Naltrexone is mostly used to help people addicted to opioid drugs safely withdraw from them, but LDN is used for a far different purpose. By temporarily blocking opioid receptors, LDN, in effect, unleashes them – causing a rebound effect and an increase in the production of the body’s endogenous opioids which reduces pain levels. LDN may also be able to inhibit microglial activity and thus reduce neuroinflammation.
LDN was pursued in FM because of its potential pain-relieving (those opioid receptors) properties but the fatigue, found in ME/CFS, however, is another matter. While this study did not assess LDN’s ability to reduce the fatigue and other symptoms in ME/CFS it explored LDN in a way that had never done before and it did it in ME/CFS to boot. That itself is quite unusual.
Siloed Fields

What’s taken years to get done in ME/CFS is getting done very quickly in long COVID – and that’s good news for both diseases.
The low dose naltrexone (LDN) saga in chronic fatigue syndrome (ME/CFS) is another example of how long it can take for findings in even a closely related disease to make it to the ME/CFS field. Despite the close biological connections between postural orthostatic tachycardia syndrome (POTS), dysautonomia, ME/CFS, and fibromyalgia (FM) researchers rarely collaborate, and rarely even seem to track findings in other diseases.
It took 8 years and dozens of small fiber polyneuropathy (SFPN) fibromyalgia studies, for instance, before David Systrom’s ME/CFS SFN study indicated, to no one’s surprise, that SFPN was commonly found in ME/CFS. Ditto with low-dose naltrexone (LDN). Despite LDN’s wide use in ME/CFS, it took 7 years from the date of the first FM trial for the first LDN ME/CFS study to show up. That study had moderately good results, but its methodology left much to be desired.
Things are already different in long COVID, though. Not much more than a year after long COVID was found, the first small fiber neuropathy has already been published, and the first low dose naltrexone study is already underway!
Aussies Take New Approach to LDN
ME/CFS may be lagging in the LDN field but Sonya Marshall-Gradisnik‘s Australian ME/CFS team at the National Centre for Neuroimmunology and Emerging Diseases (NCNED) undoubtedly shook the field up a bit with their new finding. Not only did they demonstrate a new property for LDN – its potential to improve natural killer cell functioning – but they linked LDN to their intriguing hypothesis that ion channels problems are causing ME/CFS
The NCNED study did not assess the impact LDN has on symptoms in ME/CFS. We’re still waiting on a good study to assess that. Instead, they assessed the effects LDN may be having on the one really major immune consistently found in ME/FS – the inability of natural killer cells to do much killing.
Natural killer cells make up from 5-20% of the lymphocytes in the human body and man the first lines of our immune defense. Twenty years after the failure of NK cells in ME/CFS to kill pathogen-infected or otherwise damaged cells in ME/CFS, the cause remains unclear.
The study wasn’t just about NK cells, though. The NCNED group has been using natural killer (NK) cells to explore their idea that reduced calcium influx through the transient receptor potential (TRPM3) ion channels is causing natural killer dysfunction as well as ME/CFS.
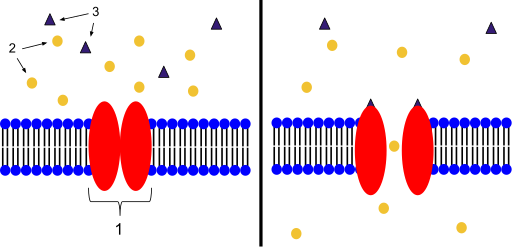
Ion channels control the action in many cells. The NCNED believes problems with a specific channel called TRPM3 could be causing the symptoms of ME/CFS.
The Griffiths team has dug deeper into the NK issue than any other group, and a recent study suggested that reduced TRPM3 activity may be preventing NK cells from tricking pathogen-infected or otherwise damaged cells into committing cellular suicide (apoptosis). (Apoptosis is an orderly process that ensures that the pathogens infecting the cells are destroyed with it.) The study suggested that increasing TRPM3 activity could improve natural killer cell functioning.
The TRPM3 receptor problem, though, potentially goes far beyond NK cells. Since TRPM3 receptors affect a fundamental process – calcium and magnesium homeostasis – they play a role in many physiological processes. They’re particularly abundant in the dorsal root ganglia, a key sensory signal transmitting station that has been implicated in fibromyalgia. Problems with heat/cold sensations and pain hypersensitivity have been associated with them.
As signaling pathways associated with opioid receptors can inhibit TRPM3 receptor activity, they were of interest to the Griffiths group. These opioid signaling pathways don’t just alleviate pain: they also affect immune and central nervous system functioning.
The latest Griffiths study, “Potential Therapeutic Benefit of Naltrexone in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Role of Transient Receptor Potential Melastatin 3 Ion Channels in Pathophysiology and Treatment“, found that NK cells of ME/CFS patients taking LDN had normal TRPM3 functioning. Since inhibited TRPM3 functioning has been linked to poor NK cell functioning, it’s possible that LDN was able to restore NK cell functioning.
To know if that’s true, we need placebo-controlled studies but the potential is there. The authors also believe that reduced endogenous opioid and beta-endorphin production in ME/CFS may be responsible for some of its symptoms.
While this study did not document that LDN reduces symptoms in ME/CFS, it does something potentially quite important: by demonstrating that LDN may be able to restore functioning in NK cells, it may help lay the groundwork for a large, effective study. Dr. Staines reported:
“This study serves to support the repurposing of marketed drugs and support prospective randomised clinical trials using Naltrexone in treating ME/CFS patients.’’
Is ME/CFS a TMPR3 Disease?
Natural killer cell dysfunction, while important, is a sideshow to the much bigger question – of whether wonky TMPR3 receptors in other cells could be causing ME/CFS? Because TMPR3 is found on so many cells problems with it could conceivably cause all the symptoms in ME/CFS.
Five years ago, it appeared that NCNED was on the cusp of truly big things. in 2016, the Griffith News report, “Screening test for Chronic Fatigue Syndrome on its way“, stated the NCNED group had “identified new markers that can be used to screen patients and is now looking to partner with diagnostic companies to bring a test to market.” Dr. Marshall-Gradisnik expected the test “to become a laboratory standard to provide more certain, and cost-efficient, diagnosis for CFS.”
Three years ago, Science Alert reported that “Staines and his team have been working to figure out the best markers that can be used to test for these faulty receptors, so they can begin to create a CFS/ME test”, and were “looking for medications” that act on these receptors. They were also looking for medications that act on these specific calcium ion channels in the hopes of finding potential treatments for the disease.
Recently, Marshall-Gradisnik said in no uncertain terms that she believes an ion channel dysfunction is causing ME/CFS.
“We now further understand that the pathophysiology of ME/CFS is due to ion channel dysfunction and the interaction of the opioid receptor that causes impaired Ca2+ signalling and Ca2+-mediated cell functions, including immune function,”
The Gist
- Low-dose naltrexone or LDN is a compounded drug often used in fibromyalgia, ME/CFS, and other diseases to reduce pain. It appears to do this by temporarily shutting down the opioid receptors – causing them to kind of explode with a burst of endogenous opioids that reduce pain. The fact that LDN often works in FM suggests that the endogenous opioid system is not working well. LDN may also be inhibiting the activity of microglial cells in the central nervous system.
- Since the first LDN trial in fibromyalgia seven years ago it wasn’t until last year that the first retrospective LDN study was done in ME/CFS. Similarly, it took almost 10 years after small fiber neuropathy was documented in FM for the first ME/CFS SFN study to appear. Long COVID seems to be breaking this trend – both LDN and SFN studies have already been completed or are underway in long COVID.
- Building on a recent finding which suggested that TRPM3 ion channels were dysfunctional in the natural killer (NK) cells in ME/CFS, the Australian team assessed TRPM3 ion channel functioning in ME/CFS patients taking LDN and found that the channels were functioning fine (!). That suggested, but does not prove – as no controls were involved in this study – that besides helping with pain, that LDN may be helping to improve immune functioning as well. The Australian group believes that a dysfunction in these ubiquitous ion channels is causing ME/CFS.
Five years ago, it seemed that the group was on the cusp of producing a diagnostic test for ME/CFS. Three years ago the search for medications to affect the TRPM3 ion channel was underway. I’m attempting to find out how those efforts are going.
Several small studies have found that LDN produces positive benefits in FM or ME/CFS but both diseases lack the large placebo-controlled, double-blinded studies needed to validate those findings. Given that drug companies have no interest in easily compounded drugs, one might think that the National Institutes of Health – with the urgent need to develop better pain drugs – might be willing to pick up the tab but it’s refused to fund LDN studies. Thankfully, two large and rigorous studies are, however, underway in Denmark and Spain.






I took very low dose Naltrexone for a while. I started having suicidal thoughts, which is virtually unprecedented for me. Turns out that the pharmacist had warned my husband of this possible side effect when my husband picked up the medication. But my husband had forgotten to mention it to me. I never see this discussed. Perhaps it’s very rare. But people should be informed.
Sorry to hear that! LDN was initially touted as pretty much of a side effect-free drug but it’s pretty clear that it’s not. While many people do very well on it, it can produce some nasty side effects in some. If it’s taken at very low doses at first and slowly ramped most of those side-effects reportedly will disappear for most people. Anyone wondering how to do this can check out the LDN Resource Section linked to at the bottom of the blog.
A friend of mine is a menopausal woman. LDN makes her ovulate again, which has great trouble for her. She can only stop taking medicine. Relevant animal research was found after inquiry. The impact of a drug may be extensive.
I felt depressed at 9 mgs but am fine at 6mgs. The benefits are mind boggling. Including helping recover from the side effects of the Pfizer vaccines. My POTS is almost completely gone. No more cold intolerance. My thyroid is normal again. My tolerance for medicines has improved significantly. The list goes on..
JD how long did it take to start seeing these improvements from LDN?
That’s amazing JD….I have to try again!
I thought “low dose” LDN was 4.5mg or lower?
I’ve had ME/CFS for 30+ years and I started LDN about 3 years ago at 1.5mgs. I didn’t see results for about 6 months. When I did see change it was so gradual that I quit for two weeks and that’s when I really started to notice the changes. Every dose change has brought new benefits but always slowly!!! Facebook has great private support groups. Many stories like mine.
Sorry to hear that Jackie!! I too had unprecedented suicidal thoughts which timing wise clearly had nothing to do w LDN and everything to do w Lyme disease (esp since they resolved after really jumping on my Lyme protocol).
I haven’t had any discernible side effects to speak of w the stuff. I started in Aug 2018 on 1 mg … worked up to 2 mg in early 2019 perhaps? Had a 3 mg at one point and then jumped to 4.5 mg when the pandemic started which I think may have helped my physical symptoms so much that I didn’t even recognize the neuropsychiatric stuff as Lyme. 😳
I’ve had Lyme since July 2017 and some undiagnosed gaslit combo of fibromyalgia and/or mild ME since 2004ish.
For anyone considering LDN I can say that for me (esp considering when I’ve gone without it? And what most drastic before/after difference is?) I think it helps keep my system from “falling off the cliff” and relapsing into very-sick territory. I still have daily fibro-flavored all-over pain and some joint pain flares from Lyme… and I still get fatigued… but the crashes that I used to think of as more ME-related?! where my glands swell up and I’m compleeetely exhausted and flulike and dysautonomic/heart weird etc for sometimes 3+ months at a time?! Don’t really happen any more? Esp after increasing to 4.5. I will continue experimenting w forms though!
I’d like to learn more about liposomal LDN and dextro-naltrexone. 🙏🏻
I’m going to be the one asking two stupid questions… I have taken 4.6 LDN daily for five years. No bad effects, no good that I can discern.
However, since I take Valium at night to sleep, and since I also still enjoy drinking wine a few times a week, am I completely undoing any good the LDN might be making? I’ve tried researching this but have not found an answer.
What dose were you taking? In the Facebook group I work with we find that some people have to take an unusually low dose.
We have been arguing the case for some time that if users have reactions when starting LDN that they should just keep dialing the dose back to a tolerable level. We’ve had some people dosing at 0.1mg and some lower. I’ve suggested that it may be that the system has to get used to the “idea” of LDN before working up to a normal dose. Unfortunately it has been common to see comments from doctors that doses below 1.5mg are “useless.”
So I am glad to see this interesting interview with Dr. John Kim where he talks about the value of starting patients on low doses — even like 0.01mg — even for those not on opiates and then working up. To jump to that part go to the 13:40 point.
image link first (video is the next link): https://www.screencast.com/t/sghGnKJKvf
https://vimeo.com/293553098
Another excellent talk from him: An Archived LDN Presentation- ULDN, Micro Dosing with Dr John Kim: https://the-ldn-radio-show.captivate.fm/episode/an-ldn-prescribers-experience-uldn-micro-dosing-with-dr-john-kim
BTW sometimes if the dose has been too high it’s good to skip a dose to let the system clear before going lower.
Dosing poll in the Chronic group… [group Low dose Naltrexone (LDN) for chronic illness & infections…. https://www.facebook.com/groups/108424385861883%5D —
https://www.facebook.com/groups/108424385861883/posts/2361598247211141/
Can LDN make symptoms worse? Dr Piper…https://ldnresearchtrust.org/can-ldn-make-symptoms-worse?fbclid=IwAR121FUyizSr9UUylrlxjDG2zGC3lS36KVmTCHSF2Ik8bZQ2Q_uwgmpt_08
A related video about anxiety and depression… https://ldnresearchtrust.org/can-ldn-cause-anxiety-and-depression?fbclid=IwAR2ICGzcF1JMwZBjrKDM-VUcotl2IoQd6_IRQiaxcPBDQZQ1XsT6fbcOy6Q
And here is a podcast where a woman with ME/CFS shares her experience about dosing…
Lori talks about LDN for ME/CFS…. https://www.youtube.com/watch?app=desktop&v=kZ2LvnpMEvA&fbclid=IwAR23ZLyT4Tu2j16K7IHTwAJh5xsHXlbrMoZDQrWlnJ-14a7aw7p6BF-DXeA
Ah, ever hopeful research…
I have tried LDN, mostly because my doctor wanted me off Norco. I have 6-7 level chronic joint pain–thank you EDS. In order to function I take low doses of Norco plus acetaminophen, curcumin and ibuprofen.
Unfortunately one cannot take Naltrexone with any opioid so I had to give up the Norco. My several months on LDN was horrible. It did nothing for either my pain or fatigue.
In desperation, I discovered kratom because it hit different pain receptors (mostly) than Norco and LDN wouldn’t interfere with them. Since LDN had a very short half life, I took kratom in the morning and LDN in the evening (and didn’t tell my doctor). This worked O.K. until I had surgery and had to formally go off LDN to be able to take opioids for post op pain.
Just sharing this because the LDN experiment in the Ehlers-Danlos community was mixed. It worked well for some, but not for all. Not sure what effect it was having on things like appropriate aptosis or inflammation etc., but when the pain level is so high that it interferes with function, in my life, pain control trumps other not so obvious effects.
I should also mention that I usually have side effects with just about every drug I take, but LDN was very a very easy drug to tolerate–at least for me. The most commonly reported side effect was vivid dreams and perhaps some initial sleep disturbance (which usually faded with time). Too bad it didn’t help, but maybe it will for some.
Glad to see an article on LDN and ME/CFS! I am working on a brief case study that will discuss how LDN (in the morning, 30 minutes before food or other supplements) has helped eliminate depression-like symptoms in my daughter, who has EDS and ME/CFS. It was like turning off a light switch! Since supplemental thyroid hormone did exactly the same thing before the body adjusted to reduce the production of natural thyroid hormone, my hypothesis is that the LDN is operating through a thyroid pathway, by reducing inflammation that is impairing the body’s ability to produce or metabolize thyroid hormones. This hypothesis builds on observations that Kent Holtorf makes in his article in the LDN Book. Will post a link to the case study when completed.
Thanks Jeffrey, looking forward to that. LDN has been so poorly studied relative to other drugs that who knows what effects it may be having. I was surprised to see it being tested in natural killer cells! We need studies with controls but so far so good with the NKC’s. The killing capacity of my NK cells is just the pits….
Isn’t low cytotoxicity in NK cells one of the most consistent findings in ME/CFS patients? Why still not used as a biomarker…
Yes. low NK cell cytotoxicity is. That’s a good question. I wonder if it’s because these tests are not easy to run? Perhaps a good biomarker needs to be readily available and easy to duplicate (???)
Here’s a write-up of my daughter’s experience with LDN and an explanation of my hypothesis for mechanism. Since it includes personal details about her condition I’ve used the pseudonymn, John Doe. https://medium.com/eds-perspectives/inflammation-masquerading-as-depression-a-case-study-of-the-beneficial-effects-of-low-dose-5bdaf0766d7f . I’d welcome feedback or corretions.
Hi Jeffrey,
I read your Medium article and have a lot of questions. I take 150mcg T4, 50mcg T3, and 4.5mg LDN daily, as I have for 4 years. I have a number of very high inflammation markers. Am trying to understand how your analysis applies to what I’m experiencing.
How do I get in touch with you?
Learner1 on Phoenix Rising
I tried it and still use it. It has SOME effect- Alone, it is totally useless. I use BCG shots every 2 weeks. It has a dramatic impact. I can work out in the gym twice a week and swim twice a week. I am able to work full time after one year on BCG vaccination. My shoulders are not very pretty from the scars but who cares. If anyone is interested in it, I am happy to inform you guys.
Adam, I’m interested to hear more about your BCG treatments. I had thought it was just one vaccine? Who does these treatments for you?
please find my reply bellow
I would also love to hear more about how you are getting the BCG vaccine. I read about it when I got the fm/a test but I have no idea how someone would go about getting it and my doctors won’t even give it a try when I tell them about pretty mainstream things like provigil
please find my reply bellow
i would defenitly like to know more on the bcg shots! did a search what it was but could not find bcg. can you also put a link to it and witch specialist gives it to you. thanks!!!
Please tell me more about the BCG Shots. How long have you had ME/CFS and what was your condition like before taking the shots? Your response is highly appreciated.
Thanks
please find my reply bellow
@Adam Keri
I am VERY interested in this because from my (quite extensive) research into the pathophysiological underpinnings of neuroinflammation (see here, soon to be published: https://osf.io/ef3n4) stimulating the innate immune system should be the way to go in ME/CFS (plus, has been successfully explored way back: https://me-pedia.org/wiki/Staphylococcus_vaccine). So fever therapy with PAMPS may be one way, using a vaccine with “trained immunity” effect (BCG, influenza, measles, oral polio) another. Where do you get the BCG from? I am living in Germany, the only source I have is via Japan, but 1 shot then costs around 120 $ … So please comment and possibly also send me a mail with as much information as possible (Herbert.Renz-Polster@posteo.de). Thank you, we need these patient driven “trials” to make up for the lack of funding in ME/CFS!
please find my reply bellow
I would like more information as well @Adam Keri. Did the dose of every 2 weeks come from trial and error or have you been using it that way from day 1? I’d love details about the manufacturer and amounts that you’re using.
Dear All,
BCG treatment was my idea. It was built on some facts:
1.CFS is an immunological disease with inflammation and autoimmune-like features (see: Scheigebogen research in Berlin)
2. There is hardly any improvement without immunomodulating substances.
3. I had to find something that is available on the market and which is relatively cheap (especially bc the result is always uncertain).
4. I was able to find publications in the Hungarian Compendium (I live in Hungary) referring to live vaccines as immunomodulating substances (BCG, MMR, polio). Thus, I was searching for medical publications in English and German.
5. I was able to locate a Swedish professor who is now 90, have CFS and treated patients with Staphylococcus vaccine. That vaccine had since been withdrawn from the market.
6. I was looking for live vaccines with antiinflammatory activity, which also have a favorable impact on autoimmunity. Live vaccines are suitable for it.
7. I found BCG vaccine, which is 100 years old. Medical publications regarding BCG revaccinations in inflammatory and autoimmune diseases are plentyful.
8. I contacted the Swedish professor and asked him to send me his Staph treatment schedule and asked him if it could also been used with BCG. The answer was yes.
9. The doctor told me to experiment with caution on my own experiences. Treatment shall start at a low dose:
0.1 dose / 1st week
0.2 dose/ 2nd week
0.3 dose/3rd week
0.4 dose/4th week
0.5 dose per 5th week
Then 0.5 dose biweekly.
It shall be administered intracutanous way. You can learn it, not difficult. It will leave scares on your shoulder but it is worth it. Sunshine helps with it.
My experience:
-from my inability to work I work full time
-from 0 gym days, I work out in the gym 2x per week, and swim 1 hour 2x week.
-my digestion has greatly improved and sleep well
I am now a stable 75%, which is very good considering the fact that this disease started more than 10 years ago. There are some residual symptoms: I am getting more easily tired after sport, need more time to sleep (8-9 hours) and have sometimes light sleepiness. It is manageable.
How I got the vaccine: I am a lawyer and no doctor wanted to experiment with BCG vaccine. Therefore, I filed myself a petition to the Hungarian Drug Regulatory Body requesting approval for BCG’s off-label use. I asked an immunologist to stamp my petition. This petition was approved one year ago. Then, I contacted a wholesaler and ordered 30 vials for approximately 800,-dollars. This is for 15 months.
All of my symptoms have improved and my body is able to adapt again (e.g.: sport, work etc.).
In the meantime, BCG proved to be effective for COVID and long-COVID as well. I contracted COVID last year and symptoms flared up. I was able to recover (from fatigue and foggy brain) in a short time. Right now, I do not have any symptoms.
Let me know if you need further information or help. I studied law in Georgia (USA), understand you very well.
https://www.ejgm.co.uk/download/bcg-is-a-good-immunotherapeutic-agent-for-viral-and-autoimmune-diseases-is-it-a-new-weapon-against-7892.pdf
https://www.researchgate.net/publication/317096522_BCG_and_protection_against_inflammatory_and_auto-immune_diseases
BCG can influence immune-metabolism. It shifts the balance in cellular metabolism towards glycolysis as energy source rather than oxidative phosphorylation. This shift known as the Warburg effect highly favors expansion and function of Treg cells which prefer glycolysis to obtain energy.BCG-induced Treg expansion by modulation of immune-metabolism might be useful for tackling several inflammatory and autoimmune disorders.
@Adam Keri
Thank you so much for posting this! It may be of tremendous value to pursue in a study. It´s unfortunate that BCG is hard to get a hold on in Europe. I have shared your experience with the Yale researcher Akiko Iwasaki who is trying to understand the effects of vaccines for Long Covid. We need as much input as possible. If you have any more experiences or insight don´t hesitate to share, Herbert (Herbert.Renz-Polster@posteo.de)
@Adam Keri
Thank you so much for your insight into treatment with BCG. I have a practical question. Once you open a BCG ampoule and mix the powder with the diluent you are supposed to use up the vaccine within a few hours. So if you only take shots every two weeks – how do you proceed? You can´t use a new amp. every time??
Thanks for an answer.
Herbert
Thank you so much @Adam Keri for your detailed response! I’m curious about Herberts question above as well regarding the shelf life of the ampoule. Are you opening one, mixing parts of it with liquid, and then storing the rest to use later or are you opening an ampoule with every injection and discarding the unused?
Also, could you provide details about which manufacturer you’re using and how you contacted them? Do they have a website where you upload your documents and ordered? I’m in the United States and I’m curious about how I could obtain an off-label use voucher and how I can place an order once I obtain it but I’m sure it’s a very different process here than it is in Hungary.
Dear Adam,
Would you mind sharing what triggered your ME/CFS ? It may have some relevance on what works better or worse as the symptoms and hence root cause spectrum despite communalities is very wide.
Thank you, M.
What is BCG?
Nice write up Cort, thanks. I didn’t have any luck with LDN. Tried at 0.5mg to start, couldn’t sleep and felt strange, then tried at what I’d call a homeopathic dose which did nothing. Was able to build up to a certain point but never had any improvement. Seems like the more severe people are doing better with it.
I have been on LDN for around 5 years and my doctor thinks it is part of the reason I a, so much better, almost normal, still have relapses after doing too much. I have ad CFS for 28 years, much of it bed ridden. I started slow and have been fine with it. I also take isoprinosine, (imunovir) which also could be the reason I a, so well. I have been taking it now for 15 years. Expensive but I think it works for me.
Hi Frankie, how many imunovir tablets do you take a day? Is this something to stay on long term? I started 3 weeks ago and still have the fatigue. Would like to hear more. Thanks!
I tried LDN once. 4.5 mg..,for a week. Maybe I should have started low and slow, as others suggest..(I have read .5 or even .25 mg)…for me it caused a massive immune response. After taking it for a week, I developed fever, chills, aches, lymph node swelling, coughing (like crazy), and some of the most nasty gunk coming out of my sinuses from way, way deep. I felt like my body was going after something it needed to, the problem was I just couldn’t take it. The coughing was so intense, lymph nodes swelled big, and I was exhausted…so I stopped. The exhaustion remained for weeks and weeks until I finally got back to my baseline. The interesting thing to me was the increased symptoms I experienced were exactly like the original symptoms I experienced when I first got sick and developed CFS, and never recovered…and this was over 10 years prior to ever trying LDN.
Definitely way too high of an initial dose but it’s interesting how it replicated your original symptoms!
I have been taking 4mg of LDN for a year now. Thyroid now completely normal (narrowly escaped a thyroidectomy). Mood has improved and pain has diminished but not totally disappeared.
When I went on LDN at night and started low and ramped up my health finally stabilized. I am not 100% but I am much more functional and know better what to expect rather than the highs and then crashes I had with only Abilify (I take both now and credit them with me doing as well as I am, being previously bed bound). I am now at 6mg of LDN and 2 mg Abilify, but I went up very slowly on LDN from around 1 mg.
I’m skeptical.
I’ve also been underwhelmed and disappointed by these Australian researchers, who seemed to promise so much, and have always talked a good talk….
In my eyes, they’ve lost credibility.
I’m trying to get more info on the status of their efforts. They did have some pretty dramatic announcements. On the other hand, things always seem to take longer than we expect. I think it’s been at least five years since both Fluge/Mella and Ron Davis reported that something in the blood of ME/CFS patients could be causing ME/CFS. I thought that something was going to be quickly identified and then we’re off to the races – yet we are all this time later with no answer to that.
Ion channels certainly are an interesting possibility that’s been proposed for both ME/CFS and FM before. I hope I hear back from them.
My problem is the ‘big talk’. Maybe some of these researchers need to tone down the hype.
Given their talk, they have failed to deliver on their own self hype.
I don’t care if people talk themselves up so long as they deliver.
Weren’t they proclaiming they had a diagnostic test about 5 years ago?
Maybe I am too cynical.
I think you’re absolutely right to ask what’s going on with the diagnostic test. It was a big and quite exciting claim. I asked them about that a couple of other things about a week ago. Have not heard back yet.
Yeah those guys science seems sound, but the claims they keep making are just gross and off-putting. Anyone can advise how to reconcile the two.
Many of these researchers don’t seem to know the concept of ‘under promise, over deliver’
I tried LDN but only got as far as three doses. I started with .5 and felt fine. The second dose made me feel really weird and in terrible pain. My head felt as if it was swollen. I tried a third dose much smaller but not sure how much as dropper measure started at .5 so may have been about .2 felt so ill and started to have terrible anxiety and was really jittery and wired. Stopped taking it but jittery feeling persisted for weeks after. Kept bottle and wanted to start again but just didn’t want to experience that again and threw it away. I could have tolerated the extra pain in the hope that it would have subsided in time but not the other strange effects that I experienced. Don’t know if the dextro-naltrexone would be a better option. Part of me wants to try again as I ducked out so early but still very concerned about those side effects for me.
Has anyone tried the Gates Foundation? : Research Grants, https://www.gatesfoundation.org/about/how-we-work
Dose: Dr. Nancy has stated in Europe they go as high as 9mg per dose, maybe some need more than 4.5mg.
The reason some prefer making there own, that way the dose can easily be altered. there are simple instructions (web) 50mL distilled water + 50mg Naltrexone = 1mg/1mL Also twenty drops = ~ 1mL stored refrigerated one month.
Naltrexone is a Serotonin, Dopamine antagonist so lost sleep is no surprise, almost all sleep meds are Serotonergic.
As for me I just can’t take the last step to kick the pain meds, at low dose but still that step is too big too much stress.
LDN is used by Dr. Klimas’s group for multiple effects. In a fall conference of 2019, Dr. Norma Rey stated that LDN is consistent in increasing NK Cells and function. They also use inosine for the same reason but LDN has proved to be more reliable. My doctor also believes it improves the function of the HPA axis as in my case after being on LDN for 9 months, I no longer needed adrenal supplements. No side effects for me. From a friend with fibro, I understand the pain relief is trickier. She has to take a rest from it once in awhile. My pain is from Myofacial Pain Syndrome and it is controlled by a combination of magnesium/Malic acid/B-ribose.
I don’t really understand why this is considered new or confusing information.
Janet MOsser, my sister has myofacial pain syndrome. Could you tell me the combination of magnesium/malic acid/B-ribose and the amount you take? Also could you tell the where you get the supplements. Any information would be greatly appreciated.
Can you go cold turkey on this stuff after starting on it?
Lono,
Yes I have gone cold turkey and didn’t even notice any symtpoms from going off it,
Just entering if anyone has found NAC useful for brain fog like our daughter has? We haven’t tried LDN yet.
The thing I find strange about the Griffiths research is that they never seem to report any evidence of subsets, unlike Systrom, Lipkin, Younger, Scheibenbogan, Prusty, etc. I may not have read their research thoroughly enough but it would be interesting to know what percentage of patients have this TRPM3 / ion channel flaw, because if it really is 100% of patients it implies it is a by-product of the illness and not the cause. We already know that LDN only works for a subset of patients so this line of research is probably still very much a work in progress.
I worked up to 3mg daily which resulted in awful side effects. With guidance from Facebook groups, I’ve worked back down to 1.5mg every second day. Currently very fatigued after Pfizer, but I am overall improving on this lower and less frequent dosing. It isn’t a cure – more a tool in my tool box. I think everyone is different 🙂
Hi cort, thank you for this interesting article. NHS does not allow for clinical trial for FM/CFS is against humanity. Unless our numbers is not large enough for them to think of it against humanity. How about a petition to request they should allow it, even encourage it.
For more information on LDN
Low dose Naltrexone (LDN) for chronic illness & infections…. https://www.facebook.com/groups/108424385861883
Hey Cort, yes it sure does help CFS, I use 8mls of naltrexone every 2 to 3 hrs to keep calcium ion channels opened. Caffiene is an important part of the protocol too, I think you have my abstract already? Thanks Vanessa