Were you an avid exerciser prior to becoming diagnosed with chronic fatigue syndrome (ME/CFS)? Are you sure you were diagnosed correctly? Symptomatically, overtraining syndrome (OTS) and ME/CFS appear almost identical. Symptoms like fatigue, pain, post-exertional malaise, sleep problems and cognitive issues pervade both “syndromes”.
If it was not for the different triggers (“overtraining” vs infection, toxic exposure, “stress” in ME/CFS), the apparently more severe loss of function and greater duration seen in ME/CFS, one might think they were the same disease.
While some websites state that recovery from overtraining often takes several months, at least one, citing a 2012 paper – states recovery can take months to years, and that the condition can be “irreversible”. Not only can OTS stop training, it can affect “activities of daily living”, and may even end one’s athletic career,
In fact, it’s quite possible that some of the more athletic of us have an unremitting case of overtraining syndrome. One wonders if Jamison Hill, a weightlifter and athletic trainer, for instance, could have been diagnosed with overtraining syndrome.
Then again, it may not matter what you were diagnosed with. This study suggests, although the authors don’t state so, that it’s quite possible that ME/CFS and OTS are two branches of the same tree – one associated with athletes and the other associated with non-athletes.
A Methodological Mess Resolved
One difference, interestingly enough, is the degree of rigor with which the two diseases are in some ways being studied. While ME/CFS is being studied rather haphazardly, a group of researchers have committed to slice through the methodological issues pervading the OTS research fields to try and get at some answers which stick…
Just as we’ve learned in numerous review papers in ME/CFS, the OTS researchers trying to make sense of the field (and its variable results) were confronted with a bewildering array of possible confounding factors which involved the usual suspects: problems with selecting patients, problems with diagnosis, problems excluding participants when necessary, problems with the control groups and, last of all, problems with the tests and procedures performed.
The research group created the Endocrine and Metabolic Responses on Overtraining Syndrome (EROS) project which has encompassed a series of rigorously produced studies designed to methodically uncover biomarkers, etc. It appears that they’re succeeding. (They are also, like Ron Davis and the Open Medicine Foundation, making their raw data publicly available.)
Novel Insights Suggest Chronic Fatigue Syndrome (ME/CFS) Connection
The four studies that led up to this overview paper (“Novel insights of overtraining syndrome discovered from the EROS study“) produced some fascinating insights. First off came a simple but important insight into how athletic training results in significant metabolic and endocrine changes, including some changes that the OTS group retained: even though they were ill, in some ways they were still “fitter” physiologically than the healthy controls.
Not so with some other measures. The OTS group had regressed in a wide variety of metabolic, endocrinologic, etc. measures. In fact, the group had fallen off the wagon to such an extent, so to speak, that their tests were similar – no doubt to their horror – to the inactive healthy controls. This indicated that the overtrained athletes had lost some of the “conditioning” that had enabled them to be athletic. (Conditioning in this context does not refer to lack of exercise, but rather to the biological state needed to carry out intense athletic activities).
Plus, the study uncovered some upregulated results which suggested an attempt to compensate for their “reduced conditioning”.
Interestingly, most of the over-trained athletes’ test results were within the normal range. No doctor would consider anything amiss with the apparently “normal” test results they displayed.
These test results were only normal, however, when compared to the healthy controls. When compared to their healthy athletic peers, a large number of their test results were significantly abnormal.
This brings up an interesting situation. We know that no matter how inactive a healthy person is, they do have the capacity to exercise and get stronger – a capacity the OTS athletes have lost. Yet their results appeared absolutely normal. This indicates that even a string of seemingly normal or within-range test results – put together – can result in disease! A redefinition of what’s “normal” is clearly needed.
The Gist
Overtraining syndrome (OTS) and ME/CFS share numerous symptom similarities including, in particular, difficulty exercising
OTS can be severe enough to affect one’s ability to carry normal, daily activities and, in some cases, can be irreversible.
Researchers associated with the EROS project have identified a number of endocrinological and metabolic abnormalites in OTS – many of which have been found in ME/CFS at one time or another.
Most of the test results are found within normal range limits but together they appear to identify a process which can severely restrict a person’s ability to exercise.
These researchers have also proposed a similar hypothesis to that proposed for ME/CFS: that people with OTS exist in hypometabolic state that’s designed to save energy resources during a time of severe energy depletion – as in starvation.
Overtraining syndrome is not actually caused by “overtraining”: instead it appears to be a condition that can occur to any athlete. Athletes with poorer sleep, who engage in high amounts of mental activity and who have lower protein and carbohydrate intake appear to be most susceptible.
No joint ME/CFS/OTS studies have yet been done but the two fields clearly have the potential to teach each other much.
This theme – a constellation of seemingly minor but still significant changes working together to produce illness – is showing up more and more as medical research takes the performance of systems into account.
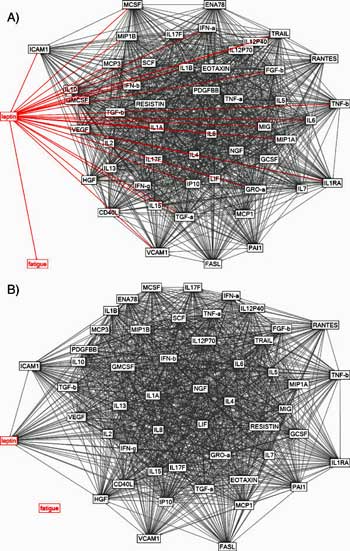
Younger’s results suggested that even at normal levels leptin may be a prime driver of immune functioning in ME/CFS.
We saw it in Dr. Klimas’s studies which identified immune hubs in ME/CFS that alter the importance a cytokine might have. In that scenario, even normal levels of a cytokine, could, if the cytokine is embedded in a hub which confers more importance on it, produce extraordinary changes. We’ve seen it in Jarred Younger’s Good Day/Bad Day medical study which suggested that, even at normal levels, leptin may be an important immune driver in ME/CFS. We saw it in Dr. Montoya’s study, which found few significant increases/decreases in cytokine levels, but still found that even at their “normal levels”, cytokines still strongly predicted fatigue levels.
The fact that none of these studies produced results that would raise a red flag to a doctor – and that none of the changes seen in the OTS group were found in all the individuals – suggests that searching for the magic bullet in OTS is fruitless. Far better to look to identify a series of changes in a system, which together, end up in a significantly altered metabolic (or other) state.
When compared to their athletic peers, the study found a wide variety of significant alterations. They included:
- blunted and late GH (growth hormone), cortisol and prolactin responses to a central stimulation test (possibly causing reductions in athletic performance).
- reduced testosterone levels (possibly causing reduced muscle mass).
- increased estradiol levels without a concurrent increase in testosterone (reduced testosterone-to-estradiol ratio) (possibly caused by metabolic abnormalities; body composition changes found).
- worsened mood states (particularly fatigue, vigor, depression and confusion) (fatigue is a “mood state?”), (probably resulting from sleep issues, hormonal dysfunctions).
- changes in body metabolism and composition (reduced metabolic rate and fat burning, more body fat, less muscle mass and hydration (possibly caused by hormonal changes that result in a state of catabolism (muscle breakdown) and hypometabolism.
Increased levels of creatine kinase and catecholamines (eg. norepinephrine/epinephrine) were also found and were believed to result from prolonged muscle recovery times and, with regard to the catecholamines, an attempt to stimulate the recruitment of energy.
Not all of the above findings in OTS have been reported in ME/CFS, but reduced testosterone (reported by doctors), blunted cortisol, increased estradiol, reduced growth hormone output, reduced metabolic rate and fat burning, reduced hydration (blood volume), muscle catabolism and hypometabolism have at one time or another been found in ME/CFS.
Given that most of the “abnormal” results in the OTS study were in the normal range, one wonders if a re-interpretation of past, seemingly negative results might be in order in ME/CFS.
Another Hypometabolic State?
However, while the changes from individual to individual differed, a general central effect was found – which led the author to advance a hypothesis – one which, they noted, needs to be validated by larger studies. That hypothesis, encouragingly, is similar to one that has arisen out of the metabolomic studies in ME/CFS.
It proposes that overtrained athletes are stuck in a hypometabolic state characterized by a “procatabolic environment”, in which the overtrained athletes’ muscles (instead of fats) are being broken down. The “global reduction in metabolic pathways” found, they believe, may have been produced to save energy and redirect energy for essential pathways during a state of (energy) starvation.
While metabolomic studies do not appear to have been done in OTS, the ME/CFS and OTS groups appear to be arriving at a similar conclusion – a starvation-like state may exist – perhaps Naviaux’s Dauer state. Hypometabolism, catabolic environments and a starvation-like scenario have all been applied at one time or another to ME/CFS. Hypometabolism is believed be an adaptive state that humans or other organisms can enter into in response to a variety of triggers. (Hypermetabolism has been proposed for ME/CFS as well!).
While the study focused on metabolic and endocrine factors, the authors proposed that virtually all the system dysfunctions found in the body (metabolic, hormonal, inflammatory, immunological, neurological, cardiovascular and psychological) have worked together synergistically to create a “dysfunctional hypometabolic” state found in OTS.
Say Hello to “Paradoxical Deconditioning Syndrome”
Interestingly, the researchers did not find overtraining to be a factor; i.e. very high levels of exercise are not necessarily associated with OTS. Instead, they found that high levels of study (>8 hours/day); lower levels of carbohydrate, protein and total caloric intake, and poor sleep – in combination with athletic training – all increased the risk of coming down with OTS.
Therefore, the authors propose OTS be called “paradoxical deconditioning syndrome” – a strikingly similar name to the “systemic exertion intolerance syndrome (SEID)” name proposed by the Institute of Medicine report for chronic fatigue syndrome).
A Collaboration Waiting (Begging?) to Happen?
ME/CFS and OTS potentially have a lot to offer each other. Using a stringent methodology – one which has probably not been employed in ME/CFS – the EROS researchers have been able to uncover numerous metabolic and endocrinologic abnormalities.
I was unable to find, however, any maximal exercise or metabolomic studies – two areas ME/CFS is strong in. The recent paper from Gordon Broderick’s and Dr. Klimas’s groups, which integrates endocrine-immune modeling with extensive sampling during exercise, would surely interest these OTS researchers. The ME/CFS field is also becoming strong in mitochondrial studies – another area of potential interest in OTS.
This is a collaboration practically begging to happen. Similar findings are cropping up in two mysterious diseases that are defined by the inability to exercise. Maybe a session devoted to the similarities and differences between ME/CFS and overtraining syndrome at the next IACFS/ME conference coming up from June 10-13th at Stony Brook University on Long Island would help spark some collaborations.
Exercise and Overtraining Syndrome Poll







No comments yet! First! Glad to see this. I am thankful that I was introduced to this perspective early on by Dr. Oddbjørn Brubakk (more than a decade ago). High-functioning individuals are often versatile and tough enough to compensate for their weaknesses, acquired or not. Because we figure out a way to survive and keep moving (to avoid deconditioning) doesn’t mean we should have to suffer. If I had no memory of being a talented, capable human being, my handicaps and pain wouldn’t bother me so much.
I don’t think I have OTS, I developed Fibro after a major back surgery (my first of 3), but yes I was in the gym most days prior to this and did HIIT at home. Mmmmmmm, is love to go into remission. Since taking HRT however, most of my Fibro symptoms have reduced, but not gone…… sex hormones and Fibro are linked and I cannot wait to start testosterone gel for women in December. Let’s see what happens then……. all very interesting.
First, I was under a lot of stress at work, then I started working out almost daily to get rid of stress, developed panic disorder, depression, doctors said that working out helps with depression also, one thing that suffered was my diet, that eventually led me to a major crash, dropped working out and started different combination of antidepressants with I still take now I’m bedbound most of my day, except when I fell strong enough to go food shopping.
I thought the finding that lower caloric intake was a risk factor was fascinating. I just wonder how that helps flip whatever switch gets flipped. There is this switch to breaking down the muscles – maybe in some people this switch gets flipped earlier than others when caloric intake declines during heavy activity.
It makes me think of when I got ill. No trigger but I was exercising a lot and exposing myself to cold temperatures a lot – I was basically seeing how much I could stand! Some weird male thing 🙂
I am a bit surprised by that lower caloric intake being a risk factor too.
But then I guessed that they did not measure fat caloric intake specifically. And many athletes (and health concerned people) swear by not that much fat so “lower levels of carbohydrate, protein and total caloric intake” could be mainly just less carbohydrate and protein. The paper seems to point that fat wasn’t taken specifically into consideration.
Why suspecting that one:
* carbohydrates (glucose) fuels the pentose phosphate pathway, an important pathway for generating NADPH that in itself is important in fighting oxidative stress (something athletes, students and people lacking sleep could have trouble with) and for the immune system in general.
* protein can quickly “create” carbohydrates when glucose dips too low.
Basically you do not only need energy for activities but also for defense and repair of your body. If you go on a burst of activity (and studying for 8 hours can be such strong load on energy consumption in the brain, which is “hampered” by not every energy source like fat passing easily trough the brain-blood barrier) then you generated plenty of ROS. If you don’t have enough “quick” sources of energy or sources that pass the BBB well enough during that burst then you may make your cells sitting ducks to aggression like ROS or pathogens.
As to lack of sleep, it makes the immune system trigger happy. Mainly the basophils and mast cells seem to be a lot easier to trigger and that causes a “shower” of inflammatory chemicals plus ROS. I doubt that is good for athletic performance.
Some of it could be part of it.
I’ve been convinced for a long time that ME/CFS is triggered by the total load of various stressors. Dr. Hans Selye described this in his work on the general adaptation syndrome, which I learned about through the work of Dr Poesnecker. Factors including extreme temperature, exercise, diet, infections, and emotional or mental exertion can all contribute. Selye described 3 stages, ending with exhaustion, which matched my experience as I went through different stages of illness. I started with insomnia, then other symptoms, then total exhaustion.
The caloric intake question intrigued me, too, as I’m one of those whose ME began in their teenage years with gastroparesis. My appetite was good, but as I couldn’t digest the food properly, I kept losing weight – whilst trying to carry on as usual, of course. It was only after some months of continuing weight loss that the fatigue and pain came fully into play.
I have often wondered about a link between eating disorders and CFS. Excessive exercising is very often a component of eating disorders.
Does the self induced famine and/or exercise induced physical stress flip the switch on CFS ?
Should eating disorders be researched as a risk factor?
I had an eating disorder in high school and college which I fully believe set the stage for my OTS/CFS/ME. Where there are micro and macronutrient deficiencies combined with genetic predisposition and stress/trauma/infection, there is a perfect storm. My symptoms began after my second Ironman race in late 2009. Fortunately I’ve been able to work and have children, but I have not been able to get anywhere close to my previous level of athletic talent and over time my symptoms have gotten worse.
An Ironman participant! Wow….Obviously in very, very good shape. This can obviously happen to anyone. That is very good for everyone to know…Thanks for sharing that.
I had no MECFS trigger and a slow downhill trajectory. I searched overtraining syndrome many times along the way as it seems to almost fit for me. My reluctance to accept it totally, was due to the fact that i wasnt training obsessively, just ‘healthily’. However i was working a busy computer job, extra project and home reno going on. (? 8 hours ‘study’)
When i decided to get fit again after a 15 year break I cleaned up my diet, dropped some calories, mostly carbs and processed food. Total calorie intake was not too low. I was however probably eating almost no salt!
Another factor that would perhaps increase the impact of this exercise/diet was that it was in midlife when most people add a few pounds, but I lost weight, got fit, felt great until it began to unravel.
Elite HRV have a fair amount of info on overtraining and how it manifests in HRV measurement
That all adds up doesn’t it? Interestingly. All that may equal the stressors imposed on the body by a serious infection. As I noted in another comment. I was in a new environment, exercising a lot and exposing myself to much colder temperatures than normal. Could that have done it?
Another interesting thing I learned is that some form of OTS – a lesser form – is actually not uncommon in athletes. It’s like they dip into a form of ME/CFS when overdoing it – and then pop back out again.
I recently went down with OTS. This is the second time I’m getting OTS, first one when I was 17 years old, 7 years ago. For the current case I exercised intensely 4-5 times per week (i’m a 57kg female powerlifter). I also did cardio (a 5k run) twice per week. My diet is healthy and sufficient in calories, however had a lot of work related stress and slept too little every night. Im currently on my 25th day of solid rest and I feel considerably better.
I’ll try to explain the situation of both times for those of you who are interested: (sorry for my English, it’s not my first language)
Overtraining case 1:
I was 17 years old, I exercised with light weights 6 times per week, 2 hour sessions. I also walked a lot ((6-7km per day). I didn’t eat enough because I wanted to lose weight. I was also studying really hard for my final exams at high school. One night, after dinner, i went to bed and as my head hit the pillow the whole world started spinning. I felt fainting, my body went stone cold and I was sweating despite the low temperature. My heart is was racing. My parents took me to the GP next day, did many blood tests, they all came back normal. After 3 days in bed, I felt better, decided to go to school again. Then after a week at school, I got the exact same episode again. My parents took me to the emergency, re-did tests etc, everything came back normal. I saw an endocrinologist a week later, no thyroid issues etc. While feeling so helpless and not being able to understand why I was feeling so extremely fatigued, severe brain fog, depression, hypoglycaemia, pain all over my body, cognitive issues, and wasn’t even able to walk.. the endocrinologist mentioned the possibility of ‘overtiredeness’
..Gave me some supplements and told me to rest and not exercise until I feel better.
Fast forward about 6 weeks later of solid rest (and a lot of studying for my exams), I went back to my normal life. However didn’t exercise again for the next 1.5 years (I was able to, the overtraining was pretty much totally over in like 2 months just didn’t want to due to ptsd from that horrible episode and having no idea what the problem was whatsoever).
I never really understood what had happened back then, until about 2 years later when I figure out that overtraining was a thing.
Case 2 (current):
Now, because this is the case I’m currently in, and being aware of CFS/ME and overtraining, I was able to fully pin-point my symptoms.
I’m 23 years old (24 in 2 weeks time). Working my first graduate job in London (for which I had to relocate and it’s been a year now) and trying to adjust to my ‘new’ life. The last few months I had a LOT of personal life stress going on, too many huge changes.. I had increased the intensity of my training a lot so I could deal with the personal stress (without taking rest weeks anymore because I somehow decided I was invincible) and slept very little every night as I had to manage my (quite large) social media.
I was okay until early August of this year that I had noticed some weird symptoms. It started with:
low mood (I cried literally everyday for no reason)
sleep disturbances (I’d wake up and struggle falling asleep afterwards)
I also had nightmares that I remembered the next day
nightsweats (I used to wake up several times during the night covered in sweat, it was disgusting)
a lot of anxiety and DOMS even by light exercise that shouldn’t have caused me DOMS at all. I started complaining about being very tired, my boyfriend was sick and tired of me talking about how tired I was every day, he had noticed something wasn’t right.
Me being me, I tried to push through the workouts even when I felt very tired and clearly something being wrong with me.
That continued for about a month, my strength in deadlifts was REALLY low (for those of you who lift, deadlifts are the first lift to go downhills when you overtrain, so keep that in mind as an indicator), however end of August I hit my last PB in squats. The next day I felt like death. Despite that, I went for a 5k run. And then dragged myself to the gym for the next 13 days.
On the 13th day, (13th September) I crashed. A similar situation as my first overtraining story. Then until the 20th September, I was struggling to even walk. My brain felt so ‘thick’ that I’ve been struggling to think clearly and I have memory loss too.
I decided to take some time off work, and finally the dizziness is now gone and I’m not so reliant on sugar anymore (I used to eat every 2 hours so I wouldn’t faint from hypoglycaemia). Today is the 25th day of my recovery and I can finally go outside and buy food when I need to (I couldn’t even do this for like 2 weeks). I’m still feeling very tired, still have cognitive issues (hand to eye coordination), elevated heart rate, a very low mood etc but at least I now have more energy to walk, I can focus on things better than 2 weeks ago.
I’m currently trying to document all this process, I’m monitoring all my symptoms everyday and note down any changes as I’m also trying to ‘find patterns’. I really want to write a very detailed report on my story of overtraining because I want to help anyone who feels the same way not feel alone.. So far the only ‘abnormal’ result I’ve had was my SHBG, which was lower than a post-menopausal woman’s. My testosterone is normal and my free androgen index is too high (note, I’m a natural athlete, never took any substances)
My blood pressure, blood sugar, heart health, full blood count, iron levels, vitamins, thyroid, electrolytes, liver function, kidney health, bladder have all been normal. No infections, no other illnesses.
I’m planning to get my cortisol checked one of these days, because my GP is convinced I have heart problems and he’s probably gonna refer me to a sports medicine doctor when I’ll have recovered already. doctor’s help has been a joke, I have no idea how some doctors nowadays even got their degrees.. they’re not even trying to help. I’ve been buying tests online to check these things.. I use a company called Thriva.
My advice to people who have overtrained:
RECOVERY
In order to understand for how you have been overtraining, you need to think about your last best session. That session has been a phase 1 overtraining with a ‘fake’ peak and adrenal crash straight after. Then when you know the X days you have been overtraining, multiply that amount by 2. That’s when you’ll start feeling normal again (maybe not good enough to train at full capacity, but good enough to carry on your daily activities). To be able to train you’d probably need another 1-2 months after that. And you’ll need to start very light and it’s good if you do the alternate recovery day. So one day recovery one day training everytime. Bear in mind that 50% of the above recovery time you’ll feel absolutely horrible. You’ll hate every minute of it. But it’s part of the process.
Another important thing: you’ll probably have to gain some weight. For me personally, extra weight has really help shift some of the symptoms quickly. Try to keep diet like 80% healthy but it’s totally okay to eat doughnuts everyday to make up for the extra calories, after all, it’s just a temporary solution.
When doctors make you try ‘elimination’ diets, I’d say, don’t listen to them unless your symptoms are related to like celiac disease or something. Or you possibly have an allergy.
Food supplements help (especially iron, B complex, magnesium and vitamin D) so make sure you supplement in those throughout your recovery.
Cut down all stimulants. No coffee, because coffee will make you crash badly.
Try to sleep at least 8 hours.
Measure your temperature frequently. If it falls, take a hot shower. For me, low temperature has been a thing so I have to keep an eye on it at all times.
Drink a lot of water. Overtraining makes you feel dehydrated so make sure you hydrate frequently to avoid that horrible ‘dry’ throat feeling that makes you choke on your food.
Try to eliminate stress. Take some days off work or get on a light duty period.
For women: if you have amenorrhea, definitely see a gynaecologist. This can prove to be irreversible.
Keep a journal and log your symptoms. It will keep you motivated and feeling better on those really bad days. And try your best to avoid overtraining at all costs in the future. For myself, I’ve definitely learnt my lesson this time. I love training, but nothing compares to waking up in the morning and not feeling excessively tired.
Also don’t expect a linear recovery. It will have ups and downs. It’s okay, it will be fine.
Last note: if you have been in a forest or something like that recently DEFINITELY check for Lyme disease. Lyme disease has the same symptoms as OTS/CFS/ME, except it can kill you. You can even order a Lyme test online, it’s just a finger prick test, no needles. Costs about £40-50. No harm in excluding the fact that you might have Lyme.
Hope that has helped someone out there, if you’re going through the same thing and need someone to talk please reach out to me.
Very similar story, Ihad been working hard and then I decided to change my working schedule, returned to a more relaxed approach to work and returned to swimming 1-2 times a week, a bit of weight lifting and surfing when the waves were good.
I improved my swimming a lot, got stronger until that day, six months later, when I felt some kind of weird tiredness before going to the pool. From that day on, it´s been a slowly downhill journey.
Currently, part time work is all I can do.
but with less carbs and no salt you likely didn’t get a lot of iodine anymore?
In genetics, most proclivities are caused by multiple ‘nudges’ from SNPs plus environmental factors. There are few disorders caused by a single gene or SNP mutation (that we know about so far).
I think first comparing what would be considered ‘normal’ chemical pathways in energy production to pathways of ME/CFS patients might be a good place to begin. Since we are all different and what treatment works for one patient often does not work or all, it seems to me that there might be, multiple minor ‘glitches’ working in concert, much like genetics, to bring about states of fatigue. Each of these clusters of ‘glitches’ might be different for each individual–hence the difficulty of defining the underpinnings of our disorder.
I know what I am suggesting is probably impractical given insurance and the costs of tests, but to compare across the board, the ‘healthiest’ with the sick and sickest, would give us some grand overview so we might better pinpoint exactly where the variances, the ‘glitches’ are. Then researchers could attempt to correct the ‘glitches’ (with supplementation, medication etc.) for each individual to see whether it might be effective treatment.
Probably I am trying to reinvent the wheel, but to have someone put together a large universal biological template (shared among researchers) to compare ME/CFS individuals with what is considered to be normal, might be useful.
I agree Nancy; I think it always helps to think ‘outside the box’ with analogies from other disciplines, like Dr Paul Davies’ (a theoretical physicist) intriguing insights into what may really be going with cancers. (I wonder if he’d be interested in tackling ME next?)
Maybe some sort of really large scale systems analysis via computer modelling of trillions of data points might enable us to clarify the underlying essential patterns and individual factors within all our heterogenous triggers and presentations. (Biobanks could perhaps be a source of such data points but more detailed info, even if it seems unrelated, about people’s lives before ME hit, might be needed from participants/donors.)
Of interest would be: do the OTS folks have unremitting flu feeling, toxic feeling, nausea, and cognitive problems?
Different websites give different symptoms but here is from one website:
Yes, flu-like symptoms like headaches, nausea, fatigue, indigestion issues etc are very common in OTS. Also cognitive issues + tinnitus. Severity varies.
Why not just call this Overwork Syndrome? Isn’t that what is being discussed? The type of overwork is a combination of daily/usual mental and physical activities, plus poor sleep and some dietary restriction or lack. The body responds eventually by going downhill and losing its former resilience for an unusually long period of time, including possibly permanently.
One thing which must be determined is why some people’s bodies do this and others’ do not. The metabolic trap?
One of the most interesting things about this review was that “overtraining syndrome” was not the result of overtraining; i.e. people who pushed themselves harder athletically were not more prone to getting sick.
On the other hand studying A LOT and not eating as much protein and taking in as many calories contributed. Poor sleep is an issue. As you note – the big question is what starts all of this off?
We are all descendants of tough people who survived human history. One thing I haven’t seen mentioned anywhere, from a historical perspective, is the success of our modern societal impact on survival rate. Just think how many people are alive today who would have died in childhood, only 100 years ago. Certainly some of us would have died from “overwork” or tuberculosis, or malnutrition, had we been born in a previous era. Imagine dying from the flu at the age of 19. Death was swift and common. Anyway, I wonder how many people are pushing themselves harder today because they are trying to overcome some physiological or chemical defect/oddity (consciously or unconsciously)? Or pushing to hard to keep the pace with peers, not knowing the line that defines “too hard”, for them as an individual, until they’ve crossed it?
I have an idea for a research project. Survey people with ME/CFS for the following information: “Have you, or one or more of your ancestors “escaped death” for any reason at any time in their lives _before_ reproductive age? Could narrow it down with more questions such as “What main reason helped them survive this event or defect long enough to reproduce?”: scientific insight | medicine | bullheadedness, luck, or miracle… etc.
I totally agree with this likely being a result of prolonged, extreme stress from multiple sources. As it has been pointed out, not everyone with OTS had been necessarily over exercising. A common theme among the descriptions here of how illness came about for people is that some sort of stressor, such as more exercise, poor sleep (that is new) or an increase in work related stress, was added and/or prolonged. Perhaps individuals who are predisposed, whether metabolically or by some other genetic variant, hit a breaking point and the body just seems to shut down. This essentially forces a person to cease engaging in activities that are the source(s) of all stress on their systems. (I believe this is what happened to me.) Maybe OTS is more common in athletes since they do have a tendency to be especially resilient and have the ability to “run through the pain”, so to speak. This resilience can be to their detriment, however, because “running the the pain” is basically ignoring the body’s signals to stop, thus worsening an injury. This can translate to just overdoing it in general, despite the extreme stress. Maybe it’s a survival mechanism? But, things do seem to go awry beyond that of just survival, especially for those who don’t seem to ever recover. Here is where inflammation may play a role? Although, thinking about that more, there is a survival mechanism that where, after multiple bouts, some body systems don’t ever recover. A good example of this is starvation, which includes over restrictive diets and yo-yo dieting (like the calorie reduction mentioned!). Metabolism slows down as a means of preserving energy to prolong survival and this can become permanent. Perhaps it’s an adaptation in the face of frequent famines? Maybe this “ability” of the body to preserve itself is how my homesteading forefathers were able to survive such extreme conditions? I also agree that a thorough look at a person’s life (and personality type?) prior to becoming ill is definitely essential. Whatever it is that is going on, I’m excited to see all this interest and possible collaboration! Cheers to everyone’s insight and input in this forum, too!
I still feel there is an infection going on here I was very athletic the last Guy I fought we both became Sick, was it a Hep B vaccine or was it antibiotics or was it Genetics Ehlers
Danlos Syndrome? I would think we are seeing here the complications of Ehlers Danlos Syndrome. If we had tests for EDS3 or HSD we would know Why? In some it is Alpha Gal & maybe some or
all have Eagle Syndrome undiagnosed, 6% of the World population have HATS & not all get Sick from it & some Negatives have Beta but they do not yet know what this
means at NIH/NIAIH…Maybe its time for an interview with Dr. Joshua Milner’s Team? I have also seen in Australia EDS3 & the Alpha Gal Meat Allergy & if Negative
on blood it could also be found in skin patch testing in an Allergist’s Office for Beef, Pork, Lamb, Dairy…Some Doctors say continue drinking Milk & numerous patients
disagree…Also it makes one Allergic to all Gelatin & also magnesium stearate…There is an Allergist in Australia she does only skin testing to diagnose
Alpha Gal…Think a Vitamin/Mineral or sugar is safe they are not they contain alpha gal…Is Alpha Gal in Antibiotics the answer is Yes numerous one the capsules usually come from Pig…
Aidan, have you seen that Alpha-Gal allergy can be triggered/transmitted by ticks: https://www.columbia-lyme.org/alpha-gal-meat-allergy
Yes, it is the main route how one gets the AG also I hear some types of flies carry this…The last Guy I had fought was a Gardener so maybe I
picked up something. The tests need to be out there I have the AG test here now & the HATS test but cannot get a Doctor to sign for Private Lab
testing. I do show Eagle Syndrome on Dental Panoramic x-ray & countless on the Group on FB are now diagnosed with Syncope/POTS
Fibro EDS so Yes it is involved…One Doctor from Scotland said she was poisoned by antibiotics she claims they caused her calcification in Eagle
Syndrome. She wrote a letter to the Editor of ‘The Eagle Has Landed’ complaining of these antibiotics…There is a Young Woman in Australia
diagnosed prior with Alpha Gal she also tested Positive to the Alpha Gal Meat Allergy I know blood & skim patch testing ‘both’ should be done, I
also believe in Sports Alpha Gal can be given if blood contact also would not be surprised the blood supply is contaminated. Wish you
wellness Debs did you get tested for the Alpha Gal? I also seen some Soldiers also test Positives to Alpha Gal numerous ones I imagine they
did all of the tests. My Friend in Australia not tested has CFS he reacts seriously to any Pork I think he has Alpha Gal as well…I think Ron Davis
should send bloods for AG testing…
Interesting. But I think it’s important to note that there’s a big difference between not being able to excersice, and PEM.
Do OTS show any sign of PEM?
PEM is not overtly mentioned but OTS is by definition a condition in which exercise eg exertion makes things worse and athletes have to ramp down or stop their exercise programs in order to recover. My guess is that it is present.
https://www.irunfar.com/2018/12/beyond-fatigue-understanding-overtraining-syndrome.html
Yep, I can unequivocally say it does from my experience. I used to get knocked out 6 weeks at a time after overtraining. And there were times I went out for a light jogging thinking that I was coming out of it, only to get knocked out again the next day.
Definitely part of the issue in my case. Myself and partner both caught some sort of stomach bug that wiped us out for a few days. We were vomiting within hours of each other. She stayed in bed for a few days but I decided to sweat it out down the gym and the rest they say is history, she was well in a few days and I slid downhill. Not totally convinced by hypometabolism in isolation but I am guessing we all have dormant genes that sent us off to hibernation not that long ago!! Maybe that why we feel worse in winter even if we live somewhere warm? I still feel my body is locked into sickness behaviour where some systems are down regulated and others hyper vigilant for infection and other stressors.
That may illustrate what I answered to Cort above. Here the key part referring to what you said:
Basically you do not only need energy for activities but also for defense and repair of your body. If you go on a burst of activity (and studying for 8 hours can be such strong load on energy consumption in the brain, which is “hampered” by not every energy source like fat passing easily trough the brain-blood barrier) then you generated plenty of ROS. If you don’t have enough “quick” sources of energy or sources that pass the BBB well enough during that burst then you may make your cells sitting ducks to aggression like ROS or pathogens.
=> A healthy person can have the energy to do activities or to fight off disease but not to do both at the same time. There likely is a reason as to why most infections make a person very tired: to save energy for defending the body and fighting of the infection. When you exercise that energy is not available.
The same happens when you are less healthy then you hoped for, when you were only a high achiever by pushing through your reserves, when not having the right fuel mix to allow for a strong burst in energy production when you had to combine activities with some increase in defending your body…
In order to clarify “not having the right fuel mix”. Even if they were athletes, they likely still had some fat reserves. So lack of available calories during the test period was unlikely the biggest problem in the “lower caloric intake risk factor”. To me it seems that “maximum energy production per time unit when needed” was a bigger problem. And fat stores (or intake) don’t add much to that one.
Danny B, that’s good evidence. It’s usually the other way around, it’s the women who push through illness. Men tend to get so wiped out (from the same illness) that they stay in bed until it’s past. Maybe this is why the percentages are so high for women, also with all “autoimmune” diseases, because more women push through pain and illness that most men would never do, and they shouldn’t.
Women also tend to have a higher pain tolerance (perhaps for child bearing?). This could maybe allow women to have a false sense that they are NOT overdoing it when they actually are? Cultural changes with more women in the workforce in addition to family and all their previous responsibilities. Overall, we are a stressed out and depressed society! It would be interesting to compare different cultures and OTS and ME/CFS.
As for theories about infection being a cause, I think it could be one of the many stressors that could tip off either syndrome. Perhaps the different combination of stressors and/or the type of stressor that was the tipping point, per se, explains the lack of consistency in abnormal findings in metabolic (catabolic, hypometabolic, mitochondrial – reduced ability to create and utilize ATP, etc) immune (Hypo or hyper immune responses, autoimmunity) vs rate of onset (rapid/sudden vs gradual) and every other factor being examined.
I was in training for my black belt in Taekwondo after 3 years when I was knocked for a loop with the most debilitating sickness that in a few short hours made me lose my memory, became excessively somnolent and hurt everywhere. As a single mother I pushed myself to continue to work and very slowly and painfully over a couple of years got much better but never again able to exert myself . I worked until age 58 and went on disability for ever weakening and increasing pain and brainfog – where I remain.
Whenever I read stories like this I am amazed that more researchers don’t find a disease which can knock out a fit person like you so quickly! This disease has so much to offer to science.
Je trouve que la recherche sur le cfs manque de méthode. Je ne comprends pas pourquoi on ne fait pas systématiquement un test du taux de métaux lourds, de perturbateurs endocriniens, de pesticides ainsi qu’un test fiable pour la maladie de Lyme. Il faudrait aussi mieux étudier l’interaction entre les stress psychologiques et les agressions physiologiques qui se sont accumulés dans l’histoire de chacun
They do diagnose this in countless Athletes Doctors but they use the term Burnout instead & think a few weeks of rest & no exercise Cures it
& if it does not, then it is Depression off to see the Wizard for some Wacko Drugs…One Woman today today told me she had a 24 hour
urine collection test for calcium levels, she has Parathyroid. Removed 2.5 of her glands, now also diagnosed with Eagle Syndrome waiting to
have Surgery done. Eagle Syndrome also seen in Sjogren’s Syndrome. This illness ME/CFS is so bizzare
Thank you for another interesting article.
Re. “In that scenario, even normal levels of a cytokine, could, if the cytokine is embedded in a hub which confers more importance on it, produce extraordinary changes” – could you maybe (for the human biology knowledge-deficient) illustrate this a bit more with a location > potential effect example/s?
I don’t think the ME/CFS – OTS similarities would be regarded as anything especially ‘eye-opening’ to Dr Ray Perrin, including the ascertained OTS risk factors. In his (2007) book, he discusses some of the past terms which have been applied historically to documented illnesses with ME-consistent symptoms. One of these was Da Costa’s Syndrome – described in 1871 by Union Army doctor Dr J M Da Costa in relation to “a fatigue disorder that affected about three hundred soldiers during the American Civil War. The soldiers had all been in active service for some while.”
Dr Perrin lists the symptoms and then continues:
“Dr Da Costa noted that when the soldiers’ signs and symptoms had eased, and after they had returned to duty, their performance on the battlefield was of a low standard and that they were unable to keep up with their healthy comrades. Dr Da Costa suggested that the cause of the problem was due to physical over-exertion and physical stress of the body, leading to an ‘irritation of the heart’. He proposed that the condition was sustained due to an imbalance in the nerve supply to the heart, which includes sympathetic nerves. It became known as Da Costa’s Syndrome, also called Irritable Heart Disease. Clinical scientist and cardiologist Sir Thomas Lewis (1881-1945), the pioneer of the electrocardiograph, wrote a paper in 1920 noting similar cases during the First World War, which labelled ‘Effort Syndrome’, also known as Neurocirculatory Asthenia. Lewis concluded that an infection was at the root of the problem.”
Dr Perrin’s belief is that the role of any infection in ME-onset is a secondary, rather than primary one. He asserts that particular (predisposing) physiological issues – mainly in the thoracic area of the spine, are present in all ME sufferers, and that these always pre-date the varying types of reported onset cause, such as infection, vaccination, environmental toxin, childbirth, physical/psychological stressor-associated.
He has also long related his finding that prior engagement in regular, prolonged study periods make for a further notable ME-development risk factor, which he believes is largely due to postural strains acting as additional exacerbation to the already over-loaded sympathetic nervous system (the latter typically resulting from a combination of problematic structural + additional SNS function-eroding stressor involvement/s). Dr Perrin theorises posture-impacting study, and other thoracic spine-strain-inducing activities, to be probable reasons behind his findings of relatively common incidence of ME amongst teachers, nurses, doctors and academics, along with athletes and performing arts-enthusiasts/professionals (such as cyclists, rowers, horse-riders, dancers and gymnasts) – and those pursuing combinations of these professions/interests.
While there may be differing pathological ‘strains’ of ME, I doubt (sticking my neck out a bit here) Dr Perrin would at this point be inclined himself to view ME and OTS as likely separate disease entities, having, over the past 3 decades, examined several thousand ME sufferers in his clinics with the same overlapping ME symptoms, and encompassing numerous variations and combinations of onset-type: whether gradual – eg, prolonged stress and/or physical effort-connected – or sudden – eg, viral, vaccine, environmental toxin exposure, post-operation/trauma/accident – or in-between/mixture of these.
Different types of ME onset all appear to be capable of producing very similar disease symptom-sets and patterns, (allowing for the reality that no ME sufferer’s illness is identical to another’s, even with ‘matching’ onset type). Dr Perrin reports the same specific, recurring structural-spinal issues to be a consistent factor present in all these cases. Surely this area of investigation is worthy of devoting more research support and funding than has so far been given?
I agree with spine involvement. I’m 46. I’ve struggled with scoliosis in back and neck my whole adult life. I studied intensively in college and grad school, had a stressful desk job. I certainly did not eat in a balanced way, focusing on keeping my weight down and limiting my time in the kitchen. My symptoms were made much worse by a car accident (whiplash). I’ve recently tested iGenex positive for Lyme and Cat Scratch fever (both of which I would have picked up in my youth). I have chronic sinus problems and difficulty keeping muscle. Before I became too tired, I loved exercising at the gym.
Thanks for your reply Nancy, and I’m sorry for what you’ve been struggling with.
I was very ‘Type A’ (mostly outdoor) exercise-wise too – that’s one of the particular torments about ME – so many doctors think it’s about deconditioning due to fear of exercise, when instead that’s the very thing that ramped up the physiological harm in the first place through your failure to get yourself to disengage with it! You then have to endure years and years of repeated, patronising and unbearably tormenting exhortations to do the very thing you can’t, and have spent decades painfully grieving over. The thing you so loved, and still psychologically *need (and are endlessly reminded is so valuable to good long term health) was long ago rendered either impossible, or both massively restricted and extremely damaging. But this terrible loss is forever pushed back in your face in a twistingly cruel, accusational form – reality inverted by their monumentally wrong-headed, but entrenched perceptions (fed by atrocious misinformation).
(I do wonder how reliable Lyme tests are at differentiating between borrelia types, but don’t know anything about the iGenex one. I think borrelia infection may be pretty much endemic, but it’s probably inconsequential in most cases, especially where the immune system is otherwise functioning reasonably.)
The caloric intake and exercise things sounds like how my ME/CFS developed, with some interferon treatment being the initial nudge.
During the treatment I developed gastritis and 2.5 years of insomnia. Since about two months into the treatment I’ve never felt like myself.
Post treatment I could still exercise at a high level 5-6 days per week, but due to the sleep issues my cognitive abilities were a mess. Memory, vocabulary, personality – they were all shadows of what they were previously. Pun intended hahaha. Once the insomnia resolved, my cognitive faculties improved a lot but left me still not feeling like myself.
Fast forward another 3 or so years, and I decided to stop eating processed sugar (200+ grams daily of milk chocolate confectionery) and resumed exercising 5-6 days per week (I’d had a year or so off from exercise and had gained quite a few kg’s). About 4 months in to the sugar-free high exercise regime, I started getting what I now know where the first signs of ME/CFS – during one week at work I could feel my energy switch off earlier each day as the week progressed (4.30pm on the Monday, down to 9.30am on the Friday). After about a week it stayed switched off and didn’t come back on until six months later. At that time and due to desperation, I gave up my exercise regime and within 2 days feel amazing (well, I felt normal but comparatively speaking, it was amazing to not feel mentally and emotionally flat 24/7). About 18 months later I exercising again but only 2-3 days a week and much less intense than I’d ever done before and this is when I started getting PEM.
I’ve long suspected either the dropping of processed sugar, or swimming in chlorinated pools may have contributed. Seems like the OTS studies might support it being the removal of calories but decreasing sugar intake. I have to say though, although I dropped about 17kg in 9 months, I still ate alot of food and didn’t feel as though I was starving myself or anything.
Anyway, testimonial aside, does anyone know where we can find info that might assist with selection of possible treatments (based on potential case of OTS?).
ManShadow, processed Sugar contains Alpha-Gal sugar protein from the Bone Char processing on the factory machines. Have you been tested for the Alpha-Gal Meat
Allergy component blood test? Also, an Allergist for skin testing for beef, pork, lamb, dairy, even processed sugar. There is a Group on Facebook called ‘SAAT Alpha-Gal Remission’
Heh, I’ve been asking people for the last 12 years to look into OTS for insights on how CFS switches on/off. OTS is reclassified as CFS if it last most than 6 months, so extreme OTS *is* CFS. Likewise for PVFS. The thing about OTS is that it can be rather reliably reproduced: just take an athlete who suffered OTS before, subject him/her to the same amount of training. (In my case it was training 2 days in a row). I know, that would be unethical on humans.. But they could try that on athletic mice.
I couldn’t make head and tail out of the conclusions they reached from what they did, so I dug up the entire article. An immediate problem popped up. Their definition of OTS includes functional overreaching, the most mild form of overreaching. OTS as I understand is an extreme nonfunctional overreaching that resembles CFS. So, when they say multiple causes for OTS, they mean multiple causes to underperformance by 10% or more. CFS is more like underperformance by more than 80%. (My OTS used to be underperformance by 100%). I consider myself a mild patient and I still can’t do 30% of what I used to be able to. In non-aerobics, it’s more like less than 10%.
The entire article is here: https://bmjopensem.bmj.com/content/5/1/e000542
If we all look back at the Metabolic Trap, he asked was there something you were taking in supplements that stands out that could have triggered your Metabolic trap, I believe the answers lies in Yes Mammals, Gelatin, Magnesium Stearate, Mammal
ingredients, cross contaminations even aerosols, house cleaners, dish soap, laundry detergents, toothpaste, countless items buying products that have these hidden ingredients. We do not always get full blown anaphylaxis we sit on the borderline &
people who do the blood test think that is all that is needed it is not, they need the skin Patch Allergy test done including each items on skin beef pork lamb & all dairy even sugar has alpha gal so if one think Honey is safe it likely has sugar
added…People countless say I reacted bad to the MRI Contrast, does it contain animal products? I almost Died in Emergency from Morphine it likely has Alpha Gal inside. Does Ampligen have animal ingredients? The lady who recently used the MS
drug for he ME/CFS did that drug have Alpha Gal inside? It is likely her Allergic reaction was to the drug with AG inside. Has she blood test for AG has she had proper skin tests for AG?
La recherche sur le cfs manque de méthode : pas de test systématique de métaux lourds ni de taux de perturbateurs endocriniens ni de la maladie de Lyme. Pas non plus d’étude sur l’histoire passée de chacun et l’accumulation de stress psychologique et physiologique pendant de nombreuses années. Pas non plus de recherche sur des modifications génétiques et épi génétiques.
Thanks Cort!
In the months after my ME/CFS trigger (viral infection), I remember the burning joint pain I experienced whenever I tried to jog or play golf. There were only two thing to which I could compare it. One was growing pains and the other was a unique sensation I felt on a few occasions after weight training too hard.
The latter happened years prior and I don’t think it played a major role in my ME. (Though caffeine-related insomnia and overstudy certainly did!) But for me the symptom overlap was always undeniable and potentially validates the point of your article.
So interesting to read this. Before ME/CFS (6 and a half years ago) I was very fit and active, and a qualified Fitness Instructor / Personal Trainer. I have often if I over trained. However, I did have a viral infection which led to the onset of ME/CFS so I guess it’s difficult to be sure. Especially with both conditions having such similar symptoms. This is certainly very thought provoking. Thanks for writing.
There is a USA Doctor who has a diagnostic test procedure & treatments for Gut issues he first rules out all Bowel possibilities even Celiac disease is ruled out, he then moves on to doing his procedure, he uses his Name he calls the condition ‘Habba
Syndrome’. There is a Video on YouTube on the television series ‘Mystery Diagnosis’ Channel, it deals with IBS type issues going too much or constipation there is bile leakage in the Gut seen on his test procedure. The Woman diagnosed at times had
trouble controlling her bowels with urgencies that just came out of nowhere. He has a treatment. The Comment section also talks about different medicine brands with same ingredients. Their lives were immediately changed & very positive comments there of success…He also has Published his work..Not many Doctors know of Habba Syndrome I sent the Video to Dr. Ron Davis’ Team
“reduced testosterone levels (possibly causing reduced muscle mass).
increased estradiol levels without a concurrent increase in testosterone (reduced testosterone-to-estradiol ratio) (possibly caused by metabolic abnormalities; body composition changes found).”
No one even mentioned this…….significant in both groups of people. Can apply to ratios between the two…..testosterone and estradiol. One may be normal levels…..but if one is low — the balance is off.
And there was a comment about eating disorders and anorexia. My sis had anorexia and was a chronic exerciser. She was severe and very critical when we finally found help for her eating disorder. The cure was anabolic steroid injections — testosterone. 5 shots and she started eating. They are used with POW when starved in camps. We don’t know if there was other things in it or not. But she does have CFS, she is still alive due to these shots.
See YouTube Video Mystery Diagnosis and Diarrhea-Habba Syndrome named after respected Gastroenterologist Dr. Habba…Habba Syndrome is still not yet an accepted
diagnosis but there are diagnostic tests & they also have treatments taken before meals…Read all of the Comments they are very Positive ones, it may not be IBS it may
be Habba all along
Recovery from over training and ME/CFS is similar. The nervous systems is engaged chronically until it breaks down. Restoration is well known by those of who built a recovery. Murry Balantine was known as the worst case of overtraining requiring 4 years to recover.
All of the science is to document the body in the freeze response and what that looks like metabolically.
Ron Davis has no emotional awareness of himself or other people to any real degree. You want an interesting study? Study his level of emotional mirroring……
Hi Cort, thanks for touching again in the similarities between ME and OTS.
To my surprise, the author is doing his research in a very good medical school in São Paulo, Brazil.
I´ve got in touch with him and we are going to talk by phone and probably I´ll schedule a visit to meet him personally; my hometown is 60 km away from São Paulo.
I´ll get back to you as soon as i have more news.
I don’t know if this was part of the study, I just came across it and thought I would share. [ My note: Overtraining for some is at an athletic level, and overtraining for some of us is just getting through the day and crashing. At either level, the result is cognitive dysfunction.] https://www.sciencedaily.com/releases/2019/09/190926141738.htm
Here is the original: “Neuro-computational Impact of Physical Training Overload on Economic Decision-Making” https://www.cell.com/current-biology/fulltext/S0960-9822(19)31104-2
I made an attempt to link athletes, reduced intake of carbs and proteins, eight hours of studying, training and over training syndrome. I posted it elsewhere to save me from writing it multiple times.
It can be read in https://www.healthrising.org/forums/threads/potential-linking-fm-mast-cells-sleep-deprivation-food-intolerance-exercise-intolerance-and-me.6217/ in comments 11 and 12. I did my best to make it relatively easy to read and understand.
Different illnesses can have similar symptoms. Obviously this doesn’t mean they are the same disease. OTS always has a recovery path and it is usually within months. If it takes someone years, that is still a recovery path. The recommendation for OTS is a decrease in the intensity of training and training less frequently. TRAINING. This is more than just exercise which we can’t do. Even when I was mild I was having a terrible time doing light exercise.
I think the different bio-markers would be revealed in a Tilt Table Test (I had low BP and in 2003 when I fainted the data revealed orthostatic intolerance, the recommendation was Florinef).
I would bet they won’t have the same NKC, cytokine, Leptin, and even metabolic results compared to a ME/CFS patient.
I was a type A overachiever, pushing myself to the max at everything I did. I exercised hard 5- days a week. I ended up going back to college and studying 8- hours a day and dropped out of weights and jogging. I also had a bulging L4-L5 disc and my Doc decided to give me a series of epidural steroid injections. I was also under a lot of stress. Sound like a perfect storm? Well it was. I’ve had CFS for 30 years now and just try to manage the symptoms. Post exercise malaise is getting overwhelming as I’m getting older. Luckily I’m highly functioning, as you cannot keep an extremely motivated person down. I try to eat exceptionally, exercise moderately, sleep as good as possible, and I try to live as stress free as possible. I’ve given up hope on doctors being of any assistance. I gave up pharmaceuticals within a few years of acquiring CFS, they only make your health worse, and I’ve tried everything plus some. I take a lot of supplements, most of which are discussed extensively on this site. I wish that I could tell you that I have found the magic bullet in my 30 year search, but sadly, I have not found anything that helps other than taking extremely good care of yourself. Food allergies were the only thing I discovered that made an appreciable impact. Good luck to all and pray for a cure.
Thanks for that Curt. I think you speak for many of us!
This was a really interesting post – thank you so much. I had heard of OTS in passing previously, but I didn’t know anything about it in depth. In my case, I had a viral infection in 1995, after which I had very baseline symptoms of ME, but they were so low, I didn’t recognize them or think that I was “ill.” Then, in 2001, I started martial arts, and gradually increased my intensity of training until I was training up to five nights a week. In the summer of 2006, I did an Olympic-level boot camp, and two months and two black belts later, I had a major crash; my health went completely downhill, and I’ve never recovered. In 2009, after I did a lot research to find out what was wrong with me, and doctor’s tests all coming back as normal, I came to the conclusion that I had ME/CFS. Looking at your information on OTS, I can see that I had sleep problems, and a low protein and low carb diet leading up to that major crash. So, I think in my case, I had an initial viral trigger that led to a compromise of my system a la ME/CFS, and I didn’t recognize that I was pushing my body too hard when exercising, and that OTS was the final push to breaking point.
Interesting…Thanks for relaying that 🙂
I’ve been suffering from chronic fatigue and overall malice for over a year. I recently found out that I get much better when I stop exercising intensely (even if low in volume, intense exercise seems to worsen the symptoms).
It first started as episodes of sudden crashes (like a sudden flu but with no fever) from which it would take me a couple of weeks to recover and then evolved into a more constant and persistent state of fatigue.
Normal tests didn’t reveal any abnormalities (just like the article says) and my doctor suggested mental stress, though I knew it couldn’t be just that. Removing exercise from the equation confirmed my suspicions.
On bad days I noticed my heart rate would remain constantly higher, even at rest (10 to 20 beats higher than usual, sometimes more).
I’ve always been very fit and athletic, combining both strength and cardio with a “no pain, no gain” approach.
I will see a sports specialist in one month to see if they can shed some light on this, it is extremely frustrating and affecting my whole life, not just exercise.
Thanks for sharing your story Santiago. I encourage you to keep an eye glued to this website (subscribe to the newsletter) and to ME/CFS doings in particular. Be careful with exercise. We have a whole section on how to exercise with ME/CFS in the resources section of this website.
Good luck!
Hi mate, it’s me again. 2 years later and still struggling to recover and starting to wonder whether the damage is permanent.
I was diagnosed with OTS on November 2020 (in what the doctor called “on of the most typical OTS cases” he had diagnosed).
After that, I stopped all activity (except easy walks) for 7 months and made great improvements. Assuming the worst was behind me and it would only get better from that point on, I got back to activity and joined a football team. Long story short, I had a relapse a few months later from which I’ve been recovering since.
Again, I’ve made great progress and this time I really did ease back into exercise, taking it very slowly and adding volume and intensity gradually. Also, I took 5 months off work.
However, this last month has been a harsh reality check. I got back to work and one month into it I had to quit. It wasn’t that the job itself was that stressful, but it seems my body is so fragile that it cannot handle 40 hours of work a week. My HRV, which was at very good levels prior to work, has dropped significantly and it doesn’t seem to recover.
I’ve done everything I could and more, still, I am struggling: I don’t drink alcohol, I eat very well, I make good sleep my top priority, I keep my coffee down to 100mg a day, I check my HRV daily, I’ve been handling exercise very carefully.
I am desperate, I don’t know what else to do. I want to see another doctor but I don’t even know where to start from, what kind of specialist I should see. Do you have any suggestions?
Hi Cort I have seen your comments all over my month of intensive research. I have had the most stressful life. I moved three times in the last 10 years. I am 67. I became disabled when I was 57. I am a surfer who moved to Hawaii age 60. I surfed every chance I got but was burdened by my autistic son being a single mom losing my teaching license to a pot bust. I also took care of my narcissistic mother who complained every day for the 5 years I cared for her. I also worked on dropping weight I am 135 lbs now but was 150 my whole life. I surfed as if each day would be my last. Here in Hawaii you can surf almost every day. Then last month I suffered the worst crash and finally accepted that my brain fog was from exercise. I have rested 1 month but am still too tired. My pain doc and my primary doc both said get back in the water. I have a headache every day. I got diagnosed with sleep apnea at age 65 2 years ago. I am still tired but even more if I take off the sleep mask. My primary did not believe me at first. I look great. I feel like death. I also have fungus on my nails hands and feet. And I have a bad case of hsv2. Now my primary will give me Lyme test and other tests to see what is wrong. My sleep center is referring me to their doc. I feel like I must help these doctors but egos get in the way of ignorance. Thank you for your studying on this topic. I have learned much from you.