Chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM) produce so many symptoms that diagnosing them can be difficult for uninformed doctors. While we know that small fiber polyneuropathy (SFPN) (or small fiber neuropathy (SFN) commonly occurs in both these diseases, what I didn’t realize until I read the two articles below was that some researchers believe that SFPN by itself could conceivably produce all the symptoms associated with ME/CFS and FM. That’s a new conception of SFPN which is not embraced by most neurologists.
It brought up the question, though: if you have ME/CFS or FM and SFPN – might you really have SFPN?
Mystery Illness
“I was increasingly faint and dizzy, with my heart racing whenever I changed position or had a shower; and I was experiencing a fatigue and bone-pain so profound that every few hours I needed to stop whatever I was doing and lie down on the floor. The exhaustion, which feels like the start of the flu, was particularly severe a day or two after I exercised.” Eric Schwable
First Eric Schwable thought he had the flu but then came some weird symptoms: cold feet, burning legs, heavy, cement feeling legs, painful electric shock feelings, vertigo problems with sleep, heart racing when he stood up, or had a shower. There was the immense fatigue, the “bone-pain” and … the post-exertional malaise.
For many of us his diagnosis seems clear – he has chronic fatigue syndrome (ME/CFS) and/or fibromyalgia. Schwable put off seeing a doctor as long as he could but when he did see a doctor, that doctor immediately referred him to a cardiologist, a vascular specialist and a neurologist.
It turned out the doctor got the order wrong. The first two specialists didn’t uncover anything but the neurologist knew right off what he had: after a positive skin biopsy test, he was diagnosed with small fiber neuropathy (SFN).
As Schwable explained in his Washington Post piece, “Pains, chills, fatigue, vomiting and vertigo plague me. Small fiber neuropathy causes it all“, small nerve fiber problems can affect our circulation, breathing, digestion, and immune and glandular functions. Because they transmit sensory impulses, they can produce bizarre sensory issues.
Schwable was lucky – his neurologist was able to quickly match his wide variety of symptoms to SFN and quickly get him tested. Schwable is not well, but he’s found two drugs (pyridostigmine bromide (Mestinon) and gabapentin) that have helped.
Two Decades
“Pain is as ingrained in me as my oldest memories or my closest friends.” Jenna Birch
Jenna Birch was not so lucky. Even though the standard test is a simple one (a skin biopsy), most doctors and even most neurologists don’t know about it. Large fiber neuropathy, they know, but small fiber neuropathy, generally not. It took Birch almost two decades to find out what she had.
In “Before She Was Diagnosed With Small Fiber Polyneuropathy, Doctors Misdiagnosed This Woman’s Pain for 18 Years“, Birch described the strange “growing pains”, the “dynamite headaches”, the problems with bladder control and diarrhea, the rashes, the full body pain she experienced during childhood, adolescence and into adulthood.
She also described the countless doctors and ER visits. She was eventually diagnosed with fibromyalgia, irritable bowel syndrome, interstitial cystitis, and premenstrual dysmorphic disorder.
Not Fibromyalgia – Small Fiber Polyneuropathy…
Then she met Dr. Anne Oaklander – the MD, PhD who’d uncovered the small nerve fiber problems in FM. Oaklander asserted that fibromyalgia was a label – not a diagnosis. What Birch really had was small fiber polyneuropathy. That made sense to Birch, who was never all that happy with her other diagnoses.
“I never felt settled in my fibromyalgia diagnosis. I have consistently had to keep my eyes and ears open for potential conditions that fit my symptoms, and then bring them to my doctors.” Jenna Birch
Given the ubiquity of the small nerve fibers in the body, Oaklander believes damage to them to could cause just about any symptom found in FM.
- Pain – damaged small nerve fibers that transmit pain sensations could be producing the pain sensitization seen in FM.
- Gut Issues – damaged small nerve fibers in the gut could be impairing gut motility, causing constipation, diarrhea, gut flora problems.
- Fatigue – damaged small nerve fibers lining the blood vessels could be producing something called “neurogenic myovasculopathy”, which appears to refer to a nervous system disease causing problems with the blood vessels in the muscles.
- Inflammation – damaged small nerve fibers that regulate and are regulated by the immune system could be producing inflammation.
- Brainfog/Fibrofog – damaged small nerve fibers that extend into the brain could be affecting cognition.
Oaklander is convinced that a substantial portion of FM patients are misdiagnosed SFPN patients. In 2018, Oaklander asserted that fibromyalgia had “no known biomedical cause” until the SFPN was found. It’s not clear what Oaklander thinks about the 50% or so of FM patients without SFPN, but she’s pretty clear about what FM patients with SFPN have – they have a neurological disorder affecting their small nerves.
“Based on this definition, patients with FMS with subsequent diagnoses of SFPN (the SFPN+ group in our study) are instantly no longer considered to have FMS, per definition.” Lodahl and Oaklander
In a recent review paper, “Scientific Advances in and Clinical Approaches to Small-Fiber Polyneuropathy: A Review“, in The Journal of the American Medical Association (JAMA), Oaklander stated:
“A recent meta-analysis concluded that small-fiber neuropathy underlies 49% of illnesses labeled as fibromyalgia.”
Fibromyalgia, ME/CFS or Small Fiber Polyneuropathy?
Given the overlap in symptoms between the three diseases, one has to ask which diagnosis explains the most? SFPN is appealing because it has an identified cause – damage to the small nerve fibers – which can produce manifold symptoms, depending on where the SNFs are found.
Since small nerve fibers are found throughout the body – but are usually tested with a skin biopsy – is it possible that some people with nerve damage in other areas are not being properly diagnosed? Given the ubiquity of the small nerve fibers in the body, are the multiple diagnoses that so many get a sign that one might suffering from undiagnosed SFN?
Different Symptoms?
If the SFPN is different from fibromyalgia, it should generate different symptoms. Using a 33-item symptom checklist called Mass General Hospital Small-fiber Symptom Survey (MGH-SSS), as well as some other symptom assessments (Composite Autonomic Symptom Score-31, Short-Form Health Survey-36, and Short-Form McGill Pain Questionnaires), Oaklander compared FM patients with SFPN and without it. (The MGH-SSS survey assesses symptoms that could occur as a result of nerve damage in five different component parts of the body – gastrointestinal, somatosensory, miscellaneous, vascular, and neurological).

Fluorescent immunohistochemistry with confocal microscopy. The nerve axons or endings are in green. Healthy controls on the left, people with small nerve loss on the right. (From Scientific Advances in and Clinical Approaches
to Small-Fiber Polyneuropathy
A Review – JAMA)
Some differences were found, but overlapping symptoms were the main theme. FM patients with and without SFPN had similar pain levels. Only one of the five components of the Small Nerve Fiber Symptom Survey stood out in the SFPN patients: the vascular component. It included the following symptoms: “Skin with unusual color or changes in color,” ”Less hair growth on lower legs or feet,” “Changed pattern of sweating on body,” “Swelling in hands or feet,” and “Skin that itches for no reason.” One other symptom – tingling sensations – was increased in FM patients with SFPN as well.
When the researchers flipped the experiment around and tried to predict which patient fit in which disease category, they found that using symptoms to diagnose patients provided only a “fair predictive value”.
The authors acknowledged that the results could have been confounded because some people with SFPN may have had negative skin biopsies and autonomic testing results: i.e. they could have had undiagnosed SFPN. (One punch skin biopsy would hardly seem to be a comprehensive test of a small fiber problem that might be able to affect everything from the vascular system to the gut to the skin.)
So, while a few symptoms of SFPN may be somewhat predictive, the study found that most of the symptoms in FM and SFPN appear to be very similar. Acknowledging that the study size was small – and that its results were preliminary – a couple of possibilities arise:
- Two Separate Diseases – SFPN and fibromyalgia are two separate diseases which just happen to produce a very similar symptom presentation.
- FM is SFPN – Perhaps because we’re not testing for SFPN in some of the places it’s found – such as the gut or vascular system – the current tests for SFPN (skin biopsies, autonomic nervous system tests) miss a lot of SFPN; i.e. FM is SFPN – and we just don’t know that yet.
- SFPN isn’t really a big deal in FM. Clauw has proposed that it’s a kind of add-on issue that isn’t contributing much to the symptoms that FM patient have. Instead, upregulated pain producing pathways in the central nervous system (central sensitization) are producing the vast majority of symptoms in FM. Given that, it made sense that FM patients with and without SFPN would have mostly similar symptoms. Clauw has suggested that central sensitization may be actually causing SFPN in FM.
The Gist
- Small fiber polyneuropathy (SFPN) refers to damaged or missing small nerve fibers that relay sensory and/or autonomic signals.
- These small nerves are long, mostly unmyelinated, fragile nerves that can be easily disturbed.
- Most descriptions of SFPN describe symptoms like tingling, numbness, electric shocks and pain.
- Dr. Anne Oaklander, though, believes SFPN could be producing just about every symptom found in FM and ME/CFS. She believes that only about 10% of SFPN cases may be diagnosed.
- Another study found that people with SFPN in the skin always tended to have SFPN in the nerves surrounding the blood vessels. The nerve problems around the blood vessels could be impeding blood flows to the muscles – causing the muscle and fatigue problems after exertion.
- Some people who did not have SFPN in their skin did have nerve fiber losses around their blood vessels. That indicated that skin biopsies may miss some people with small nerve fiber problems elsewhere in their body.
- The good news is that if the small nerve fibers are damaged, they can grow back. Dr. Oaklander suspects inflammation is the cause behind the SFPN in FM. Treatment options are limited and need more study but steroids or IVIG can help. Because steroids are cost-effective and may be helpful, Oaklander strongly recommends more studies of steroids.
Review Article
In a recent Journal of the American Medical Association review article “Scientific Advances in and Clinical Approaches to Small-Fiber Polyneuropathy A Review” , Oaklander and Nolano asserted SFPN is much more common that we think. They believe only 10% of SFPN cases have diagnosed.
The small nerve fibers that are affected in SFPN, it turns out, are very thin, are spread out over long distances, and most are not myelinated; in short – they’re very fragile – and can be injured in a number of ways.
Many conditions can damage them: pathogens, diabetes, autoimmunity (particularly Sjogren’s Syndrome), alcohol abuse, chemotherapy, antiretroviral HIV drugs, colchicine, vitamin B6, metronidazole, nitrofurantoin, fluoroquinolones, and arsenic, Ehlers-Danlos syndrome, ion channelopathies…
Nature appears to have compensated for the small nerves fragility, though, by giving them a unique nerve superpower: given the right conditions, they can regrow.
They’re involved in a number of systems implicated in FM and ME/CFS: the somatosensory (sensory), motor (movement), and autonomic (fight/flight/rest/digest) systems and they also help regulate the immune system. Their purpose – monitoring the internal and external environments for danger and responding with sensations such as pain which trigger both “conscious and involuntary evasive maneuvers” – sounds like a process, which if it went awry, could set one’s systems on edge in a very FM and ME/CFS-like way.
Their ubiquity suggests SFN as the potential to produce a wide variety of symptoms. Note, though, that the classic descriptions of SFN mention only a few symptoms (pins-and-needles, pricks, tingling and numbness, burning pain, coldness and electric shock-like, brief, painful sensations.)
In what would constitute a kind of paradigm shift for this field, Oaklander and Nalono assert, though, that SFPN can also cause deep aching, fatigue, post-exertional malaise, heart racing (postural orthostatic tachycardia syndrome (POTS)), and the gut and sweating issues that many of us are familiar with. They also believe that doctors also get hoodwinked by believing that SFPN is associated with stocking-and-glove presentation (symptoms first appear in the feet and hands) – which is not always the case in FM.
The authors propose that damaged small nerve fibers leading to the spinal cord could be producing the chronic, long-term “potentiation” of pain signals (that process begins in the spinal cord) which results in pain amplification in FM. Pointing to a Sjogren’s Syndrome study, they proposed that SFPN could even be causing cognitive problems found in ME/CFS/FM.
SFPN in the Blood Vessels = ME/CFS?
Oaklander, and David Systrom believe small fiber neuropathy may be producing something called “neuropathic microvasculopathy” in chronic fatigue syndrome (ME/CFS) and fibromyalgia. This occurs when small fiber loss in the shunts (the arteriovenous anastomosis) between the arteries and the veins in the skeletal muscles results in the blood bypassing the capillaries (and the working muscles) and going straight into the venules. In other words, the exercising muscles get little blood, while most of it goes straight into the veins where it is returned to the heart.
One wonders if a study, four years ago, with the engaging title, “Myovascular Innervation”: Axon Loss in Small Fiber Neuropathies“, may someday be described as a seminal paper. The authors speculated that damage to small nerves surrounding the blood vessels was also present in FM patients with SFPN, and produced the first study to demonstrate that.
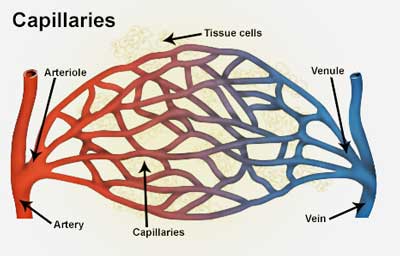
Arteries, arterioles and capillaries. Could small nerve loss near the blood vessels be stopping blood from getting to the muscles?
They found that reduced levels of the small nerves around the blood vessels (myovascular degeneration) were correlated with reduced small nerve levels in the skin: i.e. the small nerve loss in the FM patients extended from the skin to their blood vessels.
This suggested that Oaklander, Systrom and others were right when they suggested that the small nerve fiber loss seen in FM and ME/CFS is likely present in other parts of the body. Depending on where the small nerve fiber loss is, of course, opens the door to production of many different symptoms.
Perhaps just as importantly, the study found also that some FM patients with reduced levels of small nerves around their blood vessels had normal small nerve levels in their skin. That suggests that the skin biopsy results – which most doctors rely on – are not necessarily indicative of what’s happening elsewhere in your body: even if you have a negative skin biopsy, your small nerves could be getting whacked somewhere else in your body.
This, of course, suggests that the 50% or so of FM with documented SFPN might be an undercount. This was just a small preliminary study but it suggested that more people with FM may have SFPN than we suspect.
Patients with small nerve loss around their blood vessels – but not in their skin – tended to experience muscle pain, stiffness, or cramps – which were worsened by activity (post-exertional malaise) and autonomic symptoms. Symptoms like numbness or sensory loss, on the other hand, were rarely found.
Unfortunately, this small study has not yet been followed up on, and needs validation, but the interest in SFPN in heating up. Two recent papers highlighted the role that SFPN may play in ME/CFS and/or POTS and other diseases. (Blogs on those are coming up.) Time will tell how far the SFPN saga in ME/CFS, FM, POTS, etc. plays out.
Diagnosis and Treatment
Oaklander and Nolano reported that several symptom assessment tools are available including the SFN specific Rasch-built overall disability scale, the Small-Fiber Symptom Survey, the Utah Early Neuropathy Scale, and most prominently, the Massachusetts General Neuropathy Exam Tool (MAGNET).
Small fiber polyneuropathy is usually diagnosed using an easy-to-access 3mm skin biopsy. The authors report, though, that the field is still evolving and that the norms to assess SFN that many laboratories use are not representative, and may lead to false negatives. Sampling error (i.e. one biopsy may not be enough) is another issue.
The quantitative autonomic function testing regimen developed at the Mayo Clinic can help, but is available at few hospitals. In vivo corneal confocal microscopy, which visualizes the small nerve innervation of the cornea, is noninvasive – and appears to be a good bet – if you can find a doctor who can do it.
Immunotherapy – corticosteriods or IVIG – appears to be providing the best solutions, but larger trials are needed. Oaklander’s retrospective IVIG study was pretty darn successful with 75% of patients with SFPN getting relief.
Small Nerves – Big, Big Problem? Drug Trial Points Finger at Autoimmunity in Fibromyalgia and ME/CFS
From Neuropathy Commons







Thank you for this info, Cort. I have never fully believed that FM is the problem. I have loads of nerve pain served with two sides of autonomic & cognitive dysfunction. Have yet to find a neurologist that cares enough to get anything done. Been deemed “too complicated” for over a decade.
I believe this is all tied to acid sensing ion channels (1a and 3). Ischemia, lactate. Thoughts?
Right – the patients certainly paid for it. A generous contribution from our community. Let’s hope it really reaps dividends.
I just got diagnosed with Small fiber neuropathy with a three skin biopsies. Two years ago, a scum of a man hit us from behind at a very high speed because he fell asleep at the wheel. Immediately after, I developed shooting pain on every inch of my body. I went through probably 15 idiot doctors 5 of which were neurologists before finding my current neurologist who was willing to bet everything that I had SFN. She was right. Most neurologists have no clue about this and that is UNACCEPTABLE. How is that possible with SO MANY PEOPLETHAT HAVE DIABETES IN THE WORLD??? I DONT UNDERSTAND. DO SOMETHING ALREADY!!! I was only 27 years old when I got this from a car accident and it makes me contemplate suicide the pain, weird sensations, itchy head, bladder problems are SO bad!!!
Hey Kelly, I know your comment is from a couple of years ago. I really hope you are doing better now. I got SFN when I was 25, diagnosed at 27 it has been a struggle to say the least.
I just had to reply to echo your sentiment: how in the world do doctors not know of/ about SFN? And it’s even more unacceptable when neurologist
don’t know – which at least here in Germany seems to be the standard.
My partner said the other day when we were talking about my long and complicated history with docs and meds that he does not understand how neurologists just decided to not know and care about SFN at all. Like how is this possible? They just decided to not acknowledge much less treat a disease with millions of sufferers which belongs to their specialty???
It is insane.
I hope there are better treatments for us in the future. All the best to you.
As I was reading your comment, I thought ….I wonder if the doctor was a woman? Glad you found a doctor who heard you’re voice! Hope someday to find myself one too!
Wow!! This is pretty amazing! Diagnosed with SFN 15 years ago.
I was complaining of electric type shock feelings in my legs when I first got sick, 40 years ago!
Ha. Those electric shock feelings! A recent paper suggested that an autoimmune reactions may be wiping out those nerves…
Not sure how possible it is to express how validating this information feels. I have been reluctant to say anything about the “painful electric shocks” that also cause the muscle to “jump,” (fire, spasm, myoclonus, whatever you want to call it.) It seemed to me, as ccx a disabled Physician Assistant, this might be seen as a conversion reaction, some somatoform disorder, or psychosis. It’s hard enough to be invalidated for everything else! And from day one, 5.5 years ago, (MY day which shall live in infamy. . .two weeks post viral infection,) I have had not only the above, (shocks accompanied by involuntary muscle jerks,) but stocking/glove pain in both hands and in both feet. I was taught there was no way that nerve distribution was possible. So there you go.
CORT THANK YOU
Well, Marti, I guess the diagnosis rate of SFPN may really be about 10%. This seems to be another kind of newish field. Neurologists know a lot more about large nerve neuropathy than small nerve neuropathy….
If you have a positive skin biopsy then IVIG might be a possibility or possibly steroids. Check this out – https://www.healthrising.org/blog/2017/12/13/small-nerves-fibromyalgia-chronic-fatigue-ivig-autoimmunity/
I want to reply to what Marti wrote. My ME/CFS began after a virus that landed me in hospital for 3 weeks. I have been fighting my way back for 2.5 years. I have made significant progress from being bed bound for months. I too have these weird muscle twitches, leg jolts and I want to pull my arm off as it drives me crazy and gets worse when I crash. I have said no to the antidepressants and sleeping pills and work with a wonderful Naturopath. My brain fog is terrible today so I am trying to understand the implications of the above article. It does make me feel beter that this is not all just in my head. I am also having pain in shoulders and my ellbows. What does it mean for us?
I’ve had those electric shocks in my brain, it’s like to hot wires meeting each other, it gives a jolt to the body. it’s been a long time since I researched that , it is nerve fibers that have broken making new connections and not to the old connection, been to long since I researched all that, I’ll try to go back and refresh my memory for using the correct terms to use here.
Synapses, neurons
Cort, can you please read my comments at the bottom , I am at a very dangerous state with my diseases and I dont know where to go next. thank you.
the article you quoted from WAPO is by Will Schwalbe. a writer and editor.
I have been in touch with Dr. Oaklander. She’s a dynamo but I’m not sure she gives any credence to the viral component of ME/CFS, which, I believe is significant.
I’m glad you posted this piece. I do believe there is a relationship here to be explored. I have had ME/CFS for 40 years. My brother had SFPN which got so painful, he had to end his life. (He had another painful condition) He left some money to Dr. Oaklander.
Sorry to hear about your brother! That was a great article – highly recommended reading. It illustrated how devastating SFPN can be. After reading what Schwable has gone through it became really clear that anything which messes with the nerves has the potential to be really bad news.
There is no doubt of that. But looking at the inflammatory side of it, it is “driven” by interleukins 6 and 8. IL-8 seems to cause the neural hypersensitivity. IL-6 and 8 both part of the immune response in IBS, and IL-8 found in blastocystis, dientamoeba and helicobacter. The puzzle pieces are coming together.
Would LDN help with SFPN?
My daughter and I were diagnosed with FM and then later with SFPN. I have been on LDN for a couple of months and it has made a huge difference in my quality of life.
Did the LDN reduce the pain?
Hello Joy what is LDN?
Ive been given the diagnosis FM which I cant accept. I tick every box here and my pain is so severe sometimes I cant walk. My life is a daily struggle and I think Doctors start to think there is a mentsl issue when you question a diagnosis.
LDN is low dose Naltrexone. is being used as a regulator of the immune system, providing relief to patients with autoimmune diseases, and central nervous system disorders.
https://www.ldnscience.org/ldn/what-is-ldn-used-for
I have taken LDN for SFN for over a year along with gabapentin, amitriptyline, tumeric, fish oil pills, lipoic acid, Acetyl L-carnitine… none these work great. I have small periods when I feel a little better, but the pain always comes back. I wish LDN helped more… in fact I’m thinkingabout stoppi ng it. But you should think about trying it out, everyone is different
Good article, Cort. Thanks.
It’s worth re-emphasizing that Oaklander’s research has not yet been universally accepted among neurologists.
I know from personal experience that many neurologists still believe that the symptoms of small fiber neuropathy are limited almost entirely to painful and tingling skin sensations, usually starting in the feet and potentially progressing up the leg. These neurologists don’t believe, at least at this point, that small fiber neuropathy causes a wider array of debilitating symptoms in other organ systems, as Oaklander does.
So as a warning to uninitiated ME/CFS and fibromyalgia patients, do not set your hopes too high that a visit to a neurologist will lead to a skin biopsy and potentially a lot of answers and validation. Oaklander’s research is best thought of as an emerging field of research. At this point, it seems that a lot of neurologists either are unaware of it or remain unconvinced by it.
I’m sure that it is not!
She’s trying to create a kind of paradigm change in the field. That was why I thought the finding of small fiber neuropathy in the blood vessels of people with (and without) SFPN was so intriguing. That study was a first of its kind as well – and so it needs to be validated as well.
Thanks for the warning (I added a few more cautionary notes) – this really is an emerging field of research. Time will tell how it all turns out.
Think it is interesting and intriguing an eye dr. can see it or dx it that way, too! Hmm..might have to talk to my eye dr. about it!
Thankx, Cort!
My husband got diagnosed at a major University medical center. He had been to local neurologists and they just don’t have the knowledge or ability to do the testing. I recommend that anyone who wants to be tested seeks out a neurologist at a University medical center who has experience with it.
Thanks so much for this information. 25 yrs with fibromyalgia.
It is just so good to read something new that I haven’t heard before. It gives me hope even if not for myself but others.
WE NEED MORE FUNDING FOR RESEARCH!!
MJ
That is really the bottom line. At about $1 per year per patient FM may be the worst funded major disease there is – and much of funding from the NIH when I last looked was going into behavioral research.
Another treatment path may be in addressing something mentioned in one of your earlier articles Cort, a BH4 deficiency – namely, using Kuvan.
https://www.healthrising.org/blog/2014/09/25/dopamine-basal-ganglia-chronic-fatigue-syndrome-treatments/
Question is, what is the hen and what is the egg really … Small fibre neuropathy occurs in many diseases. What is the cause for small fibre neuropathy? Or what is the cause of fibomyalgia or for ME/CFS? Is SFN caused by metabolic disease or does SFN cause problems with the metabolic system? Etc, etc.
I guess we do not know, or rather the researchers dont know – yet. Another thing is that it probably can be both ways at the same time. No doubt it is there, SFN, though. And maybe sometimes it is the only cause.
Interesting field of research though. Almost happy to have been unvoluntarily drawn into it 😉 .
That is the big question….Are the small nerve fiber problems really found throughout the body in ME/CFS and FM? If they are then that would make them distinct from the SFN found in diabetes and other diseases. Then again if I remember correctly the small nerve problems in FM are distinct – the nerves are both disappearing and getting smaller.
On the other hand Dr. Clauw appeared to make a pretty interesting case that the central sensitization problems in the brain could be whacking the small nerves in an attempt to stop the flow of pain producing nerve signals….
And then again don’t mix sfn with polyneuropathy! Diabetics often have polyneuropathy. It’s a mess! ;D
And in the research of FM they have found another painsystem, beside nerves. I do not remember much, but it is interesting.
Could a limbic system problem theoretically cause SNF? Any thought on that?
I don’t know if the limbic system has been proposed but other parts of the brain such as the insula has:
“They proposed that hyperactivity in the insula is producing such strong pain sensations that the body was effectively burning out the nerves in the periphery in an attempt to stop them.”
“The authors presented two possibilities: the peripheral nervous system “reorganization” to stop the flow of sensory stimuli to an already overheated brain; and the possibility that the alterations in the insula – a major autonomic nervous system regulator – could be impacting the small autonomic nervous system fibers found in conjunction with the sensory nerve fibers in the skin.”
https://www.healthrising.org/blog/2019/08/12/brain-small-fiber-neuropathy-fibromyalgia-chronic-fatigue/
Good to see this ‘out there’. It has taken me 50 years of ICC ME to get a proper punch biopsy this January which is highly positive for SFPN. That is just the start. Subsequently I’ve had heaps more blood tests (even more than those normally scheduled by Oaklander) which have revealed certain observations, a possible potassium channelopathy being one and having to rule out Fabry Disease using genetic testing (which I’m trying to organise but a pandemic has inconveniently got in the way) being another. I’m in the UK and have had to self fund all of this. In fact I was turned down for a punch biopsy by my local ‘SFPN Expert’ on the basis that ‘people like you aren’t positive so we don’t test you’ (!!!). Clearly I had to find a neurologist who was better educated! This amounts, thus far, to about £9000 worth of testing. I have little expectation of the Fabry test being positive, but properly interrogating this stuff should be ordered by our medics as the default of good medicine. Having to be my own physician is wearing and expensive.
Good for you Lilpink! So much for the local SFPN (people like you! ). Good luck and please keep us informed how it all turns out. I imagine that you’re opening minds over there.
If only that were true! It feels like walking through treacle!
My husband was diagnosed with SFN last year, after a lifetime of pain and other mysterious symptoms. Getting diagnosed is great because you finally know you’re not imagining things.
Then, you get tested for all of the possible causes. If they find something, it can range from something that is easy to treat (like a B6 overload or B12 deficiency) to something that is harder to treat (like some of the autoimmune causes).
Then there is the other category, “idiopathic,” which basically means they have no idea what’s causing it, and therefore, no idea how to treat it. This is where he ended up. So, you’re left with damaged nerves, no treatment, and only pain medications that may or may not help at all.
It’s certainly hopeful to have moved from not knowing IF there was something that could be diagnosed (the SFN itself,) to knowing that there is, and that at least there is good research going on. However, it’s rather disheartening to be back at square one when the doctor says we have no idea what’s causing it and nothing to offer you as far as treatment.
Still, I encourage everyone to get tested for it if you can get it covered by your insurance. If you do get diagnosed find a cause, there may be things you can do to recover or improve.
The lack of treatment options is disturbing. I can’t but imagine that there’s work being done to improve that. With regard to ME/CFS and FM – in order to come up with a good treatment I imagine that knowing the cause – whether it’s inflammation or something else will be critical. Hopefully studies will uncover that.
I was always so embarrassed during PT for various pain issues over many years, when my muscles would “jump”. Like an electrical impulse or current. I still have this, and have never mentioned it to my MD. The neurologists in my area leave much to be desired. Testing reflexes (mine are ok) is all they have ever done.
Thank you for expanding on SFN, Cort. I didn’t know that there is evidence that the nerve issues could be unevenly distributed within the body. For several years now, the Ehlers-Danlos community has been aware that up to 50% will test positive for SFN–which has always made sense to me because so many of us have ‘fibromyalgia-like’ symptoms as well as the usual EDS stuff.
Unfortunately, many of my zebra friends who have gotten this diagnosis, haven’t gotten much effective treatment (excepting pain meds such as gabapentin or if lucky, some sort of opioid). The doctors really don’t know what to do with it. You mentioned corticosteroids, and just a few days ago I read an article about yet more problems associated with their use. As far as IVIG goes, there is always the (big) problem of getting insurance to pay.
Myself, with achalasia of the esophagus where all the nerve fibers involved in peristalsis die off, which is thought to be autoimmune, I do wonder if there is any similarity to developing SFN in the rest of the body.
Now, on something completely different, and wanting to share it with you, my friend forwarded me this VERY interesting article about how viral fragments might be an underlying cause of ME/CFS. Sorry this is off topic, but I don’t know how else to get it to you;
https://www.clinicalpainadvisor.com/home/topics/general-pain/chronic-fatigue-syndrome-viruses-and-the-innate-immune-system/
Ha. Thomas Henderson – that is good to see. I did a blog on him for Simmaron a couple of years ago.
http://simmaronresearch.com/2014/09/treatment-resistant-depression-chronic-fatigue-syndrome-child-psychiatrist-finds-success-antivirals/
Thanks for passing that on 🙂
What goes around, comes around. Thanks for alerting me to that 2014 blog you wrote. I have only been reading your blogs for a couple of years, so I missed that one!
Seems as if certain research areas get picked up and then forgotten and then picked up again when new questions/information appear. The ‘something’ which signals cells to be turned off and on again sounds similar to what Ron Davis has mentioned (a yet unidentified factor in the blood serum).
I’m surprised that Stanford has not mentioned Montoya’s antiviral trial so they have probably concluded that it isn’t worth trying again. Poor Stanford–so far no new ideas of what to do with us… ;-(
Do you know of any other research which as pursued using long term antivirals with success? (Bonus points–could be useful for Covid ‘long haulers).
P.S. Here’s the link to some additional corticosteroid side effects; https://www.medpagetoday.com/primarycare/generalprimarycare/87422
Double thanks, Nancy B!!
Great article by Theodore with useful diagram.
He also explains work that
Prusty and colleages have done.
Favorite statment in article:
“Therefore, this protocol could serve as a new
quantifiable, nonsubjective, and therefore inarguable
test for CFS/ME, representing a major step forward for
the treatment and research in this neglected disease.”
anyone interested in Prusty’s work, i see he shares some of his thoughts on twitter:
https://mobile.twitter.com/bhupeshprusty?lang=en
I don’t buy this at all.
Cort (or anyone knowledgeable) is there anything that links SFPN and MCAS? My bone pain, neuropathy pain, vertigo and brain fog were all drastically reduced once I started treatment for MCAS. Treatment consisting mostly of H1, H2, and Neuroprotek…
As I remember the review article by Oaklander in the blog did mention mast cell activation amongst other things that could spark SFPN. There’s a case history too –
Case 71: Small Fiber Neuropathy, Postural Tachycardia, and Mast Cell Activation Syndrome
Chapter:Case 71: Small Fiber Neuropathy, Postural Tachycardia, and Mast Cell Activation SyndromeAuthor(s):Peter NovakDOI:10.1093/med/9780190889227.003.0076
The patient has history of mast cell activation syndrome (MCAS) in which mast cells inappropriately release active substances including leukotriene and histamines, triggering symptoms of flushing and orthostatic intolerance. Small fiber neuropathy was length-dependent, mild, affecting predominantly sensory fibers. Tilt test showed postural tachycardia syndrome (POTS).
https://oxfordmedicine.com/view/10.1093/med/9780190889227.001.0001/med-9780190889227-chapter-76
Mast cells are able to tweak the nerve endings – so it looks like there is a possible connection – which is not surprising given that all the mast cells are purported to do
is the sfn more for FM or for me/CFS?
that I did not understood.
It was first found in FM quite a while ag and has been documented repeatedly there. Only recently have we heard that it’s apparently just as common in ME/CFS. We are waiting for the first paper to come out on that, though.
Hello Joy what is LDN?
Ive been given the diagnosis FM which I cant accept. I tick every box here and my pain is so severe sometimes I cant walk. My life is a daily struggle and I think Doctors start to think there is a mentsl issue when you question a diagnosis.
LDN is Low Dose Naltrexone. A compound medication used for pain.
Thank you for this blog. I went to a ME specialist after falling acutely ill overnight and she told me that she didn’t think I had ME, but instead she diagnosed me with autoimmune small fiber neuropathy and recommended IVIG.
I was uncertain because it didn’t seem to fully explain the severity of my cognitive impairment (couldn’t read, write, speak) and profound muscle weakness (couldn’t lift a fork), but your article helps better explain those symptoms.
Insurance came on board when Stanford and UCSF neurologists recommended same treatment after my lumbar puncture showed autoimmune inflammation. Interestingly, there are lots of people in my IVIG group receiving the infusion for POTs and SFN. Some had to appeal insurance denials but it certainly seems like it is becoming more of a mainstream treatment.
Six months of IVIG and I’m making some progress, but it is maddeningly slow. I was told that peripheral nerves take longer to regenerate than nerves in the central nervous system. I actually think my cognitive function is improving faster than my autonomic dysfunction.
Mestinon and steroids have also helped immensely.
Your ME specialist was on the top of her game. Autoimmune small fiber neuropathy hasn’t gotten around that much. Interesting, but I suppose not surprising, that it’s being found in POTS as well.
Finding the right doctor to do the right tests if obviously really important.
Thanks for sharing your story and good luck with the IVIG. I hope it will kick in and those nerves will start to regrow.
Hi Charlotte,
I know this is an older post at this point, but where did you get your infusions? I was diagnosed with small fiber neuropathy and POTS at Stanford. The SFN diagnosis includes autonomic neuropathy and was initially diagnosed as autoimmune in nature, but my doctor has told me repeatedly that my insurance will likely not cover IVIG and there is no evidence the treatment will work, so we have never even attempted to get it (despite failing well over 30 medication trials for SFN, autonomic symptoms, POTS, MCAS, etc.). I am pushing my doctor on IVIG again, so any information would help. Thank you.
The challenge with ME/CFS is that over time, the symptoms can change. When I was first diagnosed in 1984, I had head ringing, Multiple Chemical Sensitivity; reactions to almost everything that hadn’t bothered me before and chronic infections of one kind of the other. But, the worst symptoms were the horrific headaches that could sometimes last three days. Then one blessed day, the headaches just disappeared. Unfortunately, they have been replaced with a weird coldness in the face and head that gets very intense around 3 in the afternoon. Pains that move from place to place have also become a thing. My balance is awful and I have fallen and broken my little toe three times, a finger and sprained my shoulder. I explored Mast Cell disorder and ended up almost killing myself when the meds they used to confirm that condition triggered narrow angle glaucoma and then a caratoid cavernous fistula that required a 7 hour brain operation. I nearly lost my right leg when a tiny cut became infected and spread into neighboring tissue (cellulitis). It took 3 months to resolve and I have a dreadful scar to remind me. Maybe my case is different, but I don’t think small fiber neuropathy could explain all these symptoms.
Betty, you mentioned that you had pains that move from place to place. That could very well be lyme disease. It is a symptom of lyme disease.
It seems that having cfs immune problems makes one more likely to get lyme disease and it also seems that having lyme disease can lead to getting cfs.
Someone on phoenix rising recently mentioned he thought that taking neem long term was a good idea until a treatment is available. Provided it is non toxic I suppose.
it probably has broad based anti bacterial anti parasitic and i would not be surprised anti- lyme properties, until the medical community can come forward with some kind of treatment. If is helps the immune system protect against lyme, etc. it might be a good idea.
I thought it was said by someone at OMF last year that they hoped to have a treatment to suggest this fall.
Hello,
I really enjoy this web site. The information is so helpful in so many areas. I was wondering if I could ask a question? I recently spent a week with my family in a nice beachfront home with a pool and hot tub with great jets. I had been taken lots of pain medication for my CFS, but while I was there, I only needed 1 pill for the whole trip. So I am asking myself why, why, why??? I would be interested in anyone’s thoughts about this in our community. Thanks so much.
Fibromyaglia and SFPN/SFN are not the same thing. I have both, the SFPN/SFN involves the nose to brain, the trigiminal nerves, the crainial nerves, the CNS the PNS.
FM involves the pressure points, SFN doesnt. Dr. Nancy Klimas and her team in setting on top of this right now.
FM goes with ME/CFS, SFN involves inhalation, nose, sinuses , olfactory, brain.
Im sick from 2 very bad mold home exposures 20+ years ago with a 3rd one to top it off 5 years ago. several years ago a doctor prescribed a steroid nasal spray, I knew steroids caused bad reaction but hadn’t tried it up the nose and I was kind of disperate for some relief so I tried it, my face around my nose and top of my mouth/gums, area instantly burned, it went straight to my brain and then I felt it as it started going down my body to my finger tips and toes, on fire! it last 5 days while the brain effects took over a month to mellow out, back to where I was before I tried the steroid nasal spray. quite a miserable time, everytime I have a bad inhalation exposure it does the same thing.
With my first moldy home exposure it was mainly Stachy and Fusarium, my fibromyalgia was severe in that home, my spinal cords were inflammed and the two pressure point in my lower back where the buttock starts were knots because it was so bad, I had like stiff man walking syndrome, it radiated down the back of my legs and up my spine and pretty much set across my shoulder and the pressure was on my BBB that no doubt had to be leaky, the 2nd moldy house that pain went away and I believe it did because at that point I had spinal fluid coming out the nose and ears and I suffered TBI. it wasn’t until after the 2nd exposure that this SFPN/SFN NERVE DAMAGE IN THE BRAIN became something I had to deal with anytime I got re-exposed because of a toxic exposure. I have known for a long time it involved the trigeminal nerves and the brain, I have waited forever for the study this to be recognised. now my FM is pretty under control, sometimes if I’m having a more chronic exposure it will get painful again but with those never ending inhalation exposures that also cause my palms and the bottom of my feet to burn along with with the SFPN/SFN, nose to brain effects without it affecting my FM, I know they are seperate and have for a long time. excuse spelling and all that please, I have not bothered to retrain my brain on that or math that I use to be so good at before my TBI from moldy home exposures, it was 6 years after that 2nd moldy home before I could even manage to function to get online and I got in the sick building syndrome group where I than became the researcher because I knew how to keywords , many years there, I’ve posted my research many places, I use to share my research with Dr, Thrasher in the group and after I left the group. some would likely know me as osisposis. I haven’t been doing to great since the 3rd exposure 5 years ago, big set back 🙁 I’m now at a very scary stage because where I live and the hospital with the clinic tied together and my primary doctor just retiring and my cancer doctor getting ready to retire and none of them will recognize me/cfs and hardly FM and the most the cancer team would do in write in my medical records that I likely had SFPN , but no biopsy yet. I had breast cancer in a breast duct, estrogen, I would not have chemo because I’ve known for a long time that fungal fragments and mycotoxins set up home in damaged tissues in my body, I know chemo suppresses the immune system and always it fungal/mold to take over, now I know chemo also causes SFN and I would kill myself if it could possibly get worse, I cant take anymore, I cant take talking to brick walls anymore, and because once again I went to the ER because of a bad exposure that tore up my lungs and caused bad inflammation in my lungs and then sweating like crazy over it and again this pain lingered in my right lung and I caughed up blood, this time I rode in a ambulance, first time risking that enclosed ride with ent’s that still wear cologne and scented cloths and stiff, luckily it didn’t make things worse (my big fear) riding in the ambulance (not this time) so anyways because I taked to this ent during the ride about my disease light bulbs went off in his head. and I told him how the ER will treat me , just like they did last time for the same thing, take a lung xray, see nothing, accuse me of lying and being a druggy because I asked for something for pain, so anyways that ent had a few words with the staff this time and I heard some of it as he came out the door telling them to listen to me because I know alot more about my disease then they do. so anyways they decided to ultrasound my heart and check for blood clots and use me for training purposes, I asked 3 times, please ultrasound right there where my lung hurts, they finally did and waaalaaa a fungal nodule, they then cat scanned my lungs, more finding on bone, ribs, strotum, lesions growths, my daughter was setting woth me when the doctor came in fungal nodule, I made him repeat that. so come home and next day I get a call, appointment with this cancer doctor (god complex) that doesnt like me because I wouldn’t do the chemo with the breast cancer or the estrogen pills. doesn’t listen to me at all, so Iget in there to see her and she has desided my cancer is back and its in my lungs because I refused chemo and estrogen pills. mayo clinic found one of those fungal nodules in my stomach many years ago. I know there are others. my life is now on the line here, yes fungal nodules that get aggervated by high inflammation and bleed can turn to cancer but she is trying to say my breast can is back in my lungs and its all my fault, this cancer doctor who refuses to listen to me about my diseases. estrogen is also involved in my disease, my 1st moldy home exposure caused endermetreeosis and a hysderictomy. mycotoxins are endocrine disrupters! my life in on the line here. I am a mother and grandmother, I want to live and now I’m being forced to choose between the wrong medical help or just letting my disease kill me. a old friend said she would take me where I needed to go to get to some experts on my disease or even the NIH clincal trial on me/cfs. where can I go from here? I went to Dr. Shoemaker, Dr. Gray in AZ. and Dr. Montoya at stanford in Calf. all my medical records point straight to mold and my me/cfs and fm. please help where can I go, Dr. Nancy Klimas and her team probably understand the most about what I’m going through. again sorry for spelling and stuff.
I should also add that the 1st moldy home was more about it growing, drying and infiltrating my home with toxic mold dust vs. the 2nd moldy home being high moisture and aspergillus, penicalin, moldys that grow well in high moisture situations. and after the 2nd moldy home I moved back to my first moldy home and realized what was going on there with mold, and while back in that 1st home my FM got very bad again.
2020
Association of small-fiber polyneuropathy with three previously unassociated rare missense SCN9A variants
Mary A. Kelleya,b and Anne Louise Oaklandera,c
Diabetes is the most common cause of SFN in developed countries, with cancer chemotherapies and other toxic exposures also well recognized.
Many of these patients remain undiagnosed and untreated for years and in some instances for decades or throughout their entire lives.14–18 Evidencebased recommendations have been developed for blood test screening of patients with initially idiopathic small fiber neuropathy (iiSFN); a list is available at https://neuropathycommons.org/.19 Such screening identifies potential medical causes or contributors in nearly half of patients with iiSFN, and when a cause is identified it not only guides medical management but offers a welcome path forward to patients.
Because different types of small fibers express different arrays of neuropeptides and innervate many different types of cells, tissues, and organs, SFN typically presents with multiple symptoms. Its sensory symptoms include widespread neuropathic itch as well as chronic pain.4 Many organs can be affected by internal and autonomic SFN. The most common complaints are new difficulty performing usual activities (exertional intolerance and chronic fatigue), postural orthostatic hypotension and tachycardia (POTS),5 postprandial bloating or nausea, diarrhea and/or constipation (irritable bowel),6 urological complaints, and chronic daily headache.7 Patients with SFN often become disabled. If they receive inadequate validation, guidance, or treatment, it can leave them confused, frightened, and often depressed. SFN can have devastating psychological, economic, and quality-of-life consequences. At least some of the consequences of SFN can be mitigated by informed, compassionate caregivers. Recent reviews and the expected 2020 publication of the first global consensus case definition of SFN are increasing its visibility.1,8 This case definition and diagnostic criteria for “definite,” “probable,” and “possible” cases, although intended for research use, will inform medical practice as well.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7384751/
SFPN/SFN SMALL FIBER POLY NEUROPATHY/SMALL FIBER NEUROPATHY
Diabetes is the most common cause of SFN in developed countries,
with cancer chemotherapies and other toxic exposures also well recognized.
SFN, severe paroxysmal burning pain in the hands and feet !!!!!
Eur J Paediatr Neurol
. 2020 Sep;28:198-204. doi: 10.1016/j.ejpn.2020.06.004. Epub 2020 Jul 7.
Acute monophasic erythromelalgia pain in five children diagnosed as small-fiber neuropathy
Nicole Faignart 1, Karine Nguyen 2, Cindy Soroken 3, Claudia Poloni 4, Heather M Downs 5, Bernard Laubscher 6, Christian Korff 3, Anne Louise Oaklander 7, Eliane Roulet Perez 8
Affiliations expand
PMID: 32723684 DOI: 10.1016/j.ejpn.2020.06.004
Abstract
The small-fiber polyneuropathies (SFN) are a class of diseases in which the small thin myelinated (Aδ) and/or unmyelinated (C) fibers within peripheral nerves malfunction and can degenerate. SFN usually begins in the farthest, most-vulnerable axons, so distal neuropathic pain and symptoms from microvascular dysregulation are common. It is well known in adults, e.g. from diabetes, human immunodeficiency virus, or neurotoxins, but considered extremely rare in children, linked mostly with pathogenic genetic variants in voltage-gated sodium channels. However, increasing evidence suggests that pediatric SFN is not rare, and that dysimmunity is the most common cause. Because most pediatric neurologists are unfamiliar with SFN, we report the diagnosis and management of 5 Swiss children, aged 6-11y, who presented with severe paroxysmal burning pain in the hands and feet temporarily relieved by cooling-the erythromelalgia presentation. Medical evaluations revealed autoimmune diseases in 3 families and 3/5 had preceding or concomitant infections. The standard diagnostic test (PGP9.5-immunolabeled lower-leg skin biopsy) confirmed SFN diagnoses in 3/4, and autonomic function testing (AFT) was abnormal in 2/3. Blood testing for etiology was unrevealing, including genetic testing in 3. Paracetamol and ibuprofen were ineffective. Two children responded to gabapentin plus mexiletine, one to carbamazepine, two to mexiletine plus immunotherapy (methylprednisolone/IVIg). All recovered within 6 months, remaining well for years. These monophasic tempos and therapeutic responses are most consistent with acute post-infectious immune-mediated causality akin to Guillain-Barré large-fiber polyneuropathy. Skin biopsy and AFT for SFN, neuropathic-pain medications and immunotherapy should be considered for acute sporadic pediatric erythromelalgia.
Keywords: Acute; Child; Dysimmune; Erythromelalgia; Monophasic; Small-fiber neuropathy.
https://pubmed.ncbi.nlm.nih.gov/32723684/
————————————-
Muscle Nerve
. 2018 Nov;58(5):625-630. doi: 10.1002/mus.26131. Epub 2018 Apr 26.
Fibromyalgia syndrome and small fiber, early or mild sensory polyneuropathy
Victoria H Lawson 1, Jessie Grewal 2, Kevin V Hackshaw 3, Phillip C Mongiovi 4, Amro M Stino 2
Affiliations expand
PMID: 29572887 PMCID: PMC6283273 DOI: 10.1002/mus.26131
Free PMC article
https://pubmed.ncbi.nlm.nih.gov/29572887/
Pain Med
. 2019 Mar 1;20(3):521-527. doi: 10.1093/pm/pny001.
Small Fiber Polyneuropathy Is Prevalent in Patients Experiencing Complex Chronic Pelvic Pain
https://pubmed.ncbi.nlm.nih.gov/29447372/
Review J Pain Res
. 2019 May 8;12:1447-1456. doi: 10.2147/JPR.S197667. eCollection 2019.
Research on central sensitization of endometriosis-associated pain: a systematic review of the literature
Ping Zheng 1, Wen Zhang 1, Jinhua Leng 1, Jinghe Lang 1
Affiliations expand
PMID: 31190954 PMCID: PMC6514255 DOI: 10.2147/JPR.S197667
Free PMC article
https://pubmed.ncbi.nlm.nih.gov/31190954/
Home / Allergy and Asthma Proceedings, Volume 31, Number 3
logo
Relationships among rhinitis, fibromyalgia, and chronic fatigue
Authors: Baraniuk, James N.; Zheng, Yin
DOI: https://doi.org/10.2500/aap.2010.31.3311
New information about the pathophysiology of idiopathic nonallergic rhinopathy indicates a high prevalence in chronic fatigue syndrome (CFS). This article shows the relevance of CFS and allied disorders to allergy practice. CFS has significant overlap with systemic hyperalgesia (fibromyalgia), autonomic dysfunction (irritable bowel syndrome and migraine headaches), sensory hypersensitivity (dyspnea; congestion; rhinorrhea; and appreciation of visceral nociception in the esophagus, gastrointestinal tract, bladder, and other organs), and central nervous system maladaptations (central sensitization) recorded by functional magnetic resonance imaging (fMRI). Neurological dysfunction may account for the overlap of CFS with idiopathic nonallergic rhinopathy. Scientific advances are in fMRI, nociceptive sensor expression, and, potentially, infection with xenotropic murine leukemia-related virus provide additional insights to novel pathophysiological mechanisms of the “functional” complaints of these patients that are mistakenly interpreted as allergic syndromes. As allergists, we must accept the clinical challenges posed by these complex patients and provide proper diagnoses, assurance, and optimum care even though current treatment algorithms are lacking.
https://www.ingentaconnect.com/content/ocean/aap/2010/00000031/00000003/art00002
FULL TEXT
https://afmr.org/abstracts/2012/Eastern/P13.cgi
Surprise Gene Finding Could Give Pathogens and Toxins a Leg Up in ME/CFS
by Cort Johnson | Jul 11, 2020 | Homepage, Neuroinflammation, Pathogens, Small Fiber Neuropathy
https://www.healthrising.org/blog/2020/07/11/mucosal-genes-chronic-fatigue-syndrome/
Travis Craddock heads Dr. Klimas’s biocomputational modeling team at the Institute for Neuroimmune Medicine (INIM) at Nova Southeastern University. MY HERO’S !!!
Thanks Jeanie!
I finally have a full body cat scan and brain scan set up by this hospital, my cancer doctor for Tuesday, I’m scared to even let them do that now, my cancer doctor who is on the verge of retiring seems to not care as much about me as she cares about being right. after 6 emails about my disease and what happened in the ER and with seeing her and what she wrote in my medical records making me look like a liar and changing the fungal nodule to just nodule, she actually sent the cat scan of my lungs to the biopsy place and they called to set up a appointment to have biopsies of my lungs when it was agreed that we would do these full body and brain scans first and see what might be safer to biopsy. 🙁 I cant take all this anymore.
3 years ago I had the breast can, first they said it was slow growing and had been there a long time, then that cancer doctor said it was fast growing and if I didn’t take those estrogen pill it would come back fast and hard. 3 years and the cancer hasn’t returned in my right breast but not it’s supposedly spread to my lungs, I don’t believe that, not for a minute. I have known since the 2nd moldy home exposure that my mucosal linings were damaged in that 2nd house, I passed a glob of it in the stool, I caughed up like a gallon of moldy colored mucus and whatever else out of my lungs after that 2nd. exposure. with the first exposure I had a stuffy nose alot when that long term low dose exposure to toxic dust started adding up in my home. in my medical records at that time I complained about my teeth and hair and everything felling dirty again right after I showed and brushed my teeth, the dust in my house at that point was black. the 1st. moldy home exposure affected me differently then the 2nd and 3rd moldy home exposure and they both wre high moisture situations. in the Phonixrising group there are pictures of the palms of my hands beet red, I think, I know I posted a picture of the cataract I got in both eyes from the 2nd moldy home, it shined green in the dark when lights shined on it, leaky eyes, the same green color that coated all my belongings in that 2nd. moldy home.
Hello! Do you know if they make any plugins to safeguard against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any suggestions?