“It’s like nothing I’ve ever seen before.” ER physician – New York
The world’s medical systems were hardly ready for COVID-19. It turns out that our bodies, in a new and strange way, were unprepared as well. A viral trickster, COVID-19 appears to be doing something no other virus has done.
It’s creating a condition called “silent hypoxia” which has become a major killer with COVID-19.
In A New York Times piece, “The Infection That’s Silently Killing Coronavirus Patients“, an ER doctor in New York describes a strange scene. COVID-19 patients without breathing problems have been shocking doctors by walking in to the ER with full-blown pneumonia. The ER rooms in NYC have been overwhelmed primarily because of the “alarming severity of (the) lung injury” the virus has been producing.
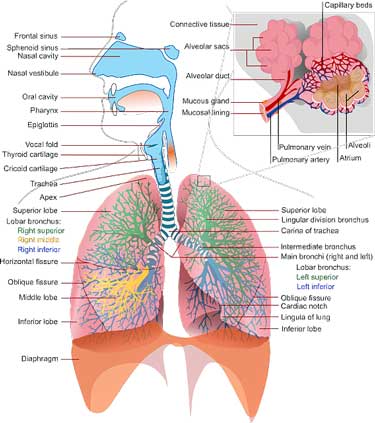
Damage to the lungs is driving many of the ER visits from COVID-19. Image-by-Clker-Free-Vector-Images-from-Pixabay
Pneumonia refers to a viral or bacterial infection which almost always causes shortness of breath, pain when taking a deep breath and/or rapid, shallow breathing, Not this time.
The lungs’ main function is gas exchange: the air sacs or alveoli in the lungs expand to take in oxygen and then expel CO2 when they deflate. During most cases of pneumonia the air sacs become inflamed and fill up with fluid, causing problems with both oxygen extraction and CO2 release.
The shortness of breath and the rapid, shallow breathing pattern seen, though, are initiated not to increase oxygen uptake, but to facilitate removal of the toxic CO2 molecules that have been building up.
COVID-19 can cause blood oxygen levels to fall dramatically and produce moderate to severe pneumonia before the normal signs of pneumonia such as shortness of breath and chest pain occur. This is causing some COVID-19 patients to become dangerously ill without knowing it.
Normal oxygen saturation for most people is 94-100% but the ER doctor reported that a “vast majority” of COVID-19 patients seen at the hospital had “remarkably low oxygen saturations”. Some COVID-19 patients, with oxygen levels so low that they seemed “incompatible with life”, were still using their cell phones! Some have had oxygen saturation levels – the level of oxygen in their blood – as low as 50%. (Normal is 94-100%).
(This seems eerily reminiscent of people with ME/CFS with seemingly life-threatening low levels of blood volume, or blood pressure.)
How are COVID-19 patients managing to get so ill without their knowing it? Probably because of the way the virus attacks the air sacs or alveoli in the lungs. Initially, COVID-19 prevents these air sacs from expanding to take in oxygen, but until the inflammation cuts in, their air sacs are still able to expel CO2 – and it’s the buildup of CO2 that leaves us short of breath, not low amounts of oxygen.
People with COVID-19 are compensating for the damage to their air sacs by taking faster, deeper breaths – not knowing that doing so causes more inflammation, more damage to the air sacs, and ultimately, a faster progression of their pneumonia.
By the time some people actually have trouble breathing, their lungs have been so damaged that they have to immediately go on a ventilator. So much damage can unknowingly occur that some COVID-19 patients die shortly after experiencing shortness of breath. The CDC warns that anyone with bluish lips or face should get immediate medical attention.
The New Normal: A Pulse Oximeter in Your Medicine Kit
The ER doctor asserted that much of the damage associated with the epidemic of “silent hypoxia” (hypoxia refers to low oxygen levels) could be prevented if people with COVID-19 could be seen before their pneumonia became severe.
Thankfully, there’s a cheap and easy way to do that – it’s called a pulse oximeter which can be purchased for as little as $30.
“(That) … requires detecting silent hypoxia early through a common medical device that can be purchased without a prescription at most pharmacies: a pulse oximeter.
Widespread pulse oximetry screening for Covid pneumonia — whether people check themselves on home devices or go to clinics or doctors’ offices — could provide an early warning system for the kinds of breathing problems associated with Covid pneumonia.”
He recommended that everyone with symptoms of the disease (cough, fever, fatigue, etc.) should have a pulse oximeter.
The doctor noted the pulse oximeters are not 100% accurate but that they are “extremely reliable”.
If you have COVID-19 symptoms you should also, whether you’ve been tested positive for it or not, lie on your stomach and sides – not your back. Simply doing that may be able to help many avoid ventilators.
The doctor’s advice flies in the face of Dr. Albert Rizzo, the chief medical officer for the American Lung Association. He doesn’t believe that most people need a pulse oximeter. He says it can help, but “monitoring your symptoms—cough, shortness of breath, chest discomfort—those are the main things.”
Rizzo apparently didn’t know of the silent hypoxia that is causing lung damage prior to symptoms like chest discomfort or shortness of breath showing up.
Dr. Klimas reported that ERs in her area are setting an alarm level of about 92%. She recommends that people with ME/CFS get up and walk around the room before taking the oxygen saturation levels.
The American Thoracic Society reports that “most people need an oxygen saturation level of at least 89% to keep their cells healthy”. They state that wearing nail polish, having artificial nails, cold hands, smoking, having poor circulation or dark skin can affect the accuracy of pulse oximeters. (Smoking artificially elevates it). The sensor should be placed at the base of the nail. If you have artificial nails, you can trying putting the probe on sideways, or use a toe instead.
The best readings are produced when your hand is warm, relaxed, and held below the level of your heart.
Accuracy Issues
A study indicated that pulse oximeters are not always precise, and that expensive ones are not necessarily better than cheap ones. All the pulse oximeters tested in one study, however, were accurate (within 2% of real values) when blood saturations were >90%. – which is around the level we’re concerned with.
The Contec CMS50DL and Beijing Choice C20 worked superbly down to 70% saturation levels. Accuracy diminished below that for some models but was generally within 3%. If your measurement is in the 80’s, knowing your exact saturation level isn’t your priority, though: at that point you need to see a doctor.
The TempIR-Oxy, Jumper JPD-500A and Nonin Vantage 9590 also did well in another study.
Pulse oximeters cost from $30 to well over $100, with most on Amazon clocking in around $50. Delivery times lagged at Amazon but I was able to get one delivered from Walmart fairly quickly.
Take the Coronavirus Poll
Please take the poll whether or not you have symptoms. If you know someone with ME/CFS/FM who is in the hospital (or has died) and cannot respond, please take the poll for them.







One person wrote:
Hit fast and hard with fever and sweats (like someone poured water over you), but no chills. Let fever burn and didn’t suppress it. Also had sore throat and hurt horribly with terrible headache and pains everywhere. Drank apple cider vinegar with honey and lemon. Took antiviral. Also did detox for liver, lymph and kidney. Drank a lot of lemon water. Got over it faster than expected.
Not sure we had it. (Hubby had it too.) But have a theory as to why it may have been milder for me, if I did.
Since this virus seems to go in on ACE2 and that is a key to it invading…….I have very low renin and aldosterone. Angiotensin is the in between of those two processes (at least in the kidney) that is where ACE is affected, angiotensin. It may be that because of one of my dysfunctions it actually saved me, by having too low amounts in my body. Angiotensin can also be in the brain and heart too. And that could explain why this virus is attacking the heart and brain (neurological) of people. I did read some information of doctors trying to decide if it is good to have lower angiotensin or higher. Big debate on it. Also trying to decide whether or not to take people off ACE and ARB inhibitors.
But this is just a hypothesis, if I did have it, as to why it wasn’t so bad for me. And this is from a girl who has Hypogammaglobulinemia and no ability to fight pneumonia. So would be a very good thing to have checked out.
We aren’t taking chances, because we don’t know if we have had it. But indications are, we did. And when antibodies testing is available, we want to find out for sure.
Another:
I nearly died of pneumonia about 6 years ago so I knew what was happening. As soon as I felt seriously unwell I contacted my GP who sent antibiotics and steroids straight away. I stayed in contact and at about 12 days in he sent me to A&E, as my breathing was poor, where I was xrayed and assessed.
However, as it was ok to stay at home with support I was not tested. Judging by the reaction of staff however I’m sure they thought it was Covid.
It is now 5 weeks since I fell ill, I am just getting my sense of smell back however I still have difficulty with breathing when walking and a new pain behind my right lung on my back. I also feel even more tired than usual.
It was definitely not the flu. My family however had a spectrum from slight cough to being floored for a week or so.
Another person:
Of course, every day for me is flu like/pain filled, but the bout I had in late January,early February was a very different type of illness. There was no awareness of a new virus, except what China was going through & neither I, nor my husband considered anything other than either a very bad flu,or pneumonia.
Went to see doctor, but could only see his PA. She dismissed me as nothing serious, took xrays(I insisted) & wrote a rx for a z-pak(I insisted). It was a infuriating visit & I came away feeling like I was a waste of her time.
My fever went up to 101 for the first few days, high for me, since my temp runs at about 97.7 to 98.1, sometimes lower. The tightness in my chest, exhaustion, pain were intense. X-rays showed no pneumonia, which was a relief, but this stuff lasted well into 4 weeks & literally wiped me out in ways I have never dealt with before, even with ME/CFS & FM.
Just now starting to feel like my normal w/ chronic pain illnesses. My RA doctor agreed that what I had may have been COVID-19, but tests in CA are scarce as hen’s teeth. So can’t be sure, but hope to find out for sure at some point. Appreciate opportunity to take this poll, sure there are many out there wondering like myself.
Thanks, Cort.
Another:
In the beginning of our symptoms, my husband and I saw our doctor at his office, but in his parking lot. He told us we likely have COVID-19, but that it was extremely difficult to get it tested with the tests in such short supply. He told us to stay home and call him before going to the ER if we were gasping for breath, otherwise DON’T GO TO THE ER.
Because of my asthma. I was using my nebulizer 2 to 3 times each day, which helped my breathlessness. Even though ME/CFS has had me housebound and recliner/bedbond for the past 6 years, I am worse now after mostly recovering from apparent COVID-19.
I have not spoken to my useless PCP since we saw him. There is no point. Our medical system ALWAYS fails us. I still have wicked headaches and horrendously weak. But my sense of smell and taste suddenly came back a few days ago. I had not even realized it was gone until it came back as if somebody turned on the “power switch”.
I didn’t even know that losing sense of smell and taste was symptoms of COVID-19 until a couple of days after they “turned back on” and we saw it on the news.
My asthma doctor told me that if I get sick with COVID like symptoms, do NOT use nebulizer. It will release virus into the air. I had never thought about that. This would make it even more contagious within the home.
Awesomeness Poll, Cort! GIVE IT A?! ESPECIALLY, the last question and last answer to bubble in,
“Pure Hellish”!
Great Job!
Wow what a conundrum. You would have to make sure you used only in a safe place in your home away from others.
Thanks Lora 🙂 A lot of hellish responses. This thing can be really nasty..
Yes I was told by a Dr to do it outside the house for the protection of others in the house.
Another person:
I’ve likely been exposed (my son is still working two jobs in the general public) and have had symptoms but not diagnosed. The symptoms overlap and it’s difficult to tell if it’s a flare or Covid. I can feel my body fighting mightily.
Back in january , i booked the usual cottage where i meet up with extended family (as my birthday falls on the 31st jan, as we all live in different parts of the uk.)
Id been suffering terribly from what i thought was a chest infection (as i get these every winter.)
On day of travel, my GP phoned me out of the blue, and said my bloods had come back and my inflammation levels were through the roof.
He said i was at risk of pneumonia and even sepsis.
I went in to see him straight away and he prescribed big dose antibiotics and steroids.
I stayed in bed for a week.
But the cough has never left me.
I just got up, and got on with it , as i usually do , despite having several chronic co morbids.
Now I’m beginning to wonder whether or not i had covid 19.
Another:
Another person asked
Dr. Bateman has said “You will know!”
Another suspected stress made things worse. (I’m sure this is true for me).
Another person with ME/CFS and FM is still struggling after 5 weeks. (Dr. Klimas said don’t be surprised if it takes 6-8 weeks for your COVID-case to resolve.
Another person is having perhaps her first fever in 20 years:
One person from the U.K. found his/her symptoms disappearing and then coming back (This has been reported elsewhere):
I live in UK.
Strangely, the virus symptoms came and went. Sometimes I thought I was recovering for a day – or two even – but then it all came back. Gradually, over 4/5 weeks the severity of these flare-ups has reduced.
On a couple of occasions I had phone appointments with medical staff and was prescribed steroids because of asthma and shortness of breath. I was never offered a test for Covid 19, despite a nurse saying I may well have it.
I was glad not to be hospitalised as I thought I’d catch even more bugs in there(!) Also, ME/CFS is not officially understood properly within NHS, so I wouldn’t be able to stick to the regimes I know help me. Though I printed out everything ME-UK produces to explain the condition and special drugs considerations – just in case. At least now I’ve got that info in my handbag for future use of needed!
I believe that having lived with ME/CFS and asthma for many years actually helped me cope with the horrid symptoms better – I’m used to muscle pain, having to rest, stay indoors, pace myself, breathe slow and deep etc. But I was frightened at one stage and that’s when my husband rang 111. The doctor was very helpful, especially when I said I get asthma but took no notice of my saying I had ME/CFS.
Somebody FM was experiencing terrible pain:
I don’t know that this is Covid-19, but if it isn’t it is one of the worst fibromyalgia flares I have ever had. Fatigue, Severe muscle & joint aches, skin itching & burning, too much pain to literally move a muscle or hold my cell phone, or sleep. 1000 mg of Tylenol and 600 mg of ibuprofen and hour later hardly helped at all. The second day was better (can use my phone propped on a pillow). I’m 63.
Another person who rarely gets colds now has a doozie:
I do not usually get colds or flu as my immune system is always on high alert so was surprised to get a nose that would not stop running,I had awful headaches and then fever and chills with shaking,also random bouts of diarrhoea followed by a wheezy hacking cough,it feels like my lungs are not expanding properly and are still tight,I felt too ill to get myself to a gp and thought as I had viral symptoms I would not need antibiotics.
Another with asthma found that her lungs and heart had been hit hard:
Whatever I had, made my normally mild asthma a big deal. I hardly ever needed an inhaler before. I’m still on two inhalers a day now, and still coughing hard enough that I think I cracked a rib, even though all other symptoms have long since subsided.
I’m still so tired and weak. I think this infection caused damage to my lungs that may be permanent, and I know it stressed my heart… I have never seen the horrible vital signs that I saw during this illness before… High bp, tachycardia that was off the charts, and wide pulse pressure… 100 points difference between systolic and diastolic numbers. Yet the hospital decided I wasn’t “sick enough” to test because I was breathing on my own with the inhalers. Unreal.
Another filled in some data on her son with ME/CFS:
I filled this out for my son who has been suffering from diagnosed ME/CFS for over 5 years . He was very sick in March but it was a strep infection that antibiotics cleared up.
Had it with partner, mid March (in NYC). Both in our late 60s with no real comorbidities. Mild, symptoms through first week. She had a sporadic cough, I’d anosmia. No prolonged fever, lower than normal, as checked ~97° but copious sweats, bad muscle/ joint pains; she had severe headaches & scary kidney pains. I’d never felt apoxia previously, snd we’d had sporadic delerium and light headedness, sporadically going into 3rd week. Both felt inflammation in trachea (heart?) lungs (but upper, like bronchitis?) intestines (like diverticulosis?) our appetites were seldom affected. Taking Quercetin, resversetrol, D3, zinc, C, A and Sambuchus nigra (eating more brightly colored greens & drinking tart, DARK berry juices). ELISA IgG ~day 59 was negative, but very low (for me) 89-95% on pulse oximiter.
One experienced fatigue like never before:
I believe I had it in January into February. Went to Urgent Care twice. Second time put on a breathing treatment/inhaler with a z-pack and 5 days of steroids. That’s when I finally started getting better. The fatigue was like nothing I’ve ever experienced before. My husband, who rarely gets sick had it too. He was able to ride it out for 6 wks.
Another described his/her worst illness experience ever.
The worst illness ive ever had, could not get out of bed for 5 days. Now 4 weeks later still have severe fatigue, good and bad days, but muscle aches come and go. Struggling. Off work.
Given that there was already a shortage of pulse oximeters for sale (e.g. on Amazon.uk), I wonder if other methods to detect “silent hypoxia” might be deployable by health authorities; I’ve not read this paper, but it seems it might be possible to assess this symptom from voice stress patterns: https://www.jsams.org/article/S1440-2440(17)31191-X/fulltext
Fascinating stuff! The creativity around us….Let’s hope that works out.
Doc on TV said I now look for blue toes and fingers.
Horrifically Ill…
My experience was a bit earlier in the year. I visited SF to celebrate New Year’s Eve, and cut my trip short abruptly when I began to feel sick. Due to my ME/CFS, it’s often hard for me to tell if I’m actually getting sick (like with a virus that might be contagious to others) or if it’s just another one of my flare ups.
Rather than sticking around to find out, I flew back to Seattle on Jan 1st. I was horrifically ill for 3-4 weeks. My husband (who rarely gets sick) caught it from me, and he was down for almost 2 weeks. That’s very unusual for him.
Allergies or coronavirus?
Might have been allergies instead of Covid-19. Same symptoms along with sore throat, but no sneezing, just dry cough. My husband, age 69 had same thing a few days later, but recovered quickly. No idea
Waiting, waiting for answers…
I had horrible headaches, a runny nose (perhaps concurrent allergies), mild intermittent fever, diarrhea, body aches and pains, fatigue, and very mild shortness of breath. I only had occasional coughing, usually in the morning.
My partner, on the other hand, had all the classic Covid symptoms. I’m sure he caught it from me about a week after I got sick.
What we both noticed is that we would think we were getting better only to have a relapse of symptoms. This has gone on for weeks to a couple of months. We are both over 65, and are only now starting to feel ‘normal.’ Fatigue was the lingering symptom.
I caught my ‘something’ mid February and am reading that Stanford (not too far from me) has recently detected Covid patients since early February and suspects that it was circulating much earlier than our ‘first West Coast patient.’
I went multiple times late January through February to a huge rummage sale where I touched thousands of objects and interacted with hundreds of people. (How would that be for contact tracing!?!) That’s where I think I caught my illness.
Trying to access a test was futile. At first a temperature was required and also foreign travel. Then it was a temperature at the time of testing, but our fevers were intermittent. Then one needed a doctor’s appointment; difficult to get unless one had the ‘classic’ qualifications and symptoms. Finally, even if we managed to get approved, who wants to sit in their car for hours when feeling shitty, to get tested? The testing sites were known to frequently run out of tests, and if you did test positive, you were only told to quarantine for two weeks unless you were seriously sick. So, total testing failure IMO.
I still don’t positively know if I was infected and so am waiting for an antibody test. Will that give me immunity? At this point nobody seems to know for sure.
What a mess! All I can do is wait inside my house…
All the symptoms but lungs were clear
I had a number of the symptoms and worries that I had COVID19 or pneumonia. I was checked by Dispatch Health and my lungs were clear and pulse ox good. I do have an infection by my central line and have been feeling better with the antibiotics. Still extraordinarily fatigued and weak.
A very unusual illness…
Unable to get tested and infection numbers are low where I am so it is difficult to know if it was COVID-19, but last month I experienced a very unusual illness. I had a mild fever and cough, terrible aches and pains, an upset stomach, and my heart rate went through the roof. I also had an incredible weakness- very different from normal.
I found myself crying when I got up, just from exhaustion. Couldn’t concentrate at all. It initially lasted 5 days, then cleared up for two days, then came back worse. However it disappeared quite quickly after a week and a half. Almost back to my baseline- perhaps slightly worse than before.
Diarrhea and COVID? (Gut problems show up first in about 10% of people with COVID-19)
I don’t think I had the virus, but I have been more tired than normal and the diahrrea seemed unusual. I have had no known exposure. I have also had extremely itchy eyes and a runny nose, more than what seasonal allergies seem to merit. No coughs or congestion.
Amazing all the different forms COVID-19 can take!
I have a question; is everybody reading this site having trouble getting toilet paper? PPE aside, it seems to be the most scarce commodity! Here it is months after the pandemic began, and STILL, TP seems to be nearly non-existent. If it does appear, it is snatched up in minutes. Order on-line? Forget it! Back orders for weeks!
Could self quarantine really account for all of it? What gives?
TP shortage a big confusion, so there are people home that are usually at school or work so I don’t remember using that much TP at those times?? Then there are eggs “one to a customer” (container) and the price?? News said a farmer had to kill 60K chickens because of low egg demand??
How exactly does lying on one’s stomach or side prevent lung damage? How does taking faster, deeper breaths cause more inflammation, more damage to the air sacs, and ultimately, a faster progression of pneumonia?
think answers are in here…
(sorry to give only link instead of answer)
https://globalnews.ca/news/6788251/breathing-technique-coronavirus/amp/
Thanks, Sunie. That’s a good partial answer.
Hi Tim,
I developed asthma, as an adult – I don’t wheeze, it affects my lower airways and nobody believed me. So I was having continuous asthma attacks repeatedly for years. The only way I could breathe at night was by lying on my front. People having an asthma attack should not lie down.
So when I heard medical professionals talk of some Covid-19 patients improving their blood oxygen levels by having them lie on their front, it made sense to me.
Please research “5G effects on oxygen”. Some people say that they have read from a book called Magnetobiology that 60GHz frequency disrupts the electrons from the oxygen molecule or something like that…
Completely different!
Completely different than any cold or flu (or bronchitis or mono or anything else I’ve had). It comes and goes so you think you’re better for several days and then you suddenly aren’t. The worst is definitely around day 10 give or take a few days. I had no fever, essentially no cough, and still was still quite ill with breathing problems, chills and weakness. Like ME/CFS COVID-19 is pretty obvious in how odd and unlike anything the symptoms are (at least in some people), and how like ME/CFS you can look and even seem fine until you try to exert yourself in some way, then everything rapidly and dramatically gets worse. I’m 5 1/2 weeks from when I got sick and still have not fully recovered the exercise ability I had before getting sick (which was limited to about 5 minutes of walking).
Several rounds???
I don’t have an actual diagnosis of ME/CFS but my symptoms began following an enterovirus and match the criteria for ME. I also get repeating viruses and am sick with either an original round or a repeating round all the time. I have had 5 different rounds (with repeating rounds in between) of a sickness which I believe to be Coronavirus and each time is a bit different but follows the same basic progression of symptoms- cold/sinus symptoms followed by sore throat, followed by lung and stomach symptoms, with aches and chills throughout all stages. I believe it is mutating and I keep catching new strains.
Extreme overwhelming fatigue
I spent over two weeks sleeping every afternoon with extreme, overwhelming fatigue. (this was early feb.). Exposed to someone traveling internationally on a regular basis (ESPN coverage) in early January. After exposure, had splitting headache and fever, but curious absence of nasal congestion.
Shaking Chills….(shaking chills are another odd manifestation of COVID-19
I had extreme shaking chills in February but just thought it was a new symptom of UTI that is recurring since cancer in 2009. Urologist said it didn’t sound like it. With our condition what is left for symptoms. During Tx for cancer the doc said, did you know you have a serious infection, I did not. Same thing with shingles. Because of a criminal lawyer am under extreme stress and you know what can do.
Very early case?
My symptoms currently are not Covid-19 related however I had those exact symptoms of Covid-19 for one week commencing on Dec 23,2019. Specifically high fever and severe cough with negative flu test caught from son-in-law. Am interested in an antibody test.
Lost sense of smell and taste overnight
I had symptoms of infected bunged up sinuses, sore but not swollen glands, lost my sense of smell and taste overnight but it returned, I had an overnight fever, my throat was sore, dry and hoarse as though something was stuck < this symptom persisted and still have it 3 weeks later. When most of the symptoms lifted I got a severe pain and fatigue flare. I don't normally catch things my family get but I caught the virus off my daughter who also had it mild. We can't be sure it's Covid19 but it was a lingering virus.. Worst cold ever….
It’s like having the worst cold, flu, migraine, and food poisoning in the world, all rolled into one. In my case, it lasted for 2 months straight, and I still get daily headaches, shortness of breath, and hot flashes.
It is the worst illness I’ve had since I fell ill with M.E. 14 years ago. Honestly, I’m amazed I didn’t have to go to the hospital.
L.moore0684@gmail.com
Just the flu or ???
My COVID-19 test was negative, so I guess I didn’t have it. It was such a coincidence to come down with some kind of flu on March 18 with fever, dry cough, chills, sore throat, serious body aches, etc., that weren’t COVID-19. I did not have shortness of breath, so I guess it was just regular flu with no congestion.
Hard to shake…
It was like a very unusual cold. It had symptoms I have never had before with a cold. So it was at the same time not a severe illness, but still grueling.
One example is the way it prevented me from sleeping at night. Another is the persistence of the symptoms. It was very hard to shake.
Stress triggers a flare – not Covid?
It is impossible for me to distinguish COVID-19 symptoms from my ME/CFS ones and I wonder if all the stress associated with COVID-19 triggered a flare.
Butyeko breathing?
Thank you for this, Cort. As soon as I saw the NY Times article, I ordered an oxymeter from Amazon. It should arrive in about a week.
Meanwhile, I wonder if the technique of Buteyko breathing, described in the book The Oxygen Advantage by Patrick McKeown, would be helpful in increasing delivery of oxygen to the tissues and reducing build up of CO2.
Personally I think that’s a great idea.
Lyme or Covid?
I’m in NYC so despite our attempts to bunker it’s possible my bf and I were exposed. My symptoms seem kinda typical for me having LYme—but the timing to me is suspect especially since I just upped my dose of LDN again and haven’t had a relapse like this in a while. Then again I’ve been sick every spring (starting in Jan/Feb) from rat mite bites (I shit you not) and/or LYme for a few years in a row now. All “squishy” symptoms that aren’t totally out of ordinary for me so it might not be COvID at all? Hard to tell.
I would also add sore throat to that.
And the fact that they’ve mostly faded but have come back repeatedly—I feel like I fought off five relapses of “bone pain”/chills in a row but j dialed last night to fight off this latest one. Could j be LYme/CFS tho?!
Former nurse highly recommends pulse oximeter
It’s worth noting that my Saturation levels are often 91-93%, with only mild asthma as well as ME/CFS & Fibromyalgia. This mild hypoxia is most obvious when I’m brain fogged and fatigued. As a former nurse I am confident that readings are accurate. Highly recommend anyone with these conditions to buy one, as it’s important to have a baseline for comparison if/ when you do become ill.
Hospitalized patient back at home after spiking fever and spiking blood sugar levels
Additional effect/symptoms of Covid-19 not listed above:
1. Horribly dry mouth 2. Some vomiting (basically Bile) 3. Hospital did blood work. My sugar spiked to 145. I am not diabetic and had blood work done three weeks before getting Covid and sugar level was normal. 4. Fever would be much lower in the morning and would start climbing again in the afternoon. This happened every day for over a week. Highest fever 103.9 (my normal is 97.0) 5. Low blood oxygen level of 86. (mine has always been normal)
A five-day something….
I have no idea if it was covid or just a bad cold of flu but i haven’t had full blown cold and flu symptoms since swine flu epidemic. everyone in my village had similar symptoms (upper respiratory infection that started with sore throat and some shortness of breath) that lasted a good 3 weeks and which they found hard to shake off from December to February. My symptoms lasted for about 5 days, mainly sore throat, urti, increased fatigue and general aches and pains.
The normal flu or COVID?
It felt like the normal flu, I had a temp of 102 for 2 days and slept a lot. The worse symptoms were over in 2 weeks. It may have been just the flu. It was at the beginning of March.
A system reset?
I am clear now. All family suffered from different symptoms. At the time fever and dry cough, we never had that. Child pink eye, Tired and headache.
I felt really bad for 2 days then had a series of symptoms over 4 weeks. Odd that I would have symptoms am disappearing pm and vice versa.
NOTE. I have experienced ME for 5 years. My experience. Nerve pain, failure to produce energy and a terrible ‘hungover’ feeling. It varied but was always there. Sometimes bedbound. Can I say since I suspected Corona, I have not had the feelings of being hungover. I haven’t told anyone apart from my wife. I can’t believe it and I am desperate to know if other might have experienced the same as me. Almost as if something has reset itself! Thank you.
Weirdest illness ever
It was the weirdest illness I’ve ever experienced, not like any cold or flu I’ve ever had. Symptoms would improve and worsen from day to day. Day 9-10 were the worst. Gradual improvement after day 14. Me, my husband and my 7 year old also had conjunctivitis and my husband had purple swelling under one eye that slowly became like a crusted blister. My husband had shortness of breath and fatigue for several weeks and he never gets sick enough with the flu to stay home from work. I think it might have helped us that we take high dose vitamin C and D with viruses, quercetin, zinc, oregano oil, olive leaf and paleo diet with lots of vegetables
Worst cold or flu ever
In early February and late January, I believe I became sick with Covid-19..my doctor diagnosed me with an upper respiratory infection. It took 3 different types of antibiotics and 3 rounds to feel well again. I developed pink eye, which I have never had before in my life, in both eyes. And I remember laying in bed, thinking and feeling like I could die from this sickness. I haven’t been sick with anything in 10 plus years. And this came out of nowhere. It was six weeks of the worst flu, pneumonia virus I have ever dealt with. Fortunately, I lived through it.
Worst flu ever
I had the worst flu I’ve ever had starting 2/24/20 that lasted about 6 weeks. See above symptoms marked. I also marked symptoms I regularly experience with MECFS but were worse with the flu. I never had a fever or chills though. I was denied testing because I didn’t meet the narrow criteria, so I don’t know if I had COVID 19. But since recovering from the flu (whatever it was) I think the Shortness of Breath and fatigue I had with MECFS are worse now and that doesn’t seem to be changing. I feel that the flu I had permanently made my MECFS worse. Especially the SOB.
Futility with testing….
I had horrible headaches, a runny nose (perhaps concurrent allergies), mild intermittent fever, diarrhea, body aches and pains, fatigue, and very mild shortness of breath. I only had occasional coughing, usually in the morning.
My partner, on the other hand, had all the classic Covid symptoms. I’m sure he caught it from me about a week after I got sick.
What we both noticed is that we would think we were getting better only to have a relapse of symptoms. This has gone on for weeks to a couple of months. We are both over 65, and are only now starting to feel ‘normal.’ Fatigue was the lingering symptom.
I caught my ‘something’ mid February and am reading that Stanford (not too far from me) has recently detected Covid patients since early February and suspects that it was circulating much earlier than our ‘first West Coast patient.’
I went multiple times late January through February to a huge rummage sale where I touched thousands of objects and interacted with hundreds of people. (How would that be for contact tracing!?!) That’s where I think I caught my illness.
Trying to access a test was futile. At first a temperature was required and also foreign travel. Then it was a temperature at the time of testing, but our fevers were intermittent. Then one needed a doctor’s appointment; difficult to get unless one had the ‘classic’ qualifications and symptoms. Finally, even if we managed to get approved, who wants to sit in their car for hours when feeling shitty, to get tested? The testing sites were known to frequently run out of tests, and if you did test positive, you were only told to quarantine for two weeks unless you were seriously sick. So, total testing failure IMO.
I still don’t positively know if I was infected and so am waiting for an antibody test. Will that give me immunity? At this point nobody seems to know for sure.
What a mess! All I can do is wait inside my house…
Thank you for conducting this poll.
Profiteering is going on here in the UK. Prices are very high. I just looked at one for £40 that evidently sold for £12 originally! Most seem to be shipping from overseas and won’t arrive until June. I have finally found one through a medical supplies company. It cost about £55
I bought myself recently a smart watch with inbuilt oxygen saturation meter. I was interested to know my oxygen saturation levels and reading that it might warn early for Covid problems made it a simple decision.
It is also a watch, counts steps a day, tracks heart rate and does a few other minor things. The oxygen saturation and heart rate tracking is on demand rather then continuous but it is easy to use. You have to hold still for about 15 seconds though.
The plus sides? You’ve got it with you all the time unlike most medical oxygen saturation meters, it doubles as a watch and the battery lasts over four days with me (with Bluetooth connection of my phone off). The price, 35 euro is also a boon. The oxygen saturation meter seems to work precise enough. I don’t have another device for comparison but it behaves reliable meaning that when I overdo it too much values crash too.
The downsides? It doesn’t work without at least connecting once to a smartphone, time starts to deviate after two weeks so I think I should reconnect it to my smart phone (that I rarely use with Bluetooth on), you have to set up an account with Huawei and have to download their app and framework and like near all smart devices they slurp your data to “monetize”. The sleep tracking is nowhere near accurate at all so don’t buy it for that.
The most annoying part for me was that I first had to “update the devices bios” before the advertised oxygen saturation meter was even available. There was nowhere any information on their own website that that needed to be done. Image the fun I had finding that out! I call that poor customer service. More recent produced version may or may not have it out of the box.
The watch (not wanting to advertise but it is the single cheap portable smart watch / oxygen saturation meter I did found and it may be interesting for many others; feel free to add other options if you find some) is the Honor band 5. The cheaper 5s with textile rather then plastic / silicone band does not seem to have that option. The watch may not be seen in the section smart watches of some shops as it’s called a “smart band”. To me, the only difference is the smaller form. It is as comfortable or in my case uncomfortable to ware as a normal watch (I stopped wearing those since I had a cell phone with a clock as the feeling / tension of the strap bugs me to some extend).
(Q—How to start new thread??)
IMO, big news re: cfs/me……
and hope will have implications for corona virus sometime….
incomplete/partial virus reactivation is enough to whack mitichondria—involved in both energy and immune—laboratory.
https://www.immunohorizons.org/content/4/4/201
associated to study..
https://www.uni-wuerzburg.de/en/news-and-events/news/detail/news/viruses-under-the-microscope/
Bravo Bhupesh Prusty and team!!
corona
https://www.thailandmedical.news/trending_news
corona
wear masks
china
https://www.sciencemag.org/news/2020/03/not-wearing-masks-protect-against-coronavirus-big-mistake-top-chinese-scientist-says#
I don’t know how to share this but there is a very good video from DrZ (Zdogg) from Saturday April 25 with Dr Scott Weingard who is treating these patients every day that explains about “happy hypoxemics” with very low O2 sats who are capable of doing OK without ventilation. This would be the outcome we’d most like to see but most of us have comorbidities that might make it so much more difficult. Still, it is possible. I just hope the docs who treat us know about this and can refrain from rushing to intubation.
The concept of herd immunity makes sense in terms of finally getting a handle on going back to work but it is terrifying for most of us who haven’t been exposed yet..and we will inevitably be exposed. It’s heartening to hear that many of us with fibro have made it through infection but survival comes at such a cost when we’re already sick to begin with.
I forgot to add one of the main problems that came along with the virus and that went on for several months after was severe sweats to the degree I had to change my clothes sometimes 3 times in a day.
Thank u for posting and sharing this very important info, Cort! As soon as I read Dr. Levitan’s op-ep, I purchased 2 oximeters on EBay. I also started wondering why hasn’t the media been reporting more about this. According to Dr. Levitan, by the time most people start having breathing problems, they’re already in critical condition, and have to be put ion a respirator. I’ve had the unfortunate experience of being intubated and put on a respirator before ( nothing to do w Covid), and know it takes time for one to recover from that.
Time is a very precious commodity in our brave new world, and if a simple device as a pulse oximeter can potentially save many lives, this information should be much more widespread! Even prime minister Boris Johnson was supposedly saved by having his blood oxygen closely monitored.
As far as getting infected and recovering, I would say that, at least in my case, I am totally clueless. I suffer from severe symptoms of ME, FM, POTS, IBS, and many neurological problems. I have lost my sense of taste & smell years ago, for instance. My pain & fatigue levels are so bad that I’ve been bedridden for almost 5 years. I also suffer from constant headaches, diarrhea, nausea, flu-like symptoms and even shortness of breath, due to the POTS. So, for someone like me, how in the world would I know if I have contracted Covid or if it’s just another day?!
I also don’t get feverish – even when I had a kidney infection I didn’t have one. Moreover, today I read that about 70% of people in NY who became ill with the virus never ran a fever.
So, all I can say is that I’m glad I can at least measure my oxygen levels! Actually, I’ve even started wondering whether I have already had Covid, Have become immune and don’t even realize it!! Hey, you never know! ?
A very useful article, thanks. I also read the Dr. Levitan’s piece, researched oxymeters and found Contec and Beijing Choice as the best for under $50. I could’ve read your article and save the research time:-)
Thanks for sharing Patricia that one can get on a respirator and get off again and then recover. 🙂
I might be mistaken but, based on my own experience, it might not be that uncommon. I nearly drowned, and did inhale quite a bit of water. The doctors weren’t very optimistic about my outcome, and told my husband to not get very hopeful.
However, after I was brought back from the induced coma, four days later, I was very lucid, and already writing down a note telling my husband to ask the nurses to remove the tubing from my throat because it was really hurting me. Given my poor health, I would’ve never expected it. The doctors were also amazed when they came to the room and found me doing so well. I still don’t understand what really happened. I did not have any sequela in my lungs, but it took me a long time to emotionally recover from the episode.
So being on a ventilator does not mean one won’t get off. The challenge with Covid is that ppl usually need to spend weeks on it, and not just a few days. But many recover. There’s hope! ?
another article on covid-hypoxia:
https://www.thailandmedical.news/news/breaking-news-covid-19-alerts-british-doctors-warns-of-new-anomaly-of-covid-19-patients-appearing-normal-despite-suffering-from-severe-hypoxia
one site seems to put news out early
and consistently
and is almost unknown:
https://www.thailandmedical.news/
an example of news item:
“MUST READ! COVID-19 Crisis Unlikely To End In The Next Few Years, Eight Distinct Mutated Strains Identified With Different Clinical Manifestations”
at
https://www.thailandmedical.news/news/must-read-covid-19-crisis-unlikely-to-end-in-the-next-few-years,-eight-distinct-mutated-strains-identified-with-different-clinical-manifestations
Are the mobile health app based oxygen saturation levels accurate? I am planning to buy oximeter over here. Just wanted to know about it’s accuracy.
I have questions about the Dagamma. It has consistently shown mine to be very low – almost in the danger zone – for the past month or so. Yet I have no coronavirus symptoms. It can also start off high and then zoom down.