ruled out. The exact aetiology has always puzzled me so I am pleased to find reference now to cardiac issues. Thanks for responding.
Thank you Cort for the valuable contribution you are making by reporting the research and providing a place for feedback.
I’ve had chronic fatigue for 35 years with MYTHFR and the “dreaded genes.” I had a silent heart attack years ago with no damage and arithymia for which I take a half of a beta blocker. I decided at age 40 that I wanted to be a “strong old lady to do service in the world” and would follow the research as I believed there would be help found before I died. Optimistic yes, but I choose optimism to do my life. I write in the self help field on positive mindset, trauma, anger management and narcissism with a lifetime of service which will continue as long as I can. Even though I have many related illnesses, I am stronger, healthier and happier than my same-age friends who do not have chronic fatigue.
Decisions I made that have helped me stay strong at age 78 are a positive attitude, clean diet, recommended supplements, weight training in small amounts as I don’t have stamania, and deep breathing. What has helped tremendously as I lie awake at night with insomnia is a CD program on Prayana breathing by Rodney Yee. His soothing voice gives guided instructions on deepening the breath. This has made my diaphragm and stomach like a bellows that must get more blood moving through my heart. The CD is at https://www.amazon.com/Breathe-Guided-Breathing-Exercises-Revive/dp/B000BT96GY/ref=sr_1_1?s=books&ie=UTF8&qid=1467126961&sr=8-1&keywords=Breathe+CD+rodney+yee
Thanks Lynne, I would not be surprised if my attention to diet in particular will end up with me healthier in some ways than my peers as time goes on even though I will be much more limited than them. (I do wonder about the lack of exercise though….)
I think deepening the breath is probably a great idea – it does help with parasympathetic nervous system functioning, for instance. Thanks for providing your protocol .
I just started on deep breathing Pranayama CDs by Richard Rosen, an excellent yoga teacher in SF Bay Area. It’s helping with sleep and moving into a parasympathetic state when pain levels are not too high. Looking forward to listening to more.
I like your image of the bellows to get the blood moving.
Being optimistic certainly doesn’t hurt. Let’s hear it for feisty women with ME.
I’m interested in the apparent distinction being made by Miwa et al. using ME vs. ME/CFS , as there has been a good amount of discussion here and elsewhere about whether ME is a brain stem-related disorder as opposed to CFS, which is another invisible disease without a known etiology. Perhaps in the case of ME, but perhaps not CFS, the heart is affected?
I suspect that the heart irregularities found in many persons with CFS are caused by hyper elasticity of the connective tissue in the the heart. There is a strong correlation between Ehlers-Danlos Syndrome, POTS, CFS and FMS. The systemic weakness caused by structurally defective collagen can result in impaired function of large organs and muscles. Unfortunately at this time it is not possible to test for this defect. In my opinion it is the most probable cause of the diverse multi system disorders found in CFS.
Methinks this study is very significant. Could explain a lot of the exercise issues. The key is what is causing it, and how do we fix that.
I’ve been itching to share this and this seems like a somewhat suitable time–only because the heart is the topic.
I’ve had tachycardia for years, which developed into A Fib with RVR. To make a long story shorter, I started taking a low dose of Flecainide, an anti-arrhythmic, a few months ago. I noticed a dramatic increase in energy soon after starting it. Tried stopping it a week ago and energy levels dropped, started it again, energy levels went up.
I haven’t had this much energy in at least fifteen years. A ballpark estimation–I’ve gone from 45-50% (housebound most of the time) of normal functioning to at least 70%. I’ve been shopping, cooking, cleaning, and socializing. WOW!
I told my electrophysiologist about it and he said Flecainide should have an opposite effect–less energy, not more.
I’m so thankful; I wanted to share. Sorry it’s off topic. Maybe one of those great researchers out there can figure out why I’m having this response.
Tami–Fabulous that this drug is helping you! It’s the perfect place to share this, while we’re now talking bout many things with heart/cardiovascular symptoms. I wish you continued improvement and many many great days. With some envy. : )
I agree – great share Tami and congratulations. How interesting that the drug increased your energy levels! I wonder what that means….I wonder if its doing something in addition to smoothing out your heartbeat irregularities.
It reminds me of Rachel who went on an MS drug Copaxone and her energy levels went way up…That does not happen in MS.
Thanks Cort and others here for the most important subject area in ME/CFS. This is my view after twenty years of this illness and heading towards age 70. I hope that good researchers will continue to target the cardiovascular system. Dr. Byron Hyde wrote that he believed that problems in the vascular system would end up being key to ME. Like some of the other commenters here, I think that an autoimmune process and problems with the autonomic nervous system are involved. These are all central players in the body affecting more than the cardiovascular system, but if researchers would hone in more on the cardiovascular system and discover its abnormalities, we might “get more respect”, funding and a helpful focuse for treatment.
Thanks for the kind reassurance, Carollynn.
I understand about a bit of envy. I’d feel the same way. Being able to do some of the things many “normal” people take for granted is something I’m so very grateful for–something that’s been a longing of mine (probably a longing of all of us), for many years.
I’ve been down a few days. Of course, when I felt better, I declared myself well and did too much.
Toni Bernhard writes about the Buddhist idea of practicing mudita, taking joy in the joy of others, when we feel envy. The poet Rumi said something about “be with those who help your being.” If we can’t find mudita and that support for our being in a patient forum, where in the world will it be?! Practicing mudita really does increase it. And then your good feelings do too. It’s a wonderful perpetual loop. Thanks for being part of it.
I have only just caught up on emails and read this post. I was very interested as I was due to go for an echocardiogram after a bout of atrial fibrillation two months ago. I mentioned it to the doctor before the scan and at the end he told me that I do indeed have a heart that is slightly smaller than usual, and all the chambers are smaller. (As for the rest of it, all is fine. My GP, the doctor today and I all agree that the atrial fibrillation was most likely a one-off reaction to a change in my asthma medication.)
I wonder if this also explains chest pain? If I’ve over-exerted myself a bit, then sit or recline on the couch, my heart aches just like any sore muscle does after over-exertion. It doesn’t last long, and is just painful enough to be a solid distraction.
My masseuse, who advises me on exercise as well, wondered if the smaller heart is actually a result of resting and not exercising it. Muscles that are exercised grow in size. An athlete’s heart is larger than normal. It would therefore follow that the heart of someone who has had to rest, would be smaller. Only a hypothesis.
In answer to your question, my heart does not ache when I over-exert myself. It could be good for you to speak to the doctor about that one.
I wonder if we could be thinking about this wrong? What if there is a viral infection of the heart that disrupts heart-hypothalamus signalling?
I had reoccurring pericarditis for 2 years before getting CFS. Makes me think.. maybe the actual infection was in the heart and not the pericardium.
Hi Deltrus–I wish that the “we” thinking about this–right, wrong, every which way–was not just the patient and small research community, but teams of cardiologists who took our overall condition seriously.
Perhaps I’d say that the “small hearts” are in the cardiologists. And small minds. We need bigger thinking and more compassion.
I wish you answers and greater health.
Hi,
I remember reading somewhere quite a while ago now that in an autopsy performed on a person with ME/CFS that they found that the heart was carrying a heavy “viral load”.
Also, I have just finished reading a book by Anthony Williams called Medical Medium and in his book he says that this illness and many other so called “mystery illnesses” are caused by the Epstein Bar Virus!
More food for thought……….
There has been a lot of research trying to link a single pathogen to ME/CFS. No one to one linkage has ever been found. Instead what has been found is that numerous pathogens can precede it. So it suggests It is about how the body reacts. A permanent alteration in the immune system, which then affects the nervous system, etc. is what is being explored. No pathogens may even be found after a while, yet the body continues on in a down-shifted state. Low and slow…
Linda B
Hi Linda,
I have only just read through the entire comments section to refresh my memory and found your post. Sorry it took so long to get back to you.
I am in New South Wales at the moment with my house up for sale and then moving back to Brisbane. I would be happy to stay in touch, you can find me on debjog@icloud.com.
Bye for now,
Debra
Thanks Deb, hope the sale goes to plan and the move is not too horrendous.
Linda
I have had ME since at least 1973. On April 25th of 2018 I had a heart attack, and that day 5 stents were put into my heart. Four weeks later 5 more stents were added, and only the skill of my cardiologist prevented open heart surgery. An echocardiogram done in August showed scaring and mitral valve problems that at least in part due to the scaring. It also showed that my heart is small. Blood work showed me to be anemic.
How do I do cardio rehab when the ME rules out the aerobic exercise? Any information and links in this regard would be most appreciated.
Perhaps Peckerman was *too* good and therefore could not be published anymore.
My nuclear stress test showed 50% ejection fraction while my ECHO showed 65%. That caught my attention right away before even knowing anything about a cardiac connection to M.E.
My supine ECHO also showed a cardiac output lower than Peckerman’s study where he links an abnormal CO to the level of disability.
Thing that blows my mind is the cardiologist didn’t find anything wrong with a sub-4 CO and decreased EF with stress. Instead he said, “you have a strong healthy young heart… your tingling cold limbs are a nerve issue.” I mean, why even do an ECHO if you’re not going to analyze the data? Wow!
I don’t know why Peckerman wasn’t able to do a follow-up study. I looked for years for one. Still, it seems like one of the great missed opportunities. I believe he retired but I’m not sure. As I remember he only participated in another study or so.