The first large study examines spinal issues in chronic fatigue syndrome (ME/CFS).
A couple of years ago, there was hardly any discussion of spinal issues in ME/CFS. It’s become clear, though, that spinal issues are present in some patients and can even, in some instances, produce virtually all the symptoms found in this disease. From cerebral spinal fluid leaks, to spinal stenosis, to intracranial hypertension, to craniocervical instability, the spine is now of intense interest.
Now comes the first large study – from Sweden – to assess spinal issues in ME/CFS.
The Study
Signs of Intracranial Hypertension, Hypermobility and Craniocervical Obstructions in patients with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Björn Bragée1,3*, Anastasios Michos3, Brandon Drum1,3, Mikael Fahlgren2,3, Robert Szulkin3, Bo C Bertilson1,2,3*
This study was notable for a couple of things. For one, it appears that Sweden is moving rapidly on

Something is happening in Stockholm – it now has two ME/CFS clinics. Bjorn Bragee – creator of the ME/CFS Bragee Clinic in Stockholm
ME/CFS. Not only has a large collaborative effort formed around the Open Medicine Foundation’s Uppsala Collaborative ME/CFS Research Center, but a newly formed – apparently quite busy – ME/CFS clinic (Bragee Clinic) has shown up in Stockholm. (That makes two ME/CFS clinics in Stockholm, now.)
Bjorn Bragee, the creator of the clinic, talked about it:
“We need quality research and a better understanding available in public health care regarding this diagnosis. At our clinic we will be working from a biomedical perspective and staying updated on new available treatments. So far, there is no treatment that works for everyone. “Many are bedridden at home and their quality of life is alarmingly low.”
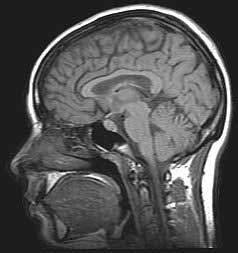
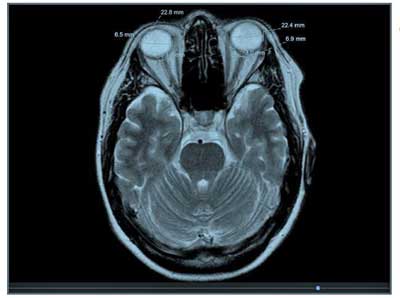
Created in 2017, the clinic worked quickly to gather what may be the largest array of MRIs collected for ME/CFS. These 200- plus MRIs were used to produce easily the biggest assessment of spinal issues in ME/CFS. The group used the MRIs and a clinical examination to assess intracranial hypertension, joint hypermobility, Ehlers Danlos Syndrome, various conditions that can obstruct spinal fluid flows, spinal issues and craniocervical instability.
Nobody expected Sweden or anywhere else to so quickly focus on spinal issues but Bragee jumped on this issue quickly, and here we are with a quite large ME/CFS spinal study.
The Conditions Assessed
Joint hypermobility – When the joints become too flexible, they can produce pain and stiffness, clicking joints, easily dislocatable joints, recurring muscle/joint injuries, constipation and irritable bowel syndrome (IBS), fatigue, dizziness and fainting, thin or stretchy skin.
Intracranial hypertension occurs when high cerebral spinal fluid pressure is present. Its symptoms are similar to those produced by a brain tumor and include frequent headaches, blurry or double vision, poor peripheral vision, dizziness, nausea and/or vomiting, stiff neck, gait and coordination problems, tinnitus (ringing in the ears), forgetfulness and depression.
Ehlers Danlos Syndrome refers to a highly heterogenous groups of connective tissue disorders characterized by hypermobile joints, a high degree of skin extensibility, and fragile tissues. Thirteen subtypes are believed to exist including classic, hypermobile and vascular EDS.
-
-
- Classic EDS is characterized by symptoms such as loose joints, elastic, velvety and fragile skin, easy bruising, extra skin folds over the eyes, muscle pain and fatigue and heart valve problems.
- Hypermobile EDS is characterized by loose joints, easy bruising, muscle pain and fatigue, early onset arthritis, degenerative joint disease, heart valve problems and chronic pain.
- Vascular EDS is characterized by thin, transparent looking skin, fragile blood vessels, thin nose and lips, sunken cheeks and small chin, protruding eyes, collapsed lungs and heart valve problems.
-
Craniocervical Instability refers to a condition where lax ligaments which hold the head up over the body allow the brain to impinge upon the brainstem, spinal cord or nerve roots. Symptoms can be diverse but generally include headache, neck pain, numbness, heavy feeling head, “bobble-head”, dizziness, vertigo, gait and coordination problems, muscle weakness, problems with sleep and visual disturbances. Jeff, Jen Brea and others diagnosed with ME/CFS were found to have CCI. Jeff and Jen Brea made full recoveries from severe cases of ME/CFS after surgery.
Chiari malformation occurs when the cerebellum dips down into the spinal column cutting impeding spinal fluid flows. Its associated pain (especially headaches aggravated by coughing/straining), weakness – especially in the hands, neck, and arm – and leg pain, numbness, temperature insensitivity, unsteadiness, double vision, slurred speech, trouble swallowing, vomiting and tinnitus (ringing in the ears).
Downside
A major downside to this study concerns its mode of publication. Instead of being published in a peer-reviewed medical journal, it was published on a non-peer reviewed “open access site“. That will greatly limit access to the study and blunt its impact.
The authors didn’t say how they determined severity but reported that the study examined a severely ill patient group.
Criteria
- The group used the 2017 International Classification of the Ehlers-Danlos Syndromes to assess the incidence of Ehlers-Danlos Syndrome.
- The Beighton Score (> or = to 4) was used to assess the degree of hypermobility. (The Beighton score, it should be noted, does not assess all types of hypermobility.) While hypermobility is associated with EDS, most people who are hypermobile do not have EDS.
- Interestingly, the group bypassed the new criteria for FM and used the 1990 criteria.
Assessments of Intracranial Hypertension (IH)
The authors used well-established non-invasive means of assessing IH including:
- The Eyeball Transverse Diameter (ETD)
- The Optic Nerve Sheath Diameter (ONSD) – CSF fluid percolates through the nerve sheath that wraps the optic nerve. Normal ONSD = 4.8-5.8; >5.8 believed to correspond with elevated CSF pressure (>25 mm Hg)
- ONSD/ETD – normal = 0.19+/- 0.02; > 0.25 = IH with severe symptoms
Spinal issues that could disrupt spinal fluid flow
The group also looked for structural problems which could result in reduced spinal fluid flows and IH. They included:
- Lowered foramen magnum – The foramen magnum is a large hole at the base of the skull through which several arteries, membranes and ligaments and a nerve passes.
- Lowered position of cerebellar tonsils – the bottom half of the cerebellum can dip down into the upper spinal canal – cutting off spinal fluid flows. In more severe cases, this is called Chiari malformation.
Craniocervical Instability
The authors used something called the clivo-axial angle (CXA) to assess craniocervical instability (CCI). Experts agreed in the 2013 Consensus Statement on Craniocervical Instability that four tests can be used to assess craniocervical instability. The Consensus states that a clivo-axial angle (CXA) 135º or less is possibly pathological, and that, in some circumstances, stress the brainstem and spinal cord. It is not a definitive test of CCI, but indicates that further investigation is warranted.
Cervical Spine MRIs
In the cervical spine MRIs, the researchers assessed a number of factors which could impact spinal cord functioning including:
- spondylolisthesis (forward or backward slippage of the vertebrae)
- osteophytes (boney projections that can impede nerves)
- spinal cyst(s) or syringomyelia
- bulging or herniated discs.
Results
An astonishing 96% of patients fulfilled the criteria for fibromyalgia. That number is quite high and may reflect the more severely ill group of ME/CFS patients the authors stated made up the study. A 1000 person ME/CFS Spain study found that 54% had fibromyalgia.
The Swedes found joint hypermobility (Beighton score >4) in a remarkable 49% of ME/CFS patients. Most of those (41% of total) fulfilled the hypermobility criteria (Beighton score >5) for hypermobile Ehlers Danlos Syndrome (hEDS). Twenty percent of ME/CFS patients met the full criteria for EDS (including hyper-elastic, extensible skin/fragile tissues).
Only a few studies have assessed hypermobility in ME/CFS. The 2002 Barron/Rowe study found that no less than 60% of children with ME/CFS had a Beighton score indicative of hypermobility. Four years later, Nijs et. Al. found 22% of the 69 ME/CFS patients had a Beighton score >4.
Similar findings have shown up in fibromyalgia. A large (150 person +) study, though, found joint hypermobility in 64% of FM women. A 236 person study found joint hypermobility in 46% of FM women.
Why the focus on joint hypermobility? Because connective tissue and lax ligament problems also underlie many of the spinal problems the authors looked at. Lax ligaments, for instance, are responsible for craniocervical instability. Connective tissue problems can contribute to a lowered cerebellum, foramen magnum, as well. (EDS is not the only “lax ligament disorder. Others include: Loeys Dietz Syndome, Stickler Syndrome, Marfan Syndrome, Cleidocranial Dysostosis, Morquio Syndrome, Down syndrome, etc..)
While more studies are needed, hypermobility and therefore connective tissue problems appear to be common in ME/CFS. We will surely learn more about the incidence of hypermobility and EDS incidence from the CDC’s multisite study.
- Take the Beighton Test – note, though, that the Beighton test does not assess hypermobility in all parts of the body
Intracranial Hypertension
Signs of intracranial hypertension (IH) were common with 55% having high ODNS ( >5.8 mm) and 83% having an ODNS/EDS ratio of greater than .25. The author reported that an ODNS/EDS ratio >.25 was associated with IH with severe symptoms.
Drooping Cerebrellar Tonsils – Fifty-six percent of patients (as opposed to a general population prevalence of 25%) had evidence of drooping cerebrellar tonsils which could be obstructing spinal fluid flows. Seventeen percent had evidence of the more severe Chiari malformation.
The authors reported that only a fraction (11%) of the patients had what is considered a normal position of the cerebellar tonsils.
Spinal Issues
Spondylolisthesis and osteophytes were found in 6 and 9% of patients. These findings appear to be similar to those found in the population at large. Spinal cysts or syrinxes were not found.
The authors did not break out bulging discs from herniated discs. Bulging discs are quite common and often do not cause problems. Herniated discs on the other hand are rare and almost always cause problems. The authors reported that eighty percent of the patients had one or more obstructions in the cervical spine. More than one vertebral segment from the neck to the lumbar region was obstructed in 64% of participants.
Craniocervical Instability
A Clivo-axial angle (CXA) angle of less than 150 degrees was found in 114 of the patients (56%). Normal CXAs are reported to range from 150-170 degrees. Henderson reported that “the CXA has a normal range of 145° to 160° in the neutral position”. One study reported a mean CXA 148° for the healthy controls – which was identical to that found in this study.
While Van Gilder (somewhere – I couldn’t find the citation) reported that a CXA of less than 150° was associated with neurological changes, most authors and the CCI Consensus Statement report that only a much smaller CXA angle (135 degrees) is considered possibly “pathological” and indicative of craniocervical instability (CCI). The authors of this paper did not report how many patients met the more restrictive criteria.
Conclusions

High cerebral spinal fluid pressure – the main finding in this study – can produce many symptoms associated with ME/CFS.
A very high incidence of fibromyalgia comorbidity and the almost 50% incidence of hypermobility suggested that this patient population was indeed severely ill. The incidence of Ehlers Danlos Syndrome (EDS) appeared to be quite high (20%) as well.
The Gist
- A large spinal study involving over 200 MRIs found:
- High rates of fibromyalgia (96%), joint hypermobility (49%) and Ehlers Danlos Syndrome (EDS) (20%) in ME/CFS
- High rates of increased spinal fluid pressure (intracranial hypertension) (55-80?) – a condition which can produce many symptoms associated with ME/CFS
- Apparently normal rates of spondylolisthesis, osteophytes and spinal cysts
- Possibly high rates of bulging or herniated discs (which could interfer with spinal flows)
- Most normal clivo-axial angles – suggesting that cranialcervical instability may not be common in ME/CFS
- The fact that the study was not published in a medical journal severely limits its impact.
It was not easy to assess the incidence of spinal issues but they appeared in line with those found in the general population. Eighty percent of the participants tested, however, had either bulging or herniated discs.
Craniocervical instability (CCI) was assessed by Clivo-axial angle. Most sources suggest that the mean CXA in ME/CFS (148 degrees), was low normal or borderline (normal = 150-170 degrees). (CXAs of 135 degrees or less are likely pathological and may be indicative of CCI). Because the authors only provided a mean for the group, it’s not clear how many patients had lowered CXAs, but some clearly did. As a whole, though, the group’s CXA – and therefore, one would assume the rate of CCI – did not appear strikingly abnormal.
The big news was the very high rates of intracranial hypertension found. Depending on which measure was being assessed, estimates ranged from a whopping 55% to over 80% of the group. Plus, the study suggested that a strikingly high percentage of patients (17%) relative to the general population (<1%) may have Chiari malformation.
It seems the more ME/CFS is studied, the more possibilities turn up. Since IH can produce or contribute many symptoms found in ME/CFS, this study, while unpublished, will hopefully incentivize others to assess spinal issues in ME/CFS. Hopefully, the CDC’s multi-site study will shed more light on the spine. Avindra Nath is also assessing spinal issues in the intramural study.
Unfortunately, the study was not published in a peer-reviewed scientific journal and therefore will not get much traction in the medical community. Doctors will need studies published in medical journals to begin to assess and diagnose spinal issues present in ME/CFS. Hopefully, the CDC’s multisite study will address these issues.
Check out a deeper dive in intracranial hypertension
Health Rising Drive Update
Pressure is building. Thanks to the 182 people contributing to our drive we’re almost 50% of the way to our goal.
Ask yourself where you get the kind of detailed analyses that you find on Health Rising and then please consider supporting HR.
Health Rising is not a hobby site. It’s the only source of support for its one full time employee (me) and it pays for a part-time employee (Stavya). HR doesn’t need much – our needs and its expenses are quite modest – but we do need to keep the lights on.
Please consider supporting HR in a manner that works for you.







Thanks for continuing to provide an overview and The Gist Cort! Even on days when I can read a bit more, reading The Gist first helps with my comprehension.
Very grateful for everything you do to keep our community informed!
I’m continuing my small monthly donation for 2020.
Happy holidays
Thanks Birdie!
Happy Holidays to you!
Is there anything our disorders are NOT associated with…dental overbite, receding hairline, low sperm count, high BMi, etc., etc., …The wastebasket of symptoms still with unknown cause. They need to sic AI on FM and ME to look for causation, not just association and sequelae.
Steve, probably not! lol
very interesting. I have moderate to severe spinal stenosis, type 3 ehlers danlos, fibro and me/cfs….and a lot of other extras that come with me/cfs and fibro….I think maybe alot of us have spine issues and connective tissue disorders…hmmm
I believe that Ron Davis may have found a connective tissue link in the severe ME/CFS study. I think its going to be a key feature of a substantial subset of patients. Fascinating stuff…
I wouldn’t say that publishing on an open access site will limit access to the paper, quite the opposite, it makes it available to anyone. But I understand what you’re saying it will limit the number of medical professionals who see the paper, and therefore it’s impact. Maybe you could inquire as to why they took this route? Perhaps they are planning on publishing it later but wanted to get out there now?
Yes – it’s the medical professionals. It’s also possible to publish in medical journals that provide free access such as PLOS.
I’m hoping they will get it out to a medical journal. My first guess is that these are doctors who published it and they’re not used to publishing in scientific journals – but I don’t know.
I developed severe intracranial pressure approximately one year.AFTER my inaugural “classic influenza” from which I never recovered (hello CFS/ME!) I medicate for it daily, and have an eye exam yearly to deck the margins of the blind spot I developed from exploded eye capillaries (wrong word.) it IS critical to get on with cause and effect or the etiology.
How did you find out you has severe intracranial pressure? Was it from eye problems?
Sorry to hear you have it Barbara, but “I medicate for it daily, and have an eye exam yearly to deck the margins of the blind spot I developed from exploded eye capillaries (wrong word.)” tells so much and does it better then I can:
When an astronaut would do a space walk without protective pressure suit it is said he would “explode” due to the pressure of the blood not being compensated by the surrounding air pressure we have on earth. It’s in fact a slight exaggeration, but the astronaut would die very soon even if provided with an oxygen mask.
I think you can get the picture: too high blood pressure without enough countering surrounding/environmental pressure and the blood vessels start to leak, tear or “explode”.
In the brain, the surrounding pressure is largely provided by the cerebral spinal liquid. If that is increased, chances are it tries to counteract a risk of the brain blood vessels (capillaries) from massive tearing.
What other indications do we have?
* Blood volumes in ME/FM/… are strongly reduced. They are reduced up to the point that a double digit percentage of people with severe blood loss due to severe hemorrhage up to the level of having as few blood as we have on average die within 24 hours.
Reducing blood volumes also happen to be one of the better ways to reduce chances of hemorrhage a lot. There is less blood pressure and far less blood in the capillaries due to it. The capillaries are very likely the most weakened blood vessels in ME/FM/… I believe.
* We likely have massive ROS and inflammation. Both weaken human tissue including capillaries a huge lot.
* We likely have very narrow capillaries. I showed the formula somewhere else, but there are few things better to strengthen a pipe then making it simultaneously smaller in diameter but also let it have a thicker pipe wall.
Contracting the blood vessels clearly makes the diameter smaller. But the cells become squeezed in that process. That makes not only the diameter smaller but also the wall thicker.
Using the same mass of material to construct a pipe with smaller diameter but thicker pipe wall has a !quadratic! effect on strength so contracting the blood vessel diameters strengthens the blood vessels a whole lot.
As a side effect, it closes any potential ruptures and wholes in the blood vessels. Think about having a deep cut. Pulling it open (compare it with dilating the blood vessels) expands the tear a whole lot and increase bleeding a lot. Compressing it on the other hand prevents further tearing the wound open and closes the wound, decreasing blood loss a lot.
* We are said to have inflexible RBC. Those by itself locally push open the smallest capillaries as round RBC have a bigger diameter then the capillaries themselves. This constant pushing (and relaxing like a small snake swallowing several too big round pieces of meat) helps tearing open the smallest capillaries, making them more prone to rupture and opening tears increasing chances for blood loss.
Now I’d love to see this study plus a low grade inflammation study and see how increased CBF pressure correlates (patient per patient versus healthy controls) with increase in low grade inflammation in the brain (and disease seriousness). I’d think we’d have a cheap and reliable brain inflammation diagnostic tool here.
The brain inflammation is an interesting idea for me because the skull limits the amount of inflammation that can occur without problems.
I would have thought any inflammation would cause some swelling and that could cause a build up of pressure within the skull, resulting in all sorts of issues…
just read an article in a magazine that when astronauts return on earth they have an enhanced intracranial pressure, that does not go away.
I wonder if they develop FM/ME symptoms?
They certainly experience fatigue and orthostatic intolerance.
Very interesting, ChrisB
“they have an enhanced intracranial pressure, that does not go away.”
Would you happen to have a link to that?
That is very much in line with the whole idea explained above:
Do to lack of gravity in space (the air is pressurized in the space station), blood has more trouble returning to the heart. Blood having more trouble returning to the heart is the whole basis of my idea to need more CBF pressure in order to limit edema and enable sufficient blood return in the skull / brain. That sort of confirms this hypothesis is quite plausible.
Also interesting, when they are back on earth it doesn’t goes away. So it sort of has memory, like with ME/FM…
It’s sort of a prolonged hit-and-run due to having been in space. We may have found part of the vicious circle here. Maybe the increased CBF pressure creates inflammation of its own helping it got locked in?
Mmay i ask what are you medicating with on a daily basis for this…?
May i ask what medications you are using for this barbara?
This is an excellent explanation, Cort. Thanks much!
Thanks!
Is there anything published in medical journals to the protruding disc issues in the neck?
I read the HR blog on Dr Rowe’s 3 patient case studies, but is there any more studies on that?
I had an MRI and disc protrusion was found narrowing the spinal cord to 9.7mm & 7.9mm. However the neurosurgeon said there was still spinal fluid around the cord. (Although it looked gone to me)
But the neurosurgeon said he would operate only if he gets a second opinion from a neurologist who he said will be more sceptical. He said he’ll want more reputable information than just the 3 patient case studies. So if anyone has links or even a contact neurosurgeon or neurologist who knows more about it, I’d be thankful for your help.
Either post details below my comment or email me at
vespa.bw@gmail.com
Thank you
Does spinal stenosis count? It’s narrowing of the spinal canal. Dr. Rowe found that correcting it returned some patients to health or helped them significantly. Check out this blog
https://www.healthrising.org/blog/2019/05/29/spinal-stenosis-chronic-fatigue-fibromyalgia/
Wow, I had back pain for many years and was never tested via MRIs until I saw a neurologist who immediately diagnosed me with degenerative disc disease. I’d been diagnosed with CFS by Dr. Lapp a few years before. But I’d had all the symptoms plus pain for many years prior to the diagnoses. I had 2 surgeries within one year. It stopped the pain for about 10 years, however. Now I’m too old to undergo that type of surgery. But with specialized chiropractic care, the pain is kept at a lower level.
Imagine what could be learned if there was money spent on research instead of paying for elections.
Never assume that everything we associate with FM and ME/CFS is actually caused by it. Thanks for passing that on.
I took part in the study and had never connected a head trauma from almost 30 years to my gradually worsening health, accelerating over the past five years to being almost completely bed bound and diagnosed with ME. Upon hearing at the clinic that head trauma had a significant correlation I investigated things further. Upright MRI gave clues but nothing fully conclusive. Followed up by thorough neurological exam, review of entire health history, all the failed treatments etc and being dismissed by neurosurgeon at home I contacted the Chiari and Hypermobility clinic in Barcelona for second opinion. Now a clear cut diagnoses of CCI and AAI along with misalignment of the atlas over the axis both in neurtal position and rotation. Slated for fusion surgery in March (C0-C2). First light in a very very long and dark tunnel. I wouldn’t be surprised if the next breaktrough, by Younger or VanElzakker will be connecting this to neuroinflammation in many parts of the brain, including the brainstem and vagus nerve.
A long road for you Joakim. I acknowledge your for your persistence in the face of no agreement and wish you the best with the March surgery. I also want to thank Joakim for making me aware of this study. 🙂
I did have a mild head trauma (concussion) when I was a teenager. That was one of the differences between myself and my identical twin who does not have ME/CFS.
Cort, one of the issues is that the head injuries can seem trivial at the time. I had whiplash in 1987, followed shortly after by a manic episode, and another one later in the same year, but had no further issues for about 20 years (then I had mixed symptoms of ADHD, bipolar episodes, eventually resolving into fatigue and episodes of sweating, with back and neck pain- both preventing me from working.
So a few things have come up- the approach of the neurosurgeons in just lumping all these symptoms into the “neuropsychiatric” basket is probably more helpful- it draws away from our prejudices related to individual conditions. Secondly there are quite a few studies of value. The book Craniocervical syndrome and MRI covers many of them.
However I would highlight:
A case-control study of cerebellar tonsillar ectopia (Chiari) and head/neck trauma (whiplash)
MICHAEL D. FREEMAN1,2, SCOTT ROSA3, DAVID HARSHFIELD3,
FRANCIS SMITH4, ROBERT BENNETT5, CHRISTOPHER J. CENTENO6, EZRIEL KORNEL7, AKE NYSTROM8, DAN HEFFEZ9, & SEAN S. KOHLES1
Brain Injury 2010
The research being done is quite diverse, so some will emphasise CSF pressure, and others will be directed more toward CSF flow.
Great summary thanks. Cort, I just want to say thank you for your tireless work in making this information accessible to everyone. Your reach is huge and valued all around the world. It is a wonderful thing that you are doing. Much respect!
I hope you have a restful Christmas.
Kindest regards
Rose (New Zealand)
I fell from quite a height when I was about two. Was unconscious in the kitchen table for three hours, with my mother laying her hands on me.
I fell off my bike, no helmet, and was concussed, when I was about six. Then as a teenager, I fell backwards onto concrete, as the rollerskates I was on shot forwards.
I also fell off lots of ponies/horses.
I had an x-ray of my neck area, when I was about twenty, as my neck was sore. It showed the bones in my neck had fused together.
I’m an EDS girl most definitely. At 67 I can still wrap my legs behind my head and if it weren’t for my abnormal elbow joints, could have a perfect Beighton Score.
Having spent thousands of hours reading all the EDS forums, I can say that autonomic dysfunction can mimmic many of the symptoms of CCI and more–so often it can be difficult to parse out exactly what is contributing to the problem.
It’s my opinion that spondylolisthesis (unstable vertebrae) is what is causing a huge share of spinal issues in people with any kind of hyper mobility. It contributes to the formation of cysts, disc problems, compression, and stenosis.
Given that I have all of the above, there have been times when I have contemplated, as Cort mentioned in his link about spinal stenosis, ‘correction’ of the problem. A few observations about ‘correction’: correction usually means fusion of the vertebrae with ‘hardware.’ It is a very serious surgery. People with EDS often do not heal well and I have read that there is close to a 50% ‘failure’ rate (does not improve or reverts or some other complication). The surgery could make things worse.
Also, when one area is fused, the joints above and below often eventually fail from the additional strain put upon them. I have read about many EDSers who have, bit by bit, had their entire spine surgically fused. Fusion like that means a person loses the ability to flex and bend their spine. Also healing from fusions is a long, long process with many restrictions.
Now, as difficult and time consuming (especially for someone with ME/CFS) can be, I urge anybody who thinks they can solve their problem by spinal ‘correction’ to first try physical therapy–I mean REALLY try it–for months if necessary. And you need to find a very good P.T. Of course if the problem is ‘something else,’ then listen to your surgeon…but please ‘do your homework!’
Since EDS is genetic, and ME/CFS usually has a beginning point sometime in a person’s life, I’m suspicious that EDS spinal problems (or similar) is a cause–a contributor maybe, but not a cause. It’s just my opinion…
On a personal note, the results of my full thyroid testing are beginning to come in and although most everything is within range, my antibodies are not! Also I am showing liver damage and potential anemia problems, even though I have been supplementing iron, methylfolate and B12 for years! So I guess it is off to the endocrinologist…
Of course fusion surgery shouldn’t be taken lightly and as expressed by my surgeon it is the last resort when everything else fails. Also, to fully diagnose CCI and AAI and not mistaking it for something else takes time and needs to be done very very carefully. For me it is the last resort and I have made the decision with open eyes and as much information, science, case studies etc that is available and I am confident that it will help some and at worst only stop the gradual decline of my status. Sure instability in non-fused segments is a reality to be counted with. As far as I can tell, the technique for fusion surgery varies and has just in recent years become much better. I have no illusion about being fully fit and healthy again after surgery, but if I can get as much as 50% of my ability back it would mean the world to me.
Well then Joakim, I wish you the best of luck! Sometimes there is no other way, especially if symptoms are very severe. My prayers and kindest wishes your way!
I only expressed my opinion because some people may not entirely grasp the seriousness and risks of certain surgical procedures, but it sounds like you certainly have.
Hi Nancy, I’m curious as to how a severely ill ME patient is going to really give physical therapy a try? Perhaps this is feasible for an EDSer. I have both & find any PT brings on PEM. It is also frustrating to feel like you are working with muscles that absolutely refuse to strengthen. Granted, I have not tried it with a PT knowledgeable about EDS & ME, being that they are few & far between. But it is of interest to note that Muldowney himself says if a patient is not strengthening despite PT efforts they most likely have some form of CCI, Chiari, Tethered cord, or similar condition that needs to be surgically addressed before they can benefit from his protocol bc if they have a condition like that their muscles are not getting proper signaling & will never strengthen properly, no matter the quality or amount of PT.
Sorry I’m so verbose today, but just though of something else related; cerebral spinal leaks. They can also cause symptoms. Some of my EDS co-horts have reported clear liquid leaking from their nose and sometimes their ears, which turned out to be CFS leaks. These indicate there is some kind of breach in system since the fluid circulating around the brain and spinal cord is very near the sinus cavities.
I’m no expert in this area, but it may be that inter cranial hypertension may be causing some of these. I do wonder if some of our idiopathic rhinitis may actually be leaking CFS fluid…
I came to the Bragée Clinic last fall in hopes of finally getting a proper diagnosis after 17 years of chronic fatigue, and I wasn’t exactly impressed.
I’d completed and sent in their questionnaires, and got an initial appointment with one of their doctors, who started to interview me on the same questions all over again, saying that they hadn’t received my questionnaire (although a nurse managed to locate it towards the end of my visit!). They later did a tilt test (though they rescheduled that appointment without telling me), sent me to a hospital for an MRI, and made me see their dietician. Then I got a second appointment with the doctor, who basically told me that as I don’t have pain, and am only borderline POTS (thanks to self-medicating with salt, which I told her), she couldn’t give a CFS diagnosis. Besides, she’d never heard of 2-day CPET and other current research I’d read of on this site.
So, I’m not at all surprised to read that the Bragée clinic also chose a less professional way of publishing its research.
Sorry to hear about your experience at the clinic. I’m no spokesperson from them but here is my take on why they chose to publish they way they did: A peer review process can take a year and takes resources to deal with, resources that can now be used for other planned studies. The published paper can be used as a means to get ethical permission for studies (which is needed). Also, they want the knowledge out there as soon as possible so that other scientists within the field get a new perspective on this complex disease, get new ideas how to do their research and so on, but also for patients like me, who got a whole new understanding of the root cause of my problems and can hopefully find a solution. I dearly hope you will find that too. Keep looking and don’t lose hope.
This study is such bullshit. Baraniuk and Natelson consistently report normal opening pressures and none of these abnormalities, and they’ve done twice as many.
Given the choice between anecdotal reports and a study I would tend to go with the study. Besides, Baraniuk was the one who told me he found it a lot in ME/CFS. (????)
De Jurgen,
A late response to the astraunaut issue:
The article is an interview in a flemish edition of Newsweek (in dutch = flemish)
They interview Angelique van Ombergen ,she is affiliated with ESA (European space agency) and is on the Forbes list of most promising researchers
“during a six months stay in space grey matter of the brain diminishes and the volume of brain fluid rises. Back on earth the gray matter restores itself but the extra brain fluid remains”
Hi what kind of specialist would I go and see if I have Craniocervical Instability etc or any of the problems above. Would this be a Neurologist?
What if blood flow to the brain is chronically reduced ie giving PoTS type symptoms.. this means there more space and so over time this produces an increase in csf pressure giving symptoms of IIH. in my case aai & cci fusion surgery greatly improved syncope symptoms but I’m at left with IIH symptoms.. ie the pressure remains high despite the blood flow being resolved.